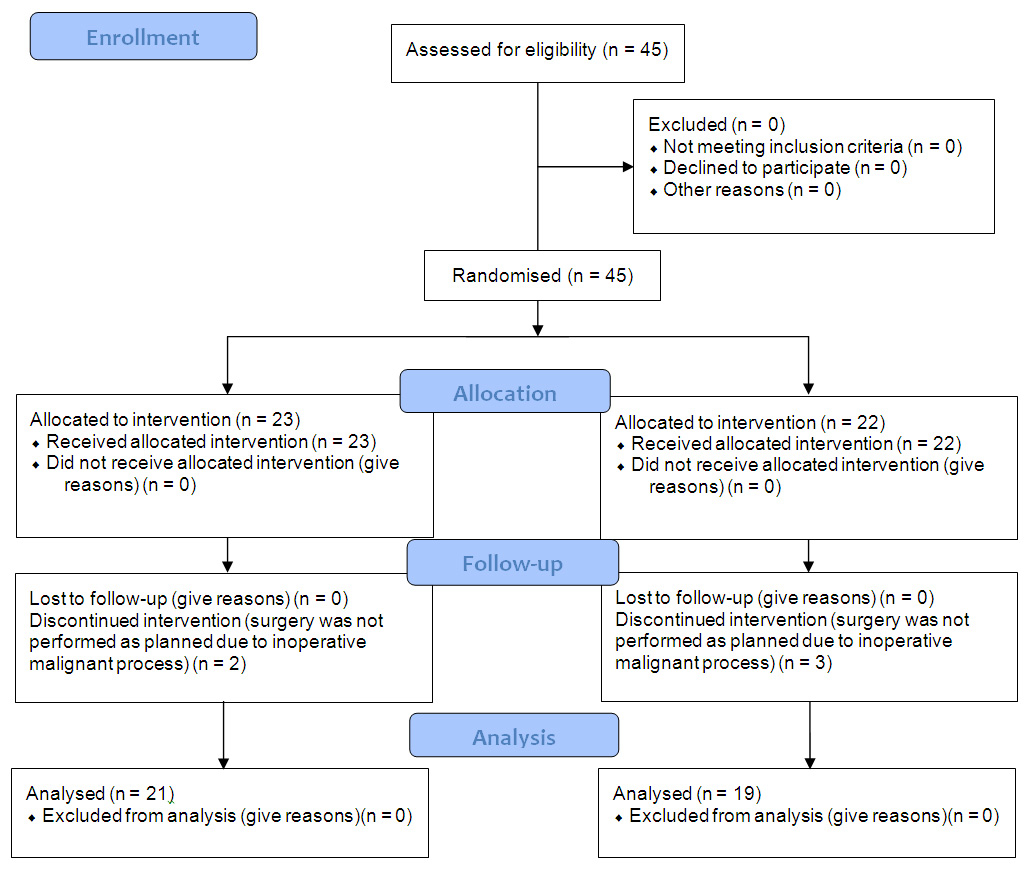
Figure 1
CONSORT flow diagram.
DOI: https://doi.org/10.4414/smw.2012.13689
Awareness during surgery is a very serious problem, affecting 0.1–0.2% of all surgical patients. Such incidents are the cause for 2% of the legal claims against anaesthetists, while patients with an intra-operative awareness experience describe it as the worst thing they have ever suffered from [1]. Pain, anxiety and inability to react due to muscle paralysis often lead to the situation called post-traumatic stress disorder which demands psychiatric support. The fact that there are patients who report intra-operative experience, even several days after surgery, raises questions about the way the anaesthetic drugs interfere with the mechanisms of memory and consciousness while, in the literature, there are studies proving that even deeply anaesthetised patients can be influenced by auditory stimuli without being able to recall them [1, 2]. In order to prevent such cases of awareness, anaesthesiologists often use larger amounts of anaesthetics which leads to prolonged ventilation and post-operative sedation of the patients. On the other hand, it has been reported that “deep” anaesthesia is associated with increased 1-year mortality, conceivably due to impairment of the immune system [4]. From all the available devices used for monitoring of anaesthesia depth, only bispectral index (BIS) monitoring has been proven to be effective [1–3, 5]. It records the electroencephalogram from 4 electrodes and after processing it with mathematic algorithms it generates a number from 0 to 100. When the BIS value is lower than 40, the patient is in a deep anaesthesia state, and when the value is over 80, the patient is under light sedation [3]. Using BIS monitoring will probably help in optimising anaesthesia levels, neither too light nor to deep. It has been reported that BIS monitoring is useful to reduce drug consumption and awareness and to shorten recovery time [6–9]. Gan et al. reported that titrating propofol with BIS levels, targeted between 45 and 60 during balanced anaesthesia, decreased propofol use and significantly improved recovery [10]. Also, Pavlin et al. reported that application of BIS monitoring is associated with a modest reduction in end-tidal sevoflurane concentration and similar reduction in recovery duration [11]. In that way, titrating anaesthesia according to the BIS levels measured will help to extubate our patients as soon as possible, avoiding all problems arising from prolonged ventilation.
In the current study, we tested the hypothesis that BIS-guided anaesthesia compared to standard anaesthesia protocol will result in faster extubation and lower intra-operative anaesthesia consumption.
The investigation was carried out with due approval from the Ethics Committee of University Hospital Dubrava, Zagreb, Croatia, and with informed consent from all study subjects. The investigation was also registered on ClinicalTrials.gov (NCT01470898).
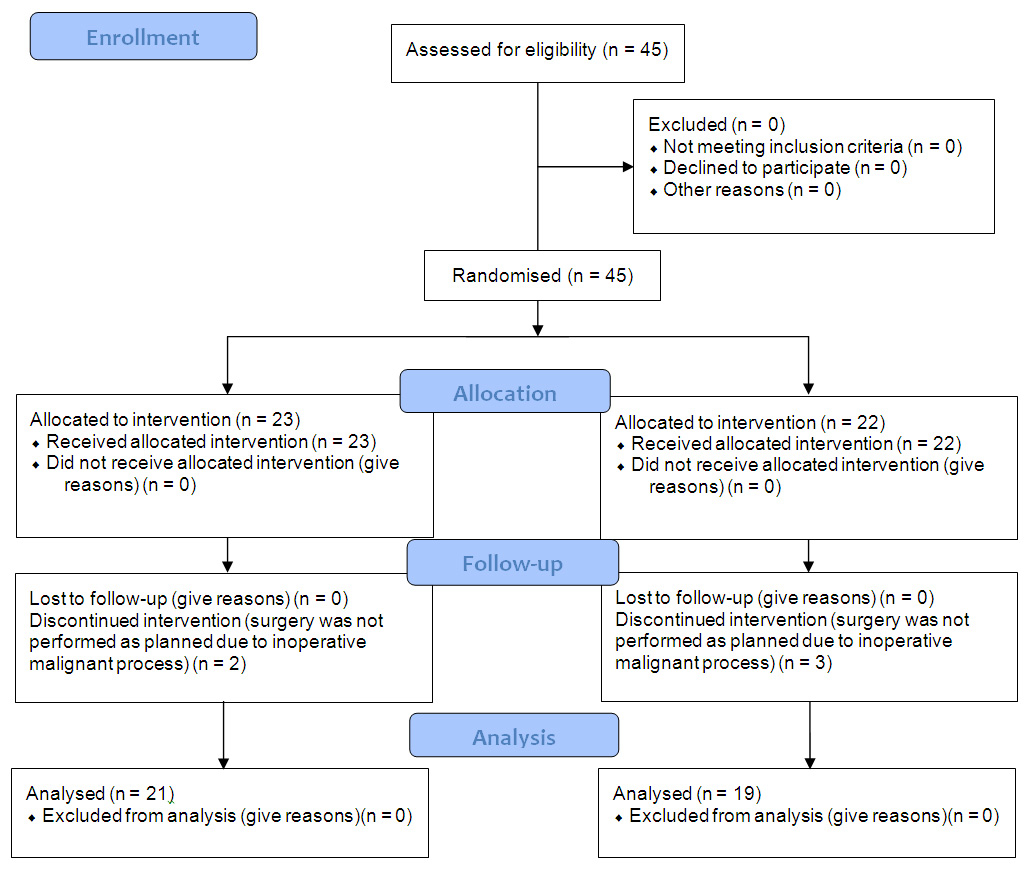
Figure 1
CONSORT flow diagram.
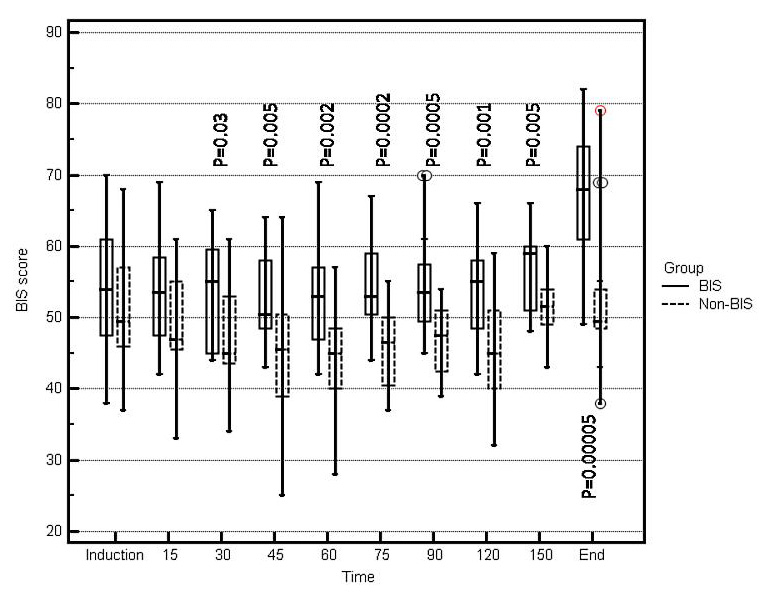
Figure 2
Comparison of BIS score at different time points during surgery between groups of patients with BIS-guided and non BIS-guided anaesthesia. Significant differences are marked and p values are given.
The study included 45 patients undergoing major abdominal surgery under general anaesthesia in University Hospital Dubrava, during a six months period, between February and July 2011.
Patients were eligible if they were aged 18 years or older, and of ASA (American Society of Anaesthesiologists) physical status II or III. According to ASA pre-operative classification, patients with ASA II are represented with mild systemic disease, and those with ASA III are represented with severe systemic disease that limits activity, but are not incapacitated. Exclusion criteria were memory impairment, psychosis, known or suspected electroencephalograph abnormality (e.g., epilepsy, previous brain operation), chronic use of psychoactive medication, and operation time exceeding six hours.
According to a computer generated randomisation list, patients were randomly assigned to receive BIS-guided anaesthesia (group 1) or routine anaesthesia care as a non BIS-guided group (group 2). The non BIS-guided group was studied while the BIS monitor was attached to patient, but the screen was blinded to the anaesthesiologist in charge. All values were recorded by the younger anaesthesiologist, who was not involved in the anaesthesia maintenance. All other aspects of peri-operative treatment were similar, including choice of anaesthetic agents and monitoring.
The operation was performed under general anaesthesia using midazolam (0.15 mg/kg), fentanyl (2 µg/kg) and vecuronium (0.1 mg/kg) to facilitate endotracheal intubation, and 1.5–2.5 MAC of sevoflurane, nitrous oxide 50% in oxygen, boluses of fentanyl and vecuronium for maintenance. Intra-operatively, after induction doses of fentanyl, anaesthesia was mainly balanced with sevoflurane. Electrocardiography (EKG), invasive blood pressure (IBP), peripheral oxygen saturation (SpO2), and end-tidal CO2 (etCO2) were monitored.
A BIS sensor was applied to the patient’s forehead before induction of anaesthesia and connected to a A-2000 BIS monitor (Aspect Medical Systems, Newton, MA, USA). In the BIS-guided group targeted levels of BIS were between 50 and 60. After the surgery and recovery from anaesthesia, patients were transferred to the intensive care unit (ICU) for continuous monitoring of vital functions and homeostasis.
At the induction of anaesthesia, and every 15 minutes during the operation BIS levels were recorded. Additional analysis included measurement of heart rate (HR), systolic blood pressure (sBP), end-tidal CO2 (etCO2), operation time and extubation time. Finally, all patients were visited on the first post-operative day and interviewed about intra-operative recall.
A randomisation schedule was computer generated by a biostatistician (not otherwise involved in the study). Random function from Microsoft Excel 2003 was used to randomise patients into arms. Patients were assigned to either BIS-guided or non BIS-guided anaesthesia.
Numeric values are presented as percentages, medians, minimal and maximal values. Comparisons between the two groups (BIS-guided vs non BIS-guided anaesthesia) were performed using Mann-Whitney U test. With alpha = 0.05 and preset values of time to extubation before the study of 30 ± 8 min in the BIS guided group and 40 ± 8 min in the non-BIS guided group (SD was estimated to 20% of higher time to extubation) and at least 20 subject per group, the power of the study was calculated to be 89%.
Out of 45 patients recruited for the study, 5 patients were excluded because of an inoperative malignant process found intra-operatively. In these cases, the surgeon performed only explorative laparotomy and colostomy. There were 21 male and 19 female patients with a median age of 65 years (25–84 years). A flow diagram of the participants is presented in figure 1. Statistical analysis of demographic and clinical data showed no significant differences among the groups in baseline values of ASA score, body mass index (BMI), body surface area (BSA), age, haemoglobin level and haematocrit level (table 1). Parameters of HR, sBP, etCO2 did not differ significantly between groups. In the non BIS-guided group, we found significantly lower BIS levels (p <0.05) from 30 min further to the end of the operation compared to BIS-guided group (fig. 2).
Time to extubation was significantly shorter (17.5 min vs 75 min, p <0.001) in the BIS-guided group (table 2). There were no statistically significant differences in the required amounts of anaesthetics and operating time (table 2). In the post-operative interview, none of the patients reported explicit awareness intra-operatively. There were no adverse events or side effects during investigations.
| Table 1: Comparisons of patients’ baseline characteristics. | |||||||||
| BIS guided anaesthesia | Non BIS-guided anaesthesia | p | |||||||
| N | Median | Minimum | Maximum | N | Median | Minimum | Maximum | ||
| Gender | 0.752 | ||||||||
| Male | 11 | 10 | |||||||
| Female | 9 | 10 | |||||||
| Age (years) | 20 | 64.50 | 39.00 | 84.00 | 20 | 66.50 | 25.00 | 81.00 | 0.499 |
| ASA score | 20 | 2.00 | 2.00 | 3.00 | 20 | 3.00 | 2.00 | 4.00 | 0.291 |
| BMI (kg/m2) | 20 | 26.50 | 17.50 | 35.00 | 20 | 25.50 | 21.00 | 30.00 | 0.946 |
| BSA (m2) | 20 | 1.90 | 1.36 | 2.24 | 20 | 2.10 | 1.60 | 2.45 | 0.051 |
| Haemoglobin (g/l) | 20 | 132.50 | 102.00 | 155.00 | 20 | 131.00 | 102.00 | 151.00 | 0.365 |
| Haematocrit (%) | 20 | 0.39 | 0.31 | 0.46 | 20 | 0.39 | 0.31 | 0.47 | 0.685 |
| Heart rate (/min) | 20 | 74.50 | 59.00 | 107.00 | 20 | 75.00 | 63.00 | 97.00 | 0.725 |
| RR systolic (mmHg) | 20 | 123.00 | 108.00 | 196.00 | 20 | 134.50 | 110.00 | 201.00 | 0.117 |
| CO2 (kPa) | 20 | 4.00 | 3.40 | 4.50 | 20 | 4.15 | 3.20 | 4.70 | 0.394 |
| BIS score | 20 | 54.00 | 38.00 | 70.00 | 20 | 49.50 | 37.00 | 68.00 | 0.291 |
| BIS = Bispectral index; BMI = Body Mass Index; BSA = body surface area; RR = blood pressure; CO2 = expiratory partial pressure of carbon; dioxide. | |||||||||
| Table 2: Comparisons of required amounts of anaesthetics, operating time and time to extubation. | |||||||||
| BIS guided anaesthesia | Non-BIS guided anaesthesia | p | |||||||
| N | Median | Minimum | Maximum | N | Median | Minimum | Maximum | ||
| Dormicum® (mg) | 20 | 9.50 | 5.00 | 12.50 | 20 | 7.50 | 5.00 | 13.00 | 0.204 |
| Fentanyl (mg) | 20 | 0.40 | 0.20 | 0.55 | 20 | 0.40 | 0.20 | 0.55 | 0.882 |
| Pavulon® (mg) | 20 | 12.00 | 6.00 | 16.00 | 20 | 10.00 | 6.00 | 16.00 | 0.148 |
| Sevorane (min) | 20 | 155.00 | 30.00 | 240.00 | 20 | 137.50 | 85.00 | 240.00 | 0.457 |
| Duration of surgery (min) | 20 | 195.00 | 130.00 | 280.00 | 20 | 166.00 | 150.00 | 245.00 | 0.060 |
| Time to extubation (min) | 20 | 17.50 | 2.00 | 95.00 | 20 | 75.00 | 10.00 | 310.00 | <0.001 |
| BIS = Bispectral index. | |||||||||
Our results showed significantly faster extubation in the BIS-guided group of patients. Carefully targeting anaesthesia using BIS monitoring between 50 and 60 facilitated patient recovery post-operatively. In the non BIS-guided group, BIS levels were significantly lower during investigation time compared to BIS-guided group. This was associated with significantly prolonged extubation compared to BIS-guided group. In the post-operative interview, none of the patients reported an episode of intra-operative awareness. This result can be compared to Akcali et al. and Johansen et al., who reported faster waking-up and recovery in BIS-guided group, with no cases of awareness intra-operatively [6, 12].
In our study, at intubation BIS levels were between 50 and 60 in the BIS-guided group, compared to lower BIS levels in the non BIS-guided group, but without a significant difference. Also, we did not find any significant difference in heart rate and blood pressure levels, as a response to nociceptive stimuli during intubation and during the whole investigation time.
Although, there are studies reporting decreased drug consumption, such as Song et al. and Liu et al. [13, 14], we did not find any significant difference in analgesic consumption and anaesthetic gas delivery, probably because of inhalational anaesthesia with sevoflurane, mainly used intra-operatively, and which decreased towards the end of the operation. Our results can be compared to Lindholm et al. and Pavlin et al., who also reported no impact on drug dosing and gas delivery using BIS, with fentanyl and sevoflurane anaesthesia [15, 16].
Limitations of the study were the small number of participants due to the financial cost of sensors needed for investigations. Our study tested the effectiveness of BIS monitoring in a restricted study population; ASA II and ASA III, elective major abdominal surgery patients. We believe that the design of the study (randomised clinical trial) provides strength and quality. Most of the recent investigations in this field have investigated the effect of BIS monitoring on recovery times in ASA I and ASA II patients, predominantly in children and morbidly obese patients during one day surgery. Also, there have been a few studies where BIS monitoring is used to compare the effect of two different anaesthetics on recovery times and analgesic consumption. These investigations are also conducted on small number of participants. A retrospective investigation by Punjasawadwong et al. included 20 studies with 4056 participants. In general, BIS-guided anaesthesia within the recommended range (40 to 60) reduced the requirement for propofol and volatile anaesthetics, and shortened the duration of post-anaesthesia care unit stay. These trials were not completely comparable according to type of surgery, duration of surgery, drugs used intra-operatively and patients’ pre-operative status [18].
The results of our study might not apply to all patients undergoing relaxant general anaesthesia, especially to ASA IV and emergency patients. Further investigations will be needed at that point.
Finally, according to Klopman et al., titrating anaesthesia using BIS level will not only result in shorter waking-up time, but also shorter stays in the ICU, possible fulfilled criteria to by-pass ICU, and reduced drug costs [17].
In conclusion, guiding anaesthesia according to BIS level will result in significantly shorter extubation time, without episodes of intra-operative awareness. In clinical practice, this should represent a benefit for the individual patient, avoiding prolonged intubation and ventilation in the ICU. This could reduce costs of prolonged ventilation, treatment of complications arising from it, and shorter stays in the ICU. It also represents a benefit for the surgical programme, in the trace of fast track surgery, saving the time and the costs of surgical treatment.
1 Kotsovolis G, Komninos G. Awareness during anesthesia: how sure can we be that the patient is sleep indeed? Hippokratia. 2001;13(2):83–9.
2 Ghoneim MM. Awareness during anesthesia. Anesthesiology. 2000;92(2):597–602.
3 Tempe DK. In search of a reliable awareness monitor. Anesth Analg. 2001;92(4):801–4.
4 Monk T, Saini V, Weldon BC, Sigl JC. Anesthetic management and one-year mortality after noncardiac surgery. Anesth Analg. 2005;100(1):4–10.
5 Green D, Paklet L. Latest development in peri-operative monitoring of the high-risk major surgery patient. International Journal of Surgery. 2010;8(2):90–9.
6 Akcali DT, Özköse Z, Yardim S. Do we need bispectral index monitoring during total intravenous anesthesia for lumbar discectomies? Turkish Neurosurgery. 2008;18(2):125–33.
7 Bonhomme V, Plourde G, Meuret P, Fiset P, Backman SB. Auditory steady-state response and bispectral index for assessing level of consciousness during propofol sedation and hypnosis. Anesth Analg. 2000;91(6):1398–403.
8 Burrow N, Bigat Z, Akyuz M, Demir S, Ertok E. Does using the bispectral index (BIS) during craniotomy affect the quality of recovery? J Neurosurg Anesthesiol. 2006;18(1):1–4.
9 Kissin I. Depth of anesthesia and bispectral index monitoring. Anesth Analg. 2000;90(5):1114–7.
10 Gan TJ, Glass PS, Windsor A, Payne F, Rosow C, Sebel P, et al. Bispectral index monitoring allows faster emergence and improved recovery from propofol, alfentanil, and nitrous oxide anesthesia. BIS Utility Study Group. Anesthesiology. 1997;87(4):808–15.
11 Pavlin DJ, Hong JY, Freund PR, Koerschgen ME, Bower JO, Bowdle TA. The effect of bispectral index monitoring on end-tidal gas concentration and recovery duration after outpatient anesthesia. Anesth Analg. 2001;93(3):613–9.
12 Johansen JW, Sebel PS, Sigl JC. Clinical impact of hypnotic-titration guidelines based on EEG bispectral index (BIS) monitoring during routine anesthetic care. J Clin Anesth. 2000;12(6):433–43.
13 Song D, Joshi GP, White PF. Titration of volatile anesthetics using bispectral index facilitates recovery after ambulatory anesthesia. Anesthesiology. 1997;87(4):842–8.
14 Liu SS. Effects of bispectral index monitoring on ambulatory anesthesia: a meta-analysis of randomized controlled trials and a cost analysis. Anesthesiology. 2004;101(2):311–5.
15 Lindholm ML, Brudin L, Sandin RH. Bispectral index monitoring: appreciated but does not affect drug dosing and hypnotic levels. Acta Anaesthesiol Scand. 2008;52(1):88–94.
16 Pavlin JD, Souter KJ, Hong JY, Freund PR, Bowdle TA, Bower JO. Effects of bispectral index monitoring on recovery from surgical anesthesia in 1,580 inpatients from an academic medical center. Anesthesiology. 2005;102(3):566–73.
17 Klopman MA, Sebel PS. Cost-effectiveness of bispectral index monitoring. Curr Opin Anesthesiol. 2011;24(2):177–81.
18 Punjasawadwong Y, Boonjeungmonkol N, Phongchiewboon A. Bispectral index for improving anaesthetic delivery and postoperative recovery. Cochrane Database Syst Rev. 2007;(4):CD003843.
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article were reported.