Diuretic use, RAAS blockade and morbidity in elderly patients presenting to the Emergency Department with non-specific complaints
DOI: https://doi.org/10.4414/smw.2012.13568
Juliane M.
Ruedinger, Christian H.
Nickel, Michael
Bodmer, Silke
Maile, Reto W.
Kressig, Roland
Bingisser
Summary
QUESTIONS UNDER STUDY: Up to 20% of elderly patients present to the emergency department (ED) with non-specific complaints (NSC), such as “generalised weakness”, the majority suffering from serious conditions requiring timely intervention. Little is known about the use and influence of diuretics and renin-angiotensin-aldosterone (RAAS) blockade on morbidity in those patients. The hypothesis was tested that the use of diuretics and RAAS blockade could be associated with an increased incidence of serious conditions in those patients.
METHODS: During a 23-month period, all adult non-trauma patients with an Emergency Severity Index (ESI) of 2 or 3 were prospectively enrolled. Serious conditions were defined as potentially life-threatening conditions or conditions requiring early intervention to prevent further morbidity and mortality.
RESULTS: Study population consisted of 633 patients with median age 82 years, median Charlson comorbidity index 2. 59% of all subjects suffered from a serious condition. 299 subjects (47.2%) used diuretics, of which 65.6% suffered from a serious condition. Combination therapy of RAAS blockade and diuretics was found in 158 subjects (24.9%), 70.3% of which suffered from a serious condition. The intake of two or more diuretics, loop diuretics and a combination therapy with diuretics and RAAS blockade were associated with an increased risk for serious condition (p = 0.036; p = 0.021; p = 0.004).
CONCLUSIONS: Treatment with two or more diuretics, loop diuretics, or a combination therapy with RAAS blockade and diuretics are independently associated with serious condition and therefore should be recognized as “red flags” in elderly patients presenting to the ED with NSC.
Background
Diuretics, especially loop and thiazide diuretics as well as blockade of the renin-angiotensin-aldosterone-system (RAAS), are widely used in patients of all ages for hypertension or congestive heart failure. Still, blood pressure control in western countries needs improvement. According to the SWISSHYPE study, Switzerland’s overall blood pressure control is with 49% one of the best in comparison to other western European countries [1]. Until summer 2011 the optimum treatment strategies for hypertension in the elderly population were under discussion. The recently published AHA/ACC/ESH expert consensus recommended a thiazide-type diuretic, a calcium antagonist, RAAS blockade, or a combination of those as first line-therapy in uncomplicated elevated blood pressure of the elderly [2]. In terms of congestive heart failure, the Heart Failure Society of America recommended in 2010 a “diuretic treatment for patients with HF and clinical evidence of volume overload, including those with preserved LVEF”. However, there is strength of evidence class C only [3]. Whereas the mentioned guidelines consider RAAS blockade to be a relatively safe therapy, the use of diuretics is a known and feared risk factor related to an imbalance in electrolyte- and hydration status. Those disturbances of the elderlies’ electrolyte- and hydration homeostasis may potentially lead to severe complications, such as renal impairment and increased mortality [4–6] and, among many others, may often cause symptoms such as “feeling dizzy or weak”. Additionally, it is empirically known that elderly patients have a diminished sense of thirst and are prone to dehydration during the hot season. Recently, a significant increase in serious heat-related adverse drug events during the hot spell 2003 was found with frequently involved drugs being, among others, diuretics and ACE inhibitors [7].
Up to 20% of all patients presenting to the emergency department (ED) suffer from non-specific complaints (NSC) [8] with notable and alarming courses of disease and underlying conditions. A recent study about patients presenting to the ED with non-specific abdominal pain demonstrated, that after a twelve month follow-up period one fourth still suffered from the same pain [9]. The recently published “Basel non-specific complaints study” (BANC) describes one of the first cohorts of this well-known but poorly studied patient group, presenting to the ED with complaints such as “feeling weak”, “being tired”, “general deterioration”, and recent falls. It was shown that 59% of all patients with NSC suffered from a serious condition (SC). SC was defined as any potentially life-threatening condition, or any condition that requires an early intervention to prevent health status deterioration leading to further morbidity, disability, or death [10].
Finding the appropriate diagnostic and treatment approach for each patient with NSC (ranging from “wait and see” to an extensive diagnostic workup), in order to prevent poor patient outcomes [11], often exceeds the resources of an ED [12]. Therefore, the ultimate goal of the BANC Study is to identify risk factors for serious condition that may be identified early, such as during history taking.
We therefore tested the hypothesis, whether the use of diuretics or their combination with RAAS blockade may be associated with serious conditions in patients presenting to the ED with NSC.
Methods
Study design
This present study is a predefined part of the BANC study, a delayed type cross-sectional diagnostic study with a prospective 30 day follow-up. The study protocol was approved by the local ethics committee (EKBB 73/07) and is registered with Clinical Trials NCT00920491.
Study setting and population
The study was carried out in the ED of the University Hospital Basel, Switzerland. The hospital is an urban 700-bed tertiary care center with an ED census of over 41’000 patients per year. From 24 May 2007 until 15 April 2009, all non-trauma patients presenting to the ED with an Emergency Severity Index (ESI) [13] 2 or 3 were consecutively screened for inclusion. The ESI was used as a validated triage tool in order to exclude all patients with unstable conditions (ESI 1), as well as patients with conditions in which a full work-up was not intended (“see-and-treat” pathway, ESI 4 or 5).
Study protocol /inclusion criteria
The BANC study is a delayed type cross-sectional diagnostic study.
Patients were included if they presented with non-specific complaints as described by Safwenberg [11], such as “generalised weakness”, “being tired”, or being unable to cope with their usual daily activities. Patients with specific complaints (e.g., syncope, chest pain), or clinical features suggestive of a working diagnosis (e.g., unilateral limb weakness) were not included. We enrolled neither hemodynamically unstable patients, nor patients with persistent signs of shock or vital parameters significantly out of the normal range (blood pressure <80 or >180 mm Hg, respiration rate >20/min, tympanal body temperature >38.5 °C, SaO2 <92%). Delirium was an exclusion criterion, since management is often based on a predefined treatment protocol and obtaining informed consent is impossible. Furthermore, patients with known terminal conditions (e.g., end stage cancer) as well as patients referred from another hospital were not eligible for inclusion.
Measurements
Demographic baseline data, ESI, all patient’s complaints (using a structured interview form), vital signs (pulse, blood pressure, respiratory rate, and oxygen saturation), medical history, physical examination, and ECG were obtained on admission and registered on the patient’s case report form. Several additional parameters including a complete list of comorbidities and prescribed drugs were gathered from physician reports and patient charts.
In all patients, a blood sample was drawn and, in the vast majority, chest X-ray and urinalysis were performed. Treatment was initiated at the discretion of the ED physician in charge.
Assessment of medication
We assessed all drugs reported by the patient, by proxies, by the family physician, or documented in our electronic patient records. Drugs were grouped into predefined pharmacological classes (e.g., beta-blockers, ACE-inhibitors/angiotensin II-receptor blockers subsumed as RAAS blockade, benzodiazepines and diuretics). Diuretics were subclassified into thiazide diuretics, loop diuretics, and other (aldosterone antagonists and potassium-sparing agents).
Assessment of comorbidity
All comorbidities were assessed by patient interviews, by proxies, and by electronic patient records dating back 10 years at our institution. For quantification of comorbidity, the Charlson Comorbidity Index was used [14]. This tool has been validated for population-based studies to estimate the risk of short-term and long-term mortality in non-surgical emergency department patients [15].
Patient follow up and endpoint ascertainment
We obtained 30-day follow-up data by hospital discharge reports and by family physicians, if discharged earlier. Two ED physicians (“outcome assessors”), certified in internal medicine and blinded to the patients’ baseline data, reviewed all discharge records and established the presence of a serious condition, as well as a final gold standard diagnosis according to the 10th International Classification of Diseases and Related Health Problems (ICD-10). The BANC “expert panel” reviewed all inclusion forms for exclusion criteria, and in case of disagreement of the outcome assessors; reviewed all arguments gathered by the outcome assessors in order to make a final decision on “gold standard diagnosis” and serious condition.
According to the predefined framework (Nemec et al. [10]), a serious condition was defined as a potentially life-threatening condition, or any condition requiring an early intervention (e.g., transfusion due to severe anemia) to prevent health status deterioration leading to further morbidity, or death within 30 days of the initial ED presentation.
Data analysis
Parts of the statistics were performed by a certified bio-statistician (Schötzau & Simmen, Basel, Switzerland). In case of categorical variables, crosstables were calculated. In case of ordinal or metric variables, mean, median, standard deviation, minimum, maximum were calculated. To predict the influence of diuretics on the outcome serious condition, a logistic regression model was chosen. Adjustment for age, gender and comorbidities was performed by adding these cofactors to the regression model. Results are presented as two-sided p-values and odds ratios (ORs) with their corresponding 95% confidence intervals. In the case of continuous or ordinal variables, odds ratios are expressed as increasing the variable from the first to the third quartile. Chi square test was performed to detect an association between the concomitant use of RAAS blockade and diuretics and serious condition. Chi square test was performed to detect a possible association between extreme outside temperatures (summer and winter, mean values) and the prevalence of serious conditions in subjects with diuretic treatment. A linear regression analysis of the monthly percentage of serious condition in subjects on diuretics and monthly mean outside temperature was performed to detect a possible association between outside temperature and a changing prevalence of serious condition.
A p-value <0.05 was considered significant. This study is exploratory; therefore p-values were not adjusted for multiple comparisons. The analyses were done using R v 2.8.0 (A Language and Environment for Statistical Computing) and GraphPad Prism 5.
Results
From 24 May 2007 until 15 April 2009 22,782 non-trauma patients presented to the ED. 9,926 patients were classified with either an ESI 2 or ESI 3 and therefore screened for inclusion. Of these, 714 patients (7.2%) presented with NSC and were consecutively enrolled in our study. During post-hoc case reviews, the BANC expert panel recalled the inclusion of 81 patients due to the presence of exclusion criteria. The final study population consisted of 633 patients with NSC. Baseline characteristics of the study population are presented in table 1. Median age was 81 years (IQR 72/87), 62.6% of all subjects were female, median BMI was 23.4 kg/m2. The median number of concomitant drugs was 5 (IQR 3/8).
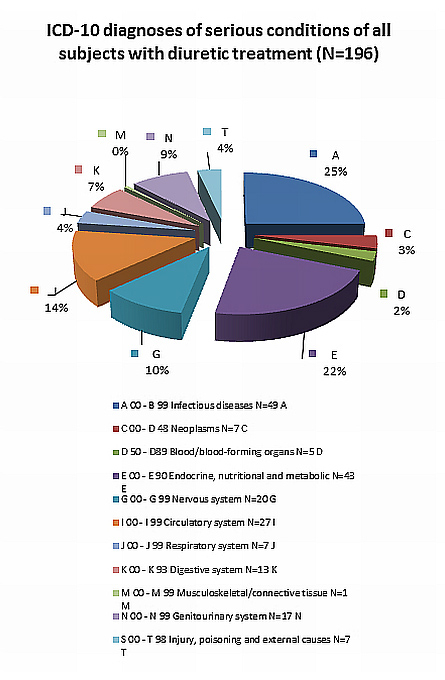
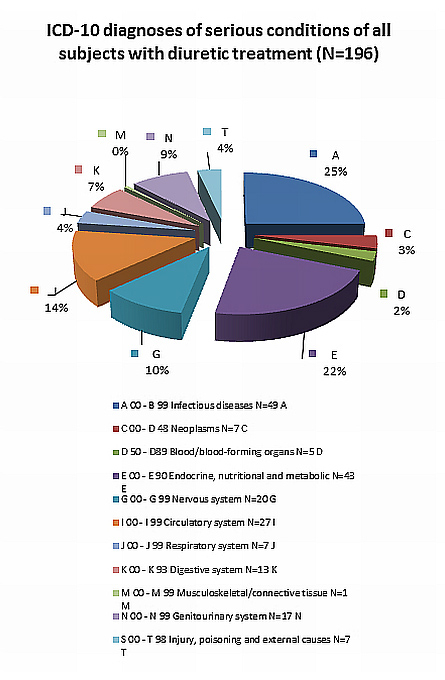
Figure 1a
Serious conditions in subjects with concomitant diuretic medication (N = 196) were classified according to the ICD-10 system by A = infectious disease to T = injury, poisoning and external causes. Beside each data bar there is the first capital letter of the respective group with the respective prevalence in the study population.
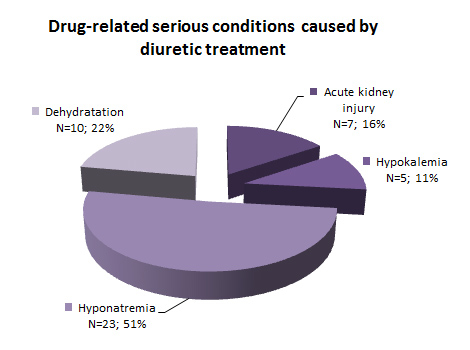
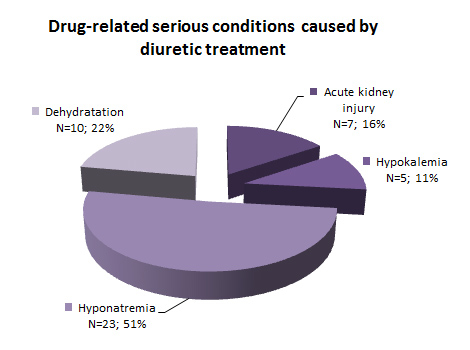
Figure 1b
The serious conditions which could directly be contributed to diuretic medication without RAAS blockade (drug-related problems DRP; N = 45) are listed with their absolute numbers and their relative frequency.
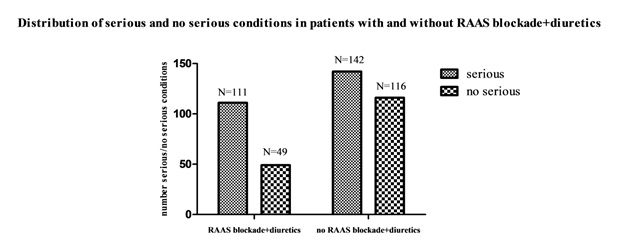
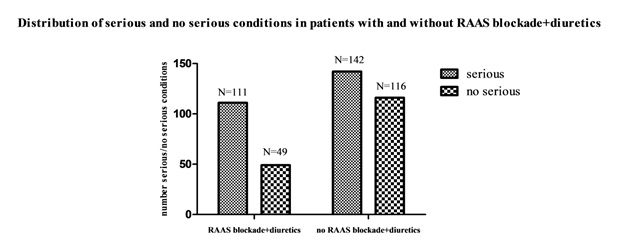
Figure 2
Juxtaposition of absolute frequencies of serious and no serious conditions in subjects with and without concomitant RAAS blockade and diuretic medication.
At presentation, 299 (47.2%) of the enrolled patients used diuretics, 180 subjects used one and 119 subjects used two or more diuretic substances. Loop diuretics ranging from 10mg to 400mg furosemide equivalent were used by 171 (27%) subjects. Thiazide diuretics were used by 137 (21.6%) subjects. 115 (18.2%) subjects used other diuretics. A combination therapy of RAAS blockade and diuretics was used by 158 subjects (24.9%).
Diuretics, RAAS blockade and associated serious conditions
In the entire BANC study population, an underlying serious condition was detected in 387 subjects (61.1%). Of all patients with diuretic medication, 196 subjects (65.6%) suffered from a serious condition.
Table 2 summarises the association between serious conditions and diuretic treatment. The use of two or more diuretics was associated with an increased risk for an underlying serious condition (adj. OR 1.65; 95% adj. CI 1.03 to 2.63, p = 0.036). In 120 patients (70.6%) using loop diuretics an underlying serious condition was detected. The use of loop diuretics was independently associated with an increased risk for an underlying serious condition (adj. OR 1.58, adj. CI 1.07 to 2.34, p = 0.021).
Among all patients using thiazide diuretics, 21.2% (29 subjects) suffered from a serious condition. There was no significant association between the use of thiazide diuretics and serious condition. The use of other diuretics was not significantly associated with an increased risk for a serious condition (adj. OR 1.52, p = 0.07).
Figure 1a shows the distribution of the serious conditions encoded as ICD-10 diagnoses of all patients treated with diuretics. The majority of which (150 of 196 subjects) was not directly caused by diuretics. The largest subgroup was infectious disease (N = 49, 24%), followed by endocrine, metabolic and nutritional disorders (N = 43, 21%), and acute cardiovascular disease (N = 27, 13%).
Serious conditions directly attributed to diuretic treatment without RAAS blockade are illustrated in figure 1b. There were 46 patients with serious conditions caused by drug-related problems, such as dehydration, electrolyte disorders (hyponatremia and hypokalemia), and acute kidney injury.
Of 158 subjects using a combination therapy of RAAS blockade and diuretics, 111 (70.3%) suffered from a serious condition, see figure 2. There was a significant association between a combination therapy of RAAS blockade and diuretics with an increased risk for a serious condition compared to subjects who used neither RAAS blockade nor diuretics (OR 1.85, 95% CI: 1.22 to 2.81, p = 0.004).
Comparing the ICD 10- encoded serious conditions in subjects with only diuretic treatment, having a combination therapy of RAAS blockade and diuretics, and taking RAAS blockade alone, there is a similar distribution of ICD 10 diagnoses in all three groups (results not shown).
In patients using diuretics, there was no significant association between months with extreme outside temperatures (during study period with a mean low temperature 2.6°C versus a mean high temperature 18.6°C) and the prevalence of serious condition (OR 0.69, 95% CI 0.4427 to 1.085, p = 0.1, see table 3). A linear regression analysis of the monthly occurring percentage of serious conditions in patients with and without diuretics (with combination therapy of diuretics and RAAS blockade) and monthly mean outside temperatures showed with p = 0.4 (p = 0.6) neither a significant difference between both lines nor a significant difference between the slopes of both lines p = 0.7 (p = 0.6).
30 day-mortality in the whole study population, was 6.8% (43 subjects). There was no significant association between the use of diuretics in general, loop diuretics, or thiazide diuretics, and 30 day-mortality (results not shown).
|
Table 1: Patient demographics. |
| |
Total population (N = 633)
|
| Age, median (IQR) |
81 (72 / 87) |
| Female, N (%) |
396 (62.6) |
| BMI, median (IQR) |
23.4 (20.4 / 26.4) |
| Living situation: – independent, N (%) |
145 (22.9) |
| – With family help, N (%) |
208 (32.9) |
| – With home care, N (%) |
214 (33.8) |
| – Nursing home, N (%) |
66 (10.4) |
| Charlson Comorbidity Index, median (IQR) |
2 (1 / 4) |
| Number of concomitant drugs, median (IQR) |
5 (3 / 8) |
| Subjects using diuretics, N (%) |
299 (47.2) |
| – 2 diuretics, N |
113 |
| – 3 diuretics, N |
6 |
| – Loop diuretics, N (%) |
171 (27) |
| – Thiazide diuretics, N (%) |
137 (21.6) |
| – Other diuretics, N (%) |
115 (18.2) |
| Subjects using RAAS blockade and diuretics, N (%) |
158 (24.9) |
| Subjects using RAAS blockade, N (%) |
74 (11.7) |
| IQR: interquartile range; N: number; BMI: body mass index. |
|
Table 2: Diuretics associated with serious condition. |
| (N serious conditions) |
Unadjusted OR for serious condition |
95% C.I. |
Adjusted OR for
serious condition †, |
95% C.I. |
P (Wald) |
| All diuretics (196) |
1.47 |
1.01–2.14 |
1.35 |
0.91–2 |
0.14 |
| 2 or more diuretics (82) |
1.79 |
1.14–2.82 |
1.65 |
1.03–2.63 |
0.03 |
| Loop diuretics (120) |
1.75 |
1.2–2.56 |
1.58 |
1.07–2.34 |
0.023 |
| Thiazide diuretics (29) |
1.04 |
0.70–1.53 |
1.03 |
0.69–1.56 |
0.965 |
| Other diuretics (43) |
1.66 |
1.07–2.58 |
1.52 |
0.97, 2.38 |
0.4 |
| N: number; OR: Odd’s Ratio; CI: confidence interval
† adjusted for age, gender, Charlson comorbidity index |
|
Table 3: Incidence of serious and no serious conditions in patients with diuretic treatment during months with extreme temperatures in Basel, Switzerland [29]. |
|
Year/winter month
|
Average
temperature
(°C)
|
Serious condition (N)
|
No serious condition (N)
|
Year/ summer month
|
Average temperature
(°C)
|
Serious condition (N)
|
No serious condition (N)
|
| 2007
November
December |
4.3
2.1 |
19
15 |
14
5 |
2007
June
July
August |
18.4
18.7
18.1 |
33
20
21 |
13
25
18 |
| 2008
January
February
December |
4.3
4.8
1.7 |
7
4
7 |
1
5
2 |
2008
June
July
August |
18.3
19.6
18.6 |
16
32
30 |
14
21
20 |
| 2009
January
February |
–0.8
2.0 |
16
13 |
9
5 |
2009
Summer |
Study closed |
| Sum |
|
81 |
41 |
|
152 |
111 |
| Pearson correlation coefficient = 2.579 (p = 0.1) |
Discussion
Of all patients presenting to the emergency department (ED) with non-specific complaints (NSC), almost every second one used diuretics and one fourth even a combination therapy with diuretics and RAAS blockade. The use of two or more diuretics as well as loop diuretics and a combination therapy with diuretics and RAAS blockade were associated with an underlying serious condition. The most frequent serious conditions were infections, endocrine and metabolic disease, and acute cardio-vascular problems.
Diuretic use has been shown to be independently associated with a less favourable functional outcome after lacunar stroke, possibly due to a decrease in blood viscosity [16]. A recent descriptive study of symptomatic hyponatremia in elderly patients concluded that diuretics should be used with caution in the elderly [17]. Furthermore, diuretics were significantly associated with all-cause mortality in elderly patients with heart failure discharged from the hospital [18]. Our own results suggest that a diuretic combination therapy (i.e., 2 or more substances) in patients presenting with non-specific complaints could constitute a “red flag” to emergency physicians as the “pre-test” probability is 60% and the odds ratio for unfavourable outcome is 1.65. Combination therapy in the elderly does not seem to be rare, as almost 40% of our patients treated with diuretics were on two or more different diuretics. Yet, even if there is an association between combination therapy and serious outcome, it may not be concluded that this combination is the cause for serious outcome, as this is a cross-sectional study trying to identify risk factors. It may well be argued that the association between combination therapy and serious condition holds true even after adjustment for age, sex, and co-morbidities – nonetheless, another common factor, such as the severity of heart disease may be the underlying reason for this association.
The other association with serious outcome was the intake of loop diuretics. They are not listed by the widely used “Screening Tool of Older Persons’ Prescriptions” (STOPP). Avoiding loop diuretics is recommended only for treating ankle edema without evidence of heart failure [19, 20]. In contrast, there is data showing a dose-dependent increase in mortality beginning at a dose of 300mg/day of furosemide equivalent in acute heart failure, and an increasing incidence of mortality, length of stay, and dialysis at a dose of 160 mg [21, 22]. Only six of our patients received more than 160 mg furosemide equivalent and there was no association with 30 day-mortality in patients treated with loop diuretics in general.
With respect to the use of thiazide diuretics, there is a controversy in literature: The revisited ALLHAT-study (Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial) stated that thiazide diuretics may not be surpassed by any other antihypertensive regimens and are therefore recommended as first line pharmacotherapy in patients with hypertension. Unfortunately, the study failed to show that lowering the systolic blood pressure had the expected benefit on the primary outcome (reduction in myocardial infarction and stroke) [23]. The results of the ACCOMPLISH trial (Avoiding Cardiovascular Events through Combination Therapy in Patients Living With Systolic Hypertension) and recently available results from the ACCORD trial may even be interpreted against the use of thiazides: There was no superiority of the antihypertensive effect, but an inferiority of hydrochlorothiazide concerning cardiovascular events and mortality [24, 25]. In our study, thiazide diuretics were not associated with a less favourable outcome in patients with NSC.
The authors of the AHA/ACC/ESH expert consensus state that there is only “limited information for evidence-based guidelines to manage older hypertension patients, and the recommendations given are based on expert opinion”. When pooling the limited available data of octogenarians from studies being originally designed for a younger population, a reduction in both cardiovascular and stroke mortality can be found. Nevertheless, there seems to be an increase in all-cause mortality compared to control subjects [2] and further research has to be conducted. Despite these open questions due to the absence of randomised controlled trials the defined target systolic blood pressure for octogenarians is <=140 mm Hg. If the blood pressure goal cannot be achieved by one substance alone, a combination of RAAS blockade and diuretics is recommended with careful dose titration. Nevertheless, our own results suggest a combination therapy of diuretics and RAAS blockade to be one more “red flag” in elderly patients with NSC which could be identified by ED physicians when taking the patient’s history.
In general, the elderly population has a high burden of comorbidity, and consequently a higher chance of poly-pharmacy [26]. Our study population had a median of six different daily medications. The altered pharmacokinetics and pharmacodynamics and age-related changes in body composition and physiology may result in indeterminable drug actions, drug-drug and drug-disease interactions [27]. In order to test the hypothesis that dehydration enhanced by diuretics had a major influence on our results, we correlated the percentage of serious conditions in patients using diuretics and a combination therapy of diuretics and RAAS blockade with average monthly temperatures without finding evidence for an association.
Several limitations must be considered: As a single-centre study without external validation sample, the generalisability of our results is limited. Furthermore, age and gender could not be disguised from the outcome assessors, leaving the possibility of some degree of incorporation bias [28].
Moreover, the association of morbidity and medication is complicated by the fact that patients with a higher burden of comorbidity use more drugs [26]. A more deleterious outcome may therefore be attributed to comorbidity rather than medication. However, in order to minimise confounding factors, associations were controlled for age, sex, and comorbidity.
Finally, the dose of diuretics was only assessed at the time of inclusion. The dosing during therapy was not studied. Nonetheless, our aim was to identify risk factors for serious conditions that were present prior to presentation. Therefore, only the part of the combined outcome that consisted of mortality could have been influenced by the in-hospital therapy and mortality contributed only 10% to the serious outcomes.
Taken together, elderly patients presenting with non-specific complaints have a high risk for serious conditions. They are treated with a high number of different drugs, and diuretics are among the most frequently prescribed in this group. A combination of diuretics, as well as loop diuretics and RAAS blockade, is associated with serious conditions. Therefore, all hospitalists should be aware of these new “red flags” when taking the patient’s history as it may help to identify elderly patients at risk of significant morbidity and mortality.
Acknowledgements:The authors would like to thank the Emergency Department nurses and physicians for their help with including patients into the study and all Basel’s general practitioners who were willing to participate in the 30 day follow-up procedure.
References
1 Brenner R, Waeber B, Allemann Y. Medical treatment of hypertension in Switzerland. The 2009 Swiss Hypertension Survey (SWISSHYPE). Swiss Med Wkly. 2011;141:w13169.
2 Aronow WS, Fleg JL, Pepine CJ, Artinian NT, Bakris G, Brown AS, et al. ACCF/AHA. Expert consensus document on hypertension in the elderly: A report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents Developed in collaboration with the American Academy of Neurology, American Geriatrics Society, American Society for Preventive Cardiology, American Society of Hypertension, American Society of Nephrology, Association of Black Cardiologists, and European Society of Hypertension. J Am Soc Hypertens. 2011;5(4):259–352.
3 Heart Failure Society of America. HFSA 2010 Comprehensive Heart Failure Practice Guideline. J Card Fail. 2010;16(6):e1–e2.
4 Butt TF, Branch RL, Beesley L, Martin U. Managing hypertension in the very elderly: effect of adverse drug reactions (ADRs) on achieving targets. J Hum Hypertens. 2010;24(8):514–8.
5 Jyrkkä J, Enlund H, Korhonen MJ, Sulkava R, Hartikainen S. Polypharmacy status as an indicator of mortality in an elderly population. Drugs Aging. 2009;26(12):1039–48.
6 Prybys KM. Deadly drug interactions in emergency medicine. Emerg Med Clin North Am. 2004;22(4):845–63.
7 Michenot F, Sommet A, Bagheri H, Lapeyre-Mestre M, Montastruc JL; French Network of PharmacoVigilance Centres. Adverse drug reactions in patients older than 70 years during the heat wave occurred in France in summer 2003: a study from the French PharmacoVigilance Database. Pharmacoepidemiol Drug Saf. 2006;15(10):735–40.
8 Vanpee D, Swine C, Vandenbossche P, Gillet JB. Epidemiological profile of geriatric patients admitted to the emergency department of a university hospital localized in a rural area. Eur J Emerg Med. 2001;8(4):301–4.
9 Banz VM, Paul K, de Moya M, Zimmermann H, Candinas D, et al. Ignoring non-specific abdominal pain in emergency department patients may be related to decreased quality of life. A follow up of an underestimated problem. Swiss Med Wkly. 2011;141:w13167.
10 Nemec M, Koller MT, Nickel CH, Maile S, Winterhalder C, Karrer C, et al. Patients presenting to the emergency department with non-specific complaints: The Basel Non-specific Complaints (BANC) Study. Acad Emerg Med. 2010;17(3):284–92.
11 Safwenberg U, Terent A, Lind L. The Emergency Department presenting complaint as predictor of in-hospital fatality. Eur J Emerg Med. 2007;14(6):324–31.
12 Rutschmann OT, Chevalley T, Zumwald C, Luthy C, Vermeulen B, Sarasin FP. Pitfalls in the emergency department triage of frail elderly patients without specific complaints. Swiss Med Wkly. 2005;135(9-10):145–50.
13 Gilboy N, Tanabe P, Travers DA. The Emergency Severity Index Version 4: changes to ESI level 1 and pediatric fever criteria. J Emerg Nurs. 2005;31(4):357–62.
14 Charlson ME, Pompei P, Ales KL, MacKenzie CR.. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83.
15 Olsson T, Terent A, Lind L. Charlson Comorbidity Index can add prognostic information to Rapid Emergency Medicine Score as a predictor of long-term mortality. Eur J Emerg Med. 2005;12(5):220–4.
16 Aerden L, van Raak E, Boreas A, Kessels A, Lodder J. Common drugs in acute ischemic stroke and their influence on outcome: An observational study in 1,013 stroke patients. Clin Neuropharmacol. 2008;31(2):74–9. 10.1097/WNF.0b013e31811ec142.
17 Rao MY, Sudhir U, Anil Kumar T, Saravanan S, Mahesh E, Punith K. Hospital-based descriptive study of symptomatic hyponatremia in elderly patients. Journal of Association of Physicians of India 2010;58:667–9.
18 Hamaguchi S, Kinugawa S, Goto D, Tsuchihashi-Makaya M, Yokota T, Yamada S, et al. Predictors of long-term adverse outcomes in elderly patients over 80 years hospitalized with heart failure - A report from the Japanese Cardiac Registry of Heart Failure in Cardiology (JCARE-CARD)-. Circ J. 2011 Sep 22;75(10):2403-10. Epub 2011 Jul 21.
19 Page RL 2nd, Linnebur SA, Bryant LL, Ruscin JM. Inappropriate prescribing in the hospitalized elderly patient: Defining the problem, evaluation tools, and possible solutions. Clin Interv Aging. 2010;5:75–87.
20 Gallagher P, Ryan C, Byrne S, Kennedy J, O'Mahony D., STOPP (Screening Tool of Older Person's Prescriptions) and START (Screening Tool to Alert doctors to Right Treatment). Consensus validation. Int J Clin Pharmacol Ther. 2008;26(2):72–83.
21 Hasselblad V, Gattis Stough W, Shah MR, Lokhnygina Y, O'Connor CM, Califf RM,, et al. Relation between dose of loop diuretics and outcomes in a heart failure population: Results of the ESCAPE Trial. Eur J Heart Fail. 2007;9(10):1064–9.
22 Costanzo MR, Johannes RS, Pine M, Gupta V, Saltzberg M, Hay J, et al. The safety of intravenous diuretics alone versus diuretics plus parenteral vasoactive therapies in hospitalized patients with acutely decompensated heart failure: A propensity score and instrumental variable analysis using the Acutely Decompensated Heart Failure National Registry (ADHERE) database. Am Heart J. 2007;154(2):267–77.
23 Wright JT Jr, Probstfield JL, Cushman WC, Pressel SL, Cutler JA, Davis BR, et al. ALLHAT findings revisited in the context of subsequent analyses, other trials, and meta-analyses. Arch Intern Med. 2009;169(9):832–42.
24 Jamerson KA, Bakris GL, Wun CC, Dahlöf B, Lefkowitz M, Manfreda S, et al. Rationale and design of the avoiding cardiovascular events through combination therapy in patients living with systolic hypertension (ACCOMPLISH) trial: The first randomized controlled trial to compare the clinical outcome effects of first-line combination therapies in hypertension. Am J Hypertens. 2004;17(9):793–801.
25 ACCORD Study Group, Cushman WC, Evans GW, Byington RP, Goff DC Jr, Grimm RH Jr. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362(17):1575–85.
26 Kaufman DW, Kelly JP, Rosenberg L, Anderson TE, Mitchell AA. Recent patterns of medication use in the ambulatory adult population of the United States: the Slone survey. JAMA. 2002;287(3):337–44.
27 Beglinger C. Ethics related to drug therapy in the elderly. Dig Dis. 2008;26(1):28–31.
28 Knottnerus JA, Buntinx F, ed. The evidence base of clinical diagnosis: Theory and methods of diagnostic research. ed. B. Books. 2008.
29 MeteoSwiss, F.O.o.M.a.C. Monthly homogenized values of temperature and precipitation in Basel / Binningen, Switzerland. Coordinates: 47° 32.5' N / 7° 35.0' E. 20.06.2011.