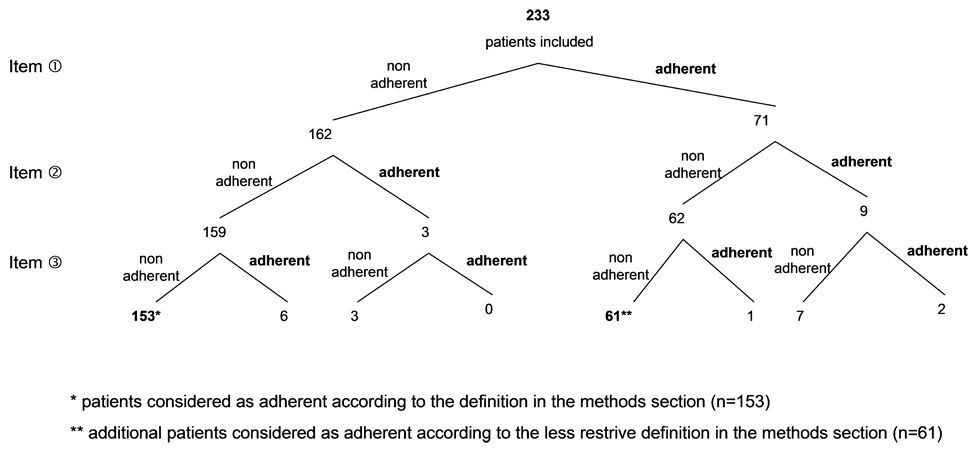
Figure 1
Responses given by the patients to the first three items of the questionnaire.
DOI: https://doi.org/10.4414/smw.2012.13642
An observational cross-sectional study
The degree of patient adherence to Highly Active Antiretroviral Therapy (HAART) is recognised to be a key factor for long-term positive health outcomes [1]. Research indicates that consistently high levels of adherence are necessary for reliable viral suppression [2, 3] and prevention of resistance [4], disease progression [5], and death [6]. An adherence level to HAART, of 80–95% for each patient, has been considered necessary to ensure treatment success [2, 7], but 40–60% of patients do not achieve these levels [8]. Despite the HAART simplification strategies in recent years [9], HIV remains a disease with some predictive characteristics of poor adherence, including its chronic asymptomatic nature, and its rapidly changing treatment regimens associated with adverse effects, which can also require dietary restrictions [10, 11].
Health-related information helps patients cope with illness by increasing knowledge and reducing feelings of uncertainty [12]. In chronic illness, comprehension of medication instructions is an essential condition for adherence [13, 14]. In the field of HIV/AIDS, accurate and appropriate information is necessary to promote adherence, and to ensure that patients achieve the best treatment outcomes [15]. Currently, when seeking medical information, outpatients have a number of sources to choose from, including health-related websites, patient information leaflets, mass media sources such as newspapers, magazines and television, family and friends, and patient associations [16–20]. In the medical literature, positive collaboration between patient and physician has been widely explored, and is associated with better patient adherence [21]. The patient-pharmacist relationship has been less studied [22]. In France, drugs are available for patients in hospital pharmacies together with community pharmacies. In theory, pharmacists are well-positioned to play a primary role in improving adherence to HAART therapies, because they are accessible without appointment and outside of hospitalisation, unlike nurses or physicians, and because they have extensive training in HAART pharmaceuticals. In the Bultman et al. study [23], patient satisfaction and medication adherence were strongly influenced by the pharmacist’s role in medication monitoring.
In this study, we wanted to know which sources of medication information HIV-infected patients used and their impact on adherence. In secondary objectives, we determined profiles of non-adherent patients and specified the role of the pharmacist.
We conducted a cross-sectional, observational study during three months, from April to June 2009, in one community pharmacy and one French university hospital pharmacy.
Subjects included were outpatients of community and university hospital pharmacies treated by HAART (naïve or not). Patients who were not able to read and understand French and those with cognitive impairment were excluded from the study. Each patient gave informed consent and participated only once in the study. The clinical data and medical history were extracted from software protected by the CNIL (National Committee on Data Protection).
The research group, composed of one infectious disease physician, one public health physician, two pharmacists and one statistician, created a self-report questionnaire divided into 7 items (table 1). The questions were formulated in a way that allowed for differentiation of (1) medication adherence measurement (items 1, 2 and 3), (2) predictors of adherence (items 1, 5 and 7), and (3) sources of medication information (items 4 and 6). The pharmacist’s role was assessed by two items: item 6, which was a direct question, and the multi-choice item 4. Items 2 and 3 were extracted from the 8-item Morisky medication adherence scale [24].
Before the study, a questionnaire was piloted with a small sample of patients (n = 10) to ensure patient understanding of the wording of the questionnaire. These patients were excluded from the present study. In the community and hospital pharmacies, the self-reported questionnaires were offered to outpatients by a pharmacist.
| Table 1: Self-reported questionnaire on taking medication and sources of information. |
| Under what circumstances, did you not take your HIV-medication? Several answers are possible I was not home and I did not have my medication with me I was busy doing something else There have been changes in my routine I felt asleep when taking my medication I had too many tablets or capsules to take I felt that the treatment was dangerous or toxic I did not want to be seen taking my medication This never happens, I always take my medication Other: ...................... When you feel better, do you sometimes stop taking your medicine? Yes No Sometimes if you feel worse when you take the medicine, do you stop taking it? Yes No When you have a question about your HIV-medication, where do you look for information? Several answers are possible Community physician Hospital physician Community pharmacist Hospital pharmacist Social workers Patient associations Internet Newspapers Patient information leaflet Family Have you experienced any side effects? Yes No Has your pharmacist informed you about your HIV-medication? Yes No Are you supported by patient associations? Yes No |
Socio-demographic information, including gender, age, marital status, profession, and duration of HIV diagnosis were collected through the self-administered questionnaire. Medical records were reviewed for CD4 cell count and baseline viral load. HAART regimens were collected from computer-entered prescriptions.
A patient was considered adherent according to the first three items that is if he/she answered he/she always takes his/her medication (“In which circumstances did you not taken your HIV-medication?” “It never happens to me, I always take my medication”), and he/she never stopped taking his/her medicine when he/she felt better or worse (“When you feel better, do you sometimes stop taking your medicine?” “No”, and “Sometimes if you feel worse when you take the medicine, do you stop taking it?” “No”). In all other cases (answers converging to nonadherence or divergent answers), the patient was considered to be non-adherent. A sensitivity analysis was performed using a less restrictive definition for adherence: a patient was considered adherent if he/she never stopped taking his/her medicine when he/she felt better or worse (items 2 and 3).
We presented the proportion of adherent patients. The 95% Confidence Intervals (CIs) were estimated using the exact binomial distribution.
We analysed potential predictors of adherence (sex, age, marital status, dispensing site and length of HAART treatment, CD4 cell count and baseline viral load, side effect and patient tolerance) in univariate analyses, using Wilcoxon’s test or Fisher’s exact test as appropriate. We also examined if the sources of treatment information (multi-choice item 4) were linked to adherence using the same tests. To avoid multiple tests, we considered only sources that were not highly correlated (correlation coefficient r <0.50 using the sources of information as dichotomous variables). Candidate variables for the multivariate logistic regression analysis were variables with p <0.20 in univariate analysis and with less than 20% missing data (age, marital status, CD4 cell count and baseline viral load were excluded). The final model was achieved using a backward selection (non significant variables were removed sequentially). P <0.05 was considered statistically significant.
The statistical software SAS (release 9.1; SAS Institute Inc., Cary, NC, USA) and R (release 2.8.1; 2008 The R Foundation for Statistical Computing) were used for all analyses.
During the 3-month study period, 233 HIV-infected patients were included. The patients were 62.2% male (145/233), and the median age was 43 (min-max: 36–51 years). 77.3% (180/233) of the patients included received their HAART medication at hospital pharmacy, and 76.4% (178/233) of them had been treated for more than 5 years (table 2).
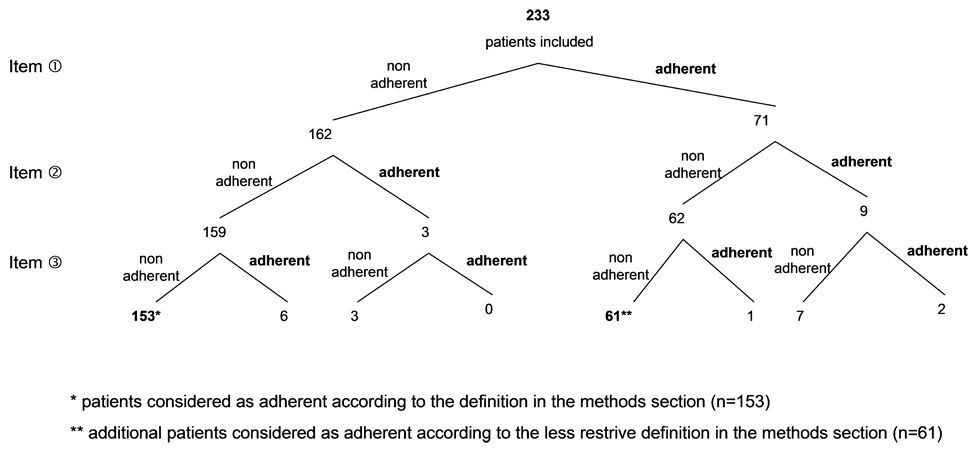
Figure 1
Responses given by the patients to the first three items of the questionnaire.
The sources of information reported by patients about their HAART treatment according to their adherence or non-adherence are presented in table 2. Amongst all patients, more than 70% of patients sought information about their HAART treatments from their physicians (hospital or community physician), and patient information leaflets. Patient associations, internet and newspapers have been consulted by 33.9%, 29.6% and 26.6% respectively. Medication information was requested by 16.3% of outpatients from their community pharmacists and by 3.4% from their hospital pharmacist.
Most sources of information were highly correlated (reported/not reported simultaneously):
“community physician” and “patient information leaflet” (r = 0.68), “internet” and “newspapers” (r = 0.59), and “patient associations” and “newspapers” (r = 0.55). The correlation coefficient between “internet” and “patient associations” was 0.43 whereas correlation coefficients between other sources of information were lower than 0.40.
| Table 2:Characteristics of patients and HAART treatment. | |||||||
| Characteristics | All patients (N = 233) | Adherent* (N = 153) | Non adherent* (N = 80) | pvalue † | |||
| Patients | |||||||
| Male, n (%) | 145 | (62.2) | 102 | (66.7%) | 43 | (53.7%) | 0.065 |
| Age, median (IQR) | 43 | (36–51) | 43 | (34–51) | 42 | (37–51) | 0.76 |
| Marital status, n (%) | 0.43 | ||||||
| Single | 74 | (31.8%) | 50 | (32.7%) | 24 | (30.0%) | |
| Married | 47 | (20.2%) | 29 | (18.9%) | 18 | (22.5%) | |
| Other | 60 | (25.8%) | 34 | (22.2%) | 26 | (32.5%) | |
| HAART treatment | |||||||
| Dispensing, n (%) | <0.001 | ||||||
| Hospital pharmacy | 180 | (77.3%) | 107 | (69.9%) | 73 | (91.2%) | |
| Community | 51 | (21.9%) | 44 | (28.8%) | 7 | (8.7%) | |
| Duration, n (%) | 0.55 | ||||||
| <1 year | 3 | (1.3%) | 3 | (2.0%) | (0.0%) | ||
| 1 to 5 years | 46 | (19.7%) | 31 | (20.3%) | 15 | (18.7%) | |
| >5 years | 178 | (76.4%) | 113 | (73.9%) | 65 | (81.2%) | |
| Medical records | |||||||
| CD4 cell count (ml3), median (IQR) | 559 | (398–730) | 548 | (396–700) | 581 | (407–776) | 0.85 |
| Baseline viral load (no. copies/ml) , median (IQR) | 40 | (20–40) | 40 | (20–40) | 40 | (20–40) | 0.49 |
| Sources of information‡ | |||||||
| Hospital physician | 186 | (79.8) | 142 | (92.8) | 44 | (55.0) | <0.001 |
| Community physician | 173 | (74.2) | 126 | (82.4) | 47 | (58.8) | <0.001 |
| Patient information leaflet ¶ | 172 | (73.8) | 127 | (83.0) | 45 | (56.3) | |
| Patient associations | 79 | (33.9) | 58 | (37.9) | 21 | (26.3) | 0.082 |
| Internet | 69 | (29.6) | 60 | (39.2) | 9 | (11.3) | <0.001 |
| Newspapers § | 62 | (26.6) | 52 | (34.0) | 10 | (12.5) | |
| Community pharmacist | 38 | (16.3) | 25 | (16.3) | 13 | (16.3) | 0.99 |
| Family | 25 | (10.7) | 18 | (11.8) | 7 | (8.8) | 0.66 |
| Hospital pharmacist | 8 | (3.4) | 4 | (2.6) | 4 | (5.0) | 0.45 |
| Social workers | (0.0) | (0.0) | (0.0) | ND | |||
| number of sources of information, mean (SD) | 3.5 | (1.8) | 4.0 | (1.8) | 2.5 | (1.5) | <0.001 |
| Discomfort and support | |||||||
| Side Effects | 100 | (42.9) | 75 | (49.0) | 25 | (31.2) | 0.012 |
| Support by patient associations | 129 | (55.4) | 106 | (69.3) | 23 | (28.8) | <0.001 |
| IQR = Interquartile Range, SD = Standard Deviation, ND = Not Defined Characteristics with more than 20% missing data (number of missing data): Age (82), Marital status (52), CD4 cell count (51), Baseline viral load (49). * See Methods for definition. † according to Wilcoxon’s test or Fisher’s exact test as appropriate ‡ Total percentages for all sources of information exceed 100%, since answers were not exclusive (item4). § To avoid multiple tests, this comparison was not tested. The source of information “newspapers” was highly correlated with “internet” (pr = 0.59) ¶ To avoid multiple tests, this comparison was not tested. The source of information “patient information leaflet” was highly correlated with “community physician” (r = 0.68) | |||||||
Responses given by the patients to the first three items of the questionnaire are described in figure 1. A total of 65.7% patients (95% CI: 59.2% to 71.7%, 153/233) were considered to be adherent according to their answers to the first three items (see definition in statistical analysis section). The reasons for non-adherence to treatment were reported by 71 patients (out of 80 non-adherent patients) and are presented in table 3. The main reasons were: feeling uncomfortable taking medication in front of other people (39.4%), and absence of their medication due to absence from home (28.2%).
Among the 80 non-adherent patients, 61 gave a circumstance in which they did not take their HIV-medication (item 1) but answered they never stopped taking their medicine when they felt better or worse (items 2 and 3). Thus, according to a less restrictive definition for adherence (considering only items 2 and 3), 91.8% patients (95% CI: 87.6% to 95.0%, 214/233) were adherent.
| Table 3:Reasons for non-adherence to treatment. | ||
| Reason, n (%)* | N = 71† | |
| Did not want to be seen during administration | 29 | (39.4) |
| Not at home and did not have medication | 20 | (28.2) |
| Fell asleep when taking medication | 14 | (19.7) |
| Change in the daily routines | 11 | (15.5) |
| Under the impression that the medication was dangerous or toxic | 10 | (14.1) |
| Busy doing something else | 5 | (7.0) |
| Other | 5 | (7.0) |
| Too many pills or capsules to take | (0.0) | |
| * Total percentages exceed 100% since answers were not exclusive † 80 patients were considered non-adherent according to their answers to the first three items (see Methods for definition) but 9 did not give reasons, since they answered to item 1 (“In which circumstances do you forget your medicine?”) “It never happens to me, I always take my medicine”. | ||
The sources of information from newspapers, patient information leaflets and social workers were not studied since the prior two were highly correlated with internet and community physicians respectively and the last one was never reported by patients (see paragraph on sources of information about HAART treatment). In univariate analysis, community pharmacy dispensing, number of sources of information, potential support of patient associations, presence of side effects and the sources of information “community physician”, “hospital physician”, and “internet” were significantly associated with adherence to treatment; male sex and the source of information “patient associations” were at the limit of significance (respectively p = 0.07 and p = 0.09). Age, marital status, length of HAART treatment, CD4 cell count, baseline viral load, and the sources of information “community pharmacist”, “hospital pharmacist” and “family” did not influence adherence (p >0.20).
In the multivariate logistic regression model (table 4), the sources of information “community physician”, “hospital physician”, “internet”, and the potential support of patient associations remained significant. Patients with “hospital physician” as source of information were almost six times more likely to be adherent than patients without (OR = 5.8 [95% CI: 2.3 to 14.2], p <0.001), patients with “community physician” as source of information were four times more likely to be adherent than patients without (OR = 4.5 [95% CI: 2.1 to 9.7], p <0.001), patients with potential support were four times more likely to be adherent than those without support (OR = 4.5 [95% CI: 2.1 to 9.4], p <0.001), and patients with “internet” as source of information were almost three times more likely to be adherent than patients without this source of information (OR = 2.7 [95% CI: 1.1 to 6.5], p = 0.028).
| Table 4:Multivariable analysis of adherence to treatment. | ||||
| N = 231 patients* | Full Model† | Final Model‡ | ||
| OR [95%CI] | pvalue | OR [95%CI] | pvalue | |
| Male (versus female) | 2.4 [1.1–5.6] | 0.037 | ||
| HAART treatment dispensing at community (vs hospital pharmacy) | 1.7 [0.5–5.8] | 0.43 | ||
| Information by community physician (versus no) | 7.3 [1.9–28.3] | 0.004 | 4.5 [2.1–9.7] | <0.001 |
| Information by hospital physician (versus no) | 5.4 [1.5–20.0] | 0.012 | 5.8 [2.3–14.2] | <0.001 |
| Information by patient associations (versus no) | 1.5 [0.4–5.7] | 0.54 | ||
| Information by Internet (versus no) | 2.2 [0.7–7.3] | 0.182 | 2.7 [1.1–6.5] | 0.028 |
| number of sources of information (for one-source increase) | 0.9 [0.5–1.4] | 0.59 | ||
| Side Effects (versus no) | 1.0 [0.5–2.3] | 0.97 | ||
| Support by patient associations (versus no) | 5.5 [2.5–12.0] | <0.001 | 4.5 |2.1–9.4] | <0.001 |
| OR = Adjusted Odds Ratio of adherence to treatment (versus non adherence) * Two missing data on site ofHAART treatment dispensing. † Including variables with p <0.20 in univariate analysis and with less than 20% missing data (age, marital status, CD4 cell count and baseline viral load were not included). ‡ After removing non significant variables sequentially (backward selection). | ||||
In our study, among sources used by HIV-infected outpatients, their physicians are the most helpful sources of information about HAART. Patients who reported both newspapers, internet, and patient associations together were the most adherent. In our study, the hospital pharmacist didn’t play a key role in informing HIV-infected outpatients; the community pharmacist had a limited role.
To date, there has been little research on HIV-positive patients’ use of information concerning HAART. In our study, we have identified patterns of patient behaviours in seeking medication information with highly correlated sources. The physician-patient collaboration has been widely explored in the medical literature [25, 26]. The goal of this collaboration is that the patient’s self-knowledge needs are combined with the medical knowledge of the physician, in order to find the best possible treatment regimen for that individual patient [27]. Despite these numerous sources of information, the relationships between patients and healthcare professionals are still significant in their perception of the disease. Additionally, patient information leaflets were widely consulted by participants. These documents were written by healthcare professionals especially to inform about the drug and prevent its misuse [28]. The internet was not classified among the prominent sources. This result is all the more surprising because the populations were young (median ages: 43 [36–51] years). Conversely, in 2002, Kalichman et al. [29, 30] found that 64% of persons with home access to Internet had searched for HAART information online.
In our study, the self-reported rate of adherence was 65.7% and the main reasons for non-adherence reported by outpatients were: feeling uncomfortable taking medication in front of other people and absence of their medication when they were away from home. The self-reported rates of non-adherence were similar to those published in the scientific literature for patients receiving treatment for chronic conditions. Recent studies of patients with HIV/AIDS have reported low adherence rates [31]. There is no ideal rate of adherence, but in HIV infection, it is accepted that each patient achieve more than 95 percent adherence to HAART [32] in order to suppress viral replication and avoid the emergence of resistance. Non-adherence to HAART can have important public health implications. Understanding treatment, anticipation of side effects, and information about therapeutic objectives could be measures for improving adherence to HAART [31]. Knowing the reasons for non-adherence to HAART is essential in elaborating educational programs and training healthcare professionals to properly advise patients. In our study, the most common reasons patients reported for skipping HAART medications included the difficulty of integrating treatment schedules into their daily activities, and worries about HIV disclosure. The same results were reported in the National Institutes of Health guidelines about antiretroviral therapy [33] which note the ability of patients to fit the medication into their daily routines and feel comfortable taking medication in front of other people were identified as psychosocial predictors of good adherence. These predictors of adherence underline the importance of tailoring the regimen to the patient’s lifestyle [34].
A multicentre qualitative survey on HIV positive adolescents’ perceptions of their disease [35], published in 2010, confirms the results of the present study. Indeed, this work has shown that the majority of the adolescents do not reveal their HIV condition to their friends and consequently take their medication secretly. In the same study, the results suggest that adherence was linked with the kind of relationship established between the patient and physician, from a fairly paternalistic type to a more collaborative one.
Our results show that, although the majority of the outpatients received their HAART at the hospital pharmacy (77.3%), only 3.4% indicated they consulted their hospital pharmacist for information about HAART. In the context of HIV, all members of the healthcare team are responsible for ensuring that patients understand their treatment. The ultimate responsibility for this understanding lies with the pharmacist [36]. The hypothesis which explains the present results, and which was often formulated by the outpatients during the study, is that the hospital pharmacists' knowledge and expertise are not well known by the patients. The main role of pharmacists is to dispense medications. They must also ensure the proper use of drugs by validating medical prescriptions and providing patient counseling. However, pharmacists may be a source of information about drug usage, such as interactions, drug benefits or side effects, and as a support about medication [22]. The results of the present study confirm that, in our teaching hospital, hospital pharmacists still have a way to go before being perceived as professionals who fully meet patients’ healthcare needs [22]. Paradoxically, many studies have reported hospital pharmacist interventions to improve HAART adherence. Like other healthcare professionals, the hospital pharmacist has also participated in patient education and counselling [37]. The pharmacist’s role as partner and active participant in patient care is relatively new, and still evolving [22].
The main limitation in our study is the measure of non-adherence. We have chosen the principal method employed, and the easiest to use in clinical practice: the self-reported questionnaire. There is no standard method for measuring non-adherence, and we did not confirm the validity of patients’ responses to the questionnaire with an objective adherence measure. The non-validation of the adherence questionnaires is common in scientific literature, but could question the predictive factors identified. Another limitation of the self-reported questionnaire is can there be a chance of recall bias which could in turn affect the measurements. In addition, results from the multivariate analysis must be considered carefully, since variables with a lot of missing data were not included in the logistic regression model. A potential limitation could be that this study was conducted in a single hospital. The other centres might have different models to counsel HIV-infected patients with their medication and hospital pharmacists might have different missions. Another limitation is that the frequency with which each source was accessed was not measured. Our study does not take into account this possibility and a person who uses a source of information once has been classified in the same way as someone who uses it frequently, to get medication information.
Regarding practice implications, pharmacists are medication experts, and could be a competent supplement to the physician in informing patients about their medication. Based on the findings of this study, there is evidence indicating the need for improved communication between the hospital pharmacist and outpatients. Pharmacistscan aid adherence by playing a key educational role, counseling patients on the importance of medication adherence and providing specific guidance on the proper use of medication, including information on any adverse effects and drug-drug interaction that may be expected.
1 Konkle-Parker DJ, Erlen JA, Dubbert PM. Lessons learned from an HIV adherence pilot study in the deep south. Patient Educ Couns. 2010;78:91–6.
2 Paterson DL, Swindells S, Mohr J, Brester M, Vergis EN, Squier C, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med. 2000;133:21–30.
3 Bangsberg DR, Hecht FM, Charlebois ED, Zolopa AR, Holodniy M, Sheiner L, et al. Adherence to protease inhibitors, HIV-1 viral load, and development of drug resistance in an indigent population. AIDS. 2000;14:357–66.
4 Bangsberg DR, Charlebois ED, Grant RM, Holodniy M, Deeks SG, Perry S, et al. High levels of adherence do not prevent accumulation of HIV drug resistance mutations. AIDS. 2003;17:1925–32.
5 Bangsberg DR, Perry S, Charlebois ED, Clark RA, Roberston M, Zolopa AR, et al. Non-adherence to highly active antiretroviral therapy predicts progression to AIDS. AIDS. 2001;15:1181–3.
6 Wood E, Hogg RS, Yip B, Harrigan PR, O’Shaughnessy MV, Montaner JS. Is there a baseline CD4 cell count that precludes a survival response to modern antiretroviral therapy? AIDS. 2003;17:711–20.
7 Gross R, Bilker WB, Friedman HM, BL Strom. Effect of adherence to newly initiated antiretroviral therapy on plasma viral load. AIDS. 2001;15:2109–17.
8 Bartlett JA. Addressing the challenges of adherence. J Acquir Immune Defic Syndr. 2002;29(Suppl 1):S2–10.
9 Nachega JB, Mugavero MJ, Zeier M, Vitoria M, Gallant JE. Treatment simplification in HIV-infected adults as a strategy to prevent toxicity, improve adherence, quality of life and decrease healthcare costs. Patient Preference and Adherence. 2011;5:357–67.
10 Walsh JC, Horne R, Dalton M, Burgess AP, Gazzard BG. Reasons for non-adherence to antiretroviral therapy: patients' perspectives provide evidence of multiple causes. AIDS Care 2001;13:709–20.
11 Ferguson TF, Stewart KE, Funkhouser E, Tolson J, Westfall AO, Saag MS. Patient-perceived barriers to antiretroviral adherence: associations with race. AIDS Care. 2002;14:607–17.
12 Johnson J. Cancer-related information seeking., ed. I. Cresskil NJ: Hampton Press. 1997.
13 Alexender S, Golin C, Kalinowski C. Provider-patient communication and treatment adherence. in Patient treatment adherence: concepts, interventions, and measurement., O.E. Bosworth H, Weinberger M, Editor. 2005, Lawrence Erlbaum: London. p. 329–72.
14 DiMatteo MR. Patient adherence to pharmacotherapy: the importance of effective communication. Formulary. 1995;30:596–8, 601–2, 605.
15 Hill H. A career as a.specialist HIV pharmacist. Hosp Pharm. 2006;1:15–6.
16 Hesse BW, Nelson DE, GL Kreps, Croyle RT, Arora NK, Rimer BK, et al. Trust and sources of health information: the impact of the Internet and its implications for health care providers: findings from the first Health Information National Trends Survey. Arch Intern Med. 2005;165:2618–24.
17 Huber JT, Cruz JM. Information needs and information-seeking behaviors of HIV positive men and women. Med Ref Serv Q. 2000;19:39–48.
18 Narhi U. Sources of medicine information and their reliability evaluated by medicine users. Pharm World Sci. 2007;29:688–94.
19 Rutten LJ, Arora NK, Bakos AD, Aziz N, J Rowland. Information needs and sources of information among cancer patients: a systematic review of research (1980–2003). Patient Educ Couns. 2005;57:250–61.
20 Sleath B, Wurst K, Lowery T. Drug information sources and antidepressant adherence. Community Ment Health J. 2003;39:359–68.
21 Lewin SA, Skea ZC, Entwistle V, Zwarenstein M, Dick J. Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database Syst Rev 2001; p. CD003267.
22 Keshishian F, Colodny N, Boone RT. Physician-patient and pharmacist-patient communication: geriatrics’ perceptions and opinions. Patient Educ Couns. 2008;71:265–84.
23 Bultman DC. Evaluation of written prescription information provided in community pharmacies. Final report 2002: Washington, DC.
24 Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens. (Greenwich). 2008;10(5):348–54.
25 Golin CE, DiMatteo MR, Gelberg L. The role of patient participation in the doctor visit. Implications for adherence to diabetes care. Diabetes Care. 1996;19:1153–64.
26 Ley P. Communicating with patients: Improving communication, satisfaction and compliance. 1988, New York: Croom Helm.
27 Arbuthnott A, Sharpe D. The effect of physician-patient collaboration on patient adherence in non-psychiatric medicine. Patient Educ Couns. 2009;77:60–7.
28 (ABPI), A.o.t.B.P.I. Patient information: Advice on drafting of leaflets. 1988: London.
29 Kalichman SC, Benotsch EG, Weinhardt LS, Austin J, Luke W. Internet use among people living with HIV/AIDS: association of health information, health behaviors, and health status. AIDS Educ Prev. 2002;14:51–61.
30 Kalichman SC, Weinhardt L, Benotsch E, DiFonzo K, Luke W, Austin J. Internet access and Internet use for health information among people living with HIV-AIDS. Patient Educ Couns. 2002;46:109–16.
31 Adherence to long-term therapies. Evidence for action. World Health Organization ed. 2003, Switzerland.
32 Chesney M. Adherence to HAART regimens. AIDS Patient Care STDS. 2003;17:169–77.
33 Panel on clinical practices for treatment of HIV. Guidelines for the use of antiretroviral agents in HIV-infected adults and adolescents (NIH 2002). in Morbidity and mortality weekly report. 2002: Atlanta, GA, Centers for diseases control and prevention.
34 Ammassari A, Trotta MP, Murri R, Castelli F, Narciso P, Noto P, et al. AdICoNA Study Group. Correlates and predictors of adherence to highly active antiretroviral therapy: overview of published literature. J Acquir Immune Defic Syndr. 2002;31(Suppl 3):S123–7.
35 Michaud PA, Suris JC, Thomas R, Gnehm HE, Cheseaux JJ; Swiss HIV Mother+Child Cohort Study (MoCHiV). Coping with an HIV infection. A multicenter qualitative survey on HIV positive adolescents’ perceptions of their disease, therapeutic adherence and treatment. Swiss Med Wkly. 2010;140(17–18):247–53.
36 Watermeyer J, Penn C. “Tell me so I know you understand”: pharmacists’ verification of patients’ comprehension of antiretroviral dosage instructions in a cross-cultural context. Patient Educ Couns. 2009;75:205–13.
37 Harmon G, Lefante J, Krousel-Wood M. Overcoming barriers: the role of providers in improving patient adherence to antihypertensive medications. Curr Opin Cardiol. 2006;21(4):310–5.
Funding / potential competing interests: All authors are requested to disclose any actual or potential conflict of interest including any financial, personal or other relationships with other people or organisations within three years of beginning the submitted work that could inappropriately influence, or be perceived to influence, their work. This study did not receive financial support.