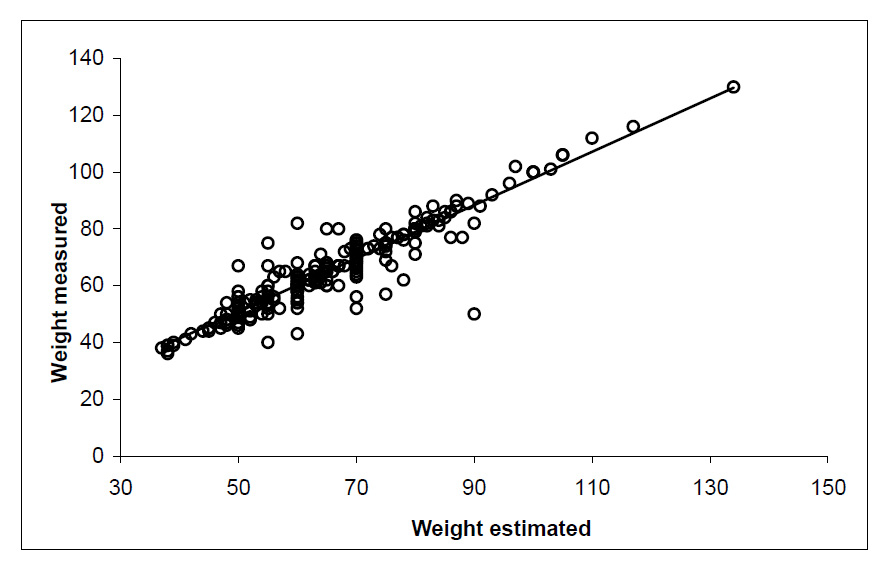
Figure 1
Scatter plot with measured and estimated body weight.
DOI: https://doi.org/10.4414/smw.2012.13585
Body weight is important medical information that is routinely assessed in the emergency department (ED) work-up. Loss of weight is suggestive of morbidity, and it is of prognostic relevance [1–3]. Furthermore, dosing drugs may depend on weight, such as in systemic lysis therapy, where the dose has to be determined [4]. Any non weight-adapted strategy would be off-label. This is only one example of why a correct determination of the patient’s weight is important in order to avoid effects such as toxicity or lack of therapeutic effectiveness. However, weighing patients is often impossible in acute disease, for example in stroke patients who are strictly confined to bed, or in geriatric patients presenting with weakness who are often unable to stand upright. In such cases, an approximation by health-care providers or estimation by the patient is used as proxy for the real body weight for clinical purposes.
Previous studies on middle-aged patients in the ED showed that the patient’s own weight estimation is superior to the weight estimation by ED staff [5, 6]. Findings of epidemiological studies suggest that community dwelling elderly are also able to estimate their body weight quite accurately [7, 8]. However, to our knowledge, there is no data showing the accuracy of self-reported weight in geriatric patients with potential acute morbidity presenting to the ED. Elderly patients presenting to the ED are at risk of adverse outcomes. Therefore, especially in the light of overcrowding in Swiss EDs [9], risk stratification tools are urgently needed [10]. A significant portion of elderly patients present to the ED with non-specific complaints, and are at risk of significant morbidity [11]. Actually, over half of them suffer from an acute medical problem requiring rapid and appropriate treatment [11, 12]. The objective of this study was to determine the precision of patient weight self-estimation, particularly in an elderly high risk population presenting to the ED with non-specific complaints.
From 15 June 2007 until 5 July 2008, 370 consecutive elderly patients (median age 75 years) presenting to the ED with non-specific complaints were included into the Basel Non-specific Complaints Study (BANC) study [11] . The present analysis was part of the sub-study on weight and nutritional status. We assessed the patients’ own estimation of weight by a bedside interview. In order to compare the estimated weight to the measured weight, the patients’ medical records were used. Verified weight was drawn from charts, clinical examination protocols, anaesthesia protocols, ECG protocols and other reports. In our hospital-wards, weight is usually drawn following the actual nursing guidelines, specifically, in the morning with the patient only wearing a nightshirt, and no shoes or other clothes. We used correlation analyses to assess the agreement of estimated weight with measured weight. We used the Bland-Altman plot to show the distribution of the differences between measured and estimated weight against the average of the two measures. Finally we tested if age, sex and critical illness (serious outcome within 30 days [11]) modified the correlation of estimated weight with measured weight.
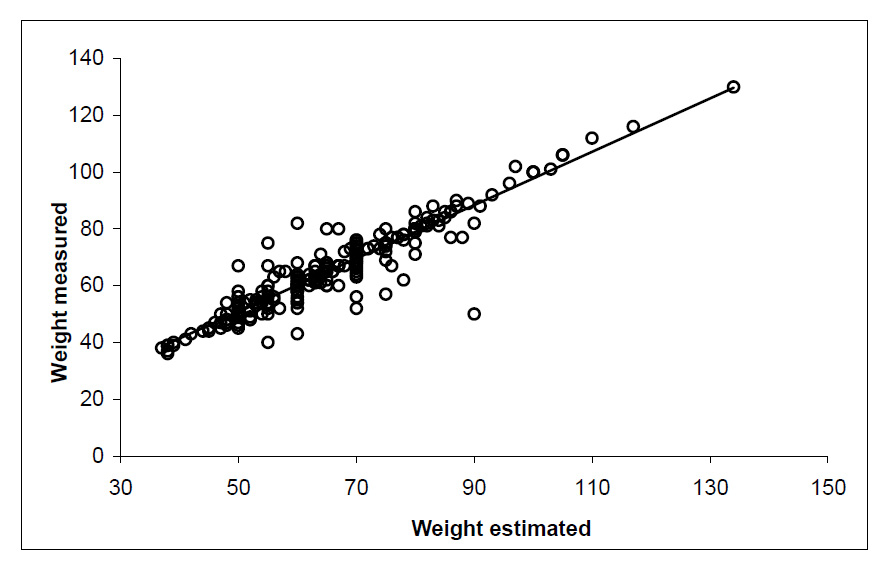
Figure 1
Scatter plot with measured and estimated body weight.
A total of 370 consecutive elderly patients were included into the BANC study. In 105 patients, a verified weight was not documented, often due to rapid discharge and disposition to geriatric community hospitals, or was not recordable for other reasons (e.g., psychiatric disease or extremely serious condition). Another 32 patients were excluded because of missing data. Mortality was similar in both included and excluded patients (5.2%, 5.8%). The rate of serious outcome within 30 days [11] was higher in included patients (65%) compared to the excluded patient group (54%), therefore a selection bias in favour of the healthier patients is unlikely. The final study population available for analysis consisted of 233 patients. Median age was 79 years (interquartile range (IQR) 71 to 86), 43% of the patients were men, and the median of both estimated and measured weight was 64 kilograms (IQR 55 to 75 kg, and 54 to 75 kg for measured and estimated weight, respectively).
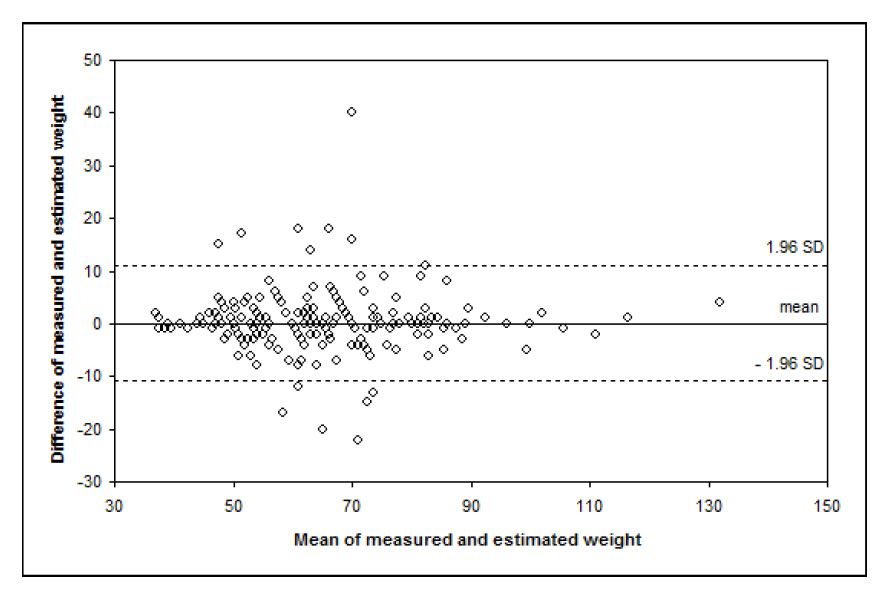
Figure 2
Bland-Altman plot of measured and estimated body weight.
Measured and estimated weights were highly correlated, indicating a good agreement of the two measures (Pearson’s correlation coefficient r = 0.94, 95% confidence interval (CI) [0.926, 0.949]).
As shown in Figure 1, the estimated and measured weights were linearly correlated and showed relatively little variation across the measured weight range. The linear association and homogenous variation showed that the self-estimated weight was an appropriate surrogate for the measured weight over the entire weight range including the margins. The correlation did not differ significantly between patients with and without serious outcomes within 30 days (p = 0.34) or between women or men (p = 0.83). Participating men slightly underestimated (mean difference –0.5 kg), and women slightly overestimated (mean difference +0.5 kg) their body weight. There was no influence of age on the accuracy of weight estimation (p = 0.32), nor was there evidence that the correlation between measured and estimated weight was affected by age (p = 0.25 for interaction).
The Bland-Altman plot (fig. 2) shows the distribution of the differences between measured and estimated weight against the average of the two measures. The horizontal lines represent the mean difference (+0.1 kg) and 1.96 times standard deviation. The estimation error (estimated minus measured weight) of 95% of all patients ranged between –10.9 and +11.1 kg. There was no evidence that patients with low or patients with high body weight under- or overestimated their weight. Figure 2 also shows that underweight (<45 kg) and overweight (>90 kg) patients tended to estimate their weight more accurately than patients in the average weight range.
| Table 1: Baselline characteristics (n = 233). | ||
| Sex: male | % (n) | 43% (100) |
| Age* | Years | 71 79 86 |
| Weight estimated* | Kg | 55 64 75 |
| Weight verified* | Kg | 54 64 75 |
| * Percentiles: P25 P50 P75 | ||
We found a negligible small mean difference (0.15 kg) between self-reported and measured weights in high risk elderly ED patients. The correlation coefficient in our study population was in the range as previously reported in middle-aged ED patients [5]. The effect of age on weight estimation was previously studied in non-ED settings where, in women 60–79 years of age, the estimated and measured weights correlated comparably well [8]. Despite the excellent correlation of estimated and measured body weight in our study population, we found relevant differences on the individual patient level (fig. 2). In our study, the 95% limits of agreement (–10.9/+11.1 kg) were higher compared to the cited study in women [8], but comparable to findings in ED patients with a median age of 45 years [6]. Interestingly, neither the rather high median age of 79 years, nor the presence of acute disease and a high co-morbidity rate (e.g. co-morbid dementia was present in 27% of our patients) impaired the accuracy of the reported weight in the vast majority of our patients, as only 6% misjudged their weight by more than 10 kilograms.
Thus, the present data support findings of non-ED settings where it was shown that, even in old age, weight self-estimation may still be accurate [7]. Nevertheless, in previous studies men tended to overestimate and women tended to underestimate their weight [7, 13]. In our population, we found only small differences between weight estimation in men and women. In contrast to previous studies showing that patients with high BMI more often underestimated their weight [14], we found no evidence of a bias towards underestimation of weight in the obese population.
In summary, our findings suggest that self-reported weight can be used as a proxy for measured weight even in sick elderly ED patients.
1 Bauer JM, Wirth R, Volkert D, Werner H, Sieber CC. Malnutrition, sarcopenia and cachexia in the elderly: from pathophysiology to treatment. Conclusions of an international meeting of experts, sponsored by the BANSS Foundation. Dtsch Med Wochenschr. 2008;133(7):305–10.
2 Newman AB, Yanez D, Harris T, Duxbury A, Enright PL, Fried LP. Weight change in old age and its association with mortality. J Am Geriatr Soc. 2001;49(10):1309–18.
3 Sullivan DH, Liu L, Roberson PK, Bopp MM, Rees JC. Body weight change and mortality in a cohort of elderly patients recently discharged from the hospital. J Am Geriatr Soc. 2004;52(10):1696–701.
4 Brott TG, Haley EC Jr, Levy DE, Barsan W, Broderick J, Sheppard GL, Spilker J, Kongable GL, Massey S, Reed R, et al. Urgent therapy for stroke. Part I. Pilot study of tissue plasminogen activator administered within 90 minutes. Stroke. 1992;23(5):632–40.
5 Anglemyer BL, Hernandez C, Brice JH, Zou B. The accuracy of visual estimation of body weight in the ED. Am J Emerg Med. 2004;22(7):526–9.
6 Menon S, Kelly AM. How accurate is weight estimation in the emergency department? Emerg Med Australas. 2005;17(2):113–6.
7 Kuczmarski MF, Kuczmarski RJ, Najjar M. Effects of age on validity of self-reported height, weight, and body mass index: findings from the Third National Health and Nutrition Examination Survey, 1988–1994. J Am Diet Assoc. 2001;101(1):28–34; quiz 5–6.
8 Lawlor DA, Bedford C, Taylor M, Ebrahim S. Agreement between measured and self-reported weight in older women. Results from the British Women's Heart and Health Study. Age Ageing. 2002;31(3):169–74.
9 Clément N, Businger A, Martinolli L, Zimmermann H, Exadaktylos AK. Referral practice among Swiss and non-Swiss walk-in patients in an urban surgical emergency department. Swiss Med Wkly. 2010;140:w13089.
10 Graf CE, Giannelli SV, Herrmann FR, Sarasin FP, Michel JP, Zekry, et al. Identification of older patients at risk of unplanned readmission after discharge from the emergency department – Comparison of two screening tools. Swiss Med Wkly. 2012;141:w13327.
11 Nemec M, Koller M, Nickel C, Maile S, Winterhalder C, Karrer C, et al. Patients presenting to the emergency department with non-specific complaints: the Basel Non-specific Complaints (BANC) study. Acad Emerg Med. 2010;17(3):284–92.
12 Rutschmann OT, Chevalley T, Zumwald C, Luthy C, Vermeulen B, Sarasin FP. Pitfalls in the emergency department triage of frail elderly patients without specific complaints. Swiss Med Wkly. 2005;135(9–10):145–50.
13 Dahl AK, Hassing LB, Fransson EI, Pedersen NL. Agreement between self-reported and measured height, weight and body mass index in old age-a longitudinal study with 20 years of follow-up. Age Ageing. 2010;39(4):445–51.
14 Nawaz H, Chan W, Abdulrahman M, Larson D, Katz DL. Self-reported weight and height: implications for obesity research. Am J Prev Med. 2001;20(4):294–8.
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article were reported.