Vertebral body stenting / stentoplasty
DOI: https://doi.org/10.4414/smw.2012.13658
Paul F.
Heini, Regula
Teuscher
Summary
Osteoporotic vertebral fractures are frequent. Although the majority of fractures follow a benign course, there are certain fracture types which result in severe spinal deformity and / or are associated with neurological complications. These patients should be detected early and undergo surgical treatment. Vertebroplasty remains an important and effective treatment option for acute painful vertebral fractures showing progressive collapse. By this procedure the fracture can be stabilised, the pain is controlled and the progression of height loss is also halted. If a vertebral body shows a higher degree of collapse and kyphotic deformity or even some posterior wall involvement, the stentoplasty procedure (further evolution of kyphoplasty) allows height resotartion by the stent and the stabilisation of the vertebral body by cement.
Introduction
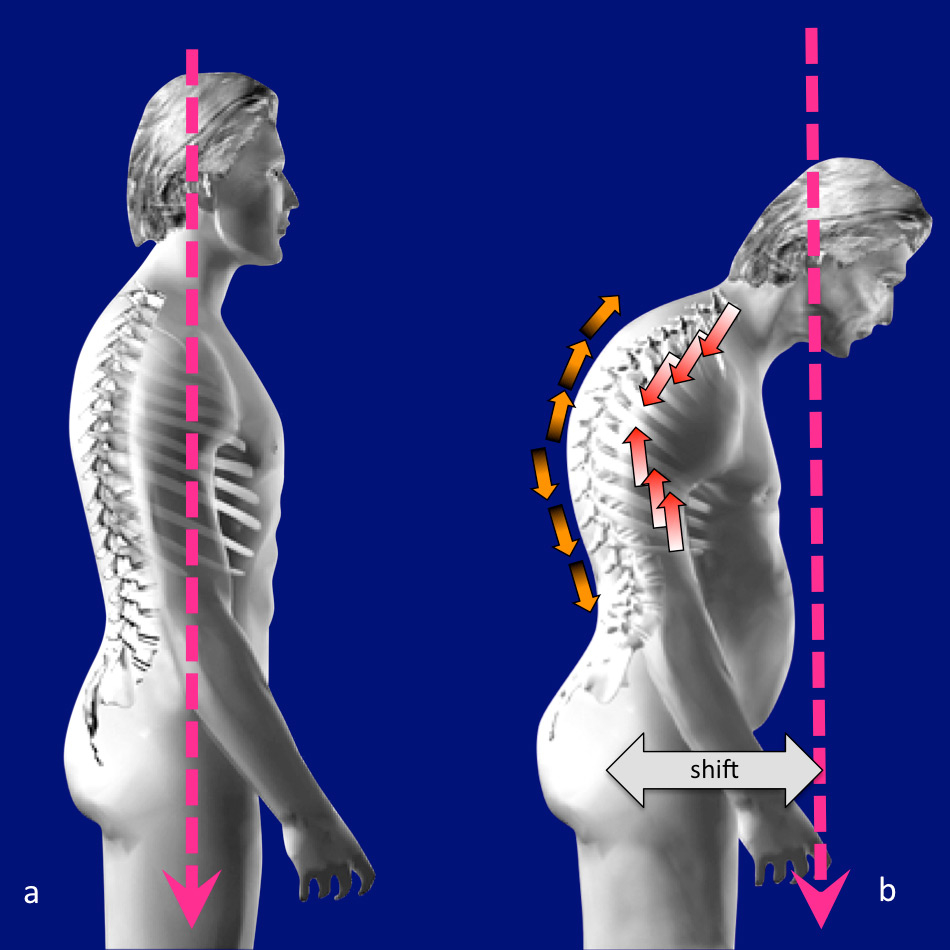
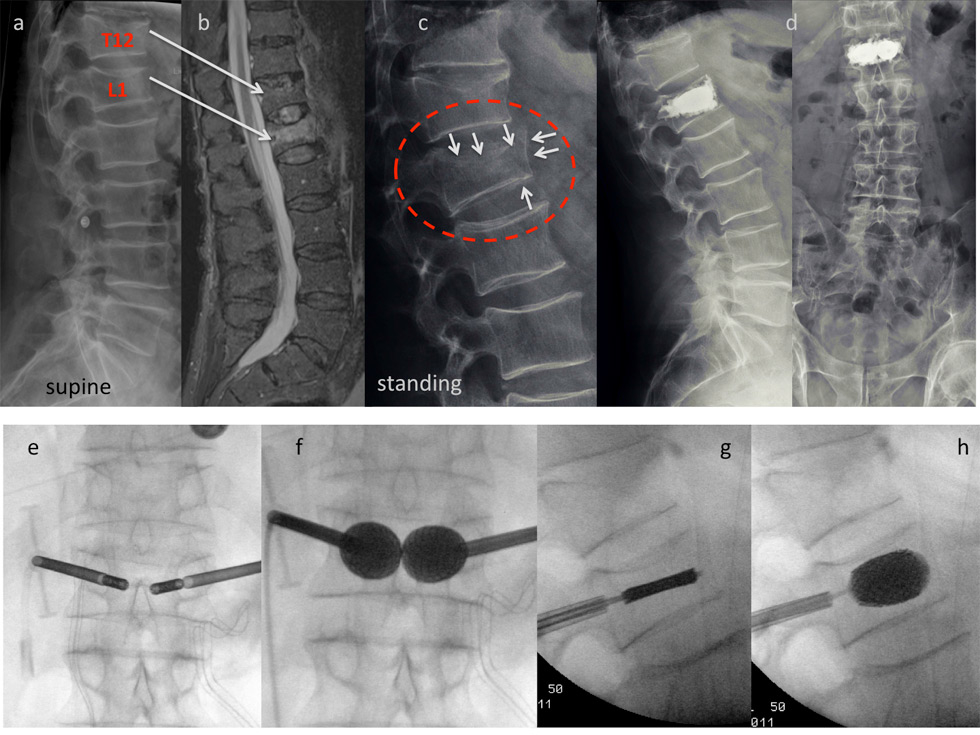
Vertebral body compression fractures (VBCF) are the hallmark of osteoporosis, and its incidence increases exponentially with increasing age [1]. In general VBCF are considered to be benign, but epidemiological data show major morbidity and loss of quality of life comparable to that of hip fractures. Mortality in patients with VBCF is higher than in a non fractured population. [2, 3]. These fractures frequently result in loss of physiological posture, which in turn leads to higher loads on the vertebrae on the one hand and higher stress for the back muscles on the other. (fig. 1)
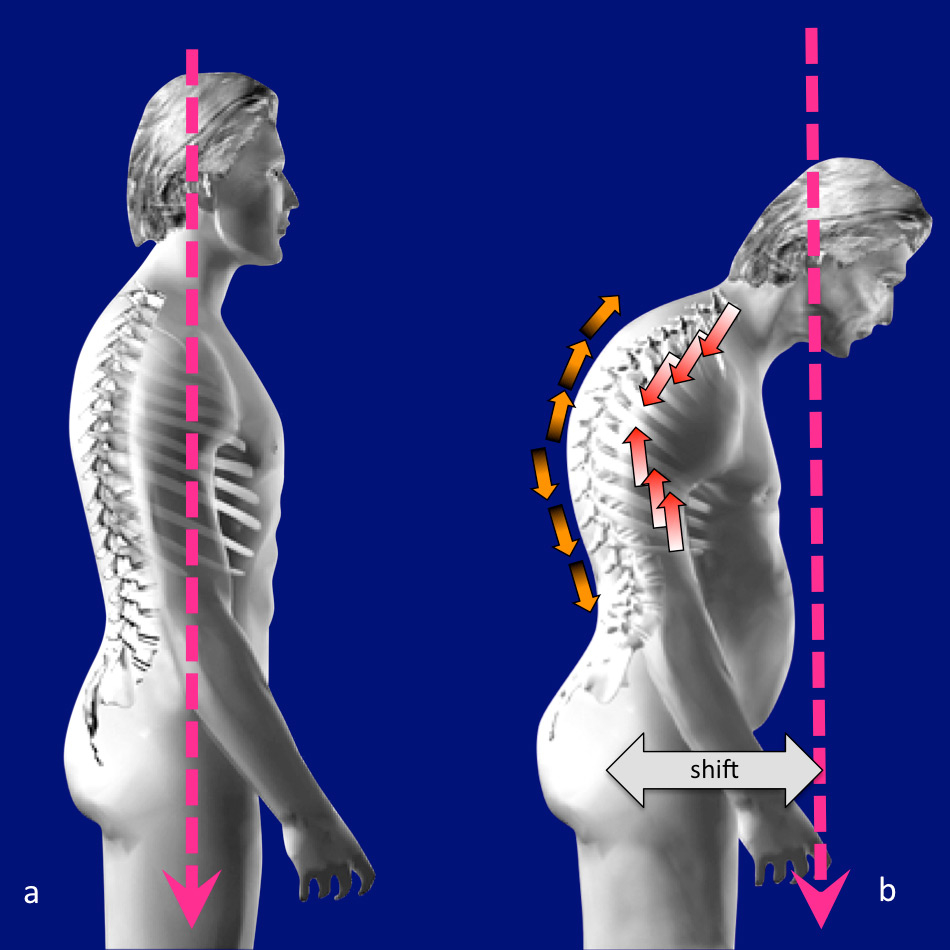
Figure 1
Loss of posture due to vertebral factures: The centre of gravity (pink) is in line with the hip joint in a balanced spine (a). Due to vertebral fractures increased kyphosis occurs and the centre of gravity is shifting forward, throwing the spine out of balance (b). This leads to higher compression loads on the vertebrae (red arrows) and higher strain on the back muscles (orange arrows).
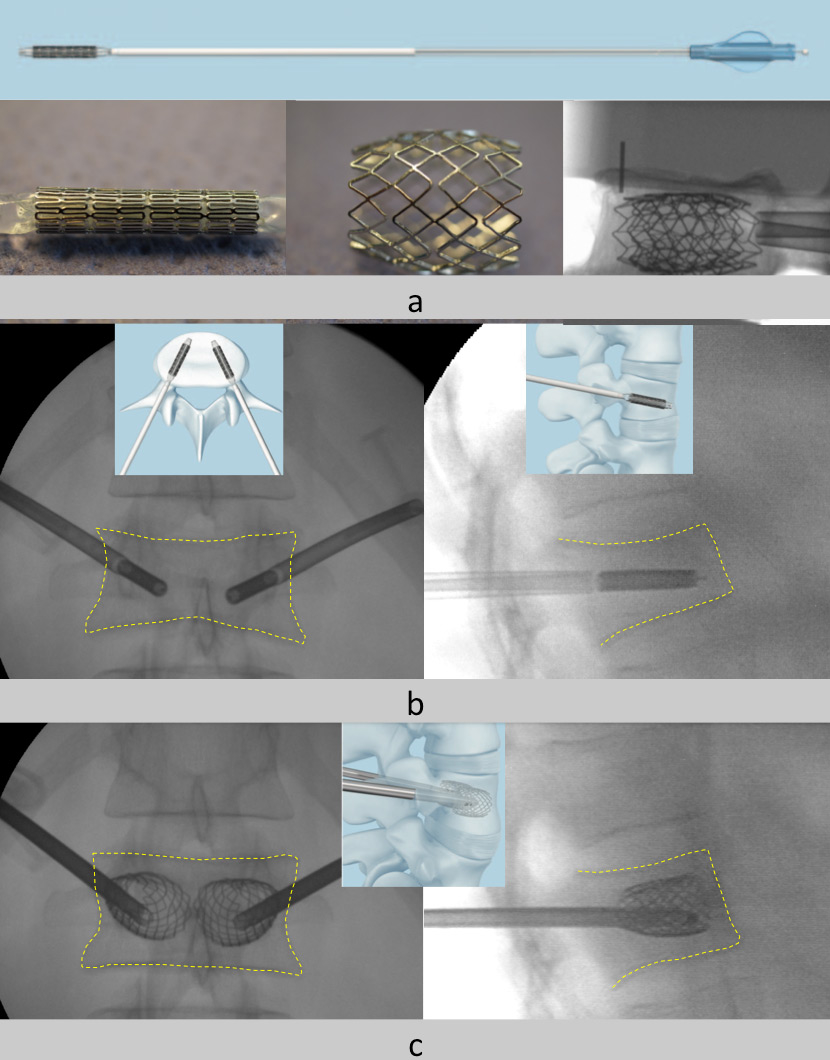
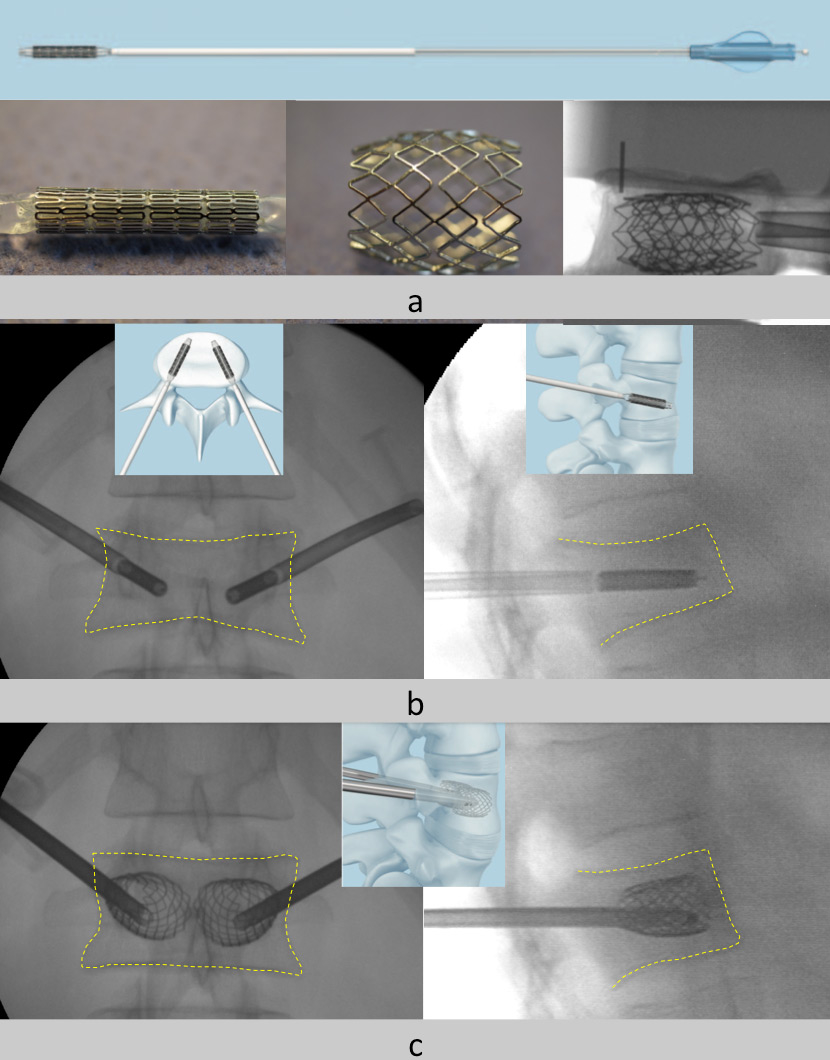
Figure 2
The vertebral body stent principle: A 4 mm stent with different lengths can be expanded up to 400%. It can provide preliminary stability and maintain the height gain before cement is injected; it cannot work as a standalone device (a). The stents are placed on each side through the pedicles (b). The stent is then expanded by the balloon. In this way the vertebral height (c) is restored. The final stabilisation is performed by the injection of bone cement (not shown here). The contours of the vertebral body are outlined by the yellow dashed lines.
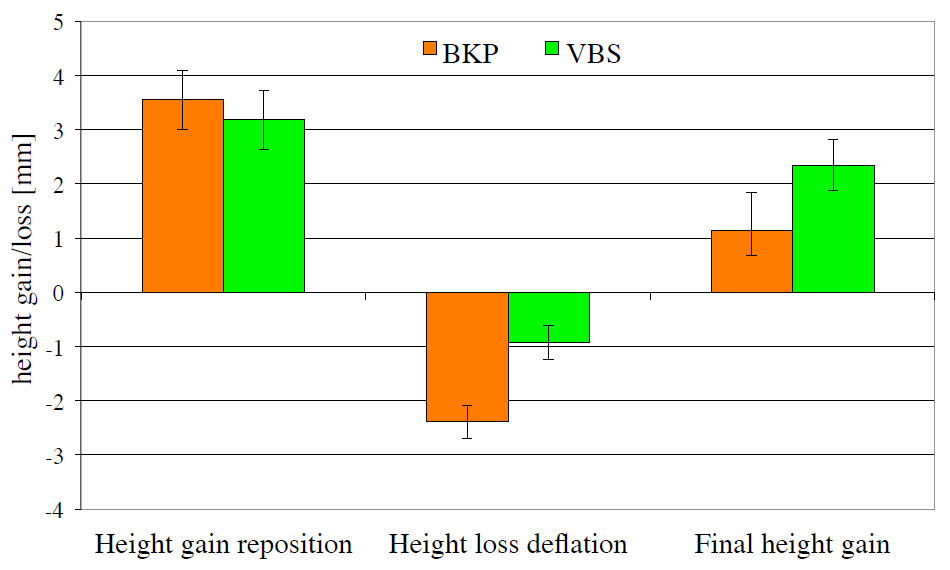
Normally VBCF are treated conservatively. However, in patients with severe pain stabilisation of the vertebral body with bone cementis now well accepted [4, 5]. The procedure consists in the injection of highly viscous cement directly into the fractured vertebral body (vertebroplasty) or by prior cavity creation with a balloon (kyphoplasty). These procedures do not allow real restoration of the compressed vertebral body, and further extension of the technique consists in vertebral body stenting, also called stentoplasty [6]. The principle resenbles that for vascular stents – a balloon mounted stent is expanded and in this way the vertebral body is lifted and, as a preliminary move, stabilised by the stent. For final stabilisation bone cement is injected. The stent can be expanded by some 400%, from 4.2 mm to 17 mm. (fig. 2). Based on in vitro experiments, greater height gain with the stent was demonstrated when compared to the balloon-only technique (fig. 3). For all patients with an osteoporotic fracture, assessment of bone metabolism and adequate medical treatment of osteoporosis are mandatory [7, 8].
Surgical principle and technique of stentoplasty
Stentoplasty represents a percutaneous minimally invasive intervention resembling a vertebroplasty or kyphoplasty procedure. Two balloon mounted stents are placed through the pedicles of the fractured vertebral body. The balloons are then deployed by a inflation system under fluoroscopic guidance until the vertebral height is restored. The balloons are then retrieved and the stent and the surrounding bone is filled with bone cement. The intervention is performed in prone position, under either local/stand-by or general anaesthesia. The duration of the procedure is some 45 minutes. The patient is allowed to get up as soon as this is tolerated and is free to resume activity depending on pain. Usually the intervention is performed within a short hospital stay of two days.
Requirements for a surgical procedure are the correct indication (see below) and the medical condition, which requires the patient to tolerate the prone position. Aspirin or even clopidogrel or its combination can be continued during the surgical procedure (if this is required); patients under coumarins should stop the medication in order to reach a INR of 1.5 or less.
Indication for a stentoplasty procedure
The use of the vertebral body stent is indicated in acutely and subacutely painful VBCF with at least 35% height loss / 15° kyphotic deformity with the potential of reducibility. In consolidated and fixed fractures the use of a stent is no longer indicated. The fracture type needs to be assessed on the basis of normal x-rays and a CT or MRI scan. The fracture to be treated needs to be mobile (greater collapse in the standing film in comparison to the images in supine position). Therefore the indication is restricted to fractures of up to 4 weeks’ duration or if there is a so-called non-union (Kummel’s disease). Burst type fractures can be treated by a stentoplasty procedure provided the posterior wall involvement is minor (<25%) and no neurological symptoms are present. With these aspects in mind the treatment of traumatic fractures is possible as well. An important group are fractures associated with metastatic lesions and myeloma. Stenting provides a well defined cavity which allows more controlled and accurate stabilisation of the vertebral body with bone cement.
The indication for a stentoplasty needs to be based on the “personality” of the fracture and the general condition of the patient. The surgeon must decide whether a simple vertebroplasty procedure is sufficient or a stentoplasty is more appropriate; in rare cases a more invasive intervention with open surgery is even required. Hence any surgeon who is performing this intervention must be familiar with the treatment of vertebral fractures and be able to provide a correct assessment of the lesion to be treated. For the general state of the patient, especially also the medical treatment of osteoporosis an interdisciplinary exchange with the attending physicians is essentiall.
|
Table 1 :Facts about osteoporosis to remember. |
| Osteoporosis represents a systemic disease which affects the bone in two ways: it changes its mineral content but also its structural architecture. |
| Vertebral compression fractures (VBCF) are the hallmark of osteoporosis, worldwide estimate 5m fractures per year. |
| The incidence of VBCF is age dependent and shows an exponential increase with age. |
| The fracture risk is increases over-exponentially with the number of pre-existing fragility fractures. |
| The majority of VBCF is not documented and wrongly interpreted as unspecific back pain. Only one third of all fractures gain clinical attention and one fourth out of this group require hospitalisation. |
| The majority of VBCF show a self-limiting pain-course. |
| VBCF affect the quality of life significantly and patients show a higher mortality. |
| VBCF can result in severe complications with neural compression/paralysis, mechanical instability/non-union. |
| Injection of PMMA into the vertebral body provides mechanical stability; furthermore it prevents further sintering. |
| Stabilization of a fracture provides pain relief. |
|
Table 2: Assessment and treatment of patients with osteoporotic vertebral fractures |
|
Patients with acute back pain and a risk profile (age, known osteoporosis; red flags) should undergo a radiological investigation (standing X-ray of the painful spine section).
|
| Patients with a documented fracture and severe / ongoing pain show a high risk for progressive collapse of the vertebral body and therefore should have a follow up X-ray check one to two weeks after the index check. |
| If the FU X-ray shows progressive height loss (>30%) patients should be considered for a vertebroplasty or stentoplasty procedure if there is a relevant deformity. |
| If patients are immobilised and / or need a hospital stay due the painful fracture, surgery should be considered. This serves to shorten the hospital stay and is therefore cost effective [17]. |
| Patients with subacute fractures and persistent pain may present with nonunion of the fracture (so called Kummel disease). The diagnosis is best performed by a CT or MRI scan. If a non-union is present, cement reinforcement can provide stability and control pain. |
| High risk patients with multiple osteoporotic fractures within a short time period should be treated early with (repetitive) cement reinforcement, if necessary also with a prophylactic purpose [9, 18]. |
| Subacute fractures (4–6 weeks) with severe collapse can be reduced by closed means or stentoplasty if needed. |
|
Vertebral fractures due to metastatic lesions or myeloma can be treated with cement reinforcement if the posterior elements remain intact and no neurological involvement is present [19].
|
Treatment rationale for osteoporotic vertebral fracutes
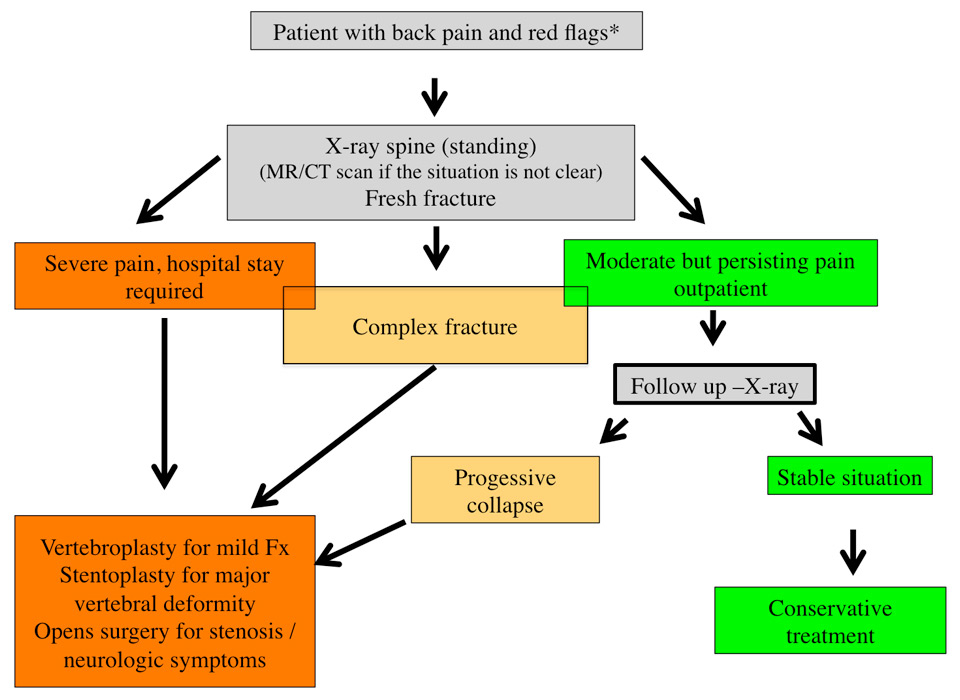
Although the majority of vertebral fractures can be treated conservatively it is necessary to avoid complications associated with these fractures. An overview for patient assessment is shown in (fig. 4). This algorithm provides a rationale for differentiation between stable/benign fractures and potentially unstable lesions. Some fracture types have a morphological pattern (complex fracture types) such that surgery is needed from the outset. These are often “traumatic” fractures in the osteoporotic patient. Generally speaking one should assess patients at risk for a possible fracture with a normal (standing) X-ray of the spine section of interest. It is recommended that an x-ray be repeated after one to two weeks if patients continue to have severe pain. In the case of further height loss a surgical procedure should be considered. By this means it is possible to control the pain on the one hand and to avoid a further collapse of the fractured vertebral body on the other. If there is major height loss at this stage the use of a stent allows restoration of the vertebral height. (fig. 6)
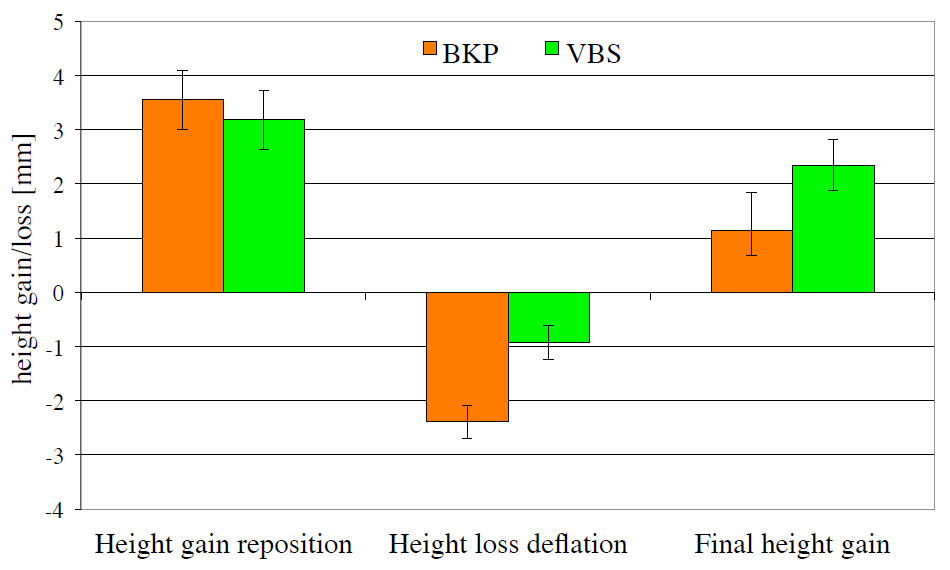
Figure 3
The potential of height restoration and maintenance has been assessed in vitro on cadaver specimens. 24 vertebral bodies were fractured and kept under a preload of 110 N in order to maintain the “physiological” pressure. Then the height was restored using either ballon kyphoplasty (BKP) or vertebral body stenting (VBS). With the stent the relapse after deflation of the balloon is significantly lower which in turn leads to better height restoration in total.
Clinical / radiological results
In the light of a preliminary assessment of the patients we have treated over a one year period the clinical outcome with respect to pain reduction is similar to that of vertebroplasty [9]. 34 patients (20 female, 14 male) have been treated. Average age was 74 years (43–92). The age and level distribution is shown in fig. 5. The amount of reduction achieved was measured by the segmental kyphosis. The average kyphosis angle preoperatively was 23°(13°–32°) and could be corrected to 12° (0°–16°) postoperatively. Height restoration was assessed semi-quantitatively. The amount was graded from 0 to 3, where 0 meant no reduction possible to 3 with complete restoration. There were 5 cases with grade 0, we have seen 12 cases with a reduction of grade 1 meaning 50% height gain, 14 cases with grade 2 which is 75% height gain and 3 cases with complete height restoration (fig. 6).
Cement leakage was observed in 9 out of 34 patients. These leaks were observed in the paravertebral tissue in 6 cases, in two cases vascular leaks were present and in one case leakage into the foramen occurred. None of these leaks were clinically symptomatic.
In our series the best potential for height gain was observed in fresh traumatic fractures (n = 6). The healthy bone provides an optimal counterfort for application of reduction forces by the stent (fig. 2).
Discussion
The treatment of VBCF with cement reinforcement has gained widespread acceptance in the last decade [4, 5]. However, its widespread use is challenged by the advocates of evidence-based medicine. The Swiss Medical Board recently published a critical review on this topic [10]. In the light of two randomised placebo controlled trials the vertebroplasty procedure did not offer significant clinical difference in comparison to a shame intervention consisting of a facet block [11, 12]. Although the studies have been published in the NEJM they obviously suffer from a selection bias related to the investigations and the results presented (which are sound within the investigated population) do not represent the situation of our daily work; the results presented lack external validity [13–15] and are contrary to common sense and clinical experience [13]. Two further randomised controlled trials compare conservative treatment with vertebroplasty or kyphoplasty for acute fractures. In both studies the advantage of surgery is demonstrated by fast and lasting pain relief. Surgically treated patients gain days/weeks of reduced pain, which in turn keeps them more active and enhances life quality [5, 16]. Clinical experience with stentoplasty is limited. The impact of height restoration needs to be assessed. A multi-centre trial is in progress to compare the different treatment modalities, but patient recruitment is slow and therefore no hard data are available for the moment.
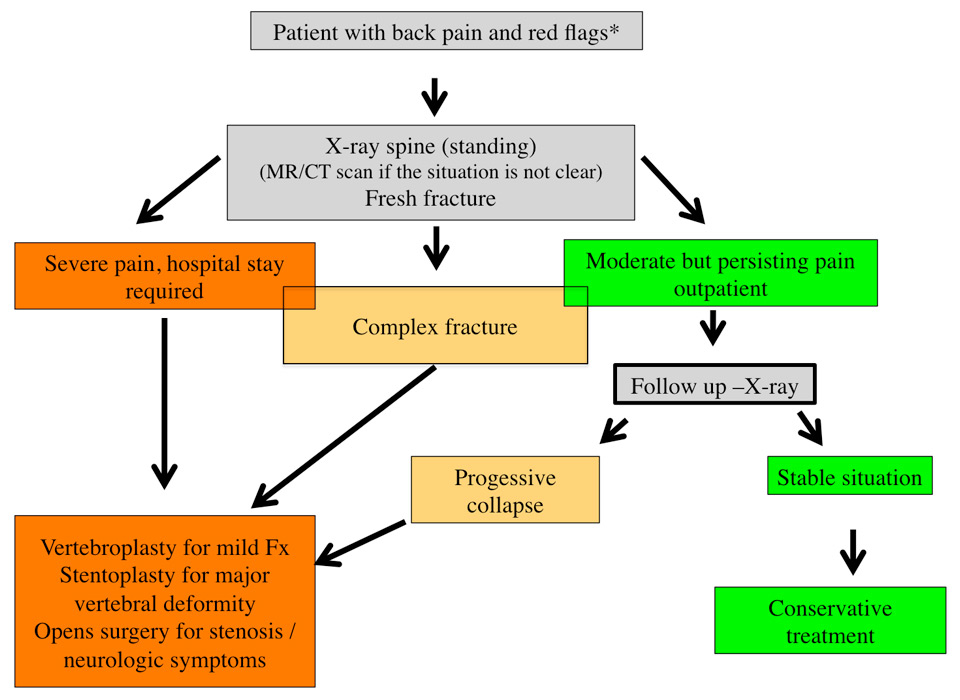
Figure 4
Algorithm for the assessment and treatment of patients with osteoporotic vertebral fractures: Patients presenting with acute, severe back or low back pain and a risk profile (red flags) age >65, history of previous fractures, renal disease, steroid medication, BMI <20 etc.) should undergo an imaging study. The investigation of first choice remains a standing X-ray of the region of interest in two planes. If there is any uncertainty an MRI or CT scan can further differentiate between old and new fractures and provide a more detailed impression regarding the exact type of lesion and allow to differentiate between a simple compression type fracture or a complex lesion. The comparison of a standing film with an investigation taken in supine position is helpful for detecting a mobility in the fractured vertebra. Based on clinical findings and the results of the imaging studies one can decide the further treatment. Patients who need hospital admission due the severity of pain or patients with complex lesions should be referred for an early surgical intervention. The majority of patients will remain outpatient. For them it is important to monitor the clinical course and if there is persisting pain or a high risk situation based on their history a follow up X-ray is mandatory in order to check for further height loss of the fractured vertebra or new fractures. If so, again a surgical intervention should be considered. Patients with a spinal stenosis and neurological symptoms usually need an open surgical procedure with decompression and stabilization.

Figure 5
Stentoplasty patients (n = 34): a) age distribution of patients treated, b) distribution of levels treated.
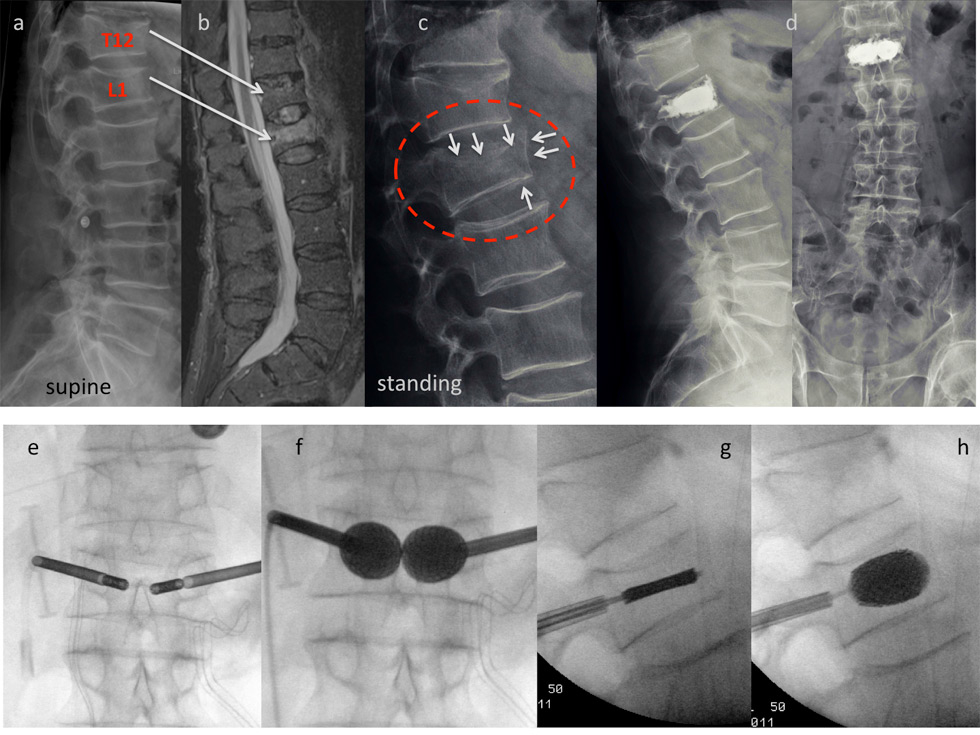
Figure 6
Case report stentoplasty: This 77-year-old male patient is referred to the emergency room after a fall from some 1.5 m. He presents with acute immobilising back pain. The x-ray taken in the supine position depicts fractures of T12 and L1 (a). The MRI scan discloses a fresh fracture of L1, whereas T12 appears old (b). The fracture was considered simple and conservative treatment was initiated with in- hospital physiotherapy and pain medication. After 3 days a standing X-ray was performed which shows a much more complex lesion in comparison to the initial pictures (white arrows): There is a split fracture with anterior wall displacement, and also the upper endplate has subsided considerably (c). A stentoplasty procedure was performed in local anesthesia, which did provide good height restoration and immediate stabilisation (d). The intraoperative pictures demonstrate complete restoration of the vertebral body’s shape (e-h).
References
1 Incidence of vertebral fracture in europe: results from the European Prospective Osteoporosis Study (EPOS). J Bone Miner Res. 2002;17:716–24.
2 Bliuc D, Nguyen ND, Milch VE, et al. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA 2009;301:513–21.
3 Edidin AA, Ong KL, Lau E, Kurtz SM. Mortality risk for operated and nonoperated vertebral fracture patients in the medicare population. J Bone Miner Res. 2011;26:1617–26.
4 Muijs SP, Nieuwenhuijse MJ, Van Erkel AR, Dijkstra PD. Percutaneous vertebroplasty for the treatment of osteoporotic vertebral compression fractures: evaluation after 36 months. J Bone Joint Surg Br. 2009;91:379–84.
5 Klazen CA, Lohle PN, de Vries J, et al. Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos II): an open-label randomised trial. Lancet. 2010;376(9746):1085–92.
6 Rotter R, Martin H, Fuerderer S, et al. Vertebral body stenting: a new method for vertebral augmentation versus kyphoplasty. Eur Spine J. 2010;19:916–23.
7 Meier C, Kranzlin ME. Calcium supplementation, osteoporosis and cardiovascular disease. Swiss Med Wkly. 2011;141:w13260.
8 Rizzoli R, Kraenzlin M, Krieg MA, et al. Indications to teriparatide treatment in patients with osteoporosis. Swiss Med Wkly. 2011;141:w13297.
9 Diel P, Freiburghaus L, Roder C, et al. Safety, effectiveness and predictors for early reoperation in therapeutic and prophylactic vertebroplasty: short-term results of a prospective case series of patients with osteoporotic vertebral fractures. Eur Spine J. 2011.
10 swiss_medical_board. Vertebroplastie und Kyphoplastie bei osteoporotischen Wirbelkörperfrakturen, 2011. http://www.medical-board.ch/index.php?id=809.
11 Kallmes DF, Comstock BA, Heagerty PJ, et al. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med. 2009;361:569–79.
12 Buchbinder R, Osborne RH, Ebeling PR, et al. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med. 2009;361:557–68.
13 Heini PF. [Vertebroplasty: an update: value of percutaneous cement augmentation after randomized, placebo-controlled trials]. Orthopade. 2010;39:658–64.
14 Boszczyk B. Volume matters: a review of procedural details of two randomised controlled vertebroplasty trials of 2009. Eur Spine J. 2010.
15 Bono CM, Heggeness M, Mick C, Resnick D, Watters WC, 3rd. North American Spine Society: Newly released vertebroplasty randomized controlled trials: a tale of two trials. Spine J. 2010;10:238–40.
16 Wardlaw D, Cummings SR, Van Meirhaeghe J, et al. Efficacy and safety of balloon kyphoplasty compared with non-surgical care for vertebral compression fracture (FREE): a randomised controlled trial. Lancet. 2009;373:1016–24.
17 Masala S, Ciarrapico AM, Konda D, et al. Cost-effectiveness of percutaneous vertebroplasty in osteoporotic vertebral fractures. Eur Spine J. 2008;17:1242–50.
18 Heini PF, Orler R. Vertebroplasty in severe osteoporosis. Technique and experience with multi-segment injection. Orthopade. 2004;33:22–30.
19 Heini PF, Pfaffli S. Cement injection for spinal metastases (vertebroplasty and kyphoplasty). Orthopade. 2009;38:335–336, 338–42.