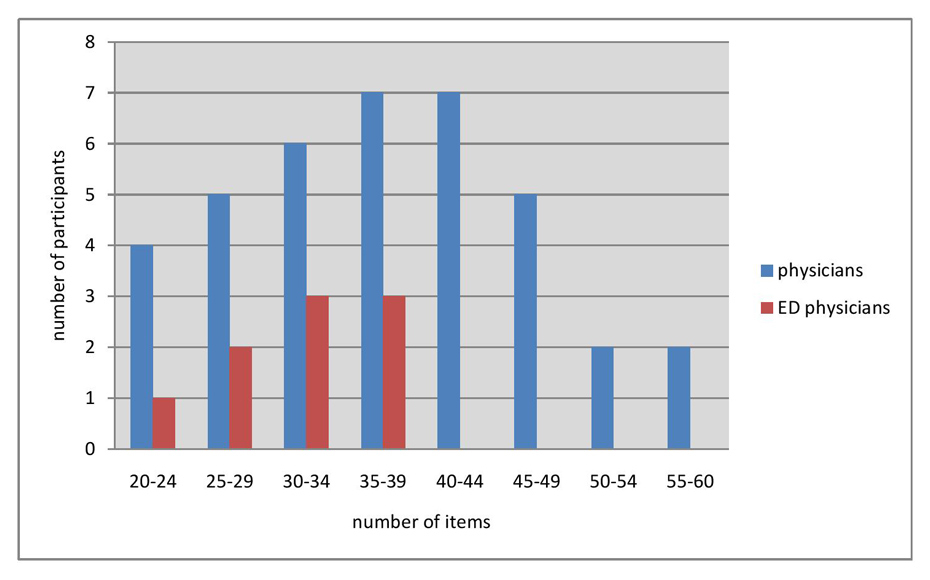
Figure 1
Number of items, chosen by physicians and by ED-physicians respectively.
DOI: https://doi.org/10.4414/smw.2012.13588
Discharge from the emergency department (ED) is a period of high vulnerability for patients [1]; they might run the risk of further clinical deterioration, suffer from a misdiagnosis, if the diagnostic process was not exhaustive, or experience side effects from newly installed drugs [2]. Compounding these risks, deficits in communication and information transfer at hospital discharge are common and may adversely affect patient care [3]. Unfortunately, there is no evidence-based protocol concerning the amount of information physicians should aim to convey to patients. Therefore, the present investigation takes a first step into examining the attributes of good discharge communication. Specifically, we ask physicians to identify the crucial items they would present throughout a discharge communication limited to 15 minutes. The ability to accurately predict the amount of information that can be conveyed in a limited time window is especially important in the context of the busy ED environment, in which a myriad of factors conspire to make patient-doctor communication especially difficult to implement, including unpredictable workload, ED crowding, simultaneous care for multiple patients, high level of uncertainty, time constraints, absence of long-term relationship with patients, and lack of feedback about outcomes of care [4]. Importantly, the practice of emergency medicine is characterised by episodic contact with patients and difficulties in establishing continuous care [5]. Furthermore, in a previous study, ED residents were found to devote far more time and attention to the collection of information than to information giving, suggesting that the latter goal receives less attention [6]. Patients treated in the ED are often presented with complex instructions at discharge [7]. Consequently, a precious opportunity may be missed during which physicians could effectively recapitulate the results of the evaluation in the ED, spell out the final working diagnosis, and recommend follow-up and treatment options [8]. Effective communication during discharge is important because the patient’s degree of accurate knowledge and insight into his or her medical condition is likely to foster compliance, patient satisfaction, adequate disease management and reduce anxiety [9] and the incidence of frequently occurring drug-drug-interactions at hospital discharge [10]. As time is a limited resource in hospitals in general and in EDs in particular, sharing information with patients will inevitably be traded-off with the time requirements of other tasks [11]. Interestingly, there is no empirical basis on which to decide, which information is essential and must be given to patients to keep them well-informed or at least to avoid harm. From the patient’s perspective a definition of crucial information would also be greatly needed. Time, however, is not the only constraint. Human working memory is limited in the number of items it can hold. In his landmark publication, Miller [12] found that humans can recall only seven chunks of information (plus or minus two). Several factors may contribute to even lower memory capacity – Cowan [13] described the “magic four” chunks recalled in a more complex type of memory experiment which is more likely to be representative of the situation in which patients find themselves. Yet, besides these more experimental investigations on general regularities of human working memory, little is known about patients’ ability to subsequently recall instructions received during hospital discharge [14]. A study of Chau et al. [15] showed that even immune-compromised patient’s knowledge of oral drugs at discharge was merely moderate. Using telephone interviews to gauge the ability to recall discharge instructions, another study [14] found that many patients were unable to even name their diagnosis or list risk factors as contributing causes. Examining elderly patients’ comprehension of discharge instructions, a further study found that 21% did not understand their diagnosis, and 56% failed to comprehend their return instructions [16]. Finally, Isaac et al. [17] observed that less than half of the important discharge information, including medication details and indicators of worsening of the patient’s clinical status, was recalled during an exit interview.
These few available findings suggest that there is ample room for discharge communication to be optimised. One component of better communication is for physicians to be well aware of the amount of information that can realistically be conveyed within an available time window. They might select necessary information with the general practitioner in mind, with whom the patient will connect after discharge and who probably is in better position to manage patients’ information and therapy needs in the longer run [18]. In order to examine the extent to which physicians are well calibrated to the amount of information and time needed, we undertook a descriptive preliminary study that probed the number of crucial items physicians, in theory, aimed to cover in a typical discharge communication and the time required to, in reality, do so.
A pilot study was conducted to determine the time taken by emergency physicians to communicate information at discharge. To this end, real episodes of discharge communication were recorded. Each physician was instructed that the respective episode was to be analysed for content; they were not told that time used was also of concern. Having received informed consent from patients and physicians, recordings were transcribed and in fact analysed for the time used. Averaged across 20 episodes involving patients presenting with acute chest pain, discharge communication took 6 minutes. We therefore decided to use the 95% percentile of the distribution of interview times and defined the time limit for the main investigation as 15 minutes.
The study was conducted in a quiet conference room at Basel University Hospital, Switzerland. The hospital is a 700-bed primary and tertiary care university hospital and the ED treats over 41,000 patients per year.
The following case vignette of a common clinical problem was presented to physicians in written form. Subsequently, they answered a questionnaire containing 81 items possible to discuss at discharge (see Appendix). Physicians were asked to first read the case history, and then to choose the crucial items they would aim to communicate during a 15-minute discharge communication:
A 63 year old male patient, accompanied by his wife, presented to the ED because of left-sided chest pain. At presentation he was free of symptoms. Chest pain was associated with exertion (walking uphill, climbing stairs) and subdued when resting. He noted progressive exercise intolerance for the past four weeks. Neither dyspnea nor orthopnea were reported. His past medical history consisted of hypertension, diagnosed 5 years ago, and an ongoing smoking history of 20 pack-years. His father died after a stroke at age 78, and his mother suffered from hypertension and diabetes mellitus II for several years. His present medication consisted of a calcium channel blocker. Even though myocardial infarction was excluded by repeated high-sensitive troponin and electrocardiogram, further work-up was warranted because of typical angina symptoms and a high degree of likelihood of coronary heart disease.
For further work-up a myocardial scintigraphy was planned the following week (date and time known), the recommended therapy consisted of aspirin and beta-blockers; nitroglycerin was given in case of chest pain, and a visit with his family physician was to be scheduled in the meantime.
Independently, seven experts were asked to estimate the time needed for communicating each item featured on the questionnaire. Experts were instructed to only consider the time spent communicating the information and omitting the time consumed by responding to a patient’s questions (examples given in table 1). Estimated times for all items were averaged across the seven experts’ ratings. Then we combined the experts’ time estimates with each physician’s personal selection of crucial items. Specifically, we multiplied, separately for each physician, each selected item with the experts’ mean time estimates for this item. Across a physician’s chosen set of crucial items, we thus estimated the total time required to actually communicate these items.
Out of total of 80 physicians working at University Hospital of Basel, whose specialty (emergency medicine, internal medicine, and cardiology) made them suitable for this study, 47 agreed to participate. From those, 9 worked as emergency physicians and 38 as internists (cardiology staff and internal medicine staff and residents taken together). Experts were chosen by their experience of more than twelve years in the field, and their staff position involving student teaching and training of junior physicians.
Collected data was analysed with SPSS (version 17.0). Mean and range of required time estimates and number of items chosen were assessed for each group. An independent-samples t-test was conducted to assess differences between groups.
| Table 1: Examples of items and the time for information-giving as estimated by experts. | |
| • To specify the suspected diagnosis • To address coronary risk factors | 1 minute |
| • To specify why further examinations are necessary • To explain alternatives to the proposed investigation | 2 minutes |
| • To give information about the differential diagnosis • To explain the association of the symptoms with the suspected diagnosis | 3 minutes |
| • To explain the pathophysiology of coronary heart disease • To give information about the consequences in case of a positive stress test | 4 minutes |
Mean (SD) clinical experience of the 47 physicians was 10.1 (8.3) years. Among these, 9 were currently working as emergency physicians, with a mean (SD) clinical experience of 12.2 (6.5) years. The remaining 38 physicians were working in internal medicine and cardiology (henceforth called “internists”), with a mean (SD) clinical experience of 9.6 (8.7) years. The experts’ mean (SD) clinical experience in the field was 18.1 (7.7) years.
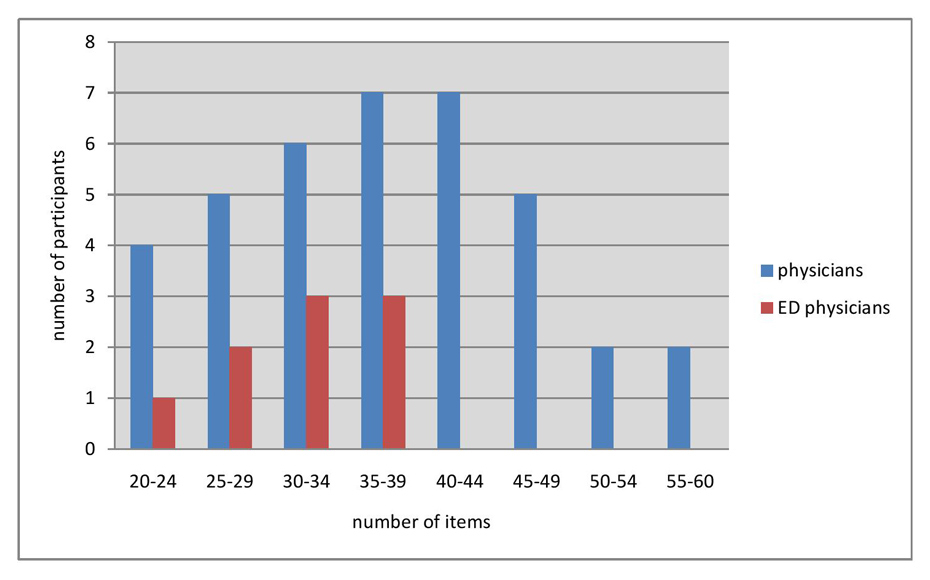
Figure 1
Number of items, chosen by physicians and by ED-physicians respectively.
Out of the 81 items provided, an overall mean (SD) of 36.3 (9.8) was chosen (45%), with a range of 20 to 57 items. Mean (SD) estimate of the time required to communicate these items was 44.5 (12.8) minutes (range 25–74 minutes).
As shown in table 2, the mean (SD) number of items chosen by internists was 37.4 (10.2), and 31.6 (6.2) chosen by emergency physicians, respectively. The difference between the two groups proved to be not statistically significant (t (45) = 1.64, p = 0.11, d = 0.41 ). The distribution of the number of items, chosen by internists and by emergency physicians, respectively, is shown in figure 1.
The mean (SD) time derived for communicating the discharge information, selected by the physicians, amounted to 46.4 (13.5) and 36.9 (6.3) minutes for internists and emergency physicians, respectively (table 2). This is 3.1 and 2.7 times longer than the preset time window for the task of discharge communication. This difference between groups proved to be significant (t (45) = 2.04, p = 0.047, d = 0.73).
| Table 2: Results. | |||
| Mean | SD | ||
| Internists (38) | No of items chosen Time needed (min) | 37.4 46.4* | 10.2 13.5 |
| Emergency physicians (9) | No of items chosen Time needed (min) | 31.6 36.9* | 6.19 6.34 |
| *p <0.05 | |||
According to our findings, physicians from different specialties (internal medicine, cardiology, and emergency medicine) choose a large number of items deemed necessary to be given to a patient with chest pain at discharge from the ED. Even though study participants were told to choose items that could be given within a 15 minutes interaction, the time most likely needed to give this amount of information exceeded the time previously set by a factor of three (45 vs.15 minutes, the latter being instructed in written and oral form). First of all, these results show that defining relevant items is a difficult task with experienced physicians choosing quite different items, and that the average number of items most likely is way beyond the capacity of typical patients to recall information. These results are all the more impressive as in reality discharge communications are likely to be even shorter than the time window we presently assumed. A study analysing audiotaped ED discharge communications observed an average length of 76 seconds (range 7 to 202 seconds) [6]. Our own pilot study, based on a small sample of 20 communications, found an average duration of 6 minutes. Furthermore, the number of crucial items selected by physicians far exceeded the amount of information humans could be expected to process and retain, assuming normal working memory capacity. Taken together, these findings suggest that our physicians had unrealistic expectations concerning the amount of information that could be crammed into a 15-minute window dedicated to convey important information to the patient. The extent to which our physicians proved to be miscalibrated is surprising in light of the fact that discharge communication represents a routine activity for all our participants.
Even though the literature on patient information has yielded different figures, it is practically impossible that any patient will recall 36 pieces of information. Here, the problem is not so much that some items get lost, the problem is that it is unknown which items are recalled and which ones are forgotten; if this is a random process, there is a good chance that a potentially life-saving piece of information is lost. This study adds to our knowledge by demonstrating that besides training programs teaching the art of giving information, clinicians have to decide which information is so relevant that it must be remembered by patients; this should be shorter than the list of over 30 items chosen by experienced physicians in this investigation. How such a reduced list of items should then best be communicated remains to be shown and will require further research. However, to the best of our knowledge, the process of advanced planning of a discharge communication and the process of determining the amount of information to be conveyed and the time needed to do so has not been studied.
In stark contrast to the scarcity of research about real patients’ ability to recall information provided during ED discharge, memory capacity in healthy volunteers has been extensively studied. Although the precise bounds of working memory are still discussed, the fact that its capacity is limited, is undisputed, ranging from 7 ± 2 [12] to 4 ± 2 chunks [13]. In light of these mnemonic limits, it is notable that the physicians in our study selected, on average, 37 (internists) and 32 (emergency physicians) items, respectively, to be communicated. The majority of these items were quite complex in nature, possibly encompassing more information than could be grouped into a memory chunk (e.g. the item “Stress the importance of returning to the ED immediately if the patient experiences chest pain not responding to nitroglycerine”).
Studies from the US have shown that written discharge information might not be the best solution: For example, a well conducted study [19] in which oncologists randomised patients into a control group receiving oral discharge information, and an intervention group receiving personalised, written discharge information, found that the median (range) number of recorded items per patient was 5 (4–9) in the control group and 6 (3–13) in the intervention group, the difference being insignificant! The factors associated with patient’s recall were the mean time used for each item (1.2 min for recalled items), and the content. E.g. smoking cessation was recalled as an item discussed in 76% of all smoking patients, whereas only 11% recalled being instructed about medication.
However, available studies have not examined ED discharge communications, in which physicians usually focus on immediate needs, and the decisions about what information will be conveyed are made in a rather ad hoc manner. One of the urgent future research questions is why experienced physicians, who were unambiguously and repeatedly instructed to plan for a typical 15 minute discharge communication, chose on average over 30 items. Actually conveying this lengthy list of items would either have taken much longer than the allotted time window or the communication would have morphed into a staccato speech. We can only tentatively offer the explanation that the selection of items physicians actually communicate is not a conscious process after careful consideration of the importance of single items. It is well possible that in reality physicians mention what comes to their mind; apparently this takes 6 minutes in our pilot study (with 95% percentile of 15 minutes) – the amount of necessary information increasing only when they are asked to deliberately choose from a given list of items. Even if our experts grossly overestimate the time per item and physicians could actually communicate all of them, the sheer number clearly exceeds the limits of normal working memory capacity. A final disconcerting possible implication of our findings is that, assuming that physicians simply cannot cram 36 items into a window of 15 minutes, physicians communicate less information than they ideally would like to convey.
Clearly, further research is needed to define the ideal quantity and quality of discharge information in the ED by means of outcome studies – the present preliminary report contributes a first step in this direction, highlighting the necessity to realistically plan daily discharge communications.
First, one might argue that the situation in which physicians chose relevant items was artificial insofar as no patient was present and as they were sitting in a quiet room sheltered from the busy atmosphere of an ED. However, if they made their choice under conditions that allow for careful consideration, is it likely that any decision made under time pressure would be more rational? Presenting a menu of 81 items from which physicians could choose may have tempted physicians to select more than they otherwise would have selected. In order to try to address this possibility, we have conducted the same analysis with another sample of 9 physicians using a shorter list of 37 items, encompassing items that were chosen by the majority of participants. We found that the mean number of items selected from this reduced list was 25 (range: 17–30), a number still exceeding working memory capacities of most patients.
Second, physicians in Switzerland (and elsewhere) cannot be expected to have profound knowledge of psychology’s research on memory and memory limitations. Therefore, the comparison between what physicians would ideally like to communicate and what patients can be expected to process may seem harsh. Yet, the comparison is informative because it indicates a potential mismatch between physicians’ ideal of information giving and the reality of patients’ limited information processing capacity.
Third, a potential bias is the selection bias: Perhaps, those physicians who were motivated enough to participate were also more vulnerable to act in accordance with concerns of social desirability. Such a concern could simultaneously foster the selection of a larger number of items. Therefore, it would be informative to replicate our study with larger and other samples of physicians in Switzerland and elsewhere.
Taken together, external validity may be questioned by all factors mentioned above – therefore, larger samples in different ED environments should be analysed.
The present study suggests a possible need for training on all levels (residents and staff physicians, cardiologist, internists, and emergency physicians alike) concerning the amount of information to be ideally conveyed in discharge communication. The available literature gives some preliminary hints to the ideal quantity of information. Notwithstanding this generic information, more targeted studies are needed on several levels: First, observational studies could help to describe the actual time (across different medical systems) physicians devote to discharge communication. Second, the ability to recall discharge information needs to be investigated in patients discharged from the ED. Third, and most importantly, studies assessing meaningful outcomes, such as the use of resources (overuse due to increased anxiety versus underuse due to “overconfident” patients), or even morbidity and mortality are required to determine the quantity and quality of information to be given at ED discharge. This preliminary report may help to ignite more research along these lines.
1 Samuels-Kalow ME, Stack AM, Porter SC. Effective discharge communication in the emergency department. Ann Emerg Med. 2012. Epub 2012/01/10.
2 Kripalani S, Jackson AT, Schnipper JL, Coleman EA. Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J Hosp Med. 2007;2(5):314–23. Epub 2007/10/16.
3 Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297(8):831–41.
4 Eisenberg E, Murphy A, Sutcliffe K, Wears R, Schenkel S, Rerry S, et al. Communication in emergency medicine: implications for patient safety. Communication Monographs. 2005;72:390–413.
5 Logan PD, Schwab RA, Salomone JA, 3rd, Watson WA. Patient understanding of emergency department discharge instructions. Southern medical journal. 1996;89(8):770–4. Epub 1996/08/01.
6 Rhodes KV, Vieth T, He T, Miller A, Howes DS, Bailey O, et al. Resuscitating the physician-patient relationship: emergency department communication in an academic medical center. Ann Emerg Med. 2004;44(3):262–7.
7 Zavala S, Shaffer C. Do patients understand discharge instructions? J Emerg Nurs. 2011;37(2):138–40. Epub 2011/03/15.
8 Vashi A, Rhodes KV. “Sign right here and you’re good to go”: A content analysis of audiotaped emergency department discharge instructions. Ann Emerg Med. 2010.
9 van der Meulen N, Jansen J, van Dulmen S, Bensing J, van Weert J. Interventions to improve recall of medical information in cancer patients: a systematic review of the literature. Psychooncology. 2008;17(9):857–68.
10 Bertoli R, Bissig M, Caronzolo D, Odorico M, Pons M, Bernasconi E. Assessment of potential drug-drug interactions at hospital discharge. Swiss Med Wkly. 2010;140:w13043. Epub 2010/04/08.
11 Scott A, Watson MS, Ross S. Eliciting preferences of the community for out of hours care provided by general practitioners: a stated preference discrete choice experiment. Soc Sci Med. 2003;56(4):803–14.
12 Miller GA. The magical number 7, plus or minus 2 – some limits on our capacity for processing information. Psychol Rev. 1956;63(2):81–97.
13 Cowan N. The magical number 4 in short-term memory: A reconsideration of mental storage capacity. Behav Brain Sci. 2001;24(1):87-+.
14 Sanderson BK, Thompson J, Brown TM, Tucker MJ, Bittner V. Assessing patient recall of discharge instructions for acute myocardial infarction. J Healthc Qual. 2009;31(6):25–33; quiz 4.
15 Chau I, Korb-Savoldelli V, Trinquart L, Caruba T, Prognon P, Durieux P, et al. Knowledge of oral drug treatment in immunocompromised patients on hospital discharge. Swiss Med Wkly. 2011;141:w13204. Epub 2011/06/28.
16 Hastings SN, Barrett A, Weinberger M, Oddone EZ, Ragsdale L, Hocker M, et al. Older patients’ understanding of emergency department discharge information and its relationship with adverse outcomes. J Patient Saf. 2011;7(1):19–25. Epub 2011/09/17.
17 Isaacman DJ, Purvis K, Gyuro J, Anderson Y, Smith D. Standardized instructions: do they improve communication of discharge information from the emergency department? Pediatrics. 1992;89(6 Pt 2):1204–8. Epub 1992/06/01.
18 Cooley WC, McAllister JW, Sherrieb K, Kuhlthau K. Improved outcomes associated with medical home implementation in pediatric primary care. Pediatrics. 2009;124(1):358–64. Epub 2009/07/01.
19 Damian D, Tattersall MH. Letters to patients: improving communication in cancer care. Lancet. 1991;338(8772):923–5.
Funding / potential competing interests: Financial support by the Scientific Fund of the Emergency Department, University Hospital Basel, Switzerland