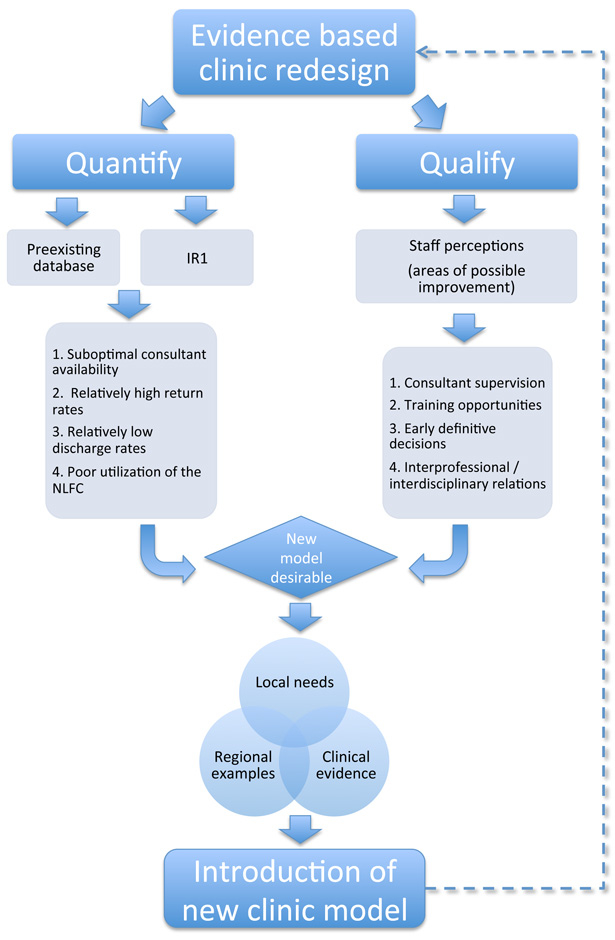
Figure 1
Implementation of new fracture clinic model using principles of evidence-based redesign.
DOI: https://doi.org/10.4414/smw.2012.13630
In 1991 the ‘New Deal’ [1] limited the maximum number of hours a junior doctor was permitted to work each week. By 2009, the European Working Time Directive (EWTD) further limited this to an average of 48 hours over a six-month period [2]. In addition, two rulings (Simap and Jaegerin) by the European Court of justice [3] effectively limited working (and training) patterns further by judging that time spent on call at a hospital counts as working time, whether or not any work is actually done. Compensatory rest to make up for missed rest periods must be taken as soon as the period of work ends, rather than at a later time. This in turn may reduce face-to-face contact time between trainee and trainer.
There are conflicting reports regarding the impact of the EWTD on patient care and medical training (table 1) [4–15]. An independent review on the impact of the EWTD on medical training chaired by Professor Sir John Temple in 2010 [16] concluded that in many healthcare settings changes are needed in the way services and training are delivered, to ensure that both are of a high quality. Reid [17] reiterated the importance of evaluating the impact of any such change in terms of its effect on the quality and safety of patient care.
Interprofessional education occurs when two or more professions learn about, from and with each other, to enable effective collaboration and improve health outcomes [18]. Interprofessional working involves professionals collaborating to work together more effectively to improve the quality of patient care. The World Health Organization and its partners recognise interprofessional collaboration in education and practice as an innovative strategy that will play an important role in mitigating the global health workforce crisis.
Traditionally, any member of the orthopaedic team, with varying seniority, can see new patients at the fracture clinic. In theory a supervisory system ensures junior doctors are supported and patients receive excellent care. In practice, however, this is not always the case, with trainees spending less than 5% of their time discussing patients with senior staff [19]. The traditional model leaves junior members of the team isolated in making clinical decisions, often with a perceived lack of support and with less than adequate opportunities for education. Although trainees frequently encounter problems, there is evidence that they frequently do not ask for help [20]. On a local level such problems resulted in several ‘near miss’ events. Buddeberg-Fischer and Stamm [21] highlighted that training should place a greater focus on the outpatient setting and that physicians should engage critically and to a greater extent with the continuous development of their profession.
Consultant-led case reviews have been central to several models of clinic redesign, resulting in reduced outpatient visits and/or improvements in trainee education [22–24]. We describe our model of the new-patient fracture clinic and how it can be used to help overcome obstacles in delivering education, in interprofessional care and in ultimately improving patient care, without additional funding.
| Table 1: Literature summary on the impact of the EWTD within the practical specialities. | |||
| Author(s) | Year | Study features | Impact of EWTD |
| Maxwell et al. [4] | 2010 | Retrospective review | Training opportunities reduced. Adverse impact on patient care. |
| Fernandez and Williams [5] | 2009 | Retrospective review | Reduction in trainee cases. |
| McIntyre et al. [6] | 2010 | Retrospective review | No effect on patient care. Increased sick leave amongst junior doctors. |
| Giles et al. [7] | 2010 | Review | EWTD may harm training. |
| Skipworth et al. [8] | 2008 | Survey | Reduced surgical exposure. Need for alternative training formats. |
| Tait et al. [10] | 2008 | Survey | Deterioration in training, patient care and quality of life. |
| West et al. [11] | 2007 | Survey | Negative impact on training. Equivocal change to quality of life. |
| Garvin et al. [9] | 2008 | Survey | Deterioration in training and patient care. Improved quality of life. |
| Sim et al. [12] | 2004 | Audit | Reduction in training lists and procedures. |
| Lim & Tsui [13] | 2006 | Logbook review | Exposure to operative surgery can be maintained. |
| Jameson et al. [14] | 2012 | Logbook review | No reduction in operative exposure. |
| Al Rawi and Spargo [15] | 2009 | Logbook review | No reduction in caseload. |
The current ‘new-patient’ fracture clinic redesign study was undertaken at Stirling Royal Infirmary, Scotland. The fracture clinic / trauma service of the Forth Valley Trust has a catchment population of approximately 300,000 patients. Stirling Royal has a large dynamic orthopaedic department with a strong emphasis on trauma care. We present our experience in the redesign of the new-patient fracture clinic, with the objective of improving patient care, trainee education, interprofessional relations and clinic efficiency. There were no conflicts of interest.
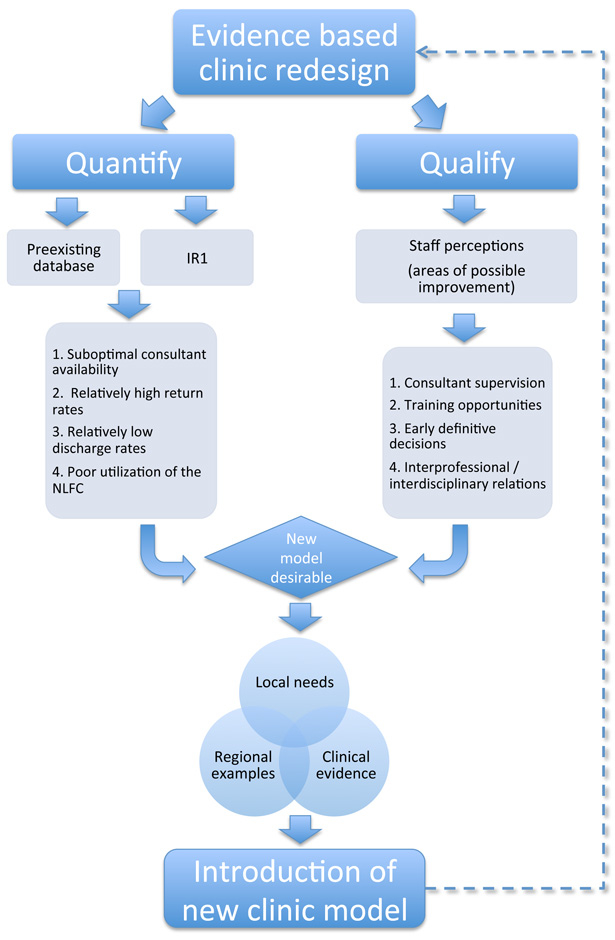
Figure 1
Implementation of new fracture clinic model using principles of evidence-based redesign.
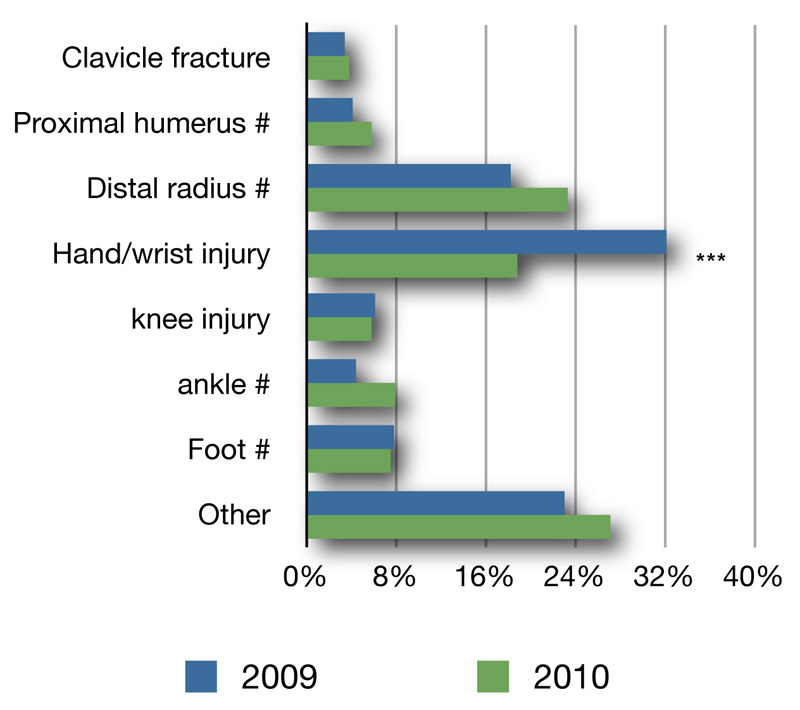
Figure 2
The 2009 & 2010 cohorts were case mix matched except for ‘hand / wrist injuries’. [*** = extremely significant, (p <0.001)].
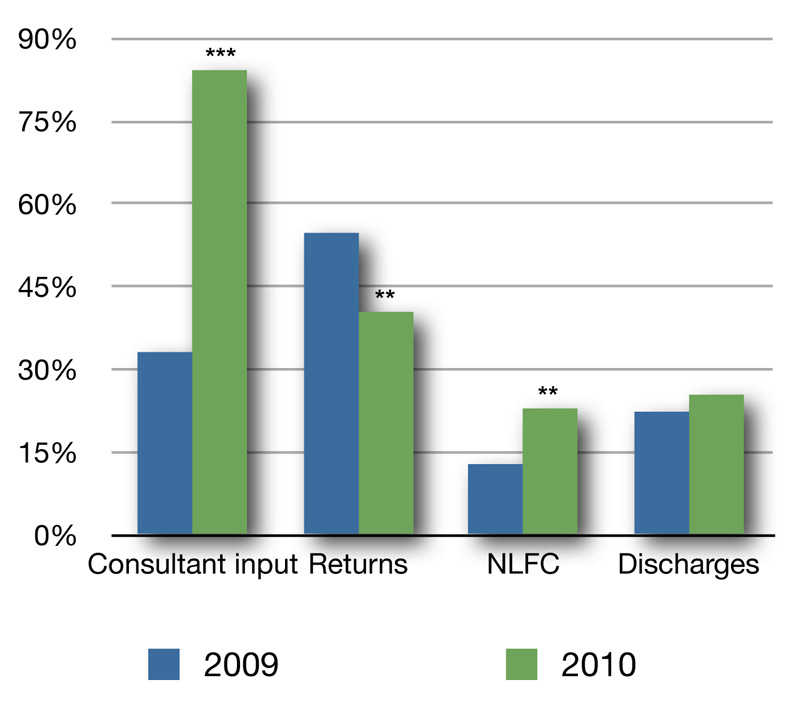
Figure 3
There were significant improvements in consultant input, use of the NLFC and a fall in return rates after the introduction of the new model of fracture clinic. Discharge rates increased, but did not reach significance. [NLFC = nurse-led fracture clinic; * = significant, (p <0.05); ** = very significant, (p 0.001–0.01); *** = extremely significant, (p <0.001)].
Using a process of evidence-based redesign (fig. 1), we gathered and analysed information to investigate existing conditions before introducing the new clinic model. 763 patients were reviewed over 8 weeks using the hospitals pre-existing database. We found relatively high return rates, low discharge rates and poor utilisation of nurse-led follow-up. This suggested that patients were being brought back to clinic unnecessarily and that our unit was not maximising outpatient opportunities.
Members of the interprofessional clinic team were informally interviewed to gauge opinion, identify problems and delineate potential improvements. Surprisingly, we discovered that senior nursing staff found it necessary to lodge several official IR1 reports [25] due to lack of consultant supervision at fracture clinic (concomitant clinical commitments). Retrospective data obtained through the freedom of information act [26] highlighted 8 IR1 reports in the year prior to fracture clinic redesign citing “delayed / non appearance of (consultant) staff”. Other issues included deteriorating trainee education, poor staff morale, strained interdepartmental relations and, most importantly, potential problems with patient care. Drawing on experience from other hospitals in the region and outpatient models in the literature [22–24], we redesigned our new-patient fracture clinic, implemented change and recorded our outcomes.
A consultant-led interprofessional pre-fracture clinic meeting was introduced to review all new outpatients referred with a musculoskeletal injury. Each patient’s case notes and radiographs were reviewed at a meeting prior to the new-patient fracture clinic. The on-call consultant chaired the meeting. Other roles include a ‘historian’ responsible for presenting the salient features from the case notes, a ‘PACS operator’ (Picture Archiving and Communications System) responsible for displaying the radiographs, and a ‘scribe’ to record the diagnosis, management plan and grade of physician suitable for reviewing each patient. The meeting is followed by standard patient consultations by a predetermined physician grade of sufficient seniority.
Adjuvants to efficacy include bar-code scanners to bring up x-rays on PACS and pre-labelling and attaching diagnosis / outcome sheets (appendix I) to each set of case notes prior to the meeting. The process takes approximately one minute per patient, but varies according to caseload. When the caseload is low, more time can be spent per case and the meeting takes on a heightened educational role, with formal questioning of trainees for example.
A particular team member can if required perform more than one role. The entire clinic team attends (nurses, auxiliary nurses, plaster technicians and doctors) as well as ER staff and medical / nursing students. The opinion of every member of the teams is respected and questions are encouraged (within daily time constraints).
301 consecutive patients attended the new-patient fracture clinic over a three-week period in the summer of 2010, compared to 346 consecutive patients during a three-week period exactly one year previously. Adequate data were available for 240 patients (80%) in 2010 and 296 patients (86%) in 2009. The attending physician collected data prospectively in 2010 by means of a pro forma immediately after each patient encounter. Data for the traditional fracture clinic model were recorded from a retrospective review of the case notes by one of the authors (K.C.). All patients reviewed by a consultant – or where there was evidence that a consultant’s opinion was sought – were deemed to have had consultant input. Complete data were available for all other outcome measures.
The proportion of cases where a consultant was involved in reaching a diagnosis and / or management plan was used as the primary outcome. Secondary outcomes including discharge rates, return rates and the use of the nurse-led fracture clinics (NLFC), for each clinical grade (junior trainee [≤specialist trainee registrar (StR) 2], senior trainee [≥ StR 3] or consultant) were also recorded. Analysis of the new clinic model in 2010 was carried out three months after it was introduced and established. Standard demographics including age, sex and reason for presentation were collected in both 2009 and 2010.
Eight orthopaedic trainees who attended both the old and new style clinics were assessed regarding their perception of the provision of education, support, staff morale & standards of patient care, before and after clinic redesign, using a Likert scoring system (where 1 represents the lowest possible score and 5 represents the highest score, appendix II) [27, 28]. Six ER personnel attending the redesigned fracture clinic completed a separate Likert questionnaire (appendix III). The quality of education provided and the degree to which it changed daily practice was determined. In addition, perception of improvements in interdisciplinary relations and intrusion into ER duties was ascertained. IR1 reports pertaining to the new-patient fracture clinic were analysed retrospectively by OM. IR1 data was obtained through the freedom of information act from the Forth Valley Trust for one year prior to and one year after the introduction of the new style clinic.
Statistical analysis of trainee Likert scores before and after the introduction of pre-fracture clinic meetings was performed using the Wilcoxon sign ranked test for repeated measure ordinal data between matched pairs. Fisher’s tests were used for categorical data. The Mann-Whitney U test was used to compare interval age groups, since although the data was non-parametric the distribution was similar between 2009 and 2010. Statistical analysis was carried out using graphpad prism version 5 (GraphPad Software, CA) and SPSS version 16.0 (SPSS Inc. Chicago, Illinois).
240 consecutive patients were reviewed in 2010 compared to 296 patients in 2009. The patients were matched in terms of age, gender and case mix, except for ‘hand / wrist injuries’ where there was a significant reduction in 2010 compared to the previous year (fig. 2). 95 cases (32%) were classified as ‘hand / wrist injuries’ in 2009 compared to 45 (19%) in 2010, (p <0.0005).

Figure 4
Emergency room staff regarded the pre-fracture-clinic meetings as highly educational to a point where it changed their practice, as well as improving interprofessional relations without impacting on their routine duties.
The proportion of cases receiving consultant input increased significantly from 33% in 2009 to 84% in 2010 (98 versus 202 patients, p <0.0001). The proportion of patients requiring physical review by a consultant fell by 21% (89 versus 22 patients, p <0.0001). Overall ‘return rates’ were reduced significantly by 14% (162 versus 97 patients, p = 0.013) and utilization of the nurse-led fracture clinic improved significantly by 10% (38 versus 55 referrals, p = 0.0028). The discharge rate improved from 22% in 2009 to 25% in 2010, but did not reach significance (66 versus 61 patients, p = 0.42; fig. 3).
There were significant improvements in median scores of staff perception of education from 2 (interquartile range 1.25–2.75) to 5 (4.25–5, p = 0.011), provision of senior support from 2 (2–3) to 5 (4–5, p = 0.017), morale from 4 (3–4) to 4 (4–4.75, p = 0.046) and overall perception of patient care from 3 (3–4) to 5 (4–5, p = 0.015). ER staff found the new style clinic was educational, practice-changing & improved interdisciplinary relations. Moreover, attendance at the pre-fracture clinic meeting did not interfere with their normal duties, as the meeting occurred in the morning when ER admissions are lowest (fig. 4).
No official IR1 reports were recorded during either three-week study period. However, there were eight reports for the year prior to the introduction of the pre-clinic meeting and no reports the following year. All eight incidents related to the delay or non-appearance of consultants.
The introduction of a pre-clinic meeting in the context of a new outpatient musculoskeletal trauma clinic is straightforward, beneficial and incurs no extra cost. We demonstrated increased consultant input and service efficiency, as well as significant improvements in staff support, morale, education and interprofessional relations.
After presenting our pilot data demonstrating shortcomings in the traditional clinic and suggesting improvement strategies, clinic staff were eager to engage in the new fracture clinic model. Initially, change in service required enthusiasm, organisation and leadership. To achieve ‘maintenance’ successfully both medical and non-medical staff should be involved as stakeholders, which also serves to identify broader clinical issues and positively impact patient care [29, 30]. Additionally, success of the pre-clinic meeting has initiated ‘spread’ to other units after national presentations.
Difficulties encountered in setting up and running the new clinic model included absent case notes prior to the clinic’s startup (clerical difficulties and patients presenting from overseas) and new referrals accepted during the clinic. Consequently, we were unable to review every patient at the pre-clinic meeting. Lack of leadership during the meeting can lead to over-running, for example, by spending a disproportionately long time teaching before a busy clinic. Additionally, lack of organisation prior to the meeting may lead to inefficient case presentations, x-ray retrieval and/or recording of outcomes.
Few comparative studies are available. A study from Leicester [22] (Leicester Royal Infirmary, Leicester, UK) demonstrated enhanced service efficiency and reduced outpatient visits when musculoskeletal trauma patients are reviewed by a consultant at a virtual clinic. Similarly, lower follow-up rates were observed in an otology clinic when comparing a consultant-led interactive case note discussion prior to clinic compared to no pre-clinic discussion [24]. Scott [23] demonstrated that postclinical meetings have the potential to increase the educational benefit of clinics as well as to provide direct benefits to patient care. A recent review article [29] illustrated that thirteen of fourteen studies reported at least one statistically significant improvement in outcome following interventions based on interprofessional collaboration
Our study combines prospective and retrospective data collection and therefore suffers from typical problems of retrospective review, specifically inability to obtain all case notes from 2009, and using clinic letters to identify whether consultant input was given. We accept that this is likely to underestimate consultant input in 2009, as not every occasion where a consultant opinion is sought will result in this being recorded. Patient demographics were well matched between the two groups after excluding seasonal variation by comparing two consecutive summers. Unfortunately, this made it difficult to match consultants in 2009 and 2010, which may introduce bias [31]. Two out of three consultant groups were paired. The new model has survived a departmental relocation to a new hospital and is now used in other hospitals in the West of Scotland, where plans are in place to audit its effectiveness and possibly to examine the savings to the health service.
Orthopaedic consultants in the UK must pass a stringent exit exam as well as successfully completing years of training in the generality of musculoskeletal trauma before obtaining a certificate of completion of training. Additionally, as a prerequisite for general medical council membership, all doctors are required to maintain and improve their standards and to maintain their knowledge and skills. Therefore, we used the ‘proportion of consultant input per clinic’ as our primary outcome measure and the gold standard in clinical care. It follows that by significantly increasing the level of consultant input we enhanced patient care. Secondary outcome measures, such as significant improvements in the perception of patient care and the reduction of IR1 reports serve to reinforce this message. However, as we did not directly measure improvements in patient care, a causal relationship cannot be stated. Further studies are therefore required to determine a causal relationship.
Unexpectedly, there was a significant fall in ‘hand and wrist’ referrals to the fracture clinic in 2010 compared to 2009. A large proportion of this heterogeneous group was composed of ‘clinical scaphoid fractures’ (clinically suspected scaphoid fracture in the absence of corroborating x-ray findings). At an early stage during the pre-clinic meetings it became evident than none of the ER advanced nurse practitioners (responsible for the majority of the referrals) could adequately examine a wrist (no advanced nurse practitioner could locate the scaphoid tubercle clinically, despite frequently documenting “tenderness of the scaphoid tubercle on palpation”). We believe that as a result of education delivered at the pre-clinic meeting, ER staff were better equipped to separate wrist sprains from likely clinical scaphoid fractures, and hence fewer inappropriate referrals were made.
We demonstrated a statistically significant fall in our overall return rates, as well as a significant increase in use of the NLFC service, in keeping with the literature [22–24]. We believe a consultant-led interprofessional service enhances the chances of patients receiving the correct treatment early in their management journey, resulting in return visits to the most appropriate clinic, fewer overall visits and better overall patient care. Reducing outpatient visits leads to less disruption to patient’s lives with less time off work, benefiting not only the patients and their families, but also the NHS and the economy as a whole. There was an overall trend towards increased discharge rates, although this did not reach significance. Amid the current pressures on medical training [16, 21] the pre-clinic meeting is an extremely valuable educational tool, not only for the trainee but also the trainer and the service provider, box 1 [23].
| Box 1 – Educational benefits of a pre–fracture clinic meeting. |
| TraineeExposure to high patient volume, with learning via repetition. Wider case mix allowing greater exposure to more unusual cases. Standardises care via repetition within interprofessional teams (more likely to develop evidence-based practice). Provide opportunity to voice management plans and receive feedback from trainer. Less need to interrupt trainer during clinic. Improve relation with trainer.TrainerBetter handle on clinic. Provides opportunity for teaching and trainee assessment. Can judge level of supervision required of trainee. Fewer interruptions during clinic. Improve relations with team / trainee. Time management, can see complex / difficult patients. Or may require spending less time at clinic. Can identify own training needs.Health serviceNeeds of trainees met. No additional cost. |
The redesigned fracture clinic model has significantly improved consultant input into the management of new fracture patients without the need for additional funding. In addition, we have demonstrated increased service efficiency and improvements in staff support, morale and education. We recommend this new outpatient clinic model as a tool for enhancing patient and trainee experiences in the face of current challenges to training and service provision.
› Appendix 1: Outcome sheets http://www.smw.ch/fileadmin/smw/images/SMW-13630-Appendix-1.pdf (PDF)
› Appendix 2: Fracture Clinic trainee Questionnaire http://www.smw.ch/fileadmin/smw/images/SMW-13630-Appendix-2.pdf (PDF)
› Appendix 3: Fracture Clinic Questionnaire - ER staff http://www.smw.ch/fileadmin/smw/images/SMW-13630-Appendix-3.pdf (PDF)
Acknowledgements: We thank Mr Lech Rymaszewski, consultant orthopaedic surgeon Glasgow Royal Infirmary, for his inspiration and all those who collected data and completed questionnaires, without which this study would not have been possible.
1 IDWL: Working Hours – the basics Available at: http://www.idwl.info/workinghours.html. Accessed 11/28/2011, 2011.
2 guichett – 32000L0034 – Available at: http://eur-lex.europa.eu/smartapi/cgi/sga_doc?smartapi!celexapi!prod!CELEXnumdoc&lg=en&numdoc=32000L0034&model=guichett. Accessed 11/28/2011, 2011.
3 EUR-Lex – 61998CJ0303 – EN Available at: http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=CELEX:61998J0303:EN:NOT. Accessed 11/28/2011, 2011.
4 Maxwell AJ, Crocker M, Jones TL, Bhagawati D, Papadopoulos MC, Bell BA. Implementation of the European Working Time Directive in neurosurgery reduces continuity of care and training opportunities. Acta Neurochir. 2010;152(7):1207–10.
5 Fernandez E, Williams DG. Training and the European Working Time Directive: a 7 year review of paediatric anaesthetic trainee caseload data. Br J Anaesth. 2009;103(4):566–9.
6 McIntyre HF, Winfield S, Te HS, Crook D. Implementation of the European Working Time Directive in an NHS trust: impact on patient care and junior doctor welfare. Clinical Medicine. 2010;10(2):134–7.
7 Giles JA. Surgical training and the European Working Time Directive: The role of informal workplace learning. Int J Surg. 2010;8(3):179–80.
8 Skipworth RJ, Terrace JD, Fulton LA, Anderson DN. Basic surgical training in the era of the European Working Time Directive: what are the problems and solutions? Scott Med J. 2008;53(4):18–21.
9 Garvin JT, McLaughlin R, Kerin MJ. A pilot project of European Working Time Directive compliant rosters in a university teaching hospital. Surgeon Journal of the Royal Colleges of Surgeons of Edinburgh & Ireland. 2008;6(2):88–93.
10 Tait MJ, Fellows GA, Pushpananthan S, Sergides Y, Papadopoulos MC, Bell BA. Current neurosurgical trainees’ perception of the European Working Time Directive and shift work. Br J Neurosurg. 2008 discussion 32-3;22(1):28–31.
11 West D, Codispoti M, Graham T, Specialty Advisory Board in Cardiothoracic Surgery of The Royal Colleges of Surgeons of Edinburgh & Ireland. The European Working Time Directive and training in cardiothoracic surgery in the United Kingdom. Surgeon Journal of the Royal Colleges of Surgeons of Edinburgh & Ireland 2007 quiz 85, 121;5(2):81–5.
12 Sim DJ, Wrigley SR, Harris S. Effects of the European Working Time Directive on anaesthetic training in the United Kingdom. Anaesthesia 2004;59(8):781–4.
13 Lim E, Tsui S. Impact of the European Working Time Directive on exposure to operative cardiac surgical training. Eur J Cardiothorac Surg. 2006;30(4):574–7.
14 Jameson S, Lamb A, Gupta S, Sher L, Wallace A, Reed M. The effect of the 48hr working week restrictions on trauma and orthopaedic operative experience: Analysis using the Elogbook. Journal of Bone & Joint Surgery, British Volume 2012;94-B(SUPP XXI):175-175.
15 Al-Rawi S, Spargo P. A retrospective study of anaesthetic caseload of specialist registrars following the introduction of new working patterns in the Wessex region*. Anaesthesia 2009;64(3):297–300.
16 Medical Education England Available at: http://www.mee.nhs.uk/our_work/work_priorities/review_of_ewtd__impact_on_tra.aspx. Accessed 11/28/2011, 2011.
17 Reid W. Developing and implementing organisational practice that delivers better, safer care. Quality and Safety in Health Care. 2004;13(4):247–8.
18 WHO | Framework for action on interprofessional education and collaborative practice Available at: http://www.who.int/hrh/resources/framework_action/en/. Accessed 11/28/2011, 2011.
19 Melgar T, Schubiner H, Burack R, Aranha A, Musial J. A time-motion study of the activities of attending physicians in an internal medicine and internal medicine-pediatrics resident continuity clinic Acad Med 2000;75(11):1138–43.
20 Green ML, Ciampi MA, Ellis PJ. Residents’ medical information needs in clinic: are they being met? Am J Med. 2000;109(3):218–23.
21 Buddeberg-Fischer B, Stamm M. The medical profession and young physicians’ lifestyles in flux: challenges for specialty training and health care delivery systems. Swiss Med Wkly. 2010;140:w13134.
22 Beiri A, Alani A, Ibrahim T, Taylor GJ. Trauma rapid review process: efficient out-patient fracture management. Ann R Coll Surg Engl. 2006;88(4):408–11.
23 Stott I. Teaching specialist trainees in the out-patient clinic. The Clinical Teacher. 2007;4(1):21–4.
24 Lo S, Eze N, Jonathan DA. The effect of consultant-led interactive pre-clinic case note review on follow-up rates of an otology outpatient clinic. Int J Clin Pract. 2005;59(2):256–8.
25 Clinical Governance – Patient Safety – How do I report an incident? Available at: http://www.clinicalgovernance.scot.nhs.uk/section5/how.asp. Accessed 11/28/2011, 2011.
26 Freedom of Information (Scotland) Act 2002 Available at: http://www.legislation.gov.uk/asp/2002/13/contents. Accessed 6/7/2012, 2012.
27 Likert R. A technique for the measurement of attitudes. Archives of Psychology. 2008;22(140):1–55.
28 Maurer TJ, Pierce HR. A comparison of Likert scale and traditional measures of self-efficacy. J Appl Psychol. 1998;83(2):324–9.
29 Martin JS, Ummenhofer W, Manser T, Spirig R. Interprofessional collaboration among nurses and physicians: making a difference in patient outcome. Swiss Med Wkly. 2010;140:w13062.
30 Schwarz D, Schwarz R, Gauchan B, Andrews J, Sharma R, Karelas G, et al. Implementing a systems-oriented morbidity and mortality conference in remote rural Nepal for quality improvement. BMJ Quality & Safety. 2011;20(12):1082–8.
31 Cosker TD, Ghandour A, Naresh T, Visvakumar K, Johnson SR. Does it matter whom you see? – a fracture clinic audit. Ann R Coll Surg Engl. 2006;88(6):540–2.
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article was reported.
Authors’ contribution: OM has given the idea, designed the study, analysed data, undertaken data gathering, and drafted the manuscript. KC has undertaken data gathering and revised the manuscript. AM has participated in designing the study and revised the manuscript. JB has participated in designing the study and undertaken data gathering