Figure 1
Time to recurrence.
DOI: https://doi.org/10.4414/smw.2012.13643
The paradigm shift in thyroid surgery away from Kocher’s principles of nodal enucleation or subtotal resection to extended thyroidectomy involving at least hemithyroidectomy (total unilateral lobectomy) is a well accepted approach for the treatment of multinodular goitre disease; it carries no increased risk of morbidity compared with subtotal resection [1–3].
The more radical approach of extended thyroid resection for benign multinodular disease is reasonable for preventing recurrent goitre [1]. Studies have already documented a significantly higher morbidity rate in redo-surgery after subtotal resection for recurrent disease compared with initial surgery [4, 5]. However, most studies do not precisely report the side, time and its side specific morbidity of reoperation after subtotal resection.
The aim of the present study was to evaluate morbidity rate in relation to the side of initial and redo-surgery for recurrent disease.
Between January 1997 and December 2010 a total of 1699 patients underwent consecutive thyroid gland surgery with 2782 nerves at risk at our tertiary institution with a special interest in endocrine surgery. As a tertiary institution and referral centre for a large region we had changed our policy towards extended resection, including at least a hemithyroidectomy (total lobectomy on one side) already in 1991. However, this move was only later performed by the surrounding institutions and surgeons. Therefore, this transition time in surgical practice, in our region from subtotal to total resection offered us (as a referral centre for redo-surgery) a unique opportunity to compare the recurrences after both types of initial surgery in regards to localisation and morbidity. Data of all patients undergoing thyroidectomy were prospectively collected and stored in an electronic database. A total of 118 patients (6.9%) underwent reoperation after subtotal resection. Of these, 109 patients with complete follow-up (including exact indication, date and extent of initial surgery) were included in the present study. The majority of initial operations on these patients were performed at an external clinic. The control group to compare morbidity rate of initial and redo-surgery consisted of 1590 patients. Overall loss of follow-up was <1%.
Patients undergoing reoperation were allocated into two groups. The ipsilateral group consists of patients with recurrent disease in the previously operated ipsilateral lobe. Patients with recurrent disease in both lobes were also allocated to the ipsilateral group. The contralateral group consists of patients with recurrent disease in the non-operated, contralateral lobe, only.
Our standard operation for strictly unilateral thyroid disease was ipsilateral hemithyroidectomy (total lobectomy on one side) including resection of the isthmus. A total thyroidectomy was performed in cases of cancer or when nodules were present in both thyroid lobes. In cases of cancer, lymphadenectomy was performed accordingly. A single preoperative dose of antibiotic prophylaxis was given. As a teaching hospital, operations were performed by residents following a strict protocol; however, a staff surgeon was present at all operations. Standardised visualisation of the recurrent laryngeal nerves, including routine laryngeal nerve monitoring, and the parathyroid glands was performed. Removed tissue was submitted for intraoperative frozen-section and fast track histological analyses in all cases.
Persistent recurrent laryngeal nerve palsy was defined as nerve palsy lasting more than 12 months after surgery. Vocal cord function was documented pre- and postoperatively by laryngoscopy in all patients. If postoperative recurrent laryngeal nerve palsy was observed, patients underwent phoniatric consultations and logotherapy and were followed for a minimum of one year by an otolaryngologist.
Persistent hypoparathyroidism was defined as hypocalcaemia lasting more than 12 months after surgery requiring treatment. Transplantation of parathyroid glands into the sternocleidomastoid muscle was performed if a parathyroid gland was intraoperatively devascularised. Patients’ general practitioners were contacted by phone one year after the operation if a prescription of vitamin D and calcium was given at discharge in order to rule out permanent hypoparathyreoidism.
The primary outcome parameter was persistent recurrent nerve palsy associated with redo-surgery for recurrent disease. Secondary outcome parameters were persistent hypoparathyreoidism, site and time of recurrence, and risk factors for contralateral recurrent disease.
Student’s t-test was performed to determine the significance between continuous variables, and Fisher’s exact test was used to compare proportions. Logistic regression analysis was performed to analyse risk factors for contralateral recurrence. P-values were two-sided and a value of <0.05 was used as the threshold for statistical significance (NCSS 2007 for Windows; NCSS, Kaysville, UT).
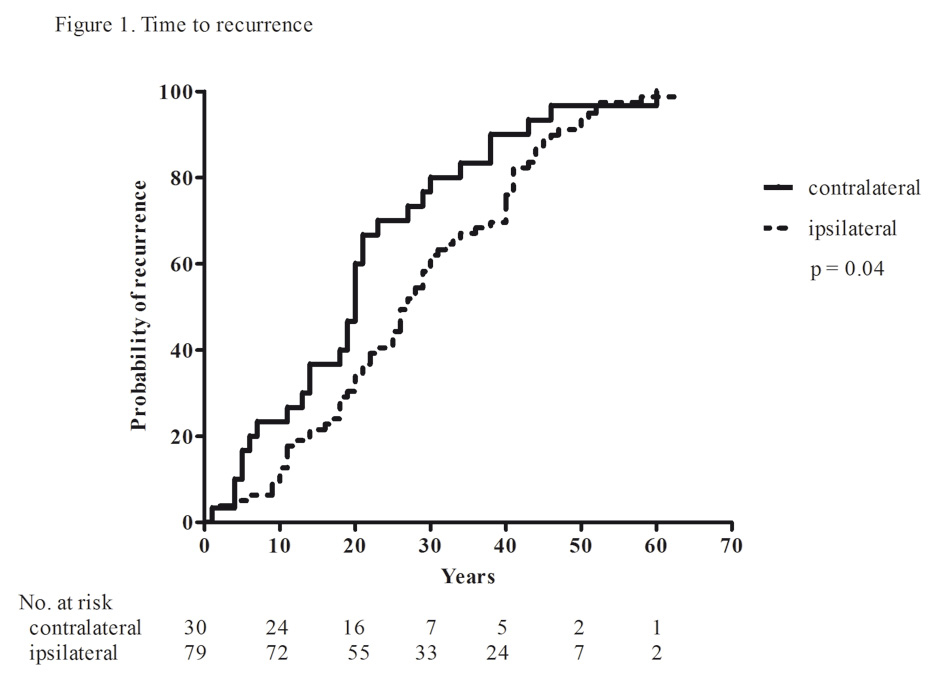
A total of 118 patients (6.9%) underwent reoperation. Recurrent disease was found in 79/109 patients (72.5%) in the ipsilateral lobe and in 30/109 patients (27.5%) in the contralateral lobe. Table 1 reports patients’ demographic parameters. Patients undergoing reoperation in the contralateral lobe were significantly younger at the time of redo-surgery (median 56 years (range 17–82) vs. 70 years (26–90); p <0.001) and median time to recurrence in the contralateral lobe was significantly shorter compared with patients undergoing ipsilateral reoperation (20 years (1-60) vs. 27 years (1-63); p = 0.03) (fig. 1). Preexisting recurrent laryngeal nerve palsy was observed in the contralateral group in 13.3% (4/30) and in the ipsilateral group in 5.1% (4/79) (p = 0. 21). Table 1 reports the extent of redo-surgery. Up to the year 2000, 13 patients in the ipsilateral group underwent hemithyroidectomy and subtotal contralateral resection due to patients’ rejections of hormone substitution.
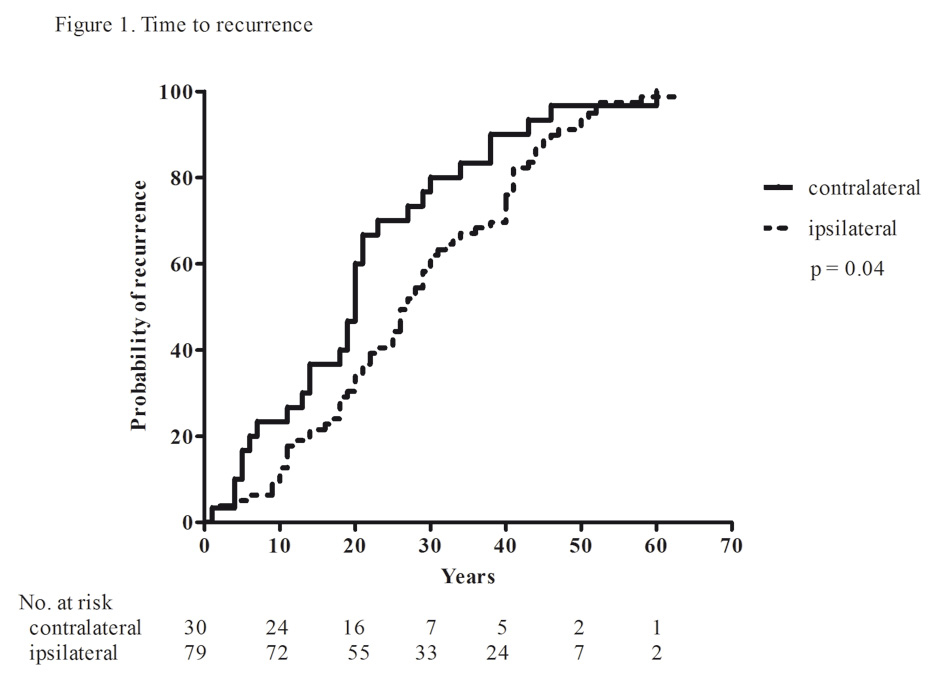
Figure 1
Time to recurrence.
Median age at initial operation was comparable between both groups (33 years (12-65) vs. 36 years (15-65); p = 0.07). Initial operation in the contralateral group was subtotal unilateral resection in 73.3% (22/30) and total unilateral resection in 26.6% (8/30). The initial operation in the ipsilateral group was a subtotal unilateral resection in 26.6% (21/79) and a subtotal bilateral resection in 73.4% (58/79).
The incidence of permanent recurrent laryngeal nerve palsy was significantly higher in patients undergoing redo-surgery on the ipsilateral lobe compared to patients undergoing initial operation (3.8% vs. 1.1%; p = 0.03), whereas no difference was found in patients with contralateral redo-surgery compared to patients undergoing initial operation (p = 1.0). Furthermore, no difference was found in permanent recurrent laryngeal nerve palsy in patients with contralateral redo-surgery and patients undergoing ipsilateral redo-surgery (p = 0.58). No difference was found in persistent hypoparathyroidism between the groups (table 2).
Significant risk factors for contralateral recurrence in multivariate regression analysis are shown in table 3. Significant risk factors for contralateral recurrence were age at primary operation <37 years (OR 4.86; 95% CI 1.58–15.01) and time to recurrence <20 years (OR 6.53; 95% CI 2.23–19.01). In contrast, female gender and cystic nodules are not risk factors for contralateral recurrence.
| Table 1: Demographic parameters. | |||
| Contralateral group n = 30 | Ipsilateral group n = 79 | p-valuea | |
| Age (years) * | 56 (17–82) | 70 (26–90) | <0.001b |
| Sex (male/female) | 2/28 | 7/72 | 1.00 |
| Benign nodular goitre | 20 (66.7) | 59 (74.7) | 0.47 |
| Hyperthyroidism | 4 (13.3) | 12 (15.2) | 1.00 |
| Carcinoma | 6 (20.0) | 8 (10.1) | 0.20 |
| Number of recurrences * | 1 (1–2) | 1 (1–3) | 0.22b |
| Time to recurrence (years) * | 20 (1–60) | 27 (1–63) | 0.03b |
| Redo-surgery | |||
| Total thyroidectomy | 3 (10.0) | 41 (51.9) | – |
| Hemithyroidectomy | 27 (90.0) | 25 (31.6) | – |
| Hemithyroidectomy and subtotal contralateral | – | 13 (16.5) | – |
| Values in parentheses are percentages. *Values are median (range). a Fisher’s exact test unless indicated otherwise. b Student’s t-test. | |||
| Table 2: Postoperative morbidity rate. | ||||
| Initial surgeryn = 1,590 | Contralateral group n = 30 | Ipsilateral group n = 79 | p-value a | |
| Nerves at risk | 2,609 | 33 | 133 | |
| Recurrent nerve palsy | 30 (1.1) | 0 (0) | 5 (3.8) 5 (3.8) | 0.03 0.58 |
| 30 (1.1) | 0 (0) | 1.00 | ||
| Hypoparathyroidism | 11 (0.7) | 1 (1.2) | 0.44 | |
| 0 (0) | 1 (1.2) | 1.00 | ||
| 11 (0.7) | 0 (0) | 1.00 | ||
| Values in parentheses are percentages. a Fisher’s exact test. | ||||
| Table 3: Multivariate analysis for risk factors for contralateral recurrence. | |||
| OR | 95% CI | p-value | |
| Female gender | 1.16 | 0.19–6.95 | 0.88 |
| Age at primary operation <37 years | 4.86 | 1.58–15.01 | 0.006 |
| Time to recurrence <20 years | 6.53 | 2.23–19.01 | <0.001 |
| Cystic nodules | 2.08 | 0.78–5.56 | 0.14 |
| Multinominal logistic regression analysis. | |||
This retrospective study shows that the morbidity rate for recurrent disease after subtotal resection was significantly higher for ipsilateral redo-surgery compared to initial surgery, whereas redo-surgery can be performed safely on the contralateral lobe. Time to occurrence of recurrent disease in the contralateral lobe was significantly shorter compared to recurrence in the ipsilateral lobe. Young age at primary operation and short time to recurrence are independent risk factors for contralateral recurrent disease.
Recurrent goitre is a frequent problem following subtotal resection of the thyroid gland for benign multinodular goitre disease. Reoperation is associated with an increased morbidity rate due to postoperative adhesions [4, 6–8]. Clear definition concerning the side of recurrence and its morbidity in relation to the previous operation is mandatory and often not mentioned in published series. Results of the present study show that morbidity rate is significantly higher in redo-surgery compared to initial surgery. Detailed analysis showed that morbidity rate of reoperation on the ipsilateral lobe is associated with a significantly higher rate of persistent recurrent laryngeal nerve palsy compared to the initial operation due to adhesions. In contrast, reoperation on the contralateral lobe was not associated with an increased persistent recurrent laryngeal nerve palsy rate compared to initial surgery. Reoperation on the contralateral side is not associated with adhesions, but tissue conditions comparable to initial surgery. No statistical difference in persistent recurrent nerve palsy was found between patients undergoing ipsi- and contralateral redo-surgery due to an undersized patients’ population.
The reported incidence of recurrence rate ranges from 12% to 42% [9–11]. In the present series the reoperation rate of 6.9% can be explained by the surgical technique employed. Extended resection, including at least a hemithyroidectomy (total lobectomy on one side) as prevention for ipsilateral recurrent goitre was introduced already in 1991 at our institution. In multivariate analysis two independent risk factors for contralateral recurrence were found. First, young age at primary operation was found as an independent risk factor for contralateral recurrence. This can be explained with the higher probability rate of recurrence, when initial operation was performed at younger age. Second, short time to recurrence was also found as an independent risk factor for contralateral recurrent disease. Apart from missing some micro nodules on the contralateral side on the initial operation there seems to be a different aetiology to explain the shorter time to occurrence between ipsi- and contralateral recurrent disease (fig. 1). Nodules within multinodular goitres in recurrent disease were of polyclonal rather than clonal character [12, 13]. The proliferation of polyclonal nodules suggests that the polyclonal nodules arise from differentiating cells with a higher than average growth potential, due to acceleration of their proliferation rate by unknown superordinate molecular events [14]. With the understanding of the molecular growth mechanism in goitrogenesis shorter time of recurrence in the contralateral lobe can be also explained.
Limitations of the study include lack of randomisation and the retrospective study design. Only patients referred to our clinic were included in the analysis of recurrent disease. However, as a tertiary referral center specialising in endocrine surgery the probability that patients with recurrent disease were treated elsewhere is very low. At the time of initial operation both lobes were checked for nodules, however lesions missed during initial surgery cannot be fully excluded. Nevertheless, shorter time of recurrence on the contralateral lobe can mainly be explained by molecular growth mechanism rather than by missed nodules.
In conclusion, reoperation on the ipsilateral lobe is associated with a significantly higher morbidity rate compared to initial surgery. In contrast, reoperation on the contralateral lobe carries no additional morbidity. Therefore, it is important to prevent redo-surgery on the previously operated lobe by performing at primary operation at least a hemithyroidectomy instead of subtotal resection.
1 Agarwal G, Aggarwal V. Is total thyroidectomy the surgical procedure of choice for benign multinodular goiter? An evidence-based review. World J Surg. 2008;32(7):1313–24.
2 Seiler CA, Vorburger SA, Burgi U, Candinas D, Schmid SW. Extended resection for thyroid disease has less operative morbidity than limited resection. World J Surg. 2007;31(5):1005–13.
3 Moalem J, Suh I, Duh QY. Treatment and prevention of recurrence of multinodular goiter: an evidence-based review of the literature. World J Surg. 2008;32(7):1301–12.
4 Lefevre JH, Tresallet C, Leenhardt L, Jublanc C, Chigot JP, Menegaux F. Reoperative surgery for thyroid disease. Langenbecks Arch Surg. 2007;392(6):685–91.
5 Muller PE, Jakoby R, Heinert G, Spelsberg F. Surgery for recurrent goitre: its complications and their risk factors. Eur J Surg. 2001;167 (11):816–21.
6 Gibelin H, Sierra M, Mothes D, Ingrand P, Levillain P, Jones C, et al. Risk factors for recurrent nodular goiter after thyroidectomy for benign disease: case-control study of 244 patients. World J Surg. 2004;28 (11):1079–82.
7 Erbil Y, Bozbora A, Yanik BT, Ozbey N, Salmaslioglu A, Ozarmagan S. Predictive factors for recurrent non-toxic goitre in an endemic region. J Laryngol Otol. 2007;121(3):231–6.
8 Menegaux F, Turpin G, Dahman M, Leenhardt L, Chadarevian R, Aurengo A, et al. Secondary thyroidectomy in patients with prior thyroid surgery for benign disease: a study of 203 cases. Surgery. 1999;126(3):479–83.
9 Wadstrom C, Zedenius J, Guinea A, Reeve T, Delbridge L. Multinodular goitre presenting as a clinical single nodule: how effective is hemithyroidectomy? Aust N Z J Surg. 1999;69(1):34–6.
10 Rojdmark J, Jarhult J. High long term recurrence rate after subtotal thyroidectomy for nodular goitre. Eur J Surg. 1995;161(10):725–7.
11 Pappalardo G, Guadalaxara A, Frattaroli FM, Illomei G, Falaschi P. Total compared with subtotal thyroidectomy in benign nodular disease: personal series and review of published reports. Eur J Surg. 1998;164(7):501–6.
12 Harrer P, Brocker M, Zint A, Derwahl M, Barbera L, Zumtobel V. The clonality of nodules in recurrent goiters at second surgery. Langenbecks Arch Surg. 1998;383(6):453–5.
13 Studer H, Gerber H, Zbaeren J, Peter HJ. Histomorphological and immunohistochemical evidence that human nodular goiters grow by episodic replication of multiple clusters of thyroid follicular cells. J Clin Endocrinol Metab. 1992;75(4):1151–8.
14 Harrer P, Broecker M, Zint A, Schatz H, Zumtobel V, Derwahl M. Thyroid nodules in recurrent multinodular goiters are predominantly polyclonal. J Endocrinol Invest. 1998;21(6):380–5.
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article was reported.