Prognosis and quality of life of elderly patients after intensive care
DOI: https://doi.org/10.4414/smw.2012.13671
Marco
Conti, Paolo
Merlani, Bara
Ricou
Summary
Ageing of the world’s population raises important questions about the utilisation of the health care system. It is not clear how much should be invested in the last years of life whereas the costs are known to increase in parallel. Since intensive care units (ICU) are costly with highly specialised personnel, it seems of paramount importance that they would be used efficiently. Indeed, in the present context of predicted shortage of physicians in Switzerland, society and politics will need evidence that the care provided by ICUs is appropriate. There is no explicit limitation of care in any country according to age and nonagerians are admitted nowadays into ICUs with critical illness.
This review article will address the question of elderly patients in ICU and their outcome. Outcome does not imply surviving ICU but only later during the hospital stay and after discharge. Furthermore, we emphasise the need of examining not solely the hospital survival but the quality of life of the patients when they return to their real life. The fundamental questions are actually “Do they go back to life?” “What is life for elderly people?” These questions lead to more basic questions such as “Are they able to go back home or are they institutionalised? How is their quality of life and functional status after ICU?”.
We tried to address these questions through the existing literature and our experience while caring for these particular patients. Some clues on the prognostic factors related to their outcome are reported.
Introduction
In parallel with the ageing of the general population throughout the world, more old patients are admitted to the intensive care unit (ICU). In Switzerland too, this trend is remarkable and raises a number of questions regarding the organisation and adequacy of the health care system, the judicious distribution of resources in particular. Indeed, ICU is costly not only because of the high technology involved but also because of the staffing by highly specialised personnel including nurse-assistants, nurses and physicians.
The increasing number of elderly patients admitted to ICU with multiple comorbidities and complex clinical situations is at the centre of debate since the appropriateness of care for these patients might be questionable. Caregivers are sensitive to the appropriateness of the care they are providing [1] and a lack of sensitivity in this care may contribute to the degradation of motivation and eventually to burnout [2]. In parallel, the caregivers working in the stressful environment of ICUs are particularly at risk of developing burnout. Recent Swiss publication reports a rate of burnout up to 32% for physicians, 20% for nurses and as much as 41% for the nurse-assistants [3]. This might become a major problem in the near future, since burnt out caregivers leave ICU for less demanding jobs, whereas the shortage of ICU caregivers has already started. It is therefore of paramount importance that the prognosis and the outcome of elderly patients are better investigated. Such knowledge should allow first, a better allocation of resources, second, confirming or invalidating the appropriateness of care for ICU caregivers, and third, arousing a social and political reflection. Indeed, we should learn more about the outcome of these patients in order to answer the difficult question, whether the present health care system and current managerial rules are still adapted to the social needs.
This article will review the present state of knowledge about the specificities of elderly patients, especially regarding the pluralities and complexities of diseases with which they are admitted to ICUs, their prognosis and outcome.
We will try to approach the difficult question of the chronological or biological age and their potential implication in determining the outcome of elderly patients.
Definition of elderlies
The first classification of humans as “elderlies” likely came from the studies performed by the Belgian mathematician of the nineteenth century, Adolphe Quetelet, who described a progressive decrease of height and of viability starting between 50 and 60 years of age [4, 5].
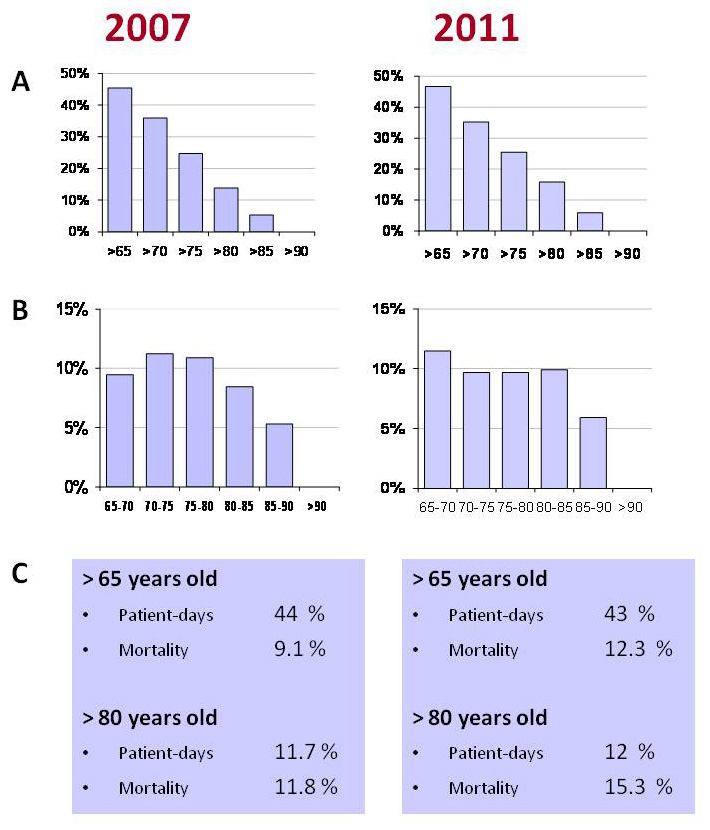
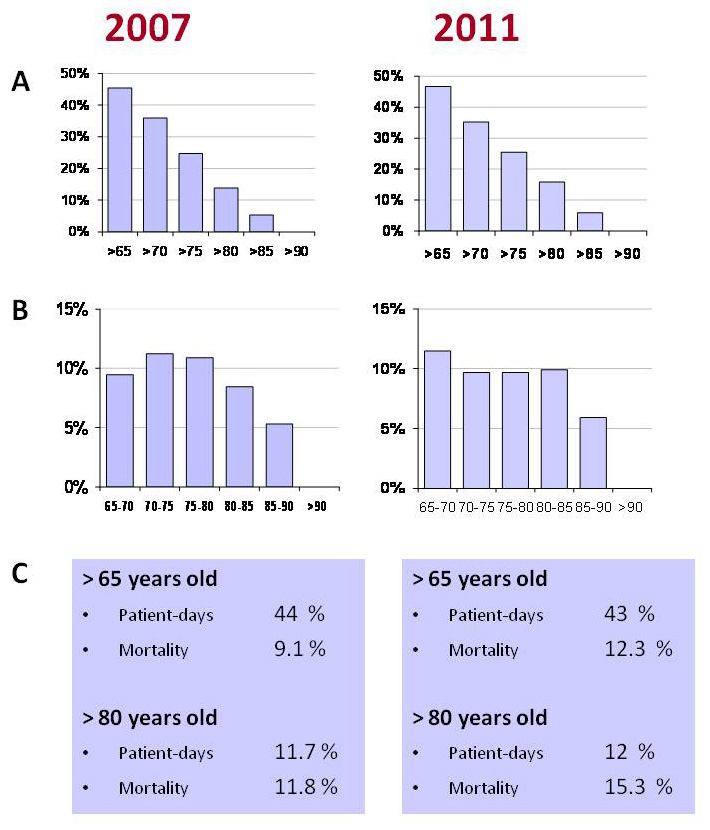
Figure 1
Evolution of the elderly population at Geneva ICU in 2007 compared to 2011.
A Percentages of patients of more than 65, 70, 75, 80, 85 and 90 years of age.
B Distribution by section of 5 years shows a trend towards more patients above 80 years in 2011.
C The consumption expressed as patients-days remains stable. The mortality remains stable, too.
These observations defined the elderly as individuals aged more than 65 years. Since this moment chronological age was considered as correlating with the degree of aging and the occurrence of chronic diseases.
Nowadays in the medical literature in general, and in the literature on critically ill patients specifically, elderly patients are defined as older than 65 years [6]. These patients are commonly categorised in 3 classes: “young old” or “young elderly”for patients between 65 and 70 or 75 years, “old-old”or “older elderly”for patients aged between 70 or 75 and 80 or 85 and “oldest-old” or “very elderly” for patients aged more than 80 or 85 years [6–9].
Although these terminologies are often used, we should emphasise that there are major inconsistencies in the use of the definition of elderly patient in critical care literature [6, 10]. This fact possibly originates from the limitations regarding the definition of chronological age. Indeed the chronological elderly definition is unreliable because of the inter-individual variability and the aging variability over time of the elderly. One of the alternative attempts to better define the elderly consists of a biological definition. However, at this time, there is no specific biomarker, list of comorbidities or prediction models that are able to assess with certainty the biological age of the elderly. Another alternative approach proposed is to analyse the “frailty” of the elderly in order to define old age. This concept may allow prediction of the vulnerability of the elderly in the near future, and seems promising in the current literature. However, up to now, there is no evidence that such definition will be adapted to and usable for critically ill patients [11].
Finally, because of the many difficulties of defining old age, the great majority of the current ICU literature relies on chronological age. Indeed, among 16 papers listed in a review article in 2005, 8 papers were using the threshold age of 65 years to define “elderly”, with the wide range of range 60 to 85 years [6].
Epidemiology
The SAPS (Simplified Acute Physiology Score) 3 study is a multinational multicentre study including more than 19,000 critically ill patients [12]. The proportion of patients aged more than 65 years was higher than 45%. In the United States and in Australia this proportion was even higher reaching respectively 56 and 50% with even 9.2% and 13% aged more than 80 years respectively [13, 14]. Furthermore, there is evidence that the percentage of the elderly is increasing, with the proportion of patients aged more than 80, 85 and 90 years increasing by every year by 5.6, 18.5 and 6.6% respectively [14].
In Geneva ICU, the total number of patients above 65 years of age did not change through the last 5 years. However, the proportion of the elderly more than 80 years tends to increase whereas their patient-days reflecting the consumption of resources remain stable (fig. 1: Geneva local data 2007–2011).
The good news is that the mortality of elderly patients in our unit does not increase significantly, as suggested in previous papers [15, 16]. However this does not mean that we are providing better care for them. The mortality depends on many factors as presented in the next chapters.
Moreover, the management of such patients in terms of treatment intensity seems to increase in comparison with treatment limitations in the past [15, 16].
Resource utilisation
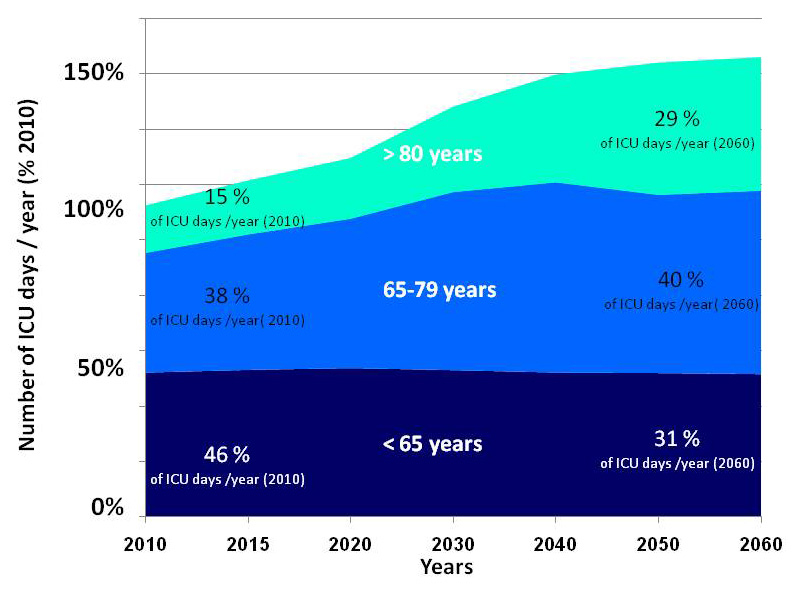
Resource utilisation for critically ill elderly patients is very important and progressively increasing. The COMPACCS (Committee On Manpower for Pulmonary and Critical Care Societies) study showed that 56% of ICU-days were used for patients over 65 years [17, 18]. Indeed the number of ICU days needed per year for 1,000 persons in a community varies enormously depending on their age (37 days for <65 years, 178 days for 65–74 years, 245 for 75–84 years and 231 for >85 years) [18]. Combining these data with the anticipated evolution of the Swiss population, we can infer the absolute and relative evolution of the resource-utilisation, related to increasing age (fig. 2) [19].
Despite the multiple morbidities of the elderly patients, the available data do not show a longer stay in ICUs compared with younger patients. Chronically critical ill patients, defined as patients staying more than three or more days in the ICU, represent a significant expenditure of ICU resources [20]. Although specific data regarding chronically critical ill elderly patients are rare, the mortality as well as the length of stay do not seem to differ when compared to younger population [21–23]. However, these data need to be read with caution, since there may be an important bias due to the triage of patients, and the attitudes regarding withholding and withdrawing therapies in elderly critically ill patients.
Mortality in ICU and after ICU
Some caution should be taken when looking at the mortality outcomes of elderly patients in ICU. Indeed the mortality rates depend on the case-mix involved and the time-point of assessment. The mortality during the ICU stay, during the hospital stay or after hospital discharge, at 1, 3, 6, 12 or 24 months or years later differ in causes and significance for the patient and the health care system. Most importantly, the mortality depends on the triage that occurred before admission into ICU. This is true for all cohorts of patients studied in ICUs, but particularly true for elderly patients for whom the indications for intensive care seem de facto tighter than for younger patients. Finally, withholding or withdrawing treatments became common practice in ICUs and it might well be that the attitude of clinicians may differ regarding elderly patients compared to younger patients. Such decisions may also impact heavily on the results of mortality of elderly patients. Finally, not all ICU can afford end-of-life care in the service itself depending on staffing and availability of beds. Therefore, the patients might be discharged to other places to die and the mortality is underestimated. The integration of these limitations might help understanding the diverse mortalities reported concerning elderly critically ill patients. Table 1 shows an overview on the mortalities of elderly patients in and after ICU published up to now.
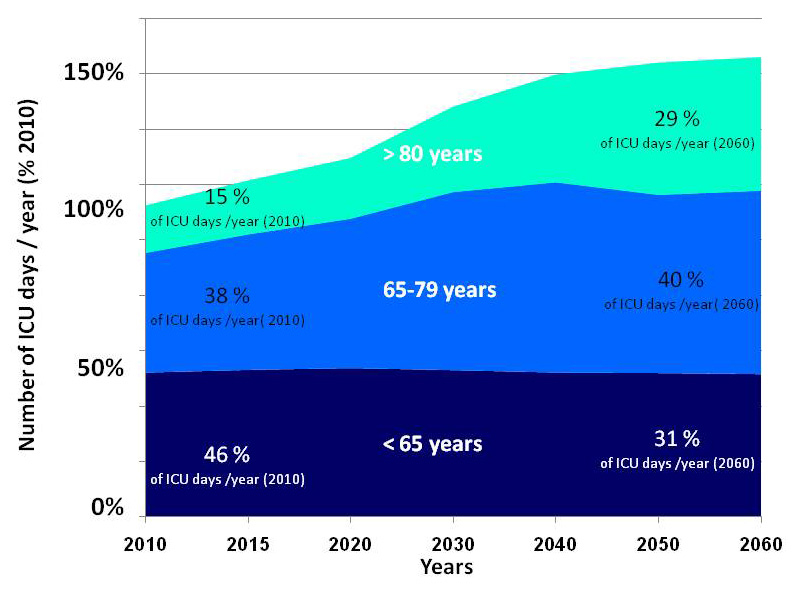
Figure 2
Evolution of the resource consumption (ICU days) in Switzerland over the next 50 years, depending on the age categories. The figure shows the evolution of the total number of ICU patient-days (expressed as the percentage of the resource consumption of 2010) needed per year from 2010 to 2060 for younger patients (aged less than 65 years), for the elderly (65–79 years) and for very elderly (>80 years) ICU patients (source of data: Bundesamt für Statistik [19]).
Compared with younger ICU patients, the elderly show a higher crude mortality. However, if the mortality is adjusted for the severity of the diseases, matched by comorbidities and adjusted for treatment, the differences almost disappear [24]. A residual “age effect” may however persist as shown by the SUPPORT study (Study to Understand Prognoses and Preferences for Outcome and Risks of Treatments) performed almost 20 years ago, that showed a linear effect of age on mortality with an inflection of the slope of the mortality at around 70 years [24]. Most recent studies report a similar effect with a delayed inflection point between 80 and 85 years [15].
We should underline that the mortality is increased compared to the age matched population, not only during the ICU stay but many months after discharge. This over-mortality seems to be maximal in the first 3 months after ICU discharge and may persist for almost 2 years and maybe even up to 15 years after ICU discharge [25, 26].
|
Table 1: Mortality of critically ill elderly patients in the literature. |
|
References
|
Age categories
(years)
|
Included patients
(n)
|
ICU mortality
(%)
|
Hospital mortality
(%)
|
Long-term mortality (%)
(follow-up in years)
|
| Campion et al., 1981 [67] |
55–64
65–74
≥75 |
648
624
560 |
5.1
7.9
10.2 |
8.3
13.5
16.3 |
21.8 (1)
32.9 (1)
43.4 (1) |
| Mahul et al., 1991 [68] |
70–79
≥80 |
226
69 |
25.7
30.4 |
|
56.2 (1)
34.9 (1) |
| Chelluri et al., 1992 [7] |
≥85 |
34 |
26.0 |
38.0 |
52.4 (1.5 ± 1) |
| Kass et al., 1992 [69] |
>85 |
105 |
29.5 |
|
64 (1) |
| Chelluri et al., 1993 [35] |
65–74
≥75 |
43
54 |
21.0
31.0 |
40.0
39.0 |
58.0 (1)
63.0 (1) |
| Rockwood et al., 1993 [70] |
<65
≥65 |
478
406 |
12.9
16 |
|
31 (1)
49 (1) |
| Djaiani et al., 1997 [8] |
70–74
75–79
80–84
≥85 |
193
128
109
44 |
|
|
45.6 (1)
42.2 (1)
42.3 (1)
72.7 (1) |
| Montuclard et al., 2000 [22] |
>70 |
75 |
33 |
53 |
|
| Rosenthal et al., 2002 [13] |
<65
65–69
70–74
75–79
80–84
85–89
≥90 |
67,890
19,876
22,607
20,602
14,386
7,511
3,264 |
|
8.5
15.0
15.9
17.1
19.0
21.1
24.1 |
|
| Somme et al., 2003 [25] |
<80
80–84
≥85 |
184
137
91 |
20
25
31 |
|
46 (0.25)
44 (0.25)
49 (0.25) |
| Bo et al., 2003 [71] |
>65 |
659 |
7.7 |
14.7 |
|
| Boumendil et al., 2004 [72] |
<80
≥80 |
1,224
233 |
13.3
16.3 |
|
67 (2) |
| Boumendil et al., 2005 [59] |
65–79
≥80 |
3,175
3,175 |
14.4
17.1 |
21.8
28.0 |
|
| Demoule et al., 2005 [73] |
20–69
≥90 |
72
36 |
18
28 |
27
47 |
|
| Kaarlola et al., 2006 [9] |
<65
65–69
70–74
75–79
≥80 |
1,827
327
301
172
82 |
16.5
19.0
19.6
19.2
17.1 |
27.4
33.0
38.5
37.2
41.5 |
55 (3 for ≥65 years) |
| De Rooij et al., 2006 [74] |
≥80 |
578 |
21.6 |
31.7 |
40.8 (1) |
| Merlani et al., 2007 [36] |
≥70 |
141 |
21.0 |
32.6 |
63.1 (2) |
| Reinikainen et al., 2007 [60] |
0–39
40–59
60–69
70–74
75–79
≥80 |
12,207
23,454
16,865
10,788
9,022
7,025 |
4.4
7.6
8.6
10.2
11.2
12.5 |
5.9
12.7
16.6
20.3
24.1
28.4 |
|
| Bagshaw et al., 2009 [14] |
18–39
40–64
65–79
≥80 |
16,732
42,285
45,466
15,640 |
5.6
7.6
9.8
12.0 |
7.1
11.4
16.6
24.0 |
|
| Sacanella et al., 2009 [75] |
65–74
≥75 |
230 |
|
27
33 |
|
| Tabah et al., 2010 [38] |
≥80 |
106 |
37.7 |
45.2 |
68.9 (1) |
| Sprung et al., 2012 [55] |
18–44
45–64
65–74
75–84
≥85 |
1,327
1,714
1,305
1,068
188 |
|
10.2*
21.2*
27.9*
35.5*
41.5* |
|
| * Mortality assessed at 28 days. Data on mortality are cumulative |
Prognostic factors
A number of risk factors were identified as associated with the mortality of critically ill elderly patients [10, 27]. Regarding the early mortality, during ICU and hospital stay, the most relevant factors pertain to the severity of the acute affection assessed by severity scores such as the APACHE score (“Acute Physiology and Chronic Health Evaluation”) or the SAPS score (that also include elements accounting for some comorbidities and the type of admission), or to the number of the organ failures [26, 28, 29]. Very advanced age (“Oldest Old”) represents only a minor risk factor for early mortality. The most relevant factors impacting on later mortality, at six months, one year or more after ICU, are the number and the type of comorbidities, the functional status and the quality of life before or just after the ICU stay.
A systematic review concerning the prognostication of the mortality of elderly ICU patients highlighted that there are only seven studies of a sufficient quality on the subject. The paper showed that there is no acceptable, credible or clinically useful model able to predict the mortality in the elderly [30]. A number of studies tried to identify the risk factors of mortality for a number of specific ICU diseases with variable success. The description of these detailed factors is beyond the scope of this review.
Outcomes after ICU
Health-related quality of life and functional status
The health-related quality of life (HrQOL) is mainly based on the World Health Organization’s definition of health: “Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity” [31]. As a consequence, HrQOL is a subjective concept that depends on individual’s perceptions concerning multiple dimensions as physical health (strength, energy), psychological state (good or bad feelings), level of independence (mobility), social relationships (social network, helps’ requirements), life environment (access to care), or personal beliefs (meaning of life) [32]. Therefore, its assessment is complex and highly dependent on individual's socio-cultural and religious context. At equivalent state of disease or infirmities, two patients can perceive a very different HrQOL. The functional status (FS) is a specific domain related to the physical component of HrQOL, frequently referred to the ability to perform the daily activities. It can be measured objectively or assessed subjectively from individuals.
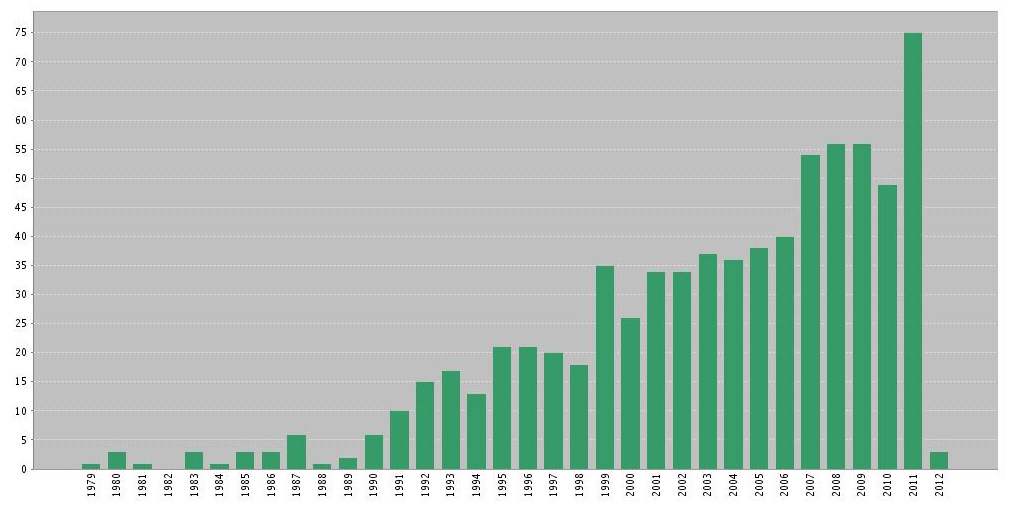
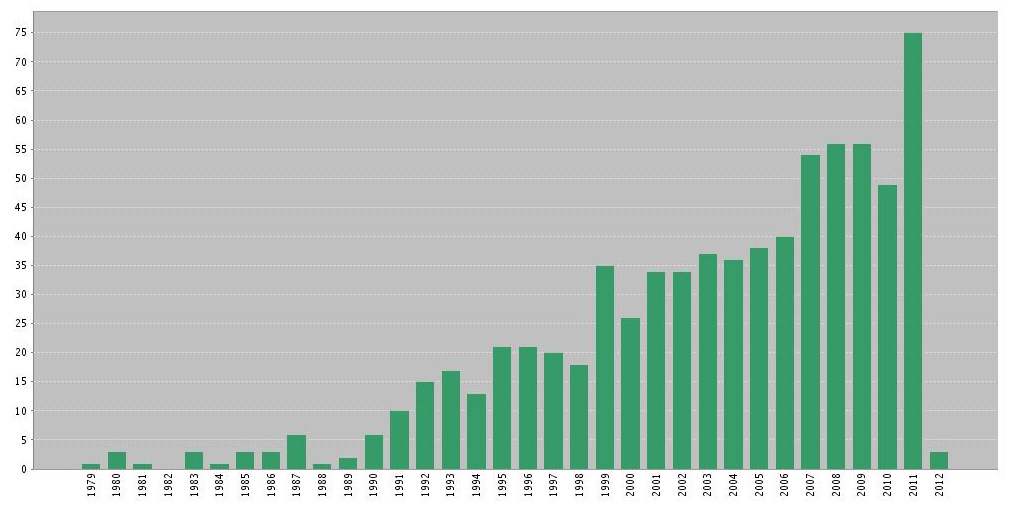
Figure 3
Referenced publications on ICU elderly patients’ outcomes. Data extracted from ISI Web of science, Web of Knowledge (2012). Key words: (“intensive care” OR “critical care” OR “icu”) AND elderly AND outcome. Results: 1,048 references
A good patient-centred management should ensure that any medical or surgical treatment and its intensity would be proposed keeping in mind the patients’ expectations in terms of the desired health state or HrQOL as previously defined. Therefore, physicians should ask themselves whether these outcomes could be reasonably met, especially when treatments are expensive and/or limited, and certainly even more when elderly patients are concerned. In this context, the assessment of HrQOL or its variation could be viewed as the measurement of treatments’ utility (or futility). It could be also used to justify the sufferings endured during a treatment or the attribution of a limited resource to patients, their families or to society.
There are numerous tools for the assessment of HrQOL or FS that are extensively presented in the review article of Hayes and collaborators [33].
For 30 years, the interest for elderly ICU patients’ outcomes has progressively increased as attested by the number of publications (fig. 3).
The elderly patients deteriorates during their ICU stay, improves after hospital discharge but fails to return to the pre-admission level even after a very long follow-up [6]. When HrQOL is considered, the elderly present worse results in most domains, especially in the physical dimensions when compared with age matched general population or younger ICU survivors [34]. Nonetheless, their HrQOL perception is fair or good and actually is similar to general population and even better than their younger counterparts [9, 22, 35–38]. This discrepancy between perceived functions and feeling of welfare is possibly related to a best acceptation of limitations with aging and a better coping capacity compared to younger patients [39].
Surprisingly, the dynamic evolution of HrQOL and FS is characterised by an alteration of health that occurs as early as one month before the ICU admission [40]. This suggests that patients were already on a declining slope and had a higher risk of developing an acute severe illness [6, 41].
These results are overall encouraging in the management of critically ill elderly patients. However, we need to draw the attention of the readers to the literature on the outcome of elderly patients, since they are burdened by a major bias that is difficult to quantify. Indeed, outcome measures require that the patients would survive their acute critical illness. Because ICU elderly patients have been highly selected during the triage process, we can easily imagine that those admitted could be the ones considered as good candidates and less fragile to benefit from an ICU care [42]. This can explain the spectacular results in the elderly’s HrQOL and FS assessment. Until now, too few large studies with good methodology have investigated these specific outcomes and these favourable conclusions should be taken with caution.
Home return after ICU
Home return (HR) is an important outcome on the point of view of elderly patients because it can be considered as a surrogate of a good FS allowing them to go back in their community setting. Indeed, factors associated with admission of geriatric patients into nursing homes are mainly a cognitive impairment and a high degree of dependency in daily activities [43]. After an acute disease and hospital admission, the same factors seem to prevail during the first months or years after discharge [44].
In the ICU setting, data about this outcome are scarce and found as annexed information in publications. In a review of 16 studies, 65 to 93% of ICU survivors were back home between 1 and 24 months after their stay [33]. If we look specifically at this outcome for elderly patients (65 years and over), we find only ten studies giving complete data about included patients (table 2). These studies were all performed in Western countries where nursing home admission rates are relatively similar (5 to 8% of elderly people) [45, 46]. Most survivors are discharged directly from hospital to their home. This proportion increases with time reaching 65 to 100% depending on age category and length of follow up. To note, the data should be read considering the differences of definitions of elderly patients, the case-mix, the length of follow up and definitions of HR. Indeed some studies considered transient admission in a rehabilitation structure as a non-HR. This can explain why some results improve during longer follow up. The HR rate is significantly diminished with increasing age but does not differ much from younger patients’ results [14].
Interestingly, the cumulative mortality (table 1) is very close to the rate of non-HR, especially at long term follow up. It seems that elderly ICU survivors have a dichotomic outcome when evaluated on the long term: dead or alive at home. Evidently, there are major selection biases regarding these results, as mentioned early regarding the mortality of elderly patients. Only three studies were conducted with this specific outcome as the objective. Nierman et al. built a model to predict the discharge location from hospital with a too small cohort of patients aged 85 years and over [47]. Gehlbach et al. have shown that old age (over 65 years) and poor strength or mobility at ICU admission are associated with a risk of non-HR after hospital discharge [48]. Finally, to our knowledge, only our group investigated factors influencing the HR probability in a pilot study [49]. We showed that the increasing age category of more than 85 years, the severity of acute illness, the presence of chronic heart failure or neoplasia, admission for trauma or neurologic trouble, and the length of hospital stay before ICU admission were associated with higher risk of non-HR.
These preliminary data should encourage the intensive care research community to develop more elaborate investigations for this paramount outcome for the elderly, their families and health care costs in the future.
|
Table 2: Home return and cumulative mortality after an ICU stay. |
|
References
|
Age categories (years)
|
Included patients
|
Cumulative mortality (%)
|
After hospital discharge to home (% of included patients)
|
After hospital discharge to home (% of survivors)
|
HR at follow up among included patients
|
HR at follow up among survivors
|
|
ICU
|
Hospital
|
Follow up
|
(%)
|
Follow up (month)
|
(%)
|
Follow up (months)
|
| Campion et al., 1981 [67] |
55–64
65–74
≥75 |
648
624
560 |
5.1
7.9
10.2 |
8.3
13.5
16.3 |
21.8
32.9
43.4 |
81.3
72
60.7 |
92
87
77 |
70.2
63.9
61.3 |
12
12
12 |
97
94
89 |
12
12
12 |
| Mahul et al., 1991 [68] |
>70 |
295 |
26.8 |
nc |
47.7 |
nc |
nc |
27.8
38.0
29.8 |
1
6
12 |
56
91
88 |
1
6
12 |
| Chelluri et al., 1992 [7] |
≥85 |
34 |
26.5 |
38.2 |
70.6 |
38.2 |
62 |
23.5 |
18 ± 10 |
80 |
18 ± 10 |
| Chelluri et al., 1993 [35] |
65–74
≥75 |
43
54 |
21.0
31.0 |
40.0
39.0 |
58.0
63.0 |
37.2
24.1 |
62
40 |
41.9
29.6 |
12
12 |
100
80 |
12
12 |
| Nierman et al., 2001 [47] |
≥85 |
455 |
nc |
24.6 |
nc |
51.4 |
68 |
nc |
nc |
nc |
nc |
| Rady et al., 2004 [76] |
<80
≥80 |
5,254
900 |
nc
nc |
5.9
9.6 |
18.7
30.0 |
75.4
55.4 |
80.1
61.3 |
66.9
45.8 |
0–42
0–42 |
82.3
65.4 |
0–42
0–42 |
| Merlani et al., 2007 [36] |
≥70 |
141 |
20.6 |
32.6 |
63.1 |
nc |
nc |
29.8 |
24 |
80.8 |
24 |
| Bagshaw et al., 2009 [14] |
18–39
40–64
65–79
≥80 |
16,732
42,285
45,466
15,640 |
5.6
7.6
9.8
12.0 |
7.1
11.4
16.6
24.0 |
nc
nc
nc
nc |
78.9
76.2
69.3
54.9 |
84.9
86.0
83.1
72.2 |
nc |
nc |
nc |
nc |
| Gehlbach et al., 2011 [48] |
<65
≥65 |
372*
176* |
nc |
nc |
nc |
nc |
79.6
61.9 |
nc |
nc |
nc |
nc |
| Conti et al., 2011 [49] |
≥65 |
526 |
8 |
18 |
22 |
nc |
nc |
72 |
6 |
93 |
6 |
| ICU = intensive care unit; HR = home return; nc = non communicated.
* Data concern only hospital survivors.
Lost to follow up patients have been considered as dead or not at home. |
Treatment intensity and preferences
Ethical and legal aspects
Throughout each step of the patients’ hospital journey, physicians are facing the fundamental question of the amount of care that the specific elderly patient should benefit from. The physicians have to consider some ethical and legal aspects when proposing therapeutics to patients, especially to the elderly. They have the complex task of matching patients’ preferences for treatment options without forgetting social interests, including considerations about resource allocation. The key steps in doing so include the triage process for ICU admission, the legitimacy of pursuing treatment in ICUs and the length of ICU stay before the transfer to normal ward. The Swiss Academy of Medical Sciences stated that in this context the chronological age is not the only criterion for the decision process and that the ethical principles should be applied to elderly patients as well for younger patients. Some specific questions addressed in these directives deserve comments. The elderly patients, even the oldest old, should be considered as competent and having their capacity to make decisions for themselves; therefore, the principle of autonomy should be respected and the decision making should include their opinion. Families’ opinion cannot and should not overwhelm patient’s own wish. This is an important point to emphasise before the introduction of the new civil law (Swiss Civil Code) in Switzerland, planned for January 2013, that will give greater decision power to family members as surrogate decision makers [50]. The beneficence and non-maleficence principles should be applied considering the specific outcomes of elderly patients and the expected duration of life of which they may benefit. The principle of justice requires that for each single case, the benefit and burden of care would be cautiously balanced in order to achieve the best decision. In doing so, the physicians need to remain conscious of the cost of care; according to the principle of justice, they have the responsibility and should have the courage to renounce treatments that are unreasonable or unable to achieve the expected results. This recommendation reminds us that an opposite attitude could be considered as ageism.
Besides these rules, convictions, socio-cultural context, beliefs and life history can influence treatment decisions. This can be a source of conflicts within the ICU team especially in difficult situations as when withholding or withdrawing sustaining treatments [51]. As mentioned in the introduction, the lack of appropriateness felt by the ICU health care professionals as well as the conflicts can eventually lead the team to burnout. ICU heads should be aware of such consequences when approaching the question of elderly patients in ICU.
Treatment intensity
There are no validated and widely accepted criteria for ICU elderly patients’ admissions. During the triage process, decisions are mainly based on physicians’ empiric experiences. Patients’ characteristics unrelated to clinical pathologies can be unconsciously considered in these situations, as for example the personality traits [52]. Chronological age negatively influences the admission probability [42]. However, even though age is still an important factor, its weight on admission decision has progressively decreased during the last decade [53–55].
When the response to maximal treatment is not sufficient and survival chances with satisfactory conditions are almost non-existent, decision of therapeutic limitations is often applied. These withhold or withdrawal situations concern as many as 10% of ICU patients [56]. Old age is a recognised factor associated with such decisions [21, 57–61]. As for admission criteria, weight of this latter factor has evolved during last decade and observational studies have shown that survival of ICU elderly patients (at equal acute illness severity) has improved without prolonging the length of stay [15].
Elderly patients’ preferences
Informed consent is the mainstay of self-determination. Murphy et al. have shown that elderly patients’ preference for cardiopulmonary resuscitation decreases from 41 to 22% after extensive information about procedure and prognosis [62]. It has been shown that the prognosis of acute disease, treatment’s burden and functional or cognitive impairment probability are factors influencing elderly patients’ preferences [63]. These findings are in line with the study of Mattimore et al. showing that 77% of interviewed patients were unwilling to live in a nursing home and among them 30% would rather die [64].
During a severe acute illness, patients are often unable to express their wishes. In these situations, caregivers have to extrapolate these preferences, basing their decisions on information provided by relatives. Hamel et al. have shown that physicians are wrong in their predictions in 55% of cases [58]. These mistakes are more frequent when patients are aged. For example, 79% of caregivers mistakenly think that patients over 80 years don’t wish an intensive treatment compared to only 36% when the age is below 50. In a study of elderly outpatients, the prediction of preferences of patients by family surrogates, primary care physicians and hospital-based physicians were accurate only at 74, 66 and 64% respectively with the own preferences of the patients [65]. The adjunct of advance directives should improve predictions of hospital-based physicians.
Finally, it is interesting to know that whatever the age, patients who survive mostly have a good perception of their ICU stay and 70% of them would agree with a new admission and mechanical ventilation [66].
Conclusions
The aging of the population and the complex clinical presentation of these particular patients confront the health care system with new challenges. The availability of intensive care medicine is not preserved from these preocca patients, and patients of more than 90 years old are often admitted into ICU. On the other hand, the number of ICU beds is limited and concerns about their availability for any patient are emerging. The available literature regarding the outcomes of elderly patients is exploding in numbers and should help health care providers and leaders to make decisions. However, these papers are difficult to understand because the populations studied differed in ages, and depended on the objectives of care that were chosen, whereas there is no social or political agreement on the most acceptable objective to achieve optimal health care for aging patients. Is it the discharge from ICU, the discharge from hospital, the quality of life, the ability for everyday activities or the possibility to return home, or have we still to discover the “holy grail” of “ the outcome” that should be considered the goal.
Another difficulty are the discrepancies between the chronological age, the biological age and the capacity of the elderly patients to recover. An interesting concept in this regard is the frailty that is a more holistic approach of the patients. However, data integrating this concept for assessing the outcome of elderly patients are missing for now.
Despite the lack of explicit indications and contraindications for ICU admission of elderly patients, there is a strong evidence that triage has already been applied. The ethical principles allowing the assessment of values at stake are of paramount importance in this matter. However, many factors other than pure ethical considerations are known to be implicitly involved in the decision-making process, and more objective criteria may help health care providers to find a more equitable distribution of health resources, including intensive care.
References
1 Piers RD, Azoulay E, Ricou B, Dekeyser Ganz F, Decruyenaere J, Max A, et al. Perceptions of appropriateness of care among European and Israeli intensive care unit nurses and physicians. JAMA. 2011;306(24):2694–703.
2 Halpern SD. Perceived inappropriateness of care in the ICU: what to make of the clinician’s perspective? JAMA. [Comment Editorial Research Support, Non-U.S. Gov’t Research Support, U.S. Gov’t, P.H.S.]. 2011;306(24):2725–6.
3 Merlani P, Verdon M, Businger A, Domenighetti G, Pargger H, Ricou B. Burnout in ICU caregivers: a multicenter study of factors associated to centers. Am J Respir Crit Care Med. 2011;184(10):1140–6.
4 Quetelet A. Sur l’Homme et le développement de ses Facultés. Bruxelles: L. Hauman; 1836.
5 Kirk H. Geriatric medicine and the categorisation of old age; the historical linkage. Ageing & Society. 1992;12(04):483–97.
6 Hennessy D, Juzwishin K, Yergens D, Noseworthy T, Doig C. Outcomes of elderly survivors of intensive care: a review of the literature. Chest. 2005;127(5):1764–74.
7 Chelluri L, Pinsky MR, Grenvik AN. Outcome of intensive care of the “oldest-old” critically ill patients. Crit Care Med. 1992;20(6):757–61.
8 Djaiani G, Ridley S. Outcome of intensive care in the elderly. Anaesthesia. 1997;52(12):1130–6.
9 Kaarlola A, Tallgren M, Pettila V. Long-term survival, quality of life, and quality-adjusted life-years among critically ill elderly patients. Crit Care Med. 2006;34(8):2120–6.
10 Conti M, Merlani P, Eckert P. Patient âgé aux soins intensifs. Rev Med suisse. 2009;5(229):2494–8.
11 Ricou B, Merlani P. What limits for acute care in the elderly? Curr Opin Anaesthesiol. 2008;21(3):380–5.
12 Metnitz PG, Moreno RP, Almeida E, Jordan B, Bauer P, Campos RA, et al. SAPS 3 – from evaluation of the patient to evaluation of the intensive care unit. Part 1: objectives, methods and cohort description. Intensive Care Med. 2005;31(10):1336–44.
13 Rosenthal GE, Kaboli PJ, Barnett MJ, Sirio CA. Age and the risk of in-hospital death: insights from a multihospital study of intensive care patients. J Am Geriatr Soc. 2002;50(7):1205–12.
14 Bagshaw SM, Webb SA, Delaney A, George C, Pilcher D, Hart GK, et al. Very old patients admitted to intensive care in Australia and New Zealand: a multi-centre cohort analysis. Crit Care. 2009;13(2):R45.
15 Lerolle N, Trinquart L, Bornstain C, Tadie JM, Imbert A, Diehl JL, et al. Increased intensity of treatment and decreased mortality in elderly patients in an intensive care unit over a decade*. Crit Care Med. 2009 Jul 23.
16 Ihra GC, Lehberger J, Hochrieser H, Bauer P, Schmutz R, Metnitz B, et al. Development of demographics and outcome of very old critically ill patients admitted to intensive care units. Intensive Care Med. 2012;38(4):620–6.
17 Angus DC, Kelley MA, Schmitz RJ, White A, Popovich J, Jr. Caring for the critically ill patient. Current and projected workforce requirements for care of the critically ill and patients with pulmonary disease: can we meet the requirements of an aging population? JAMA. 2000;284(21):2762–70.
18 Pronovost PJ, Waters H, Dorman T. Impact of critical care physician workforce for intensive care unit physician staffing. Curr Opin Crit Care. 2001;7(6):456–9.
19 Bundesamt für Statistik (BAFS). [Accessed 10th may 2012]; Available from: http://www.bfs.admin.ch/bfs/portal/de/index/themen/01/03/blank/key/ind_erw.html.
20 Merlani P, Conti M, Ricou B. After ICU. ICU Management. 2011;11(3):6–10.
21 Castillo-Lorente E, Rivera-Fernandez R, Vazquez-Mata G. Limitation of therapeutic activity in elderly critically ill patients. Project for the Epidemiological Analysis of Critical Care Patients. Crit Care Med. 1997;25(10):1643–8.
22 Montuclard L, Garrouste-Orgeas M, Timsit JF, Misset B, De Jonghe B, Carlet J. Outcome, functional autonomy, and quality of life of elderly patients with a long-term intensive care unit stay. Crit Care Med. 2000;28(10):3389–95.
23 Laupland KB, Kirkpatrick AW, Kortbeek JB, Zuege DJ. Long-term mortality outcome associated with prolonged admission to the ICU. Chest. 2006;129(4):954–9.
24 Hamel MB, Davis RB, Teno JM, Knaus WA, Lynn J, Harrell F, Jr., et al. Older age, aggressiveness of care, and survival for seriously ill, hospitalized adults. SUPPORT investigators. Study to understand prognoses and preferences for outcomes and risks of treatments. Ann Intern Med. 1999;131(10):721–8.
25 Somme D, Maillet JM, Gisselbrecht M, Novara A, Ract C, Fagon JY. Critically ill old and the oldest-old patients in intensive care: short- and long-term outcomes. Intensive Care Med. 2003;29(12):2137–43.
26 Williams TA, Dobb GJ, Finn JC, Webb SA. Long-term survival from intensive care: a review. Intensive Care Med. 2005;31(10):1306–15.
27 Boumendil A, Somme D, Garrouste-Orgeas M, Guidet B. Should elderly patients be admitted to the intensive care unit? Intensive Care Med. 2007;33(7):1252–62.
28 Knaus WA, Wagner DP, Draper EA, Zimmerman JE, Bergner M, Bastos PG, et al. The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest. 1991;100(6):1619–36.
29 Le Gall JR, Lemeshow S, Saulnier F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA. 1993;270(24):2957–63.
30 Minne L, Ludikhuize J, de Jonge E, de Rooij S, Abu-Hanna A. Prognostic models for predicting mortality in elderly ICU patients: a systematic review. Intensive Care Med. 2011;37(8):1258–68.
31 World Health Organization. Basic documents. 46th ed. Geneva: World Health Organization; 2007.
32 What quality of life? The WHOQOL Group. World Health Organization Quality of Life Assessment. World Health Forum. 1996;17(4):354–6.
33 Hayes JA, Black NA, Jenkinson C, Young JD, Rowan KM, Daly K, et al. Outcome measures for adult critical care: a systematic review. Health Technol Assess. 2000;4(24):1–111.
34 Oeyen SG, Vandijck DM, Benoit DD, Annemans L, Decruyenaere JM. Quality of life after intensive care: a systematic review of the literature. Crit Care Med. 2010;38(12):2386–400.
35 Chelluri L, Pinsky MR, Donahoe MP, Grenvik A. Long-term outcome of critically ill elderly patients requiring intensive care. JAMA. 1993;269(24):3119–23.
36 Merlani P, Chenaud C, Mariotti N, Ricou B. Long-term outcome of elderly patients requiring intensive care admission for abdominal pathologies: survival and quality of life. Acta Anaesthesiol Scand. 2007;51(5):530–7.
37 de Rooij SE, Govers AC, Korevaar JC, Giesbers AW, Levi M, de Jonge E. Cognitive, functional, and quality-of-life outcomes of patients aged 80 and older who survived at least 1 year after planned or unplanned surgery or medical intensive care treatment. J Am Geriatr Soc. 2008;56(5):816–22.
38 Tabah A, Philippart F, Timsit JF, Willems V, Francais A, Leplege A, et al. Quality of life in patients aged 80 or over after ICU discharge. Crit Care. 2010;14(1):R2.
39 Carstensen LL, Fung HH, Charles ST. Socioemotional selectivity theory and the regulation of emotion in the second half of life. Motiv Emotion. 2003;27(2):103–23.
40 Graf J, Koch M, Dujardin R, Kersten A, Janssens U. Health-related quality of life before, 1 month after, and 9 months after intensive care in medical cardiovascular and pulmonary patients. Crit Care Med. 2003;31(8):2163–9.
41 Dowdy DW, Eid MP, Sedrakyan A, Mendez-Tellez PA, Pronovost PJ, Herridge MS, et al. Quality of life in adult survivors of critical illness: a systematic review of the literature. Intensive Care Med. 2005;31(5):611–20.
42 Garrouste-Orgeas M, Montuclard L, Timsit JF, Misset B, Christias M, Carlet J. Triaging patients to the ICU: a pilot study of factors influencing admission decisions and patient outcomes. Intensive Care Med. 2003;29(5):774–81.
43 Luppa M, Luck T, Weyerer S, Konig HH, Brahler E, Riedel-Heller SG. Prediction of institutionalization in the elderly. A systematic review. Age Ageing. 2010;39(1):31–8.
44 Campbell SE, Seymour DG, Primrose WR, Lynch JE, Dunstan E, Espallargues M, et al. A multi-centre European study of factors affecting the discharge destination of older people admitted to hospital: analysis of in-hospital data from the ACMEplus project. Age Ageing. 2005;34(5):467–75.
45 Ribbe MW, Ljunggren G, Steel K, Topinkova E, Hawes C, Ikegami N, et al. Nursing homes in 10 nations: a comparison between countries and settings. Age Ageing. [Comparative Study Research Support, Non-U.S. Gov’t]. 1997;26(Suppl 2):3–12.
46 Anderson GF, Hussey PS. Population aging: a comparison among industrialized countries. Health Aff (Millwood). Comparative Study. 2000;19(3):191–203.
47 Nierman DM, Schechter CB, Cannon LM, Meier DE. Outcome prediction model for very elderly critically ill patients. Crit Care Med. 2001;29(10):1853–9.
48 Gehlbach BK, Salamanca VR, Levitt JE, Sachs GA, Sweeney MK, Pohlman AS, et al. Patient-related factors associated with hospital discharge to a care facility after critical illness. Am J Crit Care. 2011;20(5):378–86.
49 Conti M, Friolet R, Eckert P, Merlani P. Home return 6 months after an intensive care unit admission for elderly patients. Acta Anaesthesiol Scand. 2011;55(4):387–93.
50 Code civil suisse (Protection de l’adulte, droit des personnes et droit de la filiation). Modification du 19 décembre 2008. Available from: http://www.admin.ch/ch/f/as/2011/725.pdf. Accessed 13th may 2012.
51 Azoulay E, Timsit JF, Sprung CL, Soares M, Rusinova K, Lafabrie A, et al. Prevalence and factors of intensive care unit conflicts: the conflicus study. Am J Respir Crit Care Med. 2009;180(9):853–60.
52 Escher M, Perneger TV, Chevrolet JC. National questionnaire survey on what influences doctors’ decisions about admission to intensive care. BMJ. 2004;329(7463):425.
53 Hubbard RE, Lyons RA, Woodhouse KW, Hillier SL, Wareham K, Ferguson B, et al. Absence of ageism in access to critical care: a cross-sectional study. Age Ageing. 2003;32(4):382–7.
54 Iapichino G, Corbella D, Minelli C, Mills GH, Artigas A, Edbooke DL, et al. Reasons for refusal of admission to intensive care and impact on mortality. Intensive Care Med. 2010;36(10):1772–9.
55 Sprung CL, Artigas A, Kesecioglu J, Pezzi A, Wiis J, Pirracchio R, et al. The Eldicus prospective, observational study of triage decision making in European intensive care units. Part II: Intensive care benefit for the elderly*. Crit Care Med. 2012;40(1):132–8.
56 Sprung CL, Cohen SL, Sjokvist P, Baras M, Bulow HH, Hovilehto S, et al. End-of-life practices in European intensive care units: the Ethicus Study. JAMA. 2003;290(6):790–7.
57 A controlled trial to improve care for seriously ill hospitalized patients. The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT). The SUPPORT Principal Investigators. JAMA. 1995;274(20):1591–8.
58 Hamel MB, Teno JM, Goldman L, Lynn J, Davis RB, Galanos AN, et al. Patient age and decisions to withhold life-sustaining treatments from seriously ill, hospitalized adults. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment. Ann Intern Med. 1999;130(2):116–25.
59 Boumendil A, Aegerter P, Guidet B. Treatment intensity and outcome of patients aged 80 and older in intensive care units: a multicenter matched-cohort study. J Am Geriatr Soc. 2005;53(1):88–93.
60 Reinikainen M, Uusaro A, Niskanen M, Ruokonen E. Intensive care of the elderly in Finland. Acta Anaesthesiol Scand. 2007;51(5):522–9.
61 Sprung CL, Woodcock T, Sjokvist P, Ricou B, Bulow HH, Lippert A, et al. Reasons, considerations, difficulties and documentation of end-of-life decisions in European intensive care units: the ETHICUS Study. Intensive Care Med. 2008;34(2):271–7.
62 Murphy DJ, Burrows D, Santilli S, Kemp AW, Tenner S, Kreling B, et al. The influence of the probability of survival on patients’ preferences regarding cardiopulmonary resuscitation. N Engl J Med. 1994;330(8):545–9.
63 Fried TR, Bradley EH, Towle VR, Allore H. Understanding the treatment preferences of seriously ill patients. N Engl J Med. 2002;346(14):1061–6.
64 Mattimore TJ, Wenger NS, Desbiens NA, Teno JM, Hamel MB, Liu H, et al. Surrogate and physician understanding of patients’ preferences for living permanently in a nursing home. J Am Geriatr Soc. 1997;45(7):818–24.
65 Coppola KM, Ditto PH, Danks JH, Smucker WD. Accuracy of primary care and hospital-based physicians’ predictions of elderly outpatients’ treatment preferences with and without advance directives. Arch Intern Med. 2001;161(3):431–40.
66 Mendelsohn AB, Chelluri L. Interviews with intensive care unit survivors: assessing post-intensive care quality of life and patients’ preferences regarding intensive care and mechanical ventilation. Crit Care Med. 2003;31(5 Suppl):S400–6.
67 Campion EW, Mulley AG, Goldstein RL, Barnett GO, Thibault GE. Medical intensive care for the elderly. A study of current use, costs, and outcomes. JAMA. 1981;246(18):2052–6.
68 Mahul P, Perrot D, Tempelhoff G, Gaussorgues P, Jospe R, Ducreux JC, et al. Short- and long-term prognosis, functional outcome following ICU for elderly. Intensive Care Med. 1991;17(1):7–10.
69 Kass JE, Castriotta RJ, Malakoff F. Intensive care unit outcome in the very elderly. Crit Care Med. 1992;20(12):1666–71.
70 Rockwood K, Noseworthy TW, Gibney RT, Konopad E, Shustack A, Stollery D, et al. One-year outcome of elderly and young patients admitted to intensive care units. Crit Care Med. 1993;21(5):687–91.
71 Bo M, Massaia M, Raspo S, Bosco F, Cena P, Molaschi M, et al. Predictive factors of in-hospital mortality in older patients admitted to a medical intensive care unit. J Am Geriatr Soc. 2003;51(4):529–33.
72 Boumendil A, Maury E, Reinhard I, Luquel L, Offenstadt G, Guidet B. Prognosis of patients aged 80 years and over admitted in medical intensive care unit. Intensive Care Med. 2004;30(4):647–54.
73 Demoule A, Cracco C, Lefort Y, Ray P, Derenne JP, Similowski T. Patients aged 90 years or older in the intensive care unit. J Gerontol A Biol Sci Med Sci. 2005;60(1):129–32.
74 de Rooij SE, Govers A, Korevaar JC, Abu-Hanna A, Levi M, de Jonge E. Short-term and long-term mortality in very elderly patients admitted to an intensive care unit. Intensive Care Med. 2006;32(7):1039–44.
75 Sacanella E, Perez-Castejon JM, Nicolas JM, Masanes F, Navarro M, Castro P, et al. Mortality in healthy elderly patients after ICU admission. Intensive Care Med. 2009;35(3):550–5.
76 Rady MY, Johnson DJ. Hospital discharge to care facility: a patient-centered outcome for the evaluation of intensive care for octogenarians. Chest. 2004;126(5):1583–91.