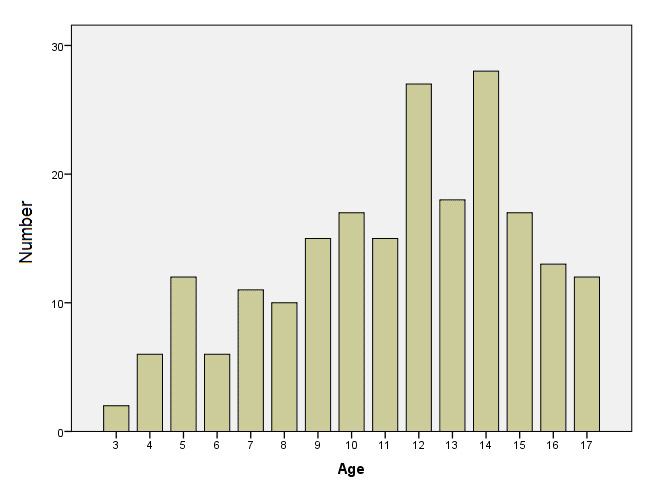
Figure 1
Age distribution (years) of patient cohort.
Mean: 11.3 ± 3.6 years
DOI: https://doi.org/10.4414/smw.2012.13625
Headache is a common problem in children and adolescents affecting some 59% of boys and 84% of girls within the age group of 13–19 years [1]. While there is considerable parental concern that headache in their children is caused by an intra-cerebral space-occupying process, in reality, this is only rarely the case.
Previous reports have stressed the importance of a carefully taken history, and a thorough physical examination rather than any testing in the initial assessment of children with headaches [2]. Nevertheless, imaging studies (cMRI and cCT) as well as neurophysiological studies (electroencephalogram = EEG) are commonly requested diagnostic tests when children and adolescents present with headaches [3, 4].
The aim of this study was to generate up-to-date data on the role of cMRI and EEG studies in the initial evaluation of children and adolescents with headaches. We also correlated risk factors as described bythe Subcommittee of the American Academy of Neurology and the Pediatric Committee of Child Neurology Society with abnormal findings (space-occupying lesions) with findings of cMRI studies [5].
This retrospective study was done in accordance with the policy of the Institutional Review Board and Ethics Committee of the University Hospital of Saarland, Homburg, Germany. Relevant data were retrieved from an electronic hospital database (SAP, Germany). In case of missing data, patients’ hospital charts were hand-searched individually.
We included all children who presented to our neuropaediatric outpatient clinics with “headache” as the main presenting symptom between January 2006 and December 2009. A detailed history was taken and a complete neurological examination was performed.
We entered all relevant information into an electronic database (SPSS 18.0, Chicago, IL, USA). Statistical analysis was performed using SPSS 18.0. For data interpretation we used frequencies and cross-tables. For further statistical analysis the Pearson Chi-Squre Test and Fischer’s exact test was employed. A p-value of ≤0.05 was considered significant.
Headaches were classified according to the second edition of the International Headache Society (IHS) classification, and its modification for the paediatric population [6].
Diagnostic work-up in children with headaches included cerebral MRI studies and EEG recordings as per our hospital protocol. Cerebral MRI studies were performed by a 1.5-T MRI system (Siemens Magnetom Sonata; Siemens; Erlangen, Germany). Electroencephalographic studies were performed using as a standardised protocol as described previously [7]. Electroencephalographic recordings were analysed by an experienced neuropaediatrician (S.M), who was blinded to the findings of cMRI studies.
During the time period 1 January 2001 to 31 December 2009 a total of 818 patients seen in our hospital with a history of headache were entered in our hospital database. These patients were screened for possible study enrolment. Six-hundred and nine of these patients were excluded from study enrolment for one or several of the following reasons: Previous history of headaches (including previous imaging studies), head trauma, age (patients younger than three years of age or older than seventeen years of age), a history of neurosurgery (including obstructive hydrocephalus with ventriculo-peritoneal shunting), other medical conditions with acute onset (most importantly infectious diseases), inadequate/incorrect documentation and data entry, and lack of parental consent to perform cMRI studies. Thus, a total of 509 patients were excluded from the study enrolment.
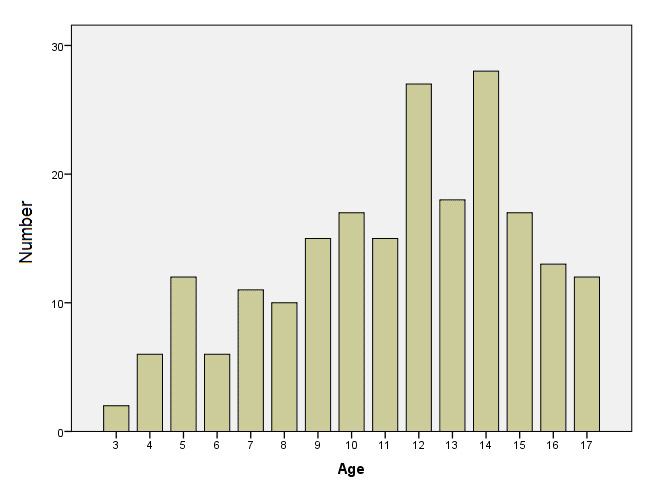
Figure 1
Age distribution (years) of patient cohort.
Mean: 11.3 ± 3.6 years
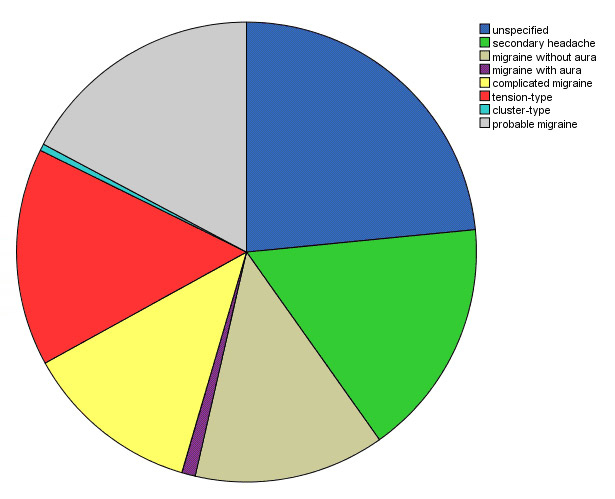
Figure 2a
Type of headache seen in our patient cohort.

Figure 2b
Type of headache seen in our patient cohort depending on gender.
Two-hundred and nine patients were included in this study (age 3 to 17 years, mean age 11.3 years; male 91 (43.5%); female 118 (56.5%)). The age distribution is detailed in figure 1. The following types of headaches were seen: Unclassified headache 49 (23.4%); probable migraine 17.2%, migraine without aura 13.4%, complicated migraine 12.4%, migraine with aura 1.0%; tension-type 15.3%, and cluster headaches 0.5%, and secondary headaches 16.7% (fig. 2a and fig. 2b).
In 44.5% (93) of all children, abnormal findings on physical and neurological examination were noted: Physical and neurologic examination findings (multiple entries possible) included the following in order of frequency: Vomiting (55; 26.2%), syncope (18; 8.6%), speech impediment (13; 6.2%), fever (9; 4.3%), papilloedema 6 (2.9%), gait abnormalities (5; 2.4%), and facial palsy (4; 1.9%). Less common symptoms and clinical signs on neurological examination were: hearing disorder (4; 1.9%), hemiplegic symptoms (2, 1.0%), aphasia, hearing disorder, miosis, amnesia, paralysis, muscle spasms, and taste disorders (each 1; 0.5%). In an additional 32.5% (68) of all children, symptoms like nausea (57; 27.2%), vision disturbance (55; 26.3%), vertigo (45; 21.5%), photophobia (27; 12.9%), phonophobia (17; 8.1%) and paraesthesias (17; 8.1%) were reported. In 55.5% (116) of all children, no physical or neurological signs/abnormalities were seen. All 6 children (n = 6) with papilloedema presented with true papilloedema.
The duration and history of headaches lasted: <1 day (49), 1–7 days (23), 1–4 weeks (31), or longer (56); no data for the duration of headaches could be elicited in 50 patients.
On cMRI studies the following findings were seen: no pathological findings 157 (75.1%), infection of sinuses 15 (7.2%), pineal cysts 5 (2.4%), arachnoidic cyst and Chiari malformation (each 4; 1.9%), unspecified signal enhancement 2 (1.0%), pituitary enlargement, cerebral ischaemia, inflammatory lesion, angioma, and intra-cerebral cyst (each 1; 0.5%).
Electroencephalographic (EEG) findings included: no pathological findings 173 (82.8%), Spike-wave complexes (7; 3.3%), both focal and generalised abnormal slowing (increased delta waves) (11; 5.3%). In 9 EEG recordings (4.3%) artefacts were noted, and unspecified/unspecific findings were seen in (3; 1.4%). Abnormal findings on EEG studies were not linked to abnormal cMRI results.
Consequences that were taken – depending both on clinical grounds and results of imaging studies – included: conservative medical treatment/therapy (10; 4.8%; e.g., anticoagulation for cerebral ischaemia, preventive measures for migraine, and analgesia). In patients with intra-cerebral cysts follow-up cMRI studies were recommended in 11 children (5.3%), antibiotic treatment in 8 (3.8%), further diagnostic investigation 4 (1.9%) (e.g., lumbar puncture and spinal MRI), interventional embolisation (1; 0.5%), operative procedures/surgery in 1 (0.5%). In the first case, the cMRI demonstrated a space-occupying lesion in the left frontal lobe as well as a haemorrhage and oedema compatible with an angioma. The findings of the cMRI correlated with the symptoms of the patient and were most likely responsible for the occurrence of headache. In the second patient, on cMRI sinusitis with an epidural abscess was seen.
Pathological findings on physical/neurological examination were not significantly associated with or predictive of abnormal findings on cMRI studies. Table 1 depicts common findings on cMRI and physical/neurological abnormalities. Also, no single factor (age, length or type of headache, gender) was significantly associated with pathological cMRI results.
| Table 1: Cranial MRI results and most common symptoms in five most common conditions on imaging studies. | |
| MRI results | Symptoms |
| Pineal cyct (5) | Headache, phonophobia, vertigo, paraesthesia, syncope |
| Arachnoid cyct (4) | Headache, vision disturbance, phonophobia, photophobia, vomiting |
| Chiari-malformation (4) | Severe headache, vomiting, nausea, vertigo, photophobia, vision disturbance |
| Unspecific contrast media enhancement (2) | Headache, vertigo, photophobia, phonophobia |
In comparison with previous reports [8–10], our study demonstrated that a substantially higher proportion of children with a history of headaches – presenting to a University neuropaediatric outpatient clinics - demonstrated abnormal findings on both physical and neurological examination. Of note and contrary to previous reports [11] in a substantial proportion of children with headaches it was impossible to classify the type of headaches (“unclassified”). This is likely, or at least in part attributable to the fact that patients were enrolled in this trial at initial presentation with a lack of subsequent serial assessment to better qualify the type of headache.
It is generally assumed that recurrent headaches occur commonly in children and are diagnosed on a clinical basis rather than by any testing. According to current guidelines obtaining a neuroimaging study on a routine basis is not indicated in children with recurrent headaches and a normal neurologic examination [5]. However, in clinical practice, cCT scans or cMRI studies are often performed to rule out an intracranial pathology and for parental re-assurance. In the study by Rho and colleagues neuroimaging procedures were performed in 77.1% of the patients. Overall, 9.3% of these studies yielded abnormal findings with the highest yield in patients with an abnormal neurological examination. Conversely, the rate of pathological findings was low when imaging was carried out in view of changes in the type of headache (12.9%), neurologic dysfunction (10.8%), demands of parent and physicians (10.1%), and recent onset of severe headaches (7.0%). No significant association was seen between abnormality on neuroimaging and age, sex, headache type, age of onset of headache, duration of symptoms before presentation, duration, frequency, location and intensity of headache. Based on their findings the authors conclude that stricter guidelines for rational use of neuroimaging are needed for paediatric headache patients and should be employed. According to the current practice parameters, neuroimaging should be considered in children with an abnormal neurologic examination or other physical findings that suggest central nervous system (CNS) disease. Variables that predicted the presence of a space-occupying lesion included 1) headache of less than 1-month duration; 2) absence of family history of migraine; 3) abnormal neurologic findings on examination; 4) gait abnormalities; and 5) occurrence of seizures [5].
Cerebral CT scanning is a useful diagnostic tool, especially under emergency circumstances, and should be used to identify subarachnoid haemorrhage, ventricular enlargement (e.g., shunt blockage), mass lesion, and haemorrhage secondary to trauma [12]. If, however, the diagnosis of CNS pathology is suspected and the situation is not urgent, MRI at times coupled with angiography (MRA) should be considered. It should be noted that as many as 40% of individuals imaged for headache may have non-specific abnormalities, including abnormalities of the sinuses, non-specific white matter abnormalities, arachnoid cysts, pineal cysts, venous angiomas, and Chiari malformation [13, 14]. Of note, a recent report demonstrated a higher incidence of abnormal findings compared to previous reports when using modern sequences in children with headache; however, there was only limited clinical gain of information using this sequences [15]. This is in line with our results. Conversely, in the series of Chu and Shinnar[16] some 30% of 104 children younger than the age of 7 years who presented with headache underwent imaging. On only one instance, a child with Chiari I malformation, did these studies uncover a previously unknown finding [16]. In the series of Maytal and coworkers, neuroimaging studies disclosed cerebral abnormalities in 3% of paediatric headache patients [8]. All abnormalities were deemed to be unrelated to the presenting complaint [8]. These findings are corroborated by another report that demonstrated that approximately 20% of paediatric headache patients with brain imaging had benign abnormalities that did not result in a change in headache management [17]. Imaging findings that required a change in management were rare in patients with an absence of abnormal neurologic symptoms and signs, occurring only in 1.2% of patients imaged in this study [17]. These findings have been confirmed in children with migraine [18]. This is somewhat in contrast to the results of our study where further treatment was at least in part dependent on the results of cMRI studies in 16.8% of patients; however, in only 2 patients (1%) were intervention or surgery deemed necessary based non cMRI studies. The findings on cMRI in both patients with subsequent intervention/surgery could be well correlated to their physical/neurological complaints, and thus cannot be considered ‘incidentaloma’. Moreover and of importance, the comparatively high number of recommended image re-investigations in our study cohort can at least in part be attributed to medical uncertainty. However, although pineal cysts and arachnoid cysts in the temporal fossa are considered normal variants, they may be causative factors in the development of headaches in children and may mandate further follow-up studies [19]. However, serial follow-up studies – both imaging/EEG studies as well as out-patient visits – were not routinely performed at our hospital for various reasons: a) in most patients one normal MRI finding was considered sufficient to exclude any relevant intracranial pathology, and second, after exclusion of an underlying pathology, many patients were seen at other regional hospitals or were followed-up in private practice. Thus, it was impossible to perform representative long-term follow-up in our cohort.
The question of how to go about finding the rare youngster in whom headache is the first and only sign of an intracerebral tumour has been addressed by several groups, most recently by Straussberg et al., who recommend performing imaging studies on youngsters younger than 4 years of age in whom headache is accompanied by vomiting, even when the neurologic examination is normal [10]. Battistella and colleagues found that headache was the first symptom in 27% of children with brain tumours and the only presenting symptom in 10% [20]. The authors noted that headache associated with brain tumours had a high incidence of projectile vomiting, nocturnal or morning onset, and a lack of triggering factors. Also of note was that rest or sleep failed to relieve pain and that nausea, photophobia, and phobophonia infrequently accompanied headaches associated with brain tumours [20].
It is further noteworthy to mention that contrary to common belief, long pre-diagnostic symptomatic interval or long doctor's delay does not result in decreased survival outcome probability in children with brain tumours [21]. It appears that the effect of tumour biology on survival seems to be dominant and overwhelms any possible opposing effect on survival [21].
Electroencephalographc studies are not recommended in the routine evaluation, as it is unlikely to define or determine the aetiology or distinguish migraine from other types of headaches. Moreover, previous studies have shown that EEG studies are of limited value in the routine evaluation of children with headaches [14, 22]. Non-specific abnormalities are frequently found in normal children as well as in children who are ill. This is in line with our findings where we did not find specific findings in a substantial percentage of children on EEG recordings. Moreover, no association between abnormal EEG studies and pathological findings on cMRI could be demonstrated in our trial. Children undergoing evaluation for recurrent headaches were found to have a paroxysmal EEG, the risk for future seizures is considered negligable; therefore, further investigation for epilepsy or treatments aimed at preventing future seizures is not indicated.
In summary, our results have shown that the rate of pathological findings on cMRI studies in children with headaches of different aetiology is low despite the occurrence of abnormal findings on both physical and neurological examination in a substantial number of children. In the future it will be important to better define those patients who are likely to have an intracranial pathology, and who will benefit from early imaging studies. The additional routine use of EEG studies in the inital diagnostic work-up of children with first-episode headaches is non-contributory to the diagnosis. Moreover, we could not confirm that the variables as defined by the American Academy of Neurology [5] will predict the presence of a space-occupying lesion. This is likely or at least in part to be attributed to the number of patients and the unbalanced distribution (normal and pathological findings) included in our trial. In future trials, a significantly higher number of children and adolescents are required to confirm or discard the possible risk factors and guidelines as suggested by American Academy of Neurology [5]. However, not withstanding the above mentioned recommendations, it is also important to take into consideration parental concerns and fears when deciding to perform a MRI study to exclude an intracranial malignancy/pathology.
1 Zwart JA, Dyb G, Holmen TL, Stovner LJ, Sand T. The prevalence of migraine and tension-type headaches among adolescents in Norway. The Nord-Trondelag Health Study (Head-HUN Study), a large population-based study. Cephalgia. 2004;24:373–9.
2 Lewis DW, Koch T. Headache evaluation in children and adolescents: when to worry? When to scan? Pediatr Ann. 2010;39:399–406.
3 Rho YI, Chung HJ, Suh ES, Lee KH, Eun BL, Nam SO, et al. The role of neuroimaging in children and adolescents with recurrent headaches – multicenter study. Headache. 2011;51:403–8. doi: 10.1111/j.1526-4610.2011.01845.x.
4 Aydin K, Okuyaz C, Serdaroğlu A, Gücüyener K. Utility of electroencephalography in the evaluation of common neurologic conditions in children. J Child Neurol. 2003;18:394–6.
5 Lewis DW, Ashwal S, Dahl G, Dorbad D, Hirtz D, Prensky A, Jarjour I; Quality Standards Subcommittee of the America Academy of Neurology; Practice Committee of the Child Neurology Society. Practice parameter: evaluation of children and adolescents with recurrent headaches: report of the Quality Standards Subcommittee of the America Academy of Neurology; Practice Committee of the Child Neurology Society. Neurology. 2001;27:490–8.
6 Headache Classification Subcommittee of the International Headache Society. The international classification of headache disorders, 2nd ed. Cephalgia. 2004;24(Suppl.):1–151.
7 Oster I, Shamdeen GM, Gottschling S, Gortner L, Meyer S. Electroencephalogram in children with minor traumatic brain injury. J Paediatr Child Health. 2010;46:373–7. Epub 2010 Jun 8
8 Maytal J, Bienkowski RS, Patel M, Eviatar L. The value of brain imaging in children with headaches. Pediatrics. 1995;96:413–6.
9 McAbee GN, Siegel SE, Kadakia S, Cantos E. Value of MRI in pediatric migraine. Headache. 1993;33:143–4.
10 Straussberg RM, Amir J. Headaches in children younger than 7 years: Are they really benign? Arch Neurol. 1993;50:130–1.
11 Deda G, Caksen H, Öcal A. Headache etiology in children: A retrospective study of 125 cases. Pediatrics International. 2000;42:668–73.
12 Dooley JM, Camfield PR, O’Neill M, Vohra A. The value of CT scans for children with headaches. Can J Neurol Sci. 1990;17:309–10.
13 Osborn RE, Alder DC, Mitchell CS. MR imaging of the brain in patients with migraine headaches. AJNR Am J Neuroradiol. 1991;12:521–4.
14 Pavone P, Conti I, Le Pira A, Pavone L, Verrotti A, Ruggieri M. Primary headache: role of investigations in a cohort of young children and adolescents. Pediatr Int. 2011 Dec;53(6):964–7. doi: 10.1111/j.1442-200X.2011.03493.x
15 Streibert PF, Piroth W, Mansour M, Haage P, Langer T, Borusiak P. Magnetic resonance imaging of the brain in children with headache: the clinical relevance with modern acquisition techniques. Clin Pediatr. 2011;50:1134–9.
16 Chu ML, Shinnar S. Headaches in children younger than 7 years of age. Arch Neurol. 1992;49:79–82.
17 Schwedt TJ, Guo Y, Rothner AD. Headache. “Benign” imaging abnormalities in children and adolescents with headache. 2006;46:387–98.
18 Lewis DW, Dorbad D. The utility of neuroimaging in the evaluation of children with migraine or chronic daily headache who have normal neurological examinations. Headache. 2000;40:629–32.
19 Lindner U, Bubl B, Steudel WI, Papanagiotou P, Käsmann-Kellner B, Gortner L, Shamdeen MG. Increased intracranial pressure caused by non-space-occupying arachnoid cysts: report of two patients. Neuropediatrics. 2009;40:89–91.
20 Battistella PA, Naccarella C, Soriani S, Perilongo G. Headaches and brain tumors: different features versus primary forms in juvenile patients. Headache Q. 1998;9:245–8.
21 Kukal K, Dobrovoljac M, Boltshauser E, Ammann RA, Grotzer MA. Does diagnostic delay result in decreased survival in paediatric brain tumours? Eur J Pediatr. 2009;168:303–10.
22 De Romanis F, Buzzi MG, Assensa S, Brusa L, Cerbo R. Basilar migraine with electroencephalographic findings of occipital spike-wave complexes: a long-term study in seven children. Cephalgia. 1993;13:192–6.
Acknowledgement: We thank Holger Nunold for technical help with the manuscript.
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article was reported.
Authors’ contribution: S. Meyer and D. Martens contributed equally to this study.