The Acute Physiology and Chronic Health Evaluation II score is helpful in predicting the need of relaparotomies in patients with secondary peritonitis of colorectal origin
DOI: https://doi.org/10.4414/smw.2012.13640
Carsten T.
Viehl, Rebecca
Kraus, Manuel
Zürcher, Thomas
Ernst, Daniel
Oertli, Christoph
Kettelhack
Summary
BACKGROUND: Secondary peritonitis of colorectal origin has considerable morbidity and mortality. Relaparotomies are frequently neccessary in the course of the disease. The objective of this study was to evaluate several scores in terms of their predictive value, i.e. whether Mannheim Peritonitis Index (MPI), Acute Physiology And Chronic Health Evaluation (APACHE) II, or Colorectal Physiological and Operative Severity Score for the Enumeration of Mortality and Morbidity (CR-POSSUM) scores can predict relaparotomies.
METHODS: Charts of 147 patients treated for secondary peritonitis of colorectal origin were retrospectively reviewed, MPI, APACHE II, and CR-POSSUM scores were calculated, and groups of patients with or without relaparotomies were compared.
RESULTS: Thirty-four percent of patients underwent one or more relaparotomies. Patients with relaparotomies showed a significantly higher APACHE II score than patients without relaparotomies (p = 0.004). MPI (p = 0.072) and CR-POSSUM score (p = 0.319) did not differ between the two groups. A high APACHE II score was also significantly associated with the need for a relaparotomy on demand (p <0.001), and for the combined outcome parameter relaparotomy and/or an interventional drainage (p = 0.046). Both other scores were not predictive for these outcomes. Overall in-hospital mortality was 21.8%. All three scores investigated were predictive for mortality. Sensitivity was 62.5%, 78.1%, and 75.0% for MPI, APACHE II score, and CR-POSSUM score, respectively.
CONCLUSION: The Acute Physiology And Chronic Health Evaluation II score might be helpful in predicting the need for relaparotomies in patients with secondary peritonitis of colorectal origin.
Introduction
Secondary peritonitis of colorectal origin has considerable morbidity and mortality. Due to a breach in the integrity of the colonic wall, significant contamination of the abdominal cavity occurs that cannot always be fully mastered during the first operation. Therefore, relaparotomies are frequently performed in the course of the disease. A relaparotomy may be planned during the first operation performed for secondary peritonitis (so-called index operation) to repeatedly clean the abdominal cavity in case of extensive pollution with intestinal contents (planned relaparotomy; PR), or may be required due to signs of persistent peritonitis or other complications (relaparotomy on demand, ROD). Different scoring systems have been developed to quantify the extent of peritonitis and to predict its outcome. The Mannheim Peritonitis Index (MPI) was constructed to predict the individual risk of death due to peritonitis based on patients’ characteristics, organ (dys)function, risk factors, and intraoperative findings [1]. The Acute Physiology And Chronic Health Evaluation (APACHE) II score was modeled as a general measure of severity of disease and to predict the in-hospital mortality of patients on intensive care units. The APACHE II score is calculated based on physiologic parameters, age, and a chronic health evaluation [2]. Finally, the ColoRectal Physiological and Operative Severity Score for the enUmeration of Mortality and morbidity (CR-POSSUM) was developed as a risk score dedicated to colorectal surgery in the United Kingdom [3], and has subsequently been evaluated for the United States as well [4]. Based on a physiological score and an operative severity score, the individual mortality risk is predicted [3]. All these scores have been validated to reliably predict mortality. However, data on whether these scores can also predict the need for relaparotomies or other reinterventions is very scarce [5, 6]. As the need for a relaparotomy is closely related to the magnitude of the disease, we hypothesised that high MPI, APACHE II, and CR-POSSUM scores could be correlated with the need for one or more relaparotomies. Therefore, the objective of the current study was to evaluate whether the MPI, APACHE II, or CR-POSSUM scoring systems can predict relaparotomies.
Patients and methods
Patients
A consecutive series of patients treated for secondary peritonitis of colorectal origin at the University Hospital Basel between 1 January 2001 and 31 December 2006 was identified using a hospital database. We performed a retrospective (post-hoc) analysis of available data: By chart review, pertinent data on patients’ characteristics, parameters for the calculation of scores, and information on the postoperative course were recorded and stored in an electronic data sheet (Excel for Macintosh X, Microsoft Corporation, Redmond, WA). Secondary peritonitis of colorectal origin was defined as an intra-abdominal infection due to breach in the integrity of the colon or rectum (perforation, infection, ischaemia, or as a result of previous surgery) [7, 8]. Patients with perforated appendicitis, with complicated diverticulitis exclusively treated percutaneously, and with abdominal trauma were excluded from this analysis. Patients with secondary peritonitis underwent (re)laparotomy, extensive lavage of all four quadrants, and control of the source for the peritonitis. In cases where the source control was not feasible or not guaranteed, a PR was invariably scheduled. A laparostoma was created when the intraabdominal pressure was found to be too high during the index operation or when a PR was scheduled. The index operation was defined as the first laparotomy performed for the secondary peritonitis. Therefore, in case of postoperative secondary peritonitis, the second laparotomy is the index operation. For comparisons, different groups were defined as follows: patients with (one or more) relaparotomies (relaparotomy group), patients without relaparotomy (no relaparotomy group), patients with a relaparotomy and/or an interventional drainage (relaparotomy-intervention group), patients without any relaparotomy or interventional drainage (no relaparotomy-intervention group). Characteristics of the patients’ population are given in table 1. The study was approved by the regional ethical committee before the data was collected.
|
Table 1: Characteristics of the population. |
|
Total
|
|
n =
147
|
%
100.0%
|
| Gender |
Male |
70 |
47.6% |
| |
Female |
77 |
52.4% |
| Aetiology of secondary peritonitis |
Perforated diverticulitis |
64 |
43.5% |
| |
Anastomotic leakage |
23 |
15.6% |
| |
Perforation due to ischaemia |
14 |
9.5% |
| |
Other |
46 |
31.3% |
| Relaparotomies |
No |
97 |
66.0% |
| |
Yes |
50 |
34.0% |
| |
– Planned relaparotomy |
17 |
11.6% |
| |
– Relaparotomy on demand |
33 |
22.4% |
| Interventional drainage |
Drainage only |
5 |
3.4% |
| |
Relaparotomy and drainage |
3 |
2.0% |
| In-hospital mortality |
|
32 |
21.8% |
| |
|
median |
range |
| Age (years) |
|
71 |
21–97 |
| Length of stay (days) |
|
19 |
1–153 |
| Scores |
ASA |
3 |
1–4 |
| |
MPI |
21 |
5–43 |
| |
APACHE II |
14 |
4–33 |
| |
CR-POSSUM |
31.8 |
14.0–46.9 |
Scores
The MPI is calculated at the time of the index operation based on patients’ characteristics (age and sex), organ function, risk factors (malignancy), and intraoperative findings (origin of peritonitis, nature and spread of the exsudate). It may range from 0 to 47 points; a higher numerical score is correlated with increased mortality [1]. The APACHE II score is calculated based on twelve different physiologic parameters recorded 24 hours after the index operation, age, organ function, and immunocompetence. It may range from 0 to 71 points; an increasing score is correlated with a higher subsequent risk of in-hospital death [2]. The CR-POSSUM is determined at the time of the index operation based on age and five different physiologic parameters (physiological score), and four parameters describing, severity, type and urgency of the operation performed (operative severity score). It ranges from 10–44 points, higher scores again being correlated with higher in-hospital mortality [3].
For this study, all scores were retrospectively calculated based on the recorded parameters. Infrequently, information on some parameters was missing. In these cases, values were assumed to be within the normal range. Thus, any “overscoring” was avoided [9].
Statistical analysis
Statistical analysis was performed with SPSS 13.0 for Macintosh (SPSS Inc., Chicago, IL). For descriptive statistics median values with ranges are given. Continuous and interval scaled variables were analysed with the Mann-Whitney U-test, and categorical variables with the χ2-test. Sensitivity analysis was performed with receiver-operator characteristic (ROC) curve analysis; the respective median score of the entire patient population was used as cut-off value. A p-value <0.05 was considered to be significant. All p-values were two-sided.
Results
Relaparotomies
One hundred forty-seven patients were treated for secondary peritonitis of colorectal origin at our institution during the six-year period investigated (table 1). Fifty patients (34.0%) received one or more relaparotomies (relaparotomy group). Patients with relaparotomies showed a significantly higher APACHE II score than patients without relaparotomies (n = 97, 66.0%; p = 0.004). However, MPI and CR-POSSUM scores did not differ between the two groups (table 2). In addition, the relaparotomy group had a significantly higher mortality rate than the no relaparotomy group (32.0% vs. 16.5%, p = 0.031), a significantly higher American Society of Anesthesiologists (ASA) score [10] (median 3 [range 2–4] vs. median 3 [range 1–4]; p = 0.002), and a significantly longer length of stay (LOS; 28 [1-153] vs. 15 days [1-97]; p <0.001). The two groups showed no differences for age (p = 0.452), gender (p = 0.947), and the aetiology of the secondary peritonitis (p = 0.084).
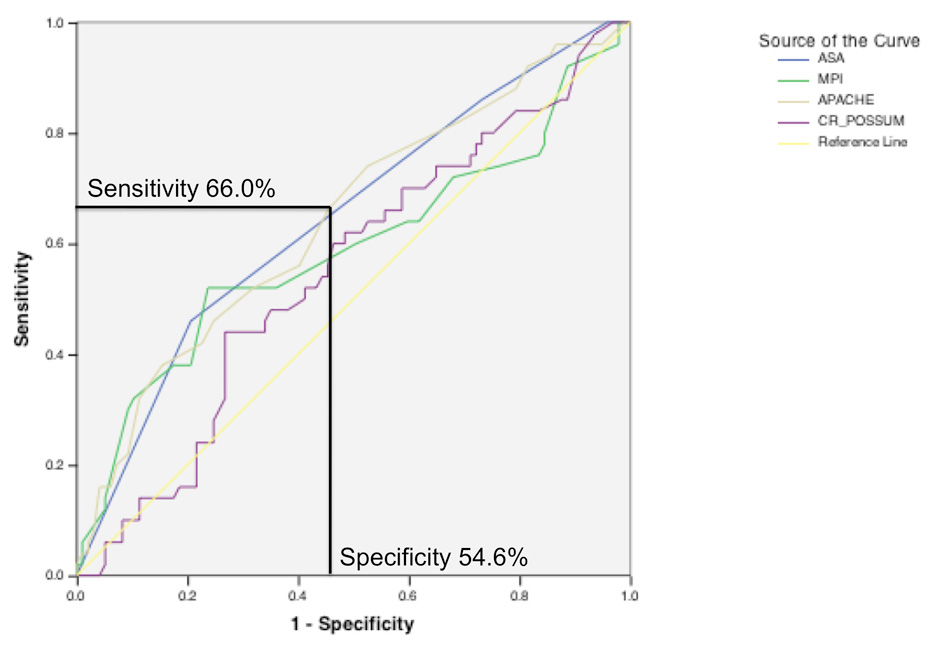
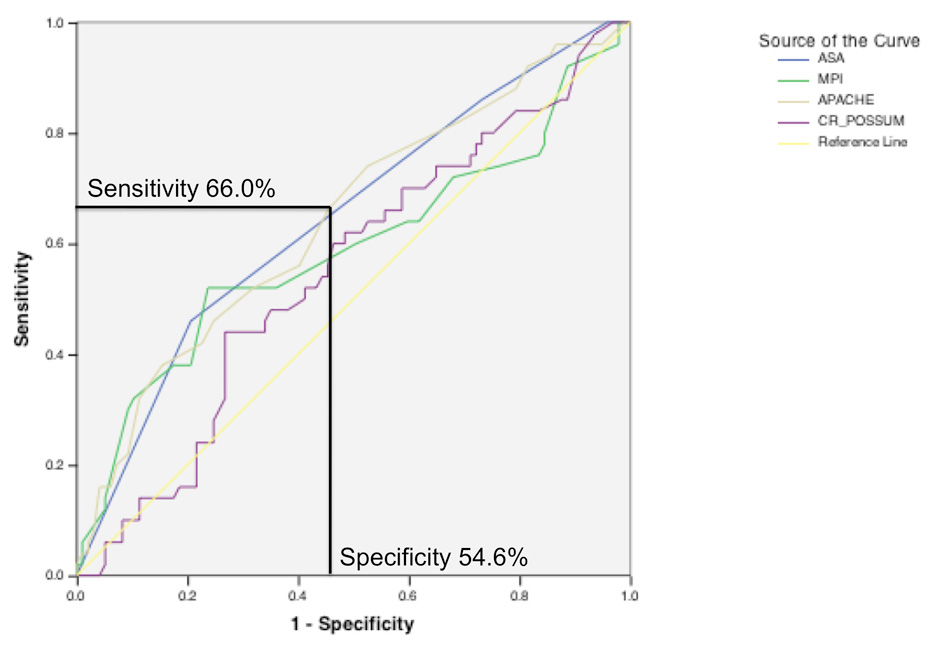
Figure 1
ROC curve. Sensitivity and 1-specificity for the prediction of a relaparotomy are plotted against each other for the different scores evaluated. At a cut-off score of 14 the APACHE II score shows a sensitivity and a specificity of 66.0%, and 54.6%, respectively.
Image-guided interventional drainage of intraabdominal abscesses may replace relaparotomies under certain circumstances. We therefore compared the group of patients with a relaparotomy and/or an interventional drainage (relaparotomy-intervention group, n = 55) with the group of patients necessitating neither intervention (no relaparotomy-intervention group, n = 92). Like the relaparotomy only group, the relaparotomy-intervention group had significantly higher APACHE II (p = 0.046), and ASA scores (p = 0.006), and a longer LOS (p <0.001) than the no relaparotomy-intervention group. Patients in the relaparotomy-intervention group had a trend towards higher mortality (29.1% vs. 17.4%; p = 0.096). No differences were found for MPI and for CR-POSSUM (p = 0.219, and p = 0.340, respectively), for age (p = 0.256), gender (p = 0.537), and aetiology of the secondary peritonitis (p = 0.108).
Planned relaparotomy
For 17 patients (11.6%), the surgeon decided during the index operation to perform a subsequent planned relaparotomy (PR). This relaparotomy actually was performed in 14 patients (9.5%); three patients died before the planned relaparotomy could be performed. The overall mortality rate in the PR group was 35.3%.
Relaparotomy on demand
If the surgeon plans a PR after the index operation, this decision will very infrequently be overruled by any scoring system. We therefore investigated whether scores might be helpful for the prediction whether a relaparotomy on demand (ROD) will be performed or not. For this analysis, all PR cases were excluded (n = 17), and patients with a ROD performed (n = 33) were compared to patients without ROD (n = 97). Patients with ROD had significantly higher APACHE II scores than patients without ROD; MPI and CR-POSSUM scores were not different between the two groups (table 3). ASA score (p = 0.046) and LOS (30 [3-153] vs. 15 days [1-97]; p <0.001) were found to be significantly higher in patients with ROD. There was a trend towards higher mortality in these patients, too (30.3% vs. 16.5%; p = 0.089). No differences were found for age, gender, and etiology of the secondary peritonitis. Similar results were found for the comparison of patients with a ROD and/or an interventional drainage to the group of patients necessitating neither intervention (data not shown).
Mortality
Overall in-hospital mortality was 21.8%. Non-survivors showed significantly higher MPI, APACHE II, and CR-POSSUM scores than survivors (table 4). Non-survivors also had a significantly higher ASA score (median 3 [range 2–4] vs. median 3 [range 1–4]; p = 0.003), were significantly older (median 79 [range 54–97] vs. median 69 years [range 21–93]; p = 0.001), and showed a significantly shorter LOS (10.5 [1–43] vs. 21 days [7–153]; p <0.001). Ischaemia as aetiology of secondary peritonitis was significantly more frequent among non-survivors (21.9%) than among survivors (6.1%; p = 0.023).
Sensitivity analysis
Sensitivity and specificity of the scores that showed significant correlation with the pertinent outcome variable (relaparotomy, ROD, or mortality) were analysed by ROC curve analysis. The respective median score of the entire patient population was used as cut-off value: 21, 14, and 31.8 for MPI, APACHE II, and CR-POSSUM, respectively. Sensitivity of APACHE II to predict relaparotomy or ROD was 66.0%, and 75.8%, respectively (table 5 and fig. 1). The corresponding specificity was 54.6%, and 54.6%, respectively. Again, MPI, APACHE II, and CR-POSSUM proved to be excellent predictors for mortality in the ROC curve analysis with the area under the curve ranging from 0.62 to 0.74. Sensitivity ranged from 62.5% to 78.1% (table 5). Specificity was 48.7%, 54.8%, and 55.7% for MPI, APACHE II, and CR-POSSUM, respectively.
|
Table 2: Patients with relaparotomies showed a significantly higher APACHE II score than patients without relaparotomies. |
| |
Relaparotomy
|
No relaparatomy
|
p
|
| MPI |
23 (9–43) |
21 (5–36) |
0.072 |
| APACHE II |
16 (5–33) |
13 (4–29) |
0.004 |
| CR-POSSUM |
33.0 (17.0–43.8) |
31.0 (14.0–46.9) |
0.319 |
| Values are medians with ranges in parentheses. |
|
Table 3: Patients with relaparotomies on demand (ROD) had a significantly higher APACHE II score than patients without ROD. |
| |
ROD
|
No ROD
|
p
|
| MPI |
20 (9–33) |
21 (5–36) |
0.719 |
| APACHE II |
17 (9–29) |
13 (4–29) |
<0.001 |
| CR-POSSUM |
34.3 (18.0–43.8) |
31.0 (14.0–46.9) |
0.198 |
| Values are medians with ranges in parentheses. ROD = relaparotomy on demand. |
|
Table 4: Non-survivors showed significantly higher MPI, APACHE II, and CR-POSSUM scores than survivors. |
| |
Non-survivors
|
Survivors
|
p
|
| MPI |
22 (5–33) |
21 (6–43) |
0.043 |
| APACHE II |
18 (11–33) |
13 (4–28) |
<0.001 |
| CR-POSSUM |
35.5 (18.0–46.9) |
30.9 (14.0–44.3) |
0.001 |
| Values are medians with ranges in parentheses. |
|
Table 5: Sensitivity. |
| |
Relaparotomy
|
ROD
|
Mortality
|
| MPI |
n/s |
n/s |
62.5% |
| APACHE II |
66.0% |
75.8% |
78.1% |
| CR-POSSUM |
n/s |
n/s |
75.0% |
| Sensitivity of the scores to predict any relaparotomy, a relaparotomy on demand (ROD), or mortality. n/s = not significant. |
Discussion
The present investigation provides suggestive evidence that the APACHE II score might be helpful in predicting the need for relaparotomies in patients with secondary peritonitis of colorectal origin. Patients with one or more relaparotomies had a significantly higher APACHE II score (p = 0.004) than patients without relaparotomy. Two other predictive scores evaluated, MPI and CR-POSSUM, did not show an association with the need for relaparotomies. Moreover, our data confirm previous observations that relaparotomies are frequently performed for secondary peritonitis of colorectal origin: more than one third of our patients received one or more relaparotomies. Finally, overall in-hospital mortality was found to be high; more than one fifth of patients did not survive.
Secondary peritonitis of colorectal origin has a considerable mortality. We found a median APACHE II score of 14 in our series, which corresponds to an expected (calculated) mortality rate of 18.6% [11]. This is very close to the observed mortality rate of 21.8%. Vermeulen and co-worker [12] described a 27% mortality rate in 200 patients with perforated diverticulitis. In a prospective multicentre study, Wacha et al. [13] analysed 355 patients with secondary peritonitis of any origin. While the overall mortality was already high (17%), secondary peritonitis of colorectal origin was the leading cause of death with a mortality rate of 20%. Different scores have been modeled to predict mortality for patients with peritonitis (e.g. MPI) [1], for patients in an intensive care unit (e.g. APACHE II) [2] or for patients undergoing colorectal surgery (e.g. CR-POSSUM) [3]. All three scores investigated in this study significantly and reliably predicted mortality (i.e. the outcome parameter they were designed for); sensitivity of the scores ranged from 62.5% to 78.1%. This observation underlines the robustness of the scores to predict mortality as well as the validity of our patients’ sample.
While the severity of the disease is mirrored by a high mortality rate and a high rate of relaparotomies or image-guided interventions, surgeons in clinical practice are often confronted with the question whether a relaparotomy is needed in a patient with secondary peritonitis of colorectal origin or whether this will only increase the surgical trauma and prolong the length of stay. As the need for a relaparotomy is closely related to the magnitude of the disease, we investigated in this study whether high MPI, APACHE II, and CR-POSSUM scores might be correlated with the need for relaparotomies. If our hypothesis holds true, these scores might facilitate the decision-making concerning an eventual relaparotomy. However, scores that are calculated at the time of the index operation (performed for the secondary peritonitis) and that heavily weigh parameters like patients’ characteristics and intraoperative findings (MPI and CR-POSSUM) were not predictive for the need for relaparotomies overall, for relaparotomies on demand (ROD) or for the combined outcome parameter relaparotomy and/or an interventional drainage (relaparotomy-intervention). This is in contrast to the study by Vermeulen et al. [12] who found a significant association of MPI with the need for reinterventions. In our study however, the APACHE II score, which uses physiologic parameters collected over a 24-hour period and a chronic health evaluation, fared much better than MPI and CR-POSSUM. A high APACHE II score was significantly associated with the need for any relaparotomy (p = 0.004), for ROD (p <0.001), and for relaparotomy-intervention (p = 0.046). A decision for a planned relaparotomy (PR) taken by a surgeon during the index operation will very infrequently be overruled; therefore, a reliable scoring system might be particularly helpful in equivocal cases, i.e. for the prediction whether a ROD should be performed or not. In our series, sensitivity of APACHE II for prediction of ROD was found to be very good (75.8%); APACHE II might therefore be helpful for the decision-making concerning an eventual ROD.
The high predictive value of scores capitalising on physiological parameters has previously been described. Van Ruler et al. [14] created a model to predict positive findings at relaparotomy for secondary peritonitis. Five out of six parameters in this model were postoperative (physiological) parameters. The authors therefore concluded that factors indicative of progressive or persistent organ failure during the postoperative period might be the best indicators. Paugam-Burtz and co-worker [15] retrospectively evaluated daily changes in the Sepsis-related Organ Failure Assessment (SOFA) score in 62 patients with postoperative peritonitis. SOFA is a physiological score quantifying the dysfunction of six organs [16]. Patients with relaparotomies were found to have persistently high SOFA scores over several days, while SOFA scores started to decrease on day 2 in patients that did not need relaparotomy [15]. Similarly, Koperna and Schulz [17] found significantly increased APACHE II scores in patients that had to undergo relaparotomy due to persisting intraabdominal infection. This study found slightly higher APACHE II scores in the relaparotomy group (average 20.7) than in our study (median 16), which is explained by the fact that patients with a “negative” relaparotomy (without intraoperative pathologic finding) were excluded from analysis in the publication by Koperna and Schulz. Consequently, the mortality rate was very high in the relaparotomy group (51%) [17]. Care must be taken when comparing publications only focusing on postoperative peritonitis to our patients’ sample, which included secondary peritonitis due to (postoperative) anastomotic leakage, but also due to perforated diverticulitis, ischaemia and other sources, as patients with postoperative peritonitis tend to have higher APACHE II and MPI scores [18].
There is considerable debate in the literature whether patients with secondary peritonitis should undergo PR or rather ROD. We did not attempt to analyse this issue in our series. However, recent publications have investigated this topic. In a multivariate analysis on 96 patients with postoperative peritonitis, Mulier et al. [19] described that failure to control the peritoneal infection and, specifically, failure to control the septic source was always fatal and associated with high APACHE II scores. They recommend a PR strategy whenever the source control is uncertain. A meta-analysis based on eight observational studies showed a (non-significant) lower in-hospital mortality for patients with ROD than for patients with PR [20]. A retrospective analysis of 278 consecutive patients with secondary peritonitis by the same group confirmed these results: patients on a ROD strategy had a significantly better in-hospital and long-term survival than patients with a PR. The choice of treatment strategy was found to be an independent predictor of survival, while APACHE II score and MPI failed to be predictive for long-term survival [8]. Finally, the Dutch Peritonitis Study Group recently published the first randomised clinical trial comparing PR versus ROD [21]. Two-hundred thirty-two patients with secondary peritonitis of any origin and an APACHE II score of ≥11 were randomly allocated to PR or ROD. Morbidity and mortality was not different in the two groups. However, patients in the ROD group had a significantly shorter LOS on the intensive care unit and in the hospital, and the medical costs were reduced by 23% in the ROD group [21]. Even though this study has been challenged based on statistical grounds [22], it is the only randomised trial evaluating this issue to date. Additional to this evidence in favour of ROD, practice patterns by many surgeons are in favour of ROD as well [23]. In light of the current tendency toward ROD rather than PR, and in light of the data presented in this paper, the APACHE II score might be particularly helpful in predicting the need for relaparotomies.
We would like to acknowledge the limitations of our study. First, it is a retrospective study. Scores can reliably be calculated retrospectively if all the pertinent information is available. If, infrequently, information on some parameters was missing, we assumed these parameters to be within the normal range. Thus, any “overscoring” was carefully avoided [9]. Therefore, our calculated scores are biased, if anything, in favour of “better” scores. For the CR-POSSUM score it has been shown that treating missing values as normal values will not influence the performance of the score [4]. Still, a prospective evaluation, preferably in a multicentre setting, is mandatory before the APACHE II score can be integrated into treatment algorithms. Second, out of a multitude of scores we had to limit our choice. However, care was taken to use exemplary scores focusing either on peritonitis (MPI) [1], on physiological parameters (APACHE II) [2] or on colorectal surgery in general (CR-POSSUM) [3]. Third, it has been shown that some scores require a calibration process when being transferred from one country to another (e.g. CR-POSSUM from the UK to the USA) [4]. For our country, this calibration process has not been performed for any of the scores utilised. However, we assume the bias from this effect to be minor, and if present, to be in the same direction for all three scores. Fourth, during the time period described only a minority of patients were treated with interventional drainage (5.4%). Nowadays interventional drainage is an established and increasingly performed procedure for localised secondary peritonitis.
Conclusions
Relaparotomies are frequently necessary for patients with secondary peritonitis of colorectal origin. The APACHE II score, which uses physiologic parameters collected over a 24-hour period and a chronic health evaluation, might be helpful in predicting the need for relaparotomies, especially in equivocal cases. The other investigated scores were not helpful in this respect. Therefore, the usefulness of the APACHE II score should be evaluated prospectively, and only afterwards should this score be integrated into algorithms describing the treatment of secondary peritonitis of colorectal origin to minimise the inherent morbidity and mortality of this disease.
References
1 Wacha H, Linder MM, Feldmann U, Wesch G, Grundlach E, Steifensand RA. Mannheim peritonitis index – prediction of risk of death from peritonitis: construction of a statistical and validation of an empirically based index. Theor Surg. 1987;1:169–77.
2 Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818–29.
3 Tekkis PP, Prytherch DR, Kocher HM, Senapati A, Poloniecki JD, Stamatakis JD, et al. Development of a dedicated risk-adjustment scoring system for colorectal surgery (colorectal POSSUM). Br J Surg. 2004;91(9):1174–82.
4 Senagore AJ, Warmuth AJ, Delaney CP, Tekkis PP, Fazio VW. POSSUM, p-POSSUM, and Cr-POSSUM: implementation issues in a United States health care system for prediction of outcome for colon cancer resection. Dis Colon Rectum. 2004;47(9):1435–41.
5 van Ruler O, Kiewiet JJ, Boer KR, Lamme B, Gouma DJ, Boermeester MA, et al. Failure of available scoring systems to predict ongoing infection in patients with abdominal sepsis after their initial emergency laparotomy. BMC Surg. 2011;11(1):38.
6 Basu A, Pai DR. Early elevation of intra-abdominal pressure after laparotomy for secondary peritonitis: a predictor of relaparotomy? World J Surg. 2008;32(8):1851–6.
7 Boermeester MA. Surgical approaches to peritonitis. Br J Surg. 2007;94(11):1317–8.
8 Lamme B, Boermeester MA, Belt EJ, van Till JW, Gouma DJ, Obertop H. Mortality and morbidity of planned relaparotomy versus relaparotomy on demand for secondary peritonitis. Br J Surg. 2004;91(8):1046–54.
9 Waydhas C, Nast-Kolb D, Ruchholtz S, Schweiberer L. Practical and theoretical limits of score systems. Unfallchirurg. 1994;97(4):185–90.
10 Anonymous. New classification of physical status. Anesthesiology. 1963;24:111.
11 http://www.sfar.org/scores2/apache22.htmleditor^editors.
12 Vermeulen J, Akkersdijk GP, Gosselink MP, Hop WC, Mannaerts GH, van der Harst E, et al. Outcome after emergency surgery for acute perforated diverticulitis in 200 cases. Dig Surg. 2007;24(5):361–6.
13 Wacha H, Hau T, Dittmer R, Ohmann C. Risk factors associated with intraabdominal infections: a prospective multicenter study. Peritonitis Study Group. Langenbecks Arch Surg. 1999;384(1):24–32.
14 van Ruler O, Lamme B, Gouma DJ, Reitsma JB, Boermeester MA. Variables associated with positive findings at relaparotomy in patients with secondary peritonitis. Crit Care Med. 2007;35(2):468–76.
15 Paugam-Burtz C, Dupont H, Marmuse JP, Chosidow D, Malek L, Desmonts JM, et al. Daily organ-system failure for diagnosis of persistent intra-abdominal sepsis after postoperative peritonitis. Intensive Care Med. 2002;28(5):594–8.
16 Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22(7):707–10.
17 Koperna T, Schulz F. Relaparotomy in peritonitis: prognosis and treatment of patients with persisting intraabdominal infection. World J Surg. 2000;24(1):32–7.
18 Bader FG, Schroder M, Kujath P, Muhl E, Bruch HP, Eckmann C. Diffuse postoperative peritonitis – value of diagnostic parameters and impact of early indication for relaparotomy. Eur J Med Res. 2009;14(11):491–6.
19 Mulier S, Penninckx F, Verwaest C, Filez L, Aerts R, Fieuws S, et al. Factors affecting mortality in generalized postoperative peritonitis: multivariate analysis in 96 patients. World J Surg. 2003;27(4):379–84.
20 Lamme B, Boermeester MA, Reitsma JB, Mahler CW, Obertop H, Gouma DJ. Meta-analysis of relaparotomy for secondary peritonitis. Br J Surg. 2002;89(12):1516–24.
21 van Ruler O, Mahler CW, Boer KR, Reuland EA, Gooszen HG, Opmeer BC, et al. Comparison of on-demand vs planned relaparotomy strategy in patients with severe peritonitis: a randomized trial. JAMA. 2007;298(8):865–72.
22 Farjah F, Flum DR. When not being superior may not be good enough. JAMA. 2007;298(8):924–5.
23 Lamme B, Boermeester MA, de Vos R, van Ruler O, van Till JW, Obertop H. Survey among surgeons on surgical treatment strategies for secondary peritonitis. Dig Surg. 2004;21(5-6):387–94; discussion 394–85.