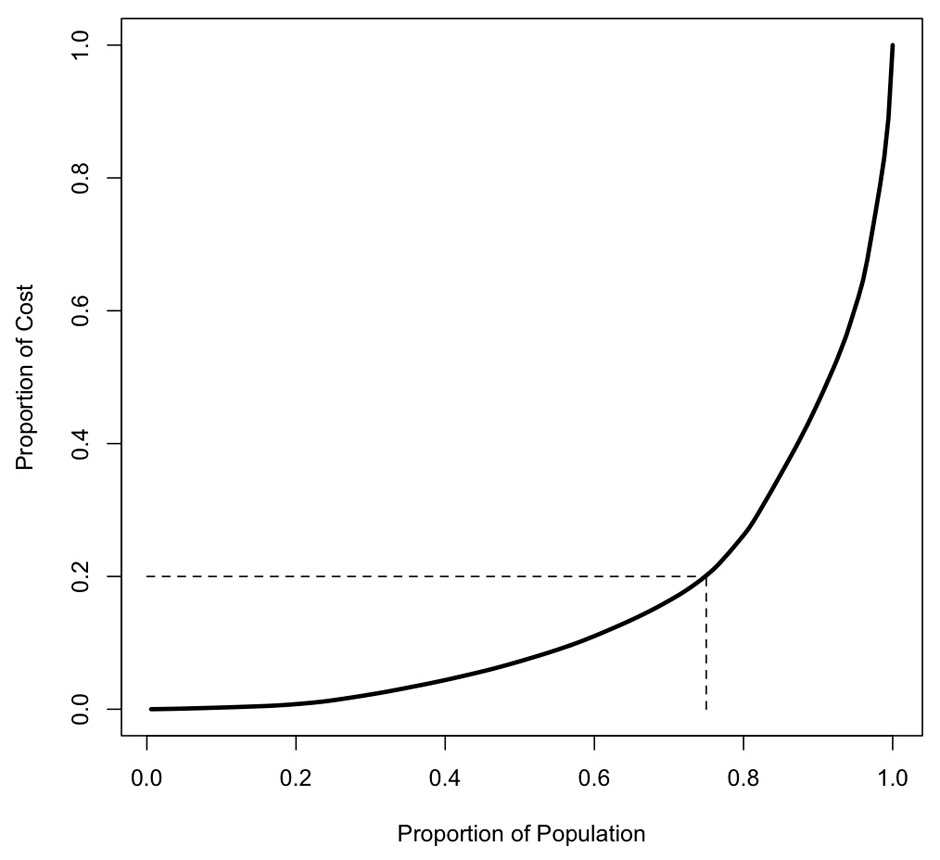
Figure 1
Concentration curve of direct medical costs of suicide attempts (n = 176).
DOI: https://doi.org/10.4414/smw.2012.13648
Every year, nearly one million people commit suicide worldwide, and suicide is among the 20 leading causes of death [1]. International health programmes such as the WHO programme “SUPRE” [2] have set mental health and suicide prevention as their priority. Data on completed suicides are widely available and indicate a substantial loss of potential years of life [3, 4]. However, data on attempted suicide are scarce, although medically, socially, ethically and economically significant. Suicide attempts are estimated to outnumber suicides by 10 to 20 times [5]. International prevalence rates for suicide attempts vary between 0.4% and 4.2% [6], suggesting that suicide attempts might incur considerable costs [7, 8].
Compared to other European countries, Switzerland has an above-average suicide rate. The lifetime prevalence of suicide attempts in Zurich, Switzerland’s most populous canton/city, was found to be 3.8% in 20–30 year olds (5.4% women, 2.1% men; [9]), while surveys among Swiss adolescents found a lifetime prevalence rate of 3.0% [10]. Based on records of registered suicide attempts in Bern, Switzerland’s capital, the total number of suicide attempts per year was estimated to be at least 10 000 for Switzerland as a whole [11]. The actual number of suicide attempts including non-registered cases is around 15 000 to 25 000 according to conservative estimates [12], suggesting a lifetime prevalence of about 10%. Suicide attempts are more common in women [13]. Prevalence rates for Bern between 1989 and 1995 were 160/100 000 in women and 100/100 000 in men [12].
Few data are available regarding the associated cost structure. Published studies focus on the costs of completed suicides [14, 15], which create indirect rather than direct costs resulting mainly from lost production. Direct costs, e.g. attributable to medical care, transportation, autopsy or funeral services, are of minor significance. Data available on suicide attempts show a reverse pattern [16, 17]. A study commissioned by the government of New Zealand [18] assessed both the financial and social costs of completed and attempted suicides. Regarding completed suicides, costs were dominated by lost productivity with 153.8 million Swiss francs (CHF) spent, and only a small fraction was attributable to direct costs (~CHF 3.6 million). For attempted suicides, the costs of medical care were approximately 1.5 times higher (~CHF 14.6 million) than those accrued due to lost production (~CHF 10 million). This shows that in the case of suicide attempts the main cost driver is direct medical cost. These findings are supported by a study conducted in Ireland [17], which comes to the conclusion that direct medical cost due to suicide attempts were around CHF 24.3 million in 2002, whereas the indirect cost summed up to only CHF 10.9 million. This research underlines the principal role of direct costs in the economic impact of suicide attempts. Therefore an assessment of the direct medical costs is a first step toward gaining a comprehensive understanding of the cost structure of attempted suicides. The identification of patient characteristics associated with high costs could provide starting-points for cost-effective prevention measures. Aim of this retrospective cost-of-illness study was to identify from a health services perspective the annual cost of attempted suicide of the Basel cohort of the WHO/EURO Multicentre Study on Suicidal Behaviour for the year 2003.
We conducted a cost-of-illness-study with retrospective analysis of direct medical costs for those suicide attempters registered in the WHO/EURO Multicentre Study on Suicidal Behaviour in Basel in 2003. Information on costs and patient characteristics were linked to identify factors influencing the cost structure of attempted suicide.
The canton Basel-City comprises Switzerland's third most populous city and two surrounding municipalities. The age distribution of the population in Basel and Switzerland, respectively, was 17.2% and 22.9% of citizens up to 19 years of age, and 21.0% and 15.4% of citizens aged 64 years and more. In Basel-City the proportion of individuals with a history of migration was higher than in the general Swiss population with 30.3% vs. 21.1%. The gender ratio, educational background, the labor force participation rate and the unemployment rate of Basel were approximately similar [19].
The University Hospital (UH), including a psychiatric crisis intervention ward, and the University Psychiatric Hospital (UPH) are the major medical service providers of the region with a mainly urban population and a catchment area of approximately 187 000 people in 2003 [19]. Approximately 50% of suicide attempters are treated in outpatient care mandated by the participating clinics, while those patients suffering from ongoing severe suicidal ideation following attempted suicide are typically treated in inpatient care.
The WHO/EURO Multicentre Study on Suicidal Behaviour collected data on individuals who attempted suicide in Basel in 2003. Inclusion criteria were attempted suicide as defined by the WHO/EURO Study (for details see [20]) and age 18 years and above. Parasuicide was defined as “an act with nonfatal outcome, in which an individual deliberately initiates a non-habitual behaviour that, without intervention from others, will cause self-harm, or deliberately ingests a substance in excess of the prescribed or generally recognised therapeutic dosage, and which is aimed at realising changes which the subject desired via the actual or expected physical consequences” [1, 8]. The definition includes acts that are interrupted before actual self-harm occurs, such as the behaviour of a person who lies across railway tracks with the intention of being run over by a train, but is rescued before the train arrives. Self-harmful acts by people who do not understand the meaning or consequences of their own actions were excluded. Repeated deliberate self-harm with the intention to reduce stress such as for instance habitual cutting, e.g., by patients suffering from Borderline personality disorder, were excluded as well. The terms “parasuicide” and “suicide attempt” are used interchangeably in this paper. In addition to socio-demographic variables, details on suicide attempts, methods according to ICD-10 X-Code [21], treatment and clinical psychiatric diagnoses were recorded.
For statistical analysis, we classified the variables of the WHO/EURO Study as follows: Age was categorised into three groups (18–24 years, 25–64, 65 and above), chosen to reflect the different stages in the social and working life of patients. Categories of suicide attempt methods ICD-10 X60–X69, including self-poisoning, were subsumed in the category “soft method”; X70-X84, including acts such as hanging, cutting, running into traffic, jumping, burning or drowning, were labeled “hard methods” [22]. Attempted suicides were also classified according to underlying intentions. Patients expressing a profound death wish were subsumed under the variable “lethal intention”. Parasuicidal gestures and pauses, deliberate self-harm or overdoses due to dependency were classified as “non-lethal intention”. ICD-10 diagnostic categories F5 and F6 were merged due to the low case numbers.
The local ethics committee approved both the WHO/EURO Multicentre Study on Suicidal Behaviour as well as our study and declined the necessity of obtaining informed consent.
We identified 195 participants fulfilling the inclusion criteria. Of these, 15 were dropped due to missing data regarding costs and 4 were dropped due to supplementary insurance (which could otherwise distort results due to differences in accounting methods). Table 1 shows the characteristics of the remaining 176 participants, which also represent the basis for the calculation of total cost. For the logistic regression, only 161 participants were included, while 15 were excluded due to missing data. The characteristics of the excluded participants did not differ significantly from those included in the logistic regression.
There is a lack of official statistics on suicide attempts in Switzerland. Therefore, to assess representativeness of our sample, we used data published on monitoring of suicidal behaviour in the catchment area of Bern covering the years 2004 until 2010 [23], permitting comparison of several sample characteristics, although we did not conduct any statistical tests. Mean age was similar with 38.9 in Basel vs. 37.4 in Bern. There was a slightly higher proportion of women in Basel with 68% compared to Bern with 56.6%. In Bern, 56.7% had a partner vs 58% in Basel. Of the Basel group, 44% had a history of migration vs. 24% of the Bern group. This difference may be partly explained with the overall higher percentage of individuals with a history of migration in Basel with roughly 10%. Bern had 44% of repeaters vs 50% in Basel and soft methods were slightly higher in Basel with 73% vs Bern with 64.2%. Further comparisons cannot be made due to lack of data but we believe that the underlying dataset can be considered fairly representative for Switzerland regarding the main variables.
| Table 1: Sample characteristicsa of the WHO/EURO-study (n = 176). | |||
| Characteristic | n | % | |
| Age in years (mean, SD) | 38.9 ± 17.6 | ||
| Gender | |||
| Female | 119 | 68 | |
| Male | 57 | 32 | |
| Occupation | |||
| In education | 17 | 10 | |
| Full occupation | 45 | 26 | |
| At home | 29 | 16 | |
| Retirement | 17 | 10 | |
| Invalidity pension | 57 | 32 | |
| Partner | |||
| Yes | 70 | 40 | |
| No | 102 | 58 | |
| History of migration | |||
| Yes | 70 | 40 | |
| No | 99 | 56 | |
| Education | |||
| More than 9 years | 76 | 43 | |
| Up to 9 years | 78 | 44 | |
| Diagnostic group (ICD-10) | |||
| F1 | 18 | 10 | |
| F2 | 17 | 10 | |
| F3 | 68 | 39 | |
| F4 | 49 | 28 | |
| F5/6 | 18 | 10 | |
| Repeater | |||
| Yes | 88 | 50 | |
| No | 81 | 46 | |
| Method of suicidal actionb | |||
| Hard | 47 | 27 | |
| Soft | 128 | 73 | |
| Intentionc | |||
| Lethal | 89 | 51 | |
| Non-lethal | 86 | 49 | |
| Treatment on ICU (intensive care unit) | |||
| Yes | 27 | 15 | |
| No | 149 | 85 | |
| a Percentages not adding up to 100 are due to missing information. b Soft methods according to ICD-10 X60-X69, including self-poisoning; hard methods ICD-10 X70-X84, including hanging, cutting, running into traffic, jumping, burning or drowning. c Intention of dying as opposed to parasuicidal gestures and pauses, deliberate self-harm or overdoses due to dependency. | |||
We assessed all direct medical costs for psychiatric and somatic care on inpatient or outpatient level by the participating hospitals following each suicide attempt occurring between 1 January and 31 December 2003, for a period of 12 months. Costs of inpatient and outpatient care were identified separately for each case by the hospitals’ financing and controlling departments. Cost items included employee time and the cost of medication and diagnostics.
Treatments delivered in the UH are given a specific case number that we used to identify associated costs. For the UPH, all hospitalisations initiated within one week of a suicide attempt were included. We checked rehospitalisations initiated within four weeks of discharge from a hospitalisation due to suicide attempt by studying patient records and included costs in the data set in case of an ongoing suicidal crisis. We applied the same inclusion procedure to all following hospitalisations. In a second step, costs of each hospitalisation were calculated using the hospital’s accounting system. If patients made repeated suicide attempts, during or after a hospitalisation, we allocated costs by separating the treatment costs according to the date of suicide attempt and therefore treated each suicide attempt as a different case.
Outpatient care was only included for subjects not already in treatment at the time of the attempt and when it was performed in the UH or UPH. We assumed that the outpatient treatment was initiated as a consequence of the suicide attempt, and that costs were directly attributable. The first outpatient appointment had to take place within two weeks of the suicide attempt in order to be included in the costs.
The clinics used for this study collaborate closely in the care of suicide attempters, and referrals between both clinics were common. Of the sample, 17 were treated exclusively in the UH; 80 only in the UPH; and 79 in both hospitals. Thirty-five patients were treated on the psychiatric crisis intervention ward of the UH.
The close cooperation of the two clinics might have produced the problem of double accounting. The respective items were identified on the basis of billing dates and included only once in the overall cost.
Statistical analysis was conducted using the “R” environment (version 2.9.0). To identify factors influencing the cost of suicide attempts, we initially compared the median cost per case across categories within potentially relevant variables. We used the Mann–Whitney U-Test or the Kruskal-Wallis-Test at the significance level of 5% to establish whether statistically significant differences exist. The exclusion of outliers had no influence on the results.
In health economics analysis, a highly skewed distribution of treatment costs is a common phenomenon. To analyse the concentration of the total costs in our sample, we calculated the Gini-coefficient [24]. This measure represents the dispersion of costs across patients. A coefficient of zero would imply that treatment costs are the same for all patients. A value of one on the other hand would indicate that one single person incurs all costs. We then calculated a cost-concentration curve, which in turn informed the logistic regression analysis of the probability of being a high-cost case.
Treatment of suicide attempters in the two main Basel-City hospitals in 2003 cost approximately CHF 3,373,025 (the exchange of US dollars to Swiss francs was 1.24 on 31 December 2003). The largest part (CHF 2,730,757; ~81%) was attributable to treatments in the UPH. Only approximately one fifth of the costs (CHF 642,268; ~19%) was caused by treatment in the UH. Table 2 shows the costs per day and the departments involved. Mean and median cost per case was 19,165 CHF (SD = 38,052) and 6,108 CHF (interquartile range [3,011; 17,311]), respectively. Table 3 shows indicators of cost per case.
A report by the Swiss Federal Office of Public Health [12] estimated that about 10 000 of a total of 15 000–25 000 suicide attempts in Switzerland entail medical treatment. Based on this estimate and the mean cost per case, the extrapolated direct medical costs for the treatment of suicide attempts in Switzerland amounted to 191 million CHF in 2003.
| Table 2: Treatment frequencies and costs in Swiss francs (CHF) by inpatient and outpatient status. | |||||
| Hospital | Number of days | Cost/day (CHF) | Total cost (CHF) | % of Total inpatient cost | |
| University hospital (UH) inpatient | |||||
| Surgical | 34 | 1,663 | 56,538 | 2 | |
| Internal medicine | 89 | 1,239 | 110,253 | 3 | |
| Intensive care unit | 78 | 2,055 | 150,048 | 5 | |
| Psychiatric | 227 | 1,079 | 239,608 | 7 | |
| University Psychiatric Hospital (UPH) Inpatient | 5,098 | 536 | 2,730,757 | 83 | |
| Inpatient total | 5,526 | 595 | 3,287,203 | 97a | |
| Number of cases | Cost/case (CHF) | Total cost (CHF) | % of total outpatient cost | ||
| UH Outpatient | |||||
| Surgical | 21 | 900 | 18,907 | 22 | |
| Internal nedicine | 78 | 562 | 43,850 | 51 | |
| Other | 17 | 584 | 9,928 | 12 | |
| Psychiatric | 27 | 487 | 13,137 | 15 | |
| Outpatient Total | 143 | 600 | 85,822 | 3a | |
| a Percentage of total costs (inpatient plus outpatient). | |||||
| Table 3:Indicators of per person cost. | ||||||
| Variable | Mean | SD | Median | 1st quartile | 3rd Quartile | pa |
| Age | 0.000 | |||||
| 18–24 | 10,892 | 21,703 | 4,076 | 842 | 8,266 | |
| 25–64 | 19,818 | 44,737 | 6,362 | 3,203 | 15,013 | |
| 64 and above | 32,591 | 26,282 | 28,122 | 13,469 | 41,536 | |
| Methodb | 0.015 | |||||
| Hard | 28,907 | 59,197 | 9,141 | 3,805 | 36,363 | |
| Soft | 14,963 | 25,945 | 5,112 | 2,141 | 11,612 | |
| Method by ICD-10 X-code | 0.006 | |||||
| X60 intentional self-poisoning by and exposure to nonopioid analgesics, antipyretics and antirheumatics | 5,134 | 7,654 | 3,519 | 1,624 | 4,450 | |
| X61 intentional self-poisoning by and exposure to antiepileptic, sedative-hypnotic, antiparkinsonism and psychotropic drugs, not elsewhere classified | 17,399 | 27,293 | 6,127 | 3,175 | 20,079 | |
| X62 intentional self-poisoning by and exposure to narcotics and psychodysleptics [hallucinogens], not elsewhere classified | 17,849 | 24,587 | 8,334 | 5,634 | 20,550 | |
| X63 intentional self-poisoning by and exposure to other drugs acting on the autonomic nervous system | 19,482 | 42,777 | 5,444 | 3,800 | 6,942 | |
| X64 intentional self-poisoning by and exposure to other and unspecified drugs, medicaments and biological substances | 6,528 | NAc | 6,528 | NA | NA | |
| X65 intentional self-poisoning by and exposure to alcohol | 8,476 | NA | 8,476 | NA | NA | |
| X66 intentional self-poisoning by and exposure to organic solvents and halogenated hydrocarbons and their vapours | 2,370 | NA | 2,370 | NA | NA | |
| X70 intentional self-harm by hanging, strangulation and suffocation | 84,068 | 118,840 | 35,414 | 23,153 | 50,037 | |
| X71 intentional self-harm by drowning and submersion | 412 | 99 | 412 | 377 | 447 | |
| X76 intentional self-harm by smoke, fire and flames | 4,540 | 4,098 | 3,198 | 2,240 | 6,170 | |
| X78 intentional self-harm by sharp object | 16,095 | 22,110 | 7,955 | 3,580 | 16,327 | |
| X79 intentional self-harm by jumping or lying before moving object | 15,749 | 19,820 | 7,844 | 5,055 | 18,538 | |
| X80 intentional self-harm by jumping from a high place | 21,850 | 19,413 | 16,012 | 6,595 | 37,396 | |
| X83 intentional self-harm by other specified means | 19,365 | 25,583 | 19,365 | 10,320 | 28,410 | |
| Not specified | 15,102 | NA | 15,102 | NA | NA | |
| Diagnostic group (ICD 10) | 0.000 | |||||
| F1 | 11,908 | 14,310 | 6,370 | 4,882 | 11,996 | |
| F2 | 58,800 | 95,536 | 11,402 | 7,231 | 55,289 | |
| F3 | 21,615 | 29,237 | 8,451 | 3,189 | 32,568 | |
| F4 | 6,320 | 9,105 | 4,098 | 751 | 6,353 | |
| F6 | 13,531 | 15,976 | 7,104 | 4,222 | 9,281 | |
| Intentiond | 0.000 | |||||
| Lethal | 28,046 | 49,047 | 9,677 | 48,767 | 37,099 | |
| Non-lethal | 9,200 | 17,518 | 4,076 | 763 | 8,266 | |
| Gender | 0.003 | |||||
| Male | 27,106 | 55,559 | 9,128 | 4,877 | 27,596 | |
| Female | 14,723 | 25,147 | 4,870 | 1,735 | 12,430 | |
| History of migration | 0.000 | |||||
| Yes | 13,772 | 44,015 | 4,114. | 1,276 | 91,334 | |
| No | 23,054 | 34,244 | 8,476 | 4,096 | 35,762 | |
| Intensive care | 0.007 | |||||
| Yes | 27,432 | 34,424 | 9,878 | 6,132 | 40,348 | |
| No | 17,157 | 38,570 | 5,140 | 2,370 | 12,818 | |
| a P-value of Mann-Whitney U-Test (for 2 groups) or of Kruskal-Wallis-Test (for 3 or more groups). b Soft methods according to ICD-10 X60-X69, including self-poisoning; hard methods ICD-10 X70-X84. c Only one case, standard deviation cannot be calculated. d Intention of dying as opposed to parasuicidal gestures and pauses, deliberate self-harm or overdoses due to dependency. | ||||||
The comparison of cost medians yielded significant differences for the following variables: gender, age, method of suicide, diagnosis, suicide intention, history of migration and treatment in the intensive care unit. The comparison of cost medians is shown in Table 3.
Table 4 displays direct psychiatric and somatic cost by method of suicide attempt. Because of low case numbers, we abstained from calculation of statistical tests, with the exception of category X61, where somatic costs where significantly higher than psychiatric costs (p = 0.012 from Mann-Whitney U-Test).
| Table 4: Direct psychiatric and somatic cost by method (ICD-10 X code) of suicide attempt. | ||||||||||
| Method | Psychiatric, n = 176 (p = 0.035 a ) | Somatic, n = 156 (p = 0.17 a ) | ||||||||
| Mean | SD b | Median | IQR c | n | Mean | SD b | Median | IQR c | n | |
| X60 intentional self-poisoning by and exposure to nonopioid analgesics, antipyretics and antirheumatics | 2,643 | 7,864 | 0–1,025 | 23 | 2,491 | 2,277 | 1,537 | 696–4,115 | 23 | |
| X61 intentional self-poisoning by and exposure to antiepileptic, sedative-hypnotic, antiparkinsonism and psychotropic drugs, not elsewhere classified | 13,513 | 26,905 | 254 | 0–16,111 | 90 | 4,115 | 4,142 | 3,505 | 730–5,322 | 85 |
| X62 intentional self-poisoning by and exposure to narcotics and psychodysleptics [hallucinogens], not elsewhere classified | 8,294 | 11,797 | 3,714 | 2,013–9,995 | 4 | 9,555 | 12,807 | 4,620 | 3,531–10,645 | 4 |
| X63 intentional self-poisoning by and exposure to other drugs acting on the autonomic nervous system | 17,463 | 43,363 | 1,753 | 0–5,353 | 8 | 2,308 | 2,409 | 569 | 472–4,132 | 7 |
| X64 intentional self-poisoning by and exposure to other and unspecified drugs, medicaments and biological substances | 3,432 | NAd | 3,432 | NA | 1 | 3,096 | NA | 3,096 | NA | 1 |
| X65 intentional self-poisoning by and exposure to alcohol | e | NA | NA | 1 | 8,476 | NA | 8,476 | NA | 1 | |
| X66 intentional self-poisoning by and exposure to organic solvents and halogenated hydrocarbons and their vapours | 1,785 | NA | 1,785 | NA | 1 | 585 | NA | 585 | NA | 1 |
| X70 intentional self-harm by hanging, strangulation and suffocation | 81,036 | 120,736 | 35,414 | 11,856–49,565 | 9 | 6,822 | 12,047 | 1,169 | 377–7,613 | 4 |
| X71 intentional self-harm by drowning and submersion | NA | NA | 2 | 412 | 99 | 412 | 377–447 | 2 | ||
| X76 intentional self-harm by smoke, fire and flames | 1,184 | 1,292 | 991 | 496–1,777 | 3 | 3,356 | 5,013 | 636 | 463–4,889 | 3 |
| X78 intentional self-harm by sharp object | 13,651 | 22,358 | 1,849 | 0–14,718 | 19 | 2,902 | 2,469 | 2,335 | 1,158–3,619 | 16 |
| X79 intentional self-harm by jumping or lying before moving object | 15,112 | 20,375 | 7,664 | 4,508–18,269 | 4 | 1,273 | 1,290 | 1,273 | 817–1,729 | 2 |
| X80 intentional self-harm by jumping from a high place | 12,749 | 15,192 | 8,101 | 450–19,563 | 8 | 10,401 | 19,898 | 2,375 | 2,035–5,107 | 7 |
| X83 intentional self-harm by other specified means | 17,953 | 23,586 | 17,953 | 9,614–26,292 | 2 | 1,412 | 1,997 | 1,412 | 706–2,118 | 2 |
| Not specified | 1,360 | NA | 1,360 | NA | 1 | 13,742 | NA | 13,742 | NA | 1 |
| a P-value of Kruskal-Wallis-test. b Standard deviation. c Interquartile range. d Only one case, standard deviation cannot be calculated. e A value of 0 can occur, when a patient is referred from one clinic to another but is discharged on the same day. In this case, costs are only allocated to the primary treatment to avoid double billing. | ||||||||||
In our sample, the value of the Gini-coefficient is 0.69. This suggests that the majority of patients incurred low or moderate treatment costs, whereas only a relatively small proportion of patients incurred a large proportion of total costs. Figure 1 shows the cost concentration curve. The slope of the curve increases steeply after the third quartile. About 80% of costs are caused by only 20% of the study population. This strong concentration implies that the prevention of relatively few suicide attempts could reduce the majority of costs. We were therefore interested in identifying what variables influence the probability of making a patient become one of the few high-cost cases rather than assessing the average effect of certain patient characteristics. Consequently we conducted a logistic regression analysis to identify the variables influencing the likelihood of a suicide attempt falling in the high-cost category. The cut-off point between “low-cost cases” and “high-cost cases” was set at the third quartile. This point was chosen because the increase in the slope seems to be highest around this quartile. We did not try to calculate an optimal cut-off value because using such a method could seriously bias the resulting estimates [25]. However, we did check whether our results are robust to the alteration of the cut-off value. For cut-off values between the 7th and 8th decile, the results are qualitatively very similar.
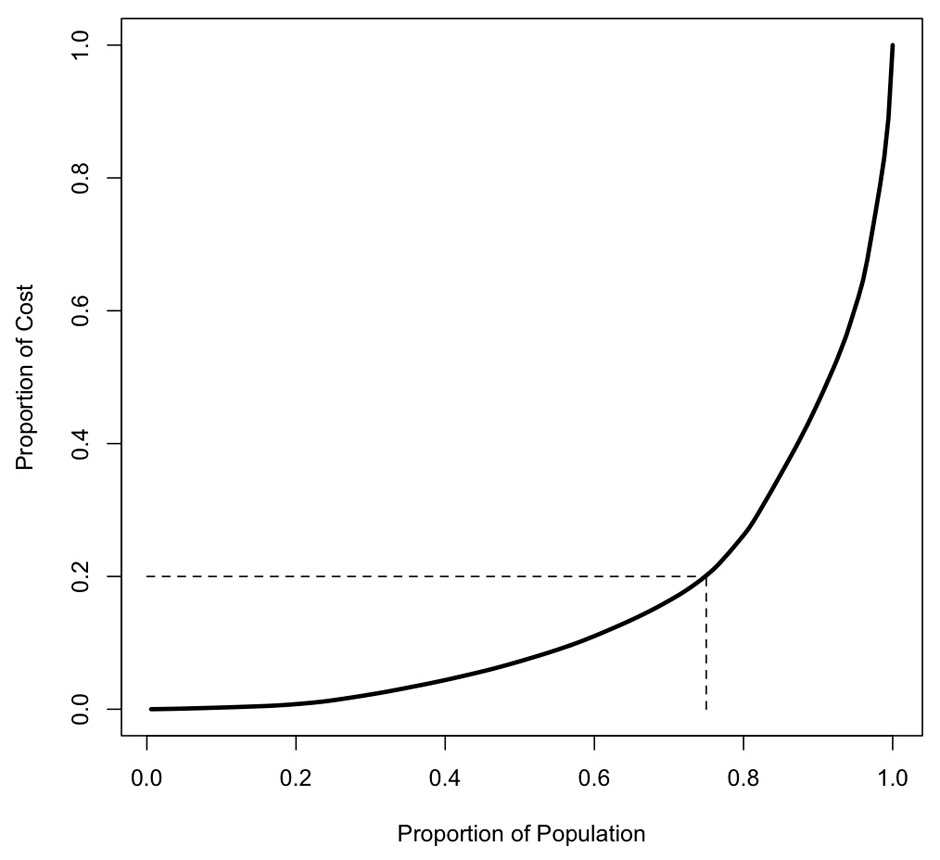
Figure 1
Concentration curve of direct medical costs of suicide attempts (n = 176).
The final regression model was based on 161 observations and included the following variables: age, method, diagnostic group, suicide intention, sex, history of migration and intensive care. Fifteen patients were excluded because not all the characteristics used in the logistic regression were recorded. There was no indication of multicollinearity of independent variables, which was tested for by calculation of a correlation matrix and variance inflation factors. Detailed results are shown in Table 5.
Individuals older than 64 were significantly more likely to be in the high-cost group with an odds ratio (OR) of 6.48 (p <0.01) compared to the group of 25–64 year olds. There was no statistically significant difference between patients aged 18–25 years and those aged 25–64 years. Patients who had attempted suicide using “hard methods” had a higher likelihood of being in the high-cost group (OR 3.38, p <0.05) although the somatic treatment was not significantly more expensive than for those using soft methods. Compared to the reference category ICD-10 F3, diagnostic categories F1 (OR 0.18, p <0.05) and F4 (OR 0.16, p <0.05) had significantly lower odds of being in the high-cost group. F2 and F5/6 showed no statistically significant difference with respect to F3. The likelihood of falling into the high-cost category was three times higher for subjects with severe suicidal ideation compared to those without lethal intention (OR 3.02, p <0.05). Intensive care treatment led to a higher likelihood (OR 3.59, p <.05) of being in the high-cost group compared to the subjects with no such treatment. Gender showed no statistically significant difference with an OR of 1.88 (p = 0.23) for females. While in univariate analysis, patients who were born in Switzerland created significantly higher costs than individuals with a history of migration, this finding was no longer significant in the regression analysis (OR for being an individual with a history of migration 0.51, p = 0.20).
| Table 5: Results of multiple logistic regression for high-cost case as outcome (n = 161, pseudo-R2 = 0.373). | |||
| Variable | Odds Ratio | 95% CI | p |
| Age 18–24a | 0.51 | 0.14–1.66 | 0.28 |
| Age 65 and abovea | 6.48 | 1.81–26.02 | 0.006 |
| Hard method | 3.38 | 1.22–9.82 | 0.02 |
| ICD-10 F 1b | 0.18 | 0.03–0.80 | 0.04 |
| ICD-10 F 2b | 0.76 | 0.19–2.86 | 0.68 |
| ICD-10 F 4b | 0.16 | 0.03–0.60 | 0.01 |
| ICD-10 F 5/6b | 0.30 | 0.05–1.41 | 0.15 |
| Lethal intention | 3.02 | 1.17–8.35 | 0.03 |
| Female gender | 1.88 | 0.69–5.42 | 0.23 |
| History of migration | 0.51 | 0.17–1.40 | 0.20 |
| Intensive care | 3.59 | 1.10–12.29 | 0.04 |
| a Reference category age 25–64. b Reference category ICD-10 F3. | |||
In Switzerland, official statistics on suicide attempts and thus detailed numbers regarding their costs are lacking. An official Swiss government report [12] estimated that, in Switzerland, only 10,000 of overall 15,000–25,000 suicide attempts are treated medically, with an extrapolated cost of approximately CHF 78.6 million. Little is known about the treatment of the remaining 5000 to 15 000 cases, which may largely consist of informal care. The present analysis based on the dataset of the WHO/EURO Multicentre Study on Suicidal Behaviour estimated total direct medical annual costs of CHF 3,373,025 in 2003 with a mean cost per case of 19,165 CHF in the canton of Basel-City. Based on our study, the extrapolated direct medical costs for the estimated 10,000 medically treated suicide attempts in Switzerland amount to 191 million CHF annually. Assuming the total number of suicide attempts in Switzerland to be about twice that number, the costs could be considerably higher. A rough comparison with the direct costs of treating common diseases can be made on the grounds of estimates for pharmaceutical cost groups provided by Beck et al. [26]. For example, the cost of treating kidney diseases was estimated to amount to 41,800 CHF per person per year. The treatment of individuals with the HI-Virus or AIDS cost 18,348 CHF per person per year.
To our knowledge, this is the first study investigating the influence of demographic and psychosocial variables on the cost structure of suicide attempts. The present analysis showed that 88% of the estimated total direct medical annual costs of CHF 3,373,025 in 2003 were spent on psychiatric treatment. These costs correlate strongly with the duration of hospitalisation due to the day-rate remuneration scheme in the UHP. These findings are in line with a recent UK-study on the cost of self-harm, which showed that 66% of overall costs were accrued in inpatient psychiatric care [27]. Complex cases, often entailing long-term physical and mental rehabilitation, are referred to the UPH as soon as stabilisation has been achieved. Physical treatment is then performed on an outpatient basis in the UH and is allocated to psychiatric costs for duration of the psychiatric hospitalisation although accrued due to somatic treatment. Additionally, suicide attempters using "hard methods" may be considered more seriously ill and consequently assigned to inpatient psychiatric care, possibly extending over a prolonged period, as use of “hard methods” and treatment in the ICU were significantly associated with higher costs both in univariate and multivariate analysis.
Patients aged older than 64 had significantly higher odds (6.48) of accruing high costs after a suicide attempt compared to the largest age-group (25–64 years). Suicidal behaviour in elderly people, therefore, seems to be not only a neglected, but also an expensive, problem. This finding becomes even more relevant in light of other research results regarding suicidal behaviour in this age group: About 71–95% of suicide victims aged 65 years or more suffered from a major mental disorder [28]. Other associated risk factors are physical illness, poverty or social isolation [29]. However, few elderly people with suicidal ideation seek out mental health services; most look for help in primary care [30–32]. Thus, prevention strategies are more likely to reach the elderly there [33, 34], and may be highly cost-effective.
Mental health problems like depression and other mood disorders, impulse-control disorders, anxiety disorders, psychosis and substance misuse have been demonstrated to have an important impact on suicidal behaviour [8, 35–39]. This is compatible with our finding of the largest subgroup of our dataset suffering from affective disorders (ICD-10 F3). Compared to the other diagnostic categories (ICD–10 F1, F2, F4 and F5/6) this group was more likely to occur in the high-cost group. This finding suggests that prevention measures improving recognition and treatment quality of mood disorders may be cost-effective strategies, and supports activities like those of the European Alliance against Depression [34, 40].
Surprisingly, gender was not significantly associated with high costs in the regression analysis. Men have a higher risk of completing suicide, since they tend to use more violent methods [41]. We therefore also expected them to incur higher costs with attempted suicides. Indeed, univariate analysis showed significantly higher costs for male subjects, but when checking for other variables in the regression analysis, males did not have significantly higher odds of being in the high-cost group. The association of “hard methods” with male gender and higher costs might have confounded the findings in univariate analysis. Ultimately, “hard methods” seem to have a greater influence on costs than gender (OR 3.38).
Our analysis indicated that subjects born in Switzerland produced higher costs than individuals with a history of migration. Although the latter seem to produce lower costs overall, there was no significant association with costs in multivariate analysis. Possibly, this group is discharged earlier from psychiatric treatment than natives, probably due to limited language proficiency, which has recently been shown in a study in our neighbour region [42]. Although a speculative supposition, the deep cultural coherence in some subgroups of individuals with a history of migration (e.g., of Turkish or Albanian origin) [43] may also promote shorter hospital stays and an earlier discharge to informal family care. Additionally, this group is less frequently in the group of the elderly, which were shown to generate higher costs.
Attempted and completed suicides may not only have a severe impact on the patients’ family and friends, but also on the professionals working with these patients [44], potentially lowering their own health and productivity levels. Future studies should aim to investigate indirect costs to patients, caregivers and professionals to clarify the significance for attempted suicide.
Our study did not consider the costs of outpatient treatment for other services and private practices, or direct non-medical costs (e.g., counseling costs), because there is little detailed data regarding number of suicide attempts treated in this environment and the number of not registered cases is considered high in Switzerland [12]. Furthermore, the indirect costs borne by patients and caregivers (e.g., attributable to productivity losses or informal care) were not considered. Nevertheless, the study assesses cost components already identified as crucial since current research identifies indirect costs, ascribed to lost life years, as being the major cost component for completed suicides, but direct medical costs as being the major cost component for attempted suicides. The generalisability of our results may vary due to differences in health care systems. Furthermore, admission policies may differ by countries or even regions. However, our sample has similar characteristics of suicide attempters in other regions of Switzerland, and our results may therefore be useful for clinicians and policy makers in other settings. Furthermore, attempted suicide is often associated with mental disorders and therefore one might argue that direct costs cannot be allocated to attempted suicide without regard to the underlying psychiatric disorder. Some of the costs might be caused by the psychiatric disorder and not necessarily be due to the suicide attempt. However, suicide attempts are often the reason for the initiation of psychiatric treatment. Moreover, they may also trigger crises of their own with a rise in cost due to intensified treatment and potential supplemental somatic care. To clarify that matter, more research comparing cost of suicide events and general cost due to psychiatric illness is needed.
Clearly, economic aspects should not be the only driver in designing a policy for suicide prevention. But from a health-economic perspective, the financial burden of suicide attempts as such justifies appropriate and targeted interventions. So far, few government-sponsored intervention schemes have addressed this issue. Our results suggest that specific subgroups, e.g. elderly patients or patients with mood disorders, cause disproportionately high costs. Programmes specifically targeting these groups could deliver a more attractive result in terms of economic outcomes.
Funding / potential competing interests: The study was supported by grants of the Voluntary Academic Society Basel (2 July 2007) and the Swiss Federal Office of Public Health (contract No. 02.001.732/2.25.01.–382). G. Stoppe has been receiving speaker and advisory board honoraria from various companies including Astra Zeneca, Bristol Myers Squibb, Desitin, Eli Lilly, Janssen Cilag, Lundbeck, Merz, Novartis, Pfizer, Sanofi, Servier. She received research grants by Bristol Myers Squibb. A. Riecher-Rössler has been receiving support from Eli Lilly, Lundbeck, Mepha Pharma, Pfizer, Servier. The other authors declare no conflicts of interest.
1 Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJL (eds). Global burden of disease and risk factors. New York, NY: Oxford University Press; Washington, DC: World Bank; 2006.
2 World Health Organization. SUPRE Prevention of suicidal behaviours: a task for all. 2012 [cited 2012 June 22nd]; Available from: http://www.who.int/mental_health/prevention/suicide/information/en/index.html.
3 Knox KL, Caine ED. Establishing priorities for reducing suicide and its antecedents in the United States. Am J Public Health. 2005;95:1898–903.
4 Schopper D, Pereira J, Torres A, Cuende N, Alonso M, Baylin A, et al. Estimating the burden of disease in one Swiss canton: what do disability adjusted life years (DALY) tell us? Int J Epidemiol. 2000;29:871–77.
5 Beautrais A, Mishara B. World Suicide Prevention Day--September 10, 2007: "suicide prevention across the life span". Crisis. 2007;28:57–60.
6 Bertolote JM, Fleischmann A, De Leo D, Bolhari J, Botega N, De Silva D, et al. Suicide attempts, plans, and ideation in culturally diverse sites: the WHO SUPRE-MISS community survey. Psychol Med. 2005;35:1457–65.
7 Kuo WH, Gallo JJ. Completed suicide after a suicide attempt. Am J Psychiatry. 2005;162:633.
8 Kessler RC, Berglund P, Borges G, Nock M, Wang PS. Trends in suicide ideation, plans, gestures, and attempts in the United States, 1990-1992 to 2001-2003. JAMA. 2005;293:2487–95.
9 Angst J, Degonda M, Ernst C. The Zurich Study: XV. Suicide attempts in a cohort from age 20 to 30. Eur Arch Psychiatry Clin Neurosci. 1992;242:135–41.
10 Rey Gex C, Narring F, Ferron C, Michaud PA. Suicide attempts among adolescents in Switzerland: prevalence, associated factors and comorbidity. Acta Psychiatr Scand. 1998;98:28–33.
11 Michel K, Knecht C, Kohler I, Sturzenegger M. Suizidversuche in der Agglomeration Bern [Attempted suicide in the Bern region]. Schweiz Med Wochenschr. 1991;121:1133–39.
12 Swiss Federal Office of Public Health. Suizid und Suizidprävention in der Schweiz: Bericht in Erfüllung des Postulates Widmer (02.3251) [Suicide and suicide prevention in Switzerland: report in answer to the Widmer postulate (02.3251)]. 2005. Swiss Federal Office of Public Health. Accessed 5 November 2010. Available from: http://www.bag.admin.ch/themen/medizin/00683/01915/index.html.
13 Weissman MM, Bland RC, Canino GJ, Greenwald S, Hwu HG, Joyce PR, et al. Prevalence of suicide ideation and suicide attempts in nine countries. Psychol Med. 1999;29:9–17.
14 Clayton D, Barcelo A. The cost of suicide mortality in New Brunswick, 1996. Chronic Dis Can. 1999;20:89–95.
15 Goldsmith SK, Committee on Pathophysiology and Prevention of Adolescent and Adult Suicide, Institute of Medicine (U.S.). Reducing suicide: a national imperative. Washington, DC: National Academies Press; 2002.
16 Runeson B, Wasserman D. Management of suicide attempters: what are the routines and the costs? Acta Psychiatr Scand. 1994;90:222–28.
17 Kennelly B, Ennis J, O'Shea E. Economic cost of suicide and deliberate self harm. Reach out. National strategy for action on suicide prevention 2005–2014. 2005, Dublin. Department of Health and Children.
18 O'Dea D, Tucker S. The Cost of Suicide to Society. 2005, Wellington. Ministry of Health.
19 Swiss Federal Statistical Office: Structure of the resident permanent population by cantons 1999–2009. Accessed March 5, 2012. Available from: http://www.bfs.admin.ch/bfs/portal/de/index/themen/01/22/lexi.Document.20567.xls.
20 Schmidtke A, Bille-Brahe U, DeLeo D, Kerkhof A, Bjerke T, Crepet P, et al. Attempted suicide in Europe: rates, trends and sociodemographic characteristics of suicide attempters during the period 1989-1992. Results of the WHO/EURO Multicentre Study on Parasuicide. Acta Psychiatr Scand. 1996;93:327–38.
21 World Health Organization. The ICD-10 classification of mental and behavioural disorders: diagnostic criteria for research. Geneva: World Health Organization; 1993.
22 Hulten A, Jiang GX, Wasserman D, Hawton K, Hjelmeland H, De Leo D, et al. Repetition of attempted suicide among teenagers in Europe: frequency, timing and risk factors. Eur Child Adolesc Psychiatry. 2001;10:161–69.
23 Steffen T, Maillart A, Michel K, Reisch T. Final report on monitoring of suicidal behavior in the Bern agglomeration of the years 2004 to 2010 in the context of the WHO/MONSUE Multicentre Study on Suicidal Behaviour and the Bernese Alliance against Depression [Abschlussbericht Monitoring des suizidalen Verhaltens in der Agglomeration Bern der Jahre 2004 bis 2010 im Rahmen der WHO/MONSUE Multicentre Study on Suicidal Behaviour und des Berner Bündnisses gegen Depressionen]. 2011, Bern. Swiss Federal Office of Public Health. Accessed March 5, 2012. Available from: http://www.bag.admin.ch/themen/medizin/00683/03923/index.html.
24 Gini C. Variabilità e mutabilità [Variability and Mutability]. 1912
25 Royston P, Altman DG, Sauerbrei W. Dichotomizing continuous predictors in multiple regression: a bad idea. Stat Med. 2006;25:127–41.
26 Beck K, Trottmann M, Käser U, Keller B, Zweifel P. Nachhaltige Gestaltung des Risikoausgleichs in der Schweizer Krankenversicherung [Sustainable Risk Adjustment in Swiss Mandatory Health Insurance]. Bern: h.e.p. Verlag; 2006.
27 Sinclair JM, Gray A, Rivero-Arias O, Saunders KE, Hawton K. Healthcare and social services resource use and costs of self-harm patients. Soc Psychiatry Psychiatr Epidemiol. 2011;46:263–71.
28 Conwell Y, Duberstein PR, Caine ED. Risk factors for suicide in later life. Biol Psychiatry. 2002;52:193-204.
29 Dennis MS, Wakefield P, Molloy C, Andrews H, Friedman T. A study of self-harm in older people: mental disorder, social factors and motives. Aging Ment Health. 2007;11:520–25.
30 Luoma JB, Martin CE, Pearson JL. Contact with mental health and primary care providers before suicide: a review of the evidence. Am J Psychiatry. 2002;159:909–16.
31 Baltes PB, Mayer KU. The Berlin aging study: aging from 70 to 100. Cambridge: Cambridge University Press; 1999.
32 Juurlink DN, Herrmann N, Szalai JP, Kopp A, Redelmeier DA. Medical illness and the risk of suicide in the elderly. Arch Intern Med. 2004;164:1179–84.
33 Stoppe G, Sandholzer H, Huppertz C, Duwe H, Staedt J. Family physicians and the risk of suicide in the depressed elderly. J Affect Disord. 1999;54:193–98.
34 Hegerl U, Althaus D, Schmidtke A, Niklewski G. The alliance against depression: 2-year evaluation of a community-based intervention to reduce suicidality. Psychol Med. 2006;36:1225–33.
35 Shaffer D, Gould MS, Fisher P, Trautman P, Moreau D, Kleinman M, et al. Psychiatric diagnosis in child and adolescent suicide. Arch Gen Psychiatry. 1996;53:339–48.
36 Hawton K, Houston K, Haw C, Townsend E, Harriss L. Comorbidity of axis I and axis II disorders in patients who attempted suicide. Am J Psychiatry. 2003;160:1494–500.
37 Yen S, Shea MT, Pagano M, Sanislow CA, Grilo CM, McGlashan TH, et al. Axis I and axis II disorders as predictors of prospective suicide attempts: findings from the collaborative longitudinal personality disorders study. J Abnorm Psychol. 2003;112:375–81.
38 Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch Gen Psychiatry. 1999;56:617–26.
39 Suominen KH, Isometsa ET, Henriksson MM, Ostamo AI, Lonnqvist JK. Inadequate treatment for major depression both before and after attempted suicide. Am J Psychiatry. 1998;155:1778–80.
40 Hegerl U, Wittmann M, Arensman E, Van Audenhove C, Bouleau JH, Van Der Feltz-Cornelis C, et al. The 'European Alliance Against Depression (EAAD)': a multifaceted, community-based action programme against depression and suicidality. World J Biol Psychiatry. 2008;9:51–8.
41 Denning DG, Conwell Y, King D, Cox C. Method choice, intent, and gender in completed suicide. Suicide Life Threat Behav. 2000;30:282–88.
42 Bermejo I, Kriston L, Berger M, Harter M. Patients' language proficiency and inpatient depression treatment in Baden-Wurttemberg (South Germany). Psychiatr Serv. 2009;60:545–48.
43 White JB. Turks in the New Germany. American Anthropologist. 1997;99:754–69.
44 Gulfi A, Castelli Dransart DA, Heeb JL, Gutjahr E. The impact of patient suicide on the professional reactions and practices of mental health caregivers and social workers. Crisis. 2010;31:202–10.