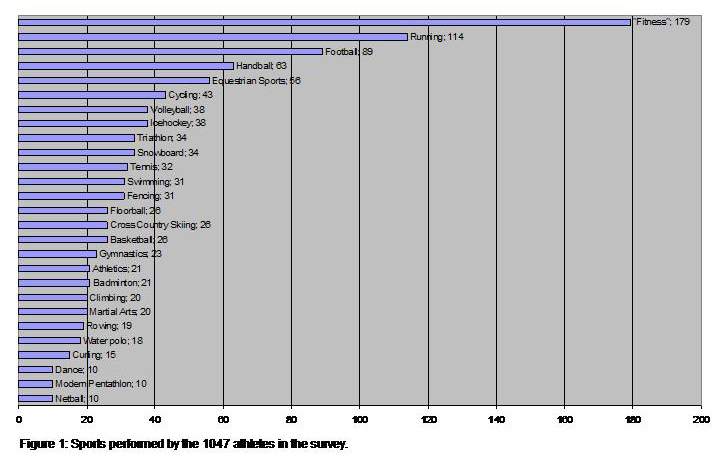
Figure 1
Sports performed by the 1047 athletes in the survey.
DOI: https://doi.org/10.4414/smw.2012.13575
Current situation in competitive athletes and short follow-up assessment of an exemplary local screening programme
Cardiac prevention in athletes is a major issue of rising medical and public interest. Within the last years, the awareness of cardiac screening programmes for athletes has increased continuously. In particular, this is due to the occurrence of sudden cardiac deaths (SCD) in athletes during sports activity. With a yearly incidence of about 1–3 SCD per 100,000 young athletes (age <35 years) [1, 2], such fatal events might appear relatively rare. However, the incidence of SCD increases undoubtedly in specific subgroups of athletes; indeed in older and un-trained, previously sedentary individuals the incidence may be as high as nearly 7 deaths in 100,000 individuals per year [3, 4]. In some surveys the epidemiologic relevance of the screening for SCD in sports was further supported by cost-effectiveness analysis [5]. Due to the fact that these tragic events are of large, emotional consequences, many sports associations and teams have recently established standardised screening concepts [5–9].
Indeed, particularly in young athletes, cardiac baseline screening appears very simple and feasible. Primarily based on the evidence of large studies from Italy, where cardiac screening of competitive athletes has been established for decades, screening recommendations in young competitive athletes have been defined [6, 10–14]: In general, such recommendations consist of 3 standard baseline tools: History (personal and family history), clinical examination and 12-lead resting ECG.
In the case of suspicious findings in any of the tools, follow-up examinations are indicated (e.g., echocardiography, exercise test, etc.). The efficacy of this simple concept appears convincing as the vast majority of sports-associated cardiac deaths could thereby be avoided [11, 14]. Of note, in the large Italian cohort of competitive athletes, which has been observed for decades, the cardiac mortality decreased dramatically by almost 90% after implementation of a cardiac pre-competition screening [11, 14].
However, what is the current situation in Switzerland? In 1998, the Swiss Society of Sports Medicine (SGSM) published and declared their recommendations for the prevention of SCD in sports, which was quite early, particularly when compared to other European countries. These adapted recommendations have been reinforced lately [15]. However, these guidelines particularly target top-level athletes. As such, athletes competing in a national squad are regularly followed up. However, the awareness of the problem does not seem to be well established in the enormous group of competitive athletes who are not integrated in an Olympic- or other high-level squad. Although some sports associations and teams have adopted the national and international recommendations, the current guidelines are not mandatory. By making use of the preliminary experience of the SGSM and the well established “Swiss Olympic” screening strategy of top-level athletes, our aim was to improve the awareness of the problem of sudden cardiac death in sports in the enormous group of “non top-level” competitive athletes. If this gap could be closed, a comprehensive Swiss cardiac pre-competition screening concept that integrates all competitive athletes irrespective of their competitive level can be established [9]. Therefore, we designed our stepwise survey to gain two different sets of results Firstly, we analysed the current situation concerning pre-competition screening in a large sample of competitive but not top-level athletes by using a detailed questionnaire, which was answered by more than 1000 athletes. Our aim was to determine the needs and expectations in this underestimated subgroup. Secondly, and based on our survey, we designed and implemented an exemplary local screening programme to test its feasibility and acceptability.
In a first step, a total of 1,047 competitive athletes participating in various sports, and of different ages and gender were contacted by phone call, e-mail or mail (informed consent). To ensure representativeness, we first contacted sports-specific organisations (associations, clubs or teams) which lead us to a certain number of individual athletes to whom the questionnaires could be distributed. Furthermore, the questionnaire was answered by competitive athletes studying at the University of Zurich (by personal request). The main inclusion criteria was the regular performance of competitive sports and our particular focus was set on the essential group of competitive athletes, not integrated in an Olympic- or other high-level squad. If the athletes agreed to participate, a standardised questionnaire was passed on to them (Appendix 1 http://www.smw.ch/fileadmin/smw/images/SMW-13575-Appendix-1.pdf ). The questionnaire was designed to answer two essential questions: Firstly, the personal and sports-specific profile of the individual athlete, and secondly the personal point of view concerning a quasi ”ideal conception” of a cardiac screening in athletes. Within only a few minutes all questions could be answered by the participant (Appendix 1 http://www.smw.ch/fileadmin/smw/images/SMW-13575-Appendix-1.pdf ).
In a second step (and based on our results), an exemplary local screening-programme was implemented at the “Academic Sports Association Zurich” (ASVZ) in Zurich, Switzerland to test its feasibility and validity. The main facilities which were used for the examinations, were located at the “Eidgenössische Technische Hochschule” (ETH) in the city centre of Zurich, Switzerland. The ASVZ is the largest university sports association in Switzerland with more than 45,000 athletes performing. However, before this study, a regular cardiac pre-competition screening was lacking. The programme, which consisted of the internationally established cardiac baseline screening (personal and family history, physical examination, 12-lead resting ECG), was announced in the official ASVZ-journal [16] and published on the homepage as well as in the official “sports schedule” (hardcopy form). Every competitive athlete performing at the ASVZ could apply for the screening. The only exclusion criteria was the performance of leisure sports (which none of the athletes met). After registration at the information desk, at least one day before the screening, a maximum of 4 athletes were examined by the same physician, a consultant in Cardiology, Internal Medicine and Sports Medicine, with specific knowledge in the field of Sports Cardiology (CS). These examinations took place every Tuesday (during lunch breaks). The 12-lead ECGs were assessed according to the current recommendations of the European Society of Cardiology [17] and acquired on a Schiller AT-101 (©Schiller AG, Baar, Switzerland).
After one year, the feasibility and validity of this screening concept and the data collected during the programme were assessed. Statistical analysis was performed using paired t-tests. The significance level was set as p <0.05. Statistical analysis was performed using standard statistical software (SPSS version 16.0, Inc, Chicago, IL). Data are given as median (range) unless stated otherwise.
The polled athletes (n = 1,047) participated in the following competitive sports: badminton, basketball, curling, ice hockey, fencing, “fitness” (unspecific but mainly endurance based with regular competition; e.g., long-distance running), football (soccer), gymnastics, handball, martial arts, climbing, netball, cross country skiing, running, athletics, modern pentathlon, equestrian sports, cycling, rowing, swimming, snowboarding, dance, tennis, triathlon, volleyball, floorball and water polo (fig. 1). The vast majority of the respondents, namely 85%, were quite experienced and had performed regular competitive sports for more than 2 years. 30% performed sports for at least 7 hours per week (or more). A total of 56% of the athletes practiced individually and 43% competed within a team, while 16% did both.
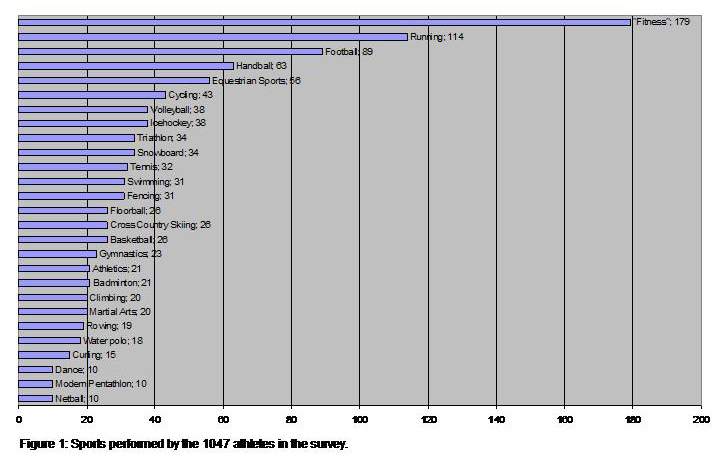
Figure 1
Sports performed by the 1047 athletes in the survey.
Only 9.2% (n = 96) of the athletes had previously participated in a cardiac pre-competition screening. Only 47% of the athletes considered a cardiac pre-competition screening necessary while 53% were not interested in such a programme. The age range of the polled athletes (n = 1,047) was between 13 to 64 years (median age 22 years, SD = 5.87) and the acceptance increased significantly with advancing age (p = 0.015). The sample was quite homogenous concerning gender ratio (49% were females and 51% males), but female athletes exhibited significantly lower interest for a screening compared to male athletes (44% vs. 51%, p = 0.029).
A significant correlation between the duration of regular exercise and a positive acceptance of cardiac screening (more than 25 months versus less than 25 months: p <0.01) was found. Furthermore, the number of weekly training hours also correlated positively with the acceptance of regular pre-competition screening.
More than 62% of the athletes who performed sports for at least 7 hours per week were interested to undergo a regular screening, while only 41% of those who performed less than 7 hours weekly accepted such a strategy.
Athletes performing sport within a team tended to support pre-competition screening more frequently (53%) than those who performed individual sports (46%). However, this difference did not reach statistical significance (p >0.05).
All of the athletes were prepared to pay a fee for a cardiac screening programme. Around two thirds of them (64%) were prepared to pay a maximal participation fee of 60 CHF, a range that is consistent with the established international standard [11, 14, 26]. However, the rest of the athletes agreed to pay more: up to 100 CHF (28.8%) or more than 100 CHF (7.2%).
Almost half of the athletes (49.2%) would only participate in a programme nearby at a travelling distance of within 10 kilometres, while 43% would accept a distance of 10 to 50 kilometres. Only 8% would consider programmes more than 50 kilometres away.
Based on our results, we proposed specific measures of a nationwide cardiac screening programme for competitive athletes (table 3).
Respecting these measures, we implemented and assessed an exemplary screening programme at the “ASVZ” in Zurich, Switzerland. Following the start of the screening programme in summer 2010, a total of 102 athletes underwent the screening during the first year. The median age of the athletes was 34 years (range: 20 to 68). A total of 69.6% (n = 71) of the participants were male while only 30.4% (n = 31) were female.
The motive to sign up for the screening was a current symptom or concern for the vast majority of athletes (82 athletes; 80.4%). Therefore, only 19.6% went through the cardiac pre-competition screening with the intention for a “routine check-up”. The vast majority of the participants without symptoms or concerns were female athletes (n = 18 or 90% of the athletes without symptoms).
According to the official questionnaire of the International Olympic Committee (IOC)/”Lausanne Recommendations” (2) only 13.3% of the athletes showed unsuspicious findings, while 86.7% gave positive answers (e.g., arrhythmic pulse 25%; light-headedness 6.9%; thoracic pain 9.7%) and 4.8% of the athletes smoked regularly.
In more than half of the athletes (54.2%) the family history was uneventful. In 45.8% positive answers, such as sudden cardiac (or unexpected) death (13.4%) or coronary heart disease/myocardial infarction (14.6%) were noted.
The median resting heart rate was 62.6bpm (range: 36 to 92bpm). Two athletes showed uncontrolled hypertension, being known but inadequately controlled hypertension in one case and newly diagnosed (severe) hypertension in another case. All other athletes with initially (mildly) elevated blood pressure showed values in a normal range after repetitive measurements. In 47% of the athletes a (systolic) heart murmur could be detected. This prevalence corresponds to our estimation according to former surveys (18). In athletes with loud or fixed systolic murmurs an echocardiography was performed (10%, n = 10). Only one of these athletes, however, showed a relevant finding (i.e. atrial septum defect, see below).
Although about 7% of the athletes showed some of the “Ghent” stigmata for Marfan’s syndrome, none proved to sufficiently fulfil these criteria (19, Ghent-Criteria).
The ECG findings were differentiated into “common, sports-related changes” and “rare changes, that are mainly not related to sports”, according to the current recommendations of the Sports Cardiology Section of the European Society of Cardiology [17], (table 1 and 2). A total of 27 athletes (26.4%) with suspicious clinical and/or ECG findings were followed up by echocardiography, an exercise stress test and/or a flecainide test in case of Brugada-like ECG pattern. In all but 5 cases (4.9%) the athletes could later be declared eligible for competitive sports. One athlete with a suspicious systolic murmur, a fixed splitting of the second heart sound and an incomplete right bundle branch block, proved to suffer from atrial septum defect (ASD). The shunt appeared to be haemodynamically relevant with enlargement of the right ventricle. There was another suspicious ECG (complete right bundle branch block and left anterior hemiblock) that proved to correlate with a hereditary AV channel defect. An athlete with suggestive family history of Brugada syndrome and suspicious resting ECG underwent multiple additional testing without positive findings.
| Table 1: Physiologic ECG findings during cardiac screening at the “ASVZ”. | ||
| n | % overall | |
| Sinus Bradycardia | 31 | 30.4 |
| 1° AV block | 19 | 18.6 |
| Incomplete RBBB | 14 | 13.8 |
| Isolated QRS high voltage | 23 | 22.4 |
| ST elevation | 7 | 6.9 |
| Table 2: Suspicious and potentially pathologic findings during cardiac screening at the “ASVZ”. The T wave inversions are differentiated according to their localisation. | ||
| n | % overall | |
| T wave inversions | 13 | 12.7 |
| anterior (V1-V4) | 10 | 9.8 |
| Inferior | 2 | 1.9 |
| Lateral | 1 | 1.0 |
| Left axis deviation/LAHB | 1 | 1.0 |
| Complete Right Bundle Branch Block | 1 | 1.0 |
| Brugada-like Pattern | 4 | 3.9 |
| WPW/short PQ | 11 | 10.8 |
| Table 3: Recommendable measures for a “Swiss cardiac screening programme for competitive athletes”. |
| 1. The ”Swiss Screening Concept” should be implemented as soon as possible and structured according to the established guidelines of the ESC (e.g. start of screening at the age of 12 to 14 and repeated every 1 to 2 years). |
| 2. The programme should be equally accessible for all competitive athletes. |
| 3. On principal, the screening should be voluntary. |
| 4. Voluntariness makes comprehensive information about the problem of SCD in sports mandatory. Thereby, the athletes may adequately base their decision on self-responsibility. Of course, associations and clubs can determine whether or not they require an unsuspicious cardiac screening for the licensing of their members. |
| 5. The programme should be based on a “Swiss Sports Cardiology Network”. |
| 6. It should be cost-effective for athletes as well as for public health. |
Although the SGSM already published recommendations in 1998 [15] and a network of especially assigned “Swiss Olympic” medical centres and bases provide extensive medical care for high-level athletes and members of “Olympic squads”, a comprehensive and nationwide approach integrating all competitive athletes is still lacking, particularly concerning the relevant group of ambitious amateur-athletes (nonetheless performing competitive sports).
In the current study we analysed a survey completed by 1,047 competitive athletes, not integrated in an Olympic- or other high-level squad, on pre-competition screening and defined recommendable measures for an optimal Swiss cardiac screening concept which integrates these athletes (table 3). Our hypothesis that this particular group of athletes is massively undertested regarding cardiac screening was confirmed. Only 9% of the competitive athletes participating in the survey had previously undergone cardiac screening although they were at relevant risk for sports-associated SCD and would qualify for a regular screening according to the European recommendations [6]. This fact is alarming and underlines the urgent need for action in this particular group of athletes.
However what are the reasons for this obvious disregard of internationally accepted guidelines?
Firstly, it is a distinct question of definition, as many athletes and sports physicians might not be aware that the particular risk of sports-associated SCD is not strictly dependent on the training level of a competitive athlete. It is the competition an athlete is exposed to that makes the individual risk for SCD increase dramatically compared to pure leisure-time sportspersons [21]. As such, a “pyramidal-like” concept, with a more elaborate screening only for athletes of an increased level [20] does not seem appropriate. Lower-level athletes in marginalised but competitive sports would be particularly disadvantaged. Competitive athletes are exposed to an increased cardiac risk due to the intensity and constancy of performing sport, and the psychological strain to which they are exposed to. However, the definition of competitive sports is not self-evident. Maron and his working group came to the following definition (2004): “A competitive athlete is one who participates in an organized team or individual sport that requires systematic training and regular competition against others and that places a high premium on athletic excellence and achievement.” [21].This definition, however, is quite vague and technically includes the majority of physically active individuals and particularly the enormous group of competitive but not top-level athletes. As a consequence, we propose to use the term “non-competitive” only if used equivalent to “leisure sports”, whereby people perform physical exercise for pure pleasure and without any physical and/or psychological stress. Most likely, such individuals would not need a specific screening. Nevertheless, pre-competition assessment and screening should immediately be provided if such “leisure-sportspersons” suddenly and spontaneously perform in competitive situations (e.g., charity sport-events, marathons etc.). Recently, these events have constituted a certain “modern lifestyle” for many. Indeed, SCD has been reported in recent marathon events [22]. A recently published review especially focussed on the contemporary phenomenon of “occasional competitive athletes” [5, 23].
For a better understanding of the low number of regularly screened “non top-level” but competitive athletes another impressive finding of our survey has to be accentuated: The overall acceptance rate of a cardiac screening was unexpectedly low. Not even half of the athletes supported a regular cardiac pre-competition screening. On the one hand this suggests a certain need of self-determination of many athletes that surely has to be respected. However, voluntariness requires that the decision of the individual athlete is informed and that comprehensive information about the risk of SCD in sports is available. Although we did not specifically assess the screened athletes satisfaction (e.g., by questionnaire), a short feedback was requested after each screening session at the ASVZ. These closing remarks suggested a great acceptability of the screening concept and after a few weeks most of the following assignments were achieved by personal recommendation and word of mouth. This supports the presumption that the uncommonly low acceptance rate can also be explained by an insufficient awareness of the risk of SCD in sports. As such, the vast majority of athletes assigned for a screening at the ASVZ due to a specific concern or symptom. This fact indicates that our exemplary cardiac screening programme may only have lowered the threshold to a doctor’s visit which would have taken place anyway. The major aim of the screening should be the detection of clinically silent but potentially harmful cardiac conditions, as most of them appear to be asymptomatic [1, 11, 24, 25]. To improve and assure sufficient information and awareness of the issue, elaborate education campaigns are crucial and should be implemented locally but based on a comprehensive national concept, supported by the government as well as by sports and medical associations.
As our data indicates, certain subgroups of competitive athletes should be particularly targeted by such educational programmes. Older athletes are more likely to participate in regular cardiac pre-competition screening, a fact that was reproduced in our screening programme at the ASVZ where the average age of the athletes was quite high (34 years). Other than the age of an athlete, there was a positive correlation between the weekly training effort and the acceptance of a regular cardiac screening. Furthermore, it appears that screening in a team-setting seems to improve the awareness and acceptance significantly. In our survey, only about one third of the athletes that signed-up for our screening programme at the ASVZ were females. However, it cannot simply be concluded that female athletes exhibited significantly lower interest in screening as the reason for male athletes to sign up for the ASVZ programme were current symptoms or concerns in about 80%, and the number of female athletes performing at the ASVZ was lower than the number of male athletes. Nevertheless, this mismatch may also be related to the well known, striking male-gender preponderance for SCD in sports [1, 2]. Not only in developing countries where many young athletes aim for seductive sporting careers, many athletes are also afraid of disqualification by the screening [9]. However, it has to be clearly noted that it should not be the primary aim to disqualify athletes for good. In fact, a tailored medical support should help to assess and treat a cardiovascular disease and provide reasonable recommendations and follow-up regarding further sporting activity. Thus, although 5 athletes were declared as “not eligible” for competitive sports during the ASVZ screening (due to haemodynamically relevant ASD, suspected Brugada syndrome, AV channel defect and hypertension), all of them could be treated adequately and finally all of them will be able to participate in certain competitive sports in the future. This “supportive” approach needs to be outlined to avoid unnecessary and potentially fatal reservation of an athlete or official confronted with the screening.
Based on the results of our large survey, strategies to further improve the established cardiac screening concept in Switzerland can be outlined (see also table 3).
One major aim should be the integration of the large but currently “under-screened” group of competitive Swiss athletes who are not performing in an Olympic- or other high-level squad, where complementary screening programmes are already well established. These “non top-level” competitive athletes need to be reached and thoroughly informed but they also need a valuable “port of call” to undergo the regular follow-up screenings. As such, a comprehensive and nationwide approach should be achieved by a specialised Sports Cardiology network involving certified Cardiologists with specific knowledge in Sports Medicine (“Sports Cardiologists”), undergoing regular and standardised education and providing a comprehensive and standardised Swiss screening programme. Regular meetings, newsletters and a “linked” internet based information platform are important tools in this setting ( http://www.sportkardiologie.ch ). This high-level cardiac care is obviously crucial to prevent fatal events of SCD [6, 8]. Our representative sample of athletes would definitely endorse such a concept. However, based on our survey, a relatively “close meshed net” should be envisaged, as most athletes would only participate in programmes nearby, at a travelling distance of within 10–50 kilometres. Of course, the involvement of the SGSM and the established “Swiss Olympic” medical care system is crucial in this network-concept. A multidisciplinary approach was already established in Switzerland, a few years ago, with patho-anatomical and molecular biological autopsy being a decisive factor in the prevention of exercise-related SCD, with a major impact on the athletes and their families [27].
Additionally, the “Sports Cardiology Network” could provide widespread basic information to athletes, teams, clubs and sports associations based on the local “network cardiologist”.
Whether or not screening programmes for competitive athletes should be mandatory, is questionable. In Italy, where cardiac screening of competitive athletes has a long-standing tradition, such preventive examinations are mandatory by law. Indeed, every competitive athlete has to undergo this screening repetitively every 1 to 2 years starting at the very beginning of their career, at the age of 12 to 14 years, in order to get and/or maintain licensing [11, 14]. Such repetitive examinations definitely make sense, as many cardiopathies develop only during adolescence or adulthood [1, 4, 6, 12, 15]. In Switzerland, such a concept, however, appears unrealistic. Although the sports scene may be predictable and the group of competitive athletes is comparatively small, the administrative and logistic requirements would be substantial. As mentioned before, voluntariness of cardiac screening, particularly in “non top-level” sports however presupposes comprehensive information and education strategies targeting all competitive athletes irrespective of the kind sport, location or gender.
Of note, although the cost for pre-competition screenings are usually not covered by the insurance companies, they do not seem to be a crucial point for the athletes. All of the 1047 athletes who answered the questionnaire, accepted to cover moderate expenses of at least 60 Swiss Francs for the baseline screening, an amount that correlates with the current international custom [11, 14, 26].
In our first survey, 1,047 athletes participated and were excluded only if they did not perform regular “competitive sports”. To assure representativeness, we contacted athletes from different sports, which may have led to a certain “selection bias”. However, this cross-sectional study consciously aimed to represent a random sample.
An apparently low notional responder rate of only 0.23% (considering that virtually more than 45,000 athletes could have read the article that announced the current screening programme at the ASVZ) should not conceal that the “screening capacity” was limited (4 athletes per week) and that the “utilisation” of the programme almost reached a maximum (27 sessions with a potential maximum of 108 screened athletes). Furthermore, the academic surrounding in which the screening programme was established, may be interpreted as a “sampling bias”, but it remains debatable whether this decisively influenced the athletes’ response. The fact that the intention of about 80% of the screened athletes was to investigate a specific symptom represents a clear selection error. However, this situation outlines the current situation in daily practice and enforces us to improve our athletes’ education and care.
The fact that only 9% of 1,047 competitive athletes participating in the current survey had previously undergone a cardiac screening is alarming and supports efforts to implement a high-level nationwide, cost-effective screening concept which includes all competitive athletes. As not even half of the participating athletes supported a cardiac pre-competition assessment, such a screening should probably be voluntary in nature, but would at the same time require accurate and comprehensive information about the risk of SCD in sports. Our implemented exemplary screening programme proved to be feasible and successful, and it pointed out that cardiac screening of athletes does not implicate permanent disqualification in the case of suspicious findings, but rather provides a supportive assessment tailored to an individual athlete in order to allow for adequate sports activity in the future.
Questionnaire (English, PDF-Format) http://www.smw.ch/fileadmin/smw/images/SMW-13575-Appendix-1.pdf .
Questionnaire (German, PDF-Format) http://www.smw.ch/fileadmin/smw/images/SMW-13575-Appendix-2.pdf .
1 Corrado D, Basso C, Thiene G. Assay Sudden death in young athletes. Lancet. 2005;47–8.
2 Maron BJ. Sudden death in young athletes. N Engl J Med., 2003;349:1064–75.
3 Siscovick DS, Weiss NS, Fletcher RH, Lasky T. The incidence of primary cardiac arrest during vigorous exercise. N Engl J Med. 1984;311:874–7.
4 Thompson PD, Funk EJ, Carleton RA, Sturner WQ. Incidence of death during jogging in Rhode Island from 1975 through 1980. JAMA. 1982;247:2535–8.
5 Corrado D, Schmied C, Basso C, Borjesson M, Schiavon M, Pelliccia A, et al. Risk of sports: do we need a pre-participation screening for competitive and leisure athletes? Eur Heart J. 2011;32(8):934–44.
6 Corrado D, Pelliccia A, Bjornstad HH, Vanhees L, Biffi A, Borjesson M, et al. Cardiovascular pre-participation screening of young competitive athletes for prevention of sudden death: proposal for a common European protocol. Consensus Statement of the Study Group of Sport Cardiology of the Working Group of Cardiac Rehabilitation and Exercise Physiology and the Working Group of Myocardial and Pericardial Diseases of the European Society of Cardiology. Eur Heart J. 2005;26:516–24.
7 Dvorak J, Grimm K, Schmied C, Junge A. Development and implementation of a standardized precompetition medical assessment of international elite football players. Clin J Sport Med. 2009;19(4):316–21.
8 Maron BJ, Thompson PD, Ackerman MJ, Balady G, Berger S, Cohen D, et al. Recommendations and considerations related to preparticipation screening for cardiovascular abnormalities in competitive athletes: 2007 update: a scientific statement from the American Heart Association Council on Nutrition, PhysicalActivity, and Metabolism: endorsed by the American College of Cardiology Foundation. Circulation. 2007;115:1643–455.
9 Schmied C, Zerguini Y, Junge A, Tscholl P, Pelliccia A, Mayosi BM, Dvorak J; Cardiac findings in the precompetition medical assessment of football players participating in the 2009 African Under-17 Championships in Algeria, Br J Sports Med. 2009;43:716–21.
10 Bille K, Fiquiras D, Schamasch P. Sudden cardiac death in athletes: the Lausanne recommendations. Eur J Cardiovasc Prev Rehabil. 2006;13:859–75.
11 Corrado D, Basso C, Pavei A, Michieli P, Schiavon M, Thiene G. Trends in sudden cardiovascular death in young competitive athletes after implementation of a preparticipation screening program. JAMA. 2006;296:1593–601.
12 Corrado D, Basso C, Schiavon M, Thiene G. Screening for hypertrophic cardiomyopathy in young athletes. N Engl J Med. 1998;339:364–9.
13 Maron BJ, Haas TS, Doerer JJ, Thompson PD, James HS. Comparison of U.S. and Italian experiences with sudden cardiac deaths in young competitive athletes and implications for preparticipation screening strategies. Am J Cardiol. 2009;104:276–80.
14 Pelliccia A, Di Paolo FM, Corrado D, Buccolieri C, Quattrini FM, Pisicchio C, et al. Evidence for efficacy of the Italian national pre-participation screening programme for identification of hypertrophic cardiomyopathy in competitive athletes. Eur Heart J. 2006;27:2196–200.
15 Villiger B, Hintermann M, Goerre S, Kriemler S, Schmied C. Task Force “Prevention of Sudden Death in Elite Sport” SGSM/SSMS 2010; The sudden cardiac death of a young athlete: Recommendations for a sensible and effective preventive exam. Schweizerische Zeitschrift für «Sportmedizin und Sporttraumatologie» (2)/2011;59:108–9.
16 Magazin des Akademischen Sportverbandes Zürich, “O2”, 29/2010: 4–5.
17 Corrado D, Pelliccia A, Heidbuchel H, Sharma S, Link M, Basso C, et al. On behalf of the Sections of Sports Cardiology of the European Association of Cardiovascular Prevention and Rehabilitation; and the Working Group of Myocardial and Pericardial Disease of the European Society of Cardiology. Recommendations for interpretation of 12-lead electrocardiogram in the athlete. Eur Heart J. 2010;31(2):243–59.
18 Etchells E, Bell C, Robb, K. Does this patient have an abnormal systolic murmur? JAMA. 1997;277(7):564.
19 Loeys BL, Dietz HC, Braverman AC, Callewaert BL, De Backer J, Devereux RB, et al. The revised Ghent nosology for the Marfan syndrome. J Med Genet. 2010;47(7):476–85.
20 Hoffmann A, Isler R. Kardiale Beurteilung der Sporttauglichkeit. Schweiz Med Forum. 2007;7(44):889–89.
21 Maron BJ, Chaitman BR, Ackerman MJ, et al. Recommendations for physical activity and recreational sports participation for young patients with genetic cardiovascular diseases. Circulation. 2004;109(22):2807–16.
22 http://www.freep.com/article/20091018/SPORTS23/91018016/3-runners-die-Detroit-marathon
23 Keller, DI, Kardiale Screening-Untersuchungen beim Kompetitiv- und Gelegenheits-Athleten. Schweizerische Zeitschrift für Sportmedizin und Sporttraumatologie. 2011;59:79–82.
24 Corrado D, Basso C, Schiavon M, Pelliccia A, Thiene G. Pre-participation screening of young competitive athletes for prevention of sudden cardiac death. J Am Coll Cardiol. 2008;52:1981–9.
25 Maron BJ, Doerer JJ, Haas TS, Tierney DM, Mueller FO. Sudden deaths in young competitive athletes: analysis of 1866 deaths in the United States, 1980–2006. Circulation. 2009;119:1085–92.
26 Borjesson M, Urhausen A, Kouidi E, Dugmore D, Sharma S, Halle M, et al. Cardiovascular evaluation of middle-aged/senior individuals engaged in leisure-time sport activities: position stand from the sections of exercise physiology and sports cardiology of the European Association of Cardiovascular Prevention and Rehabilitation. Eur J Cardiovasc Prev Rehabil. 2010 Jun 19.
27 Michaud K, Fellmann F, Abriel H, Beckmann JS, Mangin P, Elger BS. Molecular autopsy in sudden cardiac death and its implication for families: discussion of the practical, legal and ethical aspects of the multidisciplinary collaboration. Swiss Med Wkly. 2009;139(49-50):712–8.
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article were reported.