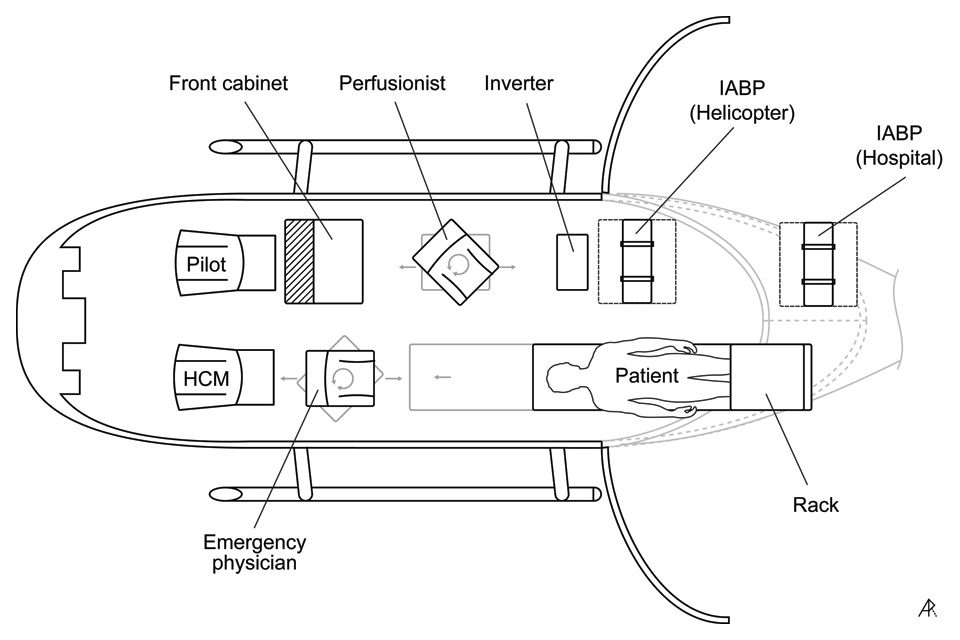
Figure 1
Positioning of patient, crew members and specific devices within the helicopter (back doors open). HCM: Helicopter Emergency Medical Services Crew Member; IABP: Intra-aortic balloon pump.
DOI: https://doi.org/10.4414/smw.2012.13552
Swiss experience and recommendations
Intra-aortic balloon pump (IABP) counter-pulsation support is a recommended option for patients with cardiac failure, mainly due to coronary artery disease or congestive heart failure [1, 2]. Early IABP support is used to accompany acute percutaneous coronary intervention (PCI) or cardiac surgery. In addition, IABP support may function as a bridge prior to invasive procedures if these specialities are not immediately available or are unavailable at the initial hospital of admission. If in such a situation inter-hospital transfer is mandatory, IABP support must be maintained. Inter-hospital transfers of patients with IABP support have been successfully carried out by ground and by air transport [3, 4]. Since July 2008, the Swiss Air-Rescue (Rega, Zurich-Airport) has been willing to provide IABP transports by helicopter or jet, 24 hours a day, 365 days a year. The IABP can be supplemented with an air transport approved extracorporeal membrane oxygenation device and/or with a left ventricular assist device (e.g., Novalung®, Impella®, Life-Box® and Cardiohelp®).
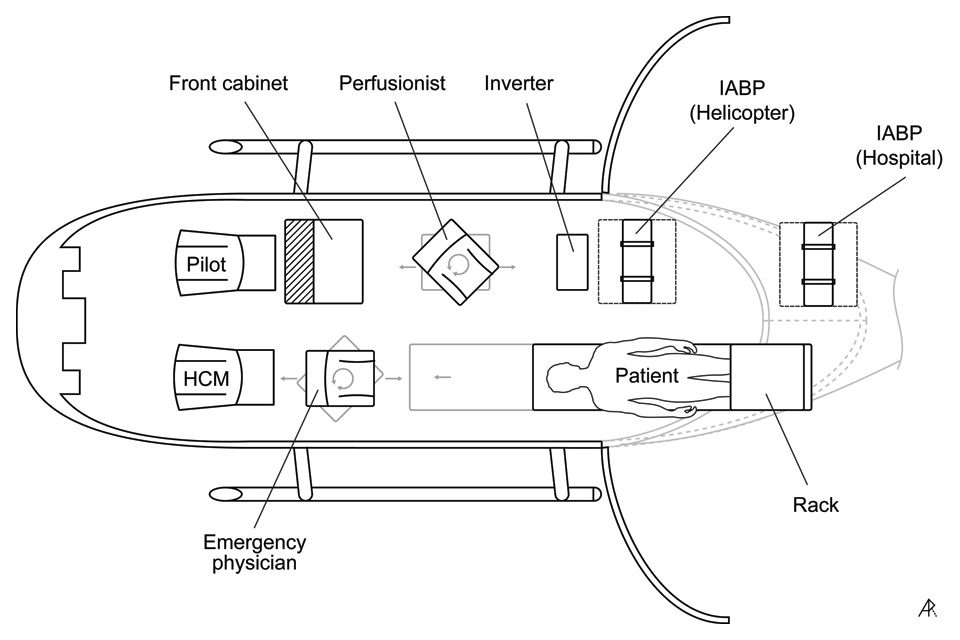
Figure 1
Positioning of patient, crew members and specific devices within the helicopter (back doors open). HCM: Helicopter Emergency Medical Services Crew Member; IABP: Intra-aortic balloon pump.
Inter-hospital transfers are high-risk operations for seriously ill patients. The aim of the present study was to review the first two years of transport of patients with IABP by Rega and based on this experience, develop and promulgate a standard operating procedure (SOP) for the hospitals involved with the intention to minimise transportation hazards and streamline the handover processes at the sending and receiving institutions, thereby increasing patient safety. In addition, we would like to provide insight into the situation experienced by emergency physicians responsible for the transfer.
All helicopter transfers of patients with IABP support by Swiss Air-Rescue (Rega, Zurich-Airport, Switzerland) between September 2008 and October 2010 were retrospectively analysed. Approval for this study was received from the responsible ethics committee (Ethikkommission beider Basel). No exclusion criteria were applied. The major endpoints included death, cardiopulmonary resuscitation, accidental loss of airway, major bleeding at the IABP puncture site or dislocation/disconnection of the device during transport. The minor endpoints were addressed as non-life-threatening cardiovascular, respiratory or neurological problems, or nausea/vomiting. In addition, data were analysed with regard to the geographical distribution of the transfers, patient demographics, aetiology of cardiac failure, haemodynamic and respiratory data. Data were extracted from the Rega patient chart and Rega database. For outcome data, a questionnaire was sent by mail to the receiving hospital to determine: death at the receiving hospital, or discharge with destination (home/institution and type of institution).

Figure 2
IABP switch occurring on the helipad.
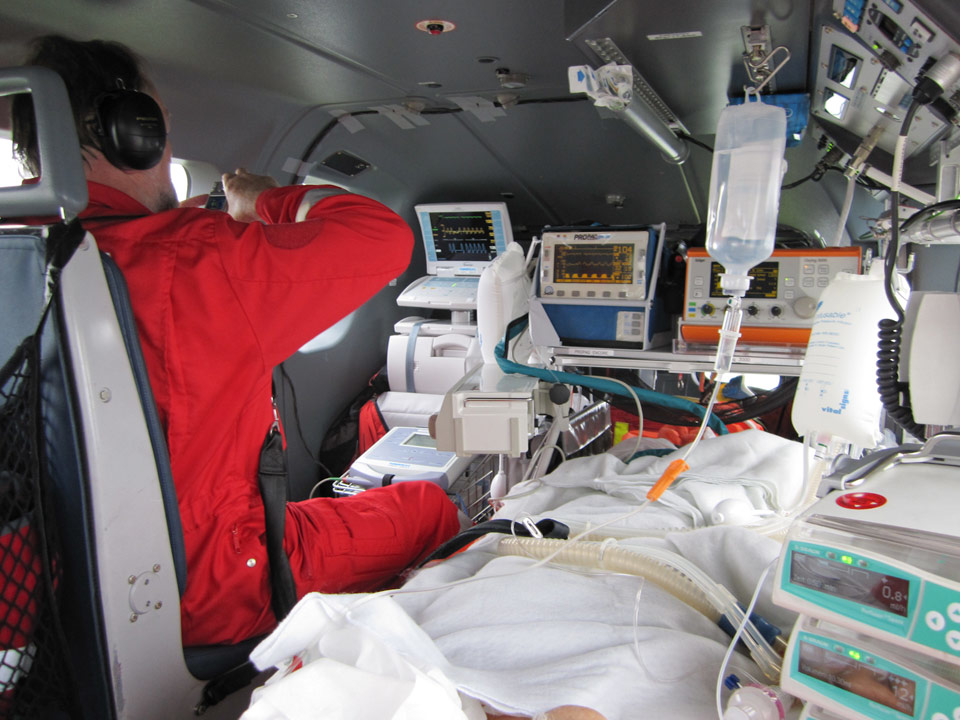
Figure 3
Rear cabin of the EC145 showing dimensions and available space when occupied by a patient and Rega team, including a perfusionist.
All patients for IABP transfer were transported by a Eurocopter EC145 helicopter, staffed with the standard Rega helicopter crew (pilot, helicopter emergency medical services crew member (HCM) and emergency physician) and reinforced by a certified perfusionist. The emergency physicians involved were board-certified anaesthesiologists or anaesthesiologists at certification level with training in cardiac anaesthesia, plus board-certified pre-hospital emergency physicians (Fähigkeitsausweis Notarzt SGNOR) or pre-hospital emergency physicians at certification level. Positioning of the patient, crew members and specific devices within the helicopter is shown in figure 1.
The process of IABP transfer is organised as follows: Upon receiving the request for transfer, the Rega IABP (Datascope GmbH, Bensheim, Germany; CS300) is immediately installed in the helicopter at the base of dispatch prior to the mission. At the hospital of pickup, the IABP-supported patient has to be transferred from the hospital unit to the helipad while still connected to the hospital’s IABP device (fig. 2). After loading the patient into the helicopter, the balloon catheter connections (Datascope, Bensheim, Germany IAB 7Fr Balloon-Catheter) are switched from the hospital’s pump unit to the helicopter’s IABP unit. At the target hospital, the process is reversed and the balloon catheter connections are switched back from the stationary IABP in the helicopter to the pump unit of the target hospital. It is important that all referring and receiving hospitals are aware of this process. Specifically, all health care providers directly involved must be fully informed about the timing, the site of handover and the respective steps of the required protocol.
During the entire transfer from the patient’s initial location in the referring hospital until the handover at the target location in the receiving hospital, the regular helicopter monitoring, infusion pumps and ventilator were employed. A Propaq Encore monitor (Protocol Systems, Inc, Beaverton, OR, USA), providing standard monitoring (ECG, non-invasive blood pressure and SpO2) including invasive arterial pressure and end-tidal CO2-measurement, was used for haemodynamic and respiratory surveillance of the patient during transport. If necessary, ventilation was provided using an Oxylog 3000 (Draeger Medical, Lübeck, Germany; SRMS 0020), and infusion pumps (Braun, Melsungen, Germany) were connected (fig. 3).
Data were recorded in Microsoft Excel (Microsoft Corp., Redmond, WA, USA). Statistics were calculated using IBM SPSS Statistics 19.0 (IBM Corp., Armonk, NY, USA). Data are presented as descriptive statistics. Values are shown as means ± SD and range.
Between September 2008 and October 2010, 38 patients (28 male, 10 female) with an IABP were transported by Rega helicopter. The geographic distribution of patient transfers within Switzerland is shown in figure 4. One patient transfer was from France to a Swiss hospital. Three patient transfers were conducted outside Switzerland (France [1 patient], Germany [2 patients]).
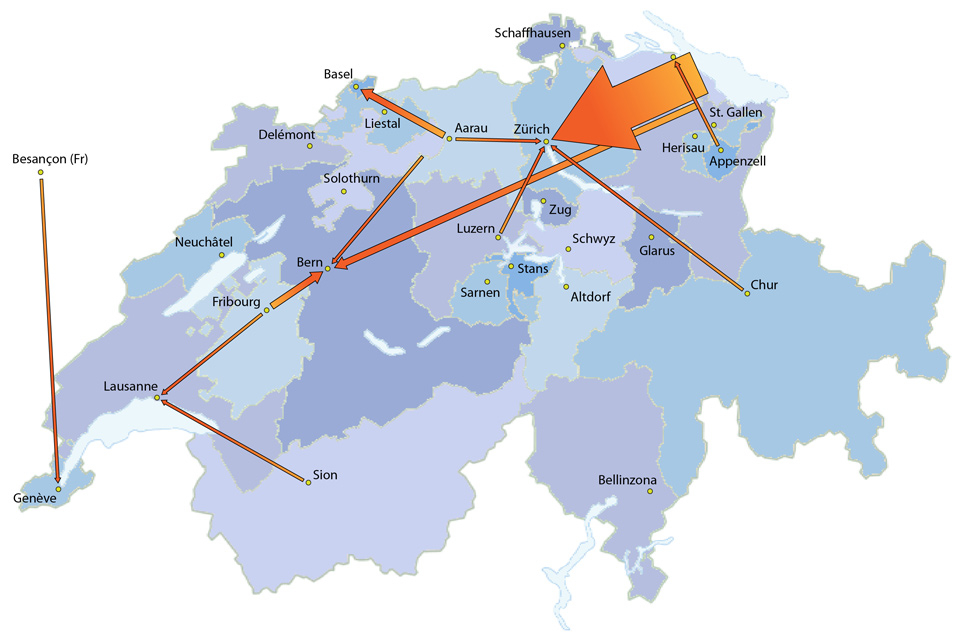
Figure 4
Geographical distribution of patient transfers in Switzerland. Transfers within France and Germany are not shown. Arrow size is proportional to the number of transfers. Thin arrows represent the transfer of 1 patient; arrows twice this width represent transfer of 2 patients; the large arrow from eastern Switzerland to Zurich represents the transfer of 21 patients.
The mean patient age was 64 ± 11 years (range: 34–85 years). A total of 24 patients (63%) were aged 34–69 years; 13 (34%) were aged 70–80 years; and one (2.5%) was older than 80 years. The leading cause for IABP support was ischaemic heart failure (32 patients, 84%). Dilated cardiomyopathy occurred in three patients (7.5%). Valvular heart failure and hypertensive heart failure occurred in 1 patient each (2.5% each). In one case (2.5%), myocarditis was suspected.
A total of 22 patients (58%) were breathing spontaneously via nasal cannula or face mask, and 16 patients (42%) were mechanically ventilated (intermittent positive pressure ventilation: 13; bilevel positive airway pressure: 2; not documented: 1).
With regard to infusion pump haemodynamic support, 18 patients (47%) were transported without any continuous inotropic or vasopressor medication.
The time course of the missions was recorded in the Rega database. The mean duration between arrival and take off at the referring hospital was 69 ± 30 min (range: 39–168 min). The mean effective flight time for the patient transfer was 22 ± 10 min (range: 9–55 min).
Follow-up of patients admitted to Swiss hospitals (35 of 38) was traced using the questionnaire mentioned above. Three patients were transferred within France or within Germany, and no outcome data were requested from these patients. Questionnaires on outcome were received from all 35 patients. Five patients (14%) died at the receiving hospital, 30 (86%) survived the time hospitalised in the receiving hospital and were discharged. According to the questionnaires, 11 patients (31%) were discharged home (2 directly, 6 via rehabilitation clinics, 3 by way of other hospitals). Another 19 patients (54%) were discharged to another institution (rehabilitation clinic or other hospital). The further follow-up of these patients was not provided in our questionnaire.
Based on our experience of the first 38 transfers of IABP patients, we developed a standard operating procedure (SOP) and a checklist for the hospital-staff involved (Appendices A and B).
Comprehensive treatment of cardiac failure includes early recognition, resuscitation at the primary hospital, inotropic and respiratory support, and in certain circumstances, mechanical circulatory support. Currently, early PCI is the decisive treatment option for ischaemic heart disease. Invasive coronary interventional therapy requires professional expertise and immediate 24-hour infrastructure including emergency and intensive care availability [5]. In a small country like Switzerland, regionalisation of respective services is essential to generate the necessary case load for the reasonable utilisation of personnel and technical resources. Transfer of patients between hospitals is and will be an increasing demand due to an aging society and the increasing invasiveness of recommended therapies. IABP is the most commonly used form of mechanical circulatory support [6]. The reduction in size and weight of the respective devices due to technical progress over the last years was the precondition to make such transfers possible [7].
In our case series of 38 patients, the inter-hospital transfer was uneventful in 37 cases. No major adverse event occurred. One minor adverse event, an initial technical failure of the helicopter’s IABP, could be solved before take-off at the referring hospital. Based on these findings, the helicopter transport, equipment provided, crew composition and predefined process offer a safe procedure for these complex transfers of high-risk patients.
Notably, a high percentage of patients (63%) in the collective presented were aged 34 to 69 years (mean age: 64 years, range: 34–85 years), demonstrating that the intervention encompassed a still active part of the population rather than a geriatric subgroup. With regard to middle range outcome data, our questionnaire was returned for all 35 investigated cases (100%). Only 5 patients (14%) died at the receiving hospital, whereas 30 (86%) survived the stay at the receiving hospital. Eleven patients (31%) were discharged home, either directly or by way of another institution and the other 19 patients (54%) survived at least the acute phase of their diseases and were transferred back to the referring hospital following acute interventional therapy or discharged to other hospitals or rehabilitation facilities. Generally, overall in-hospital mortality from acute myocardial infarction is between 3% and 6% [8]. In view of patients suffering from acute ischaemic heart disease that are treated with an IABP and PCI, the mortality differs widely and seems to depend on the co-existence of cardiogenic shock. Patients with ST segment elevation myocardial infarction without signs of cardiogenic shock, routinely treated with IABP and PCI, showed a 6-month mortality of 1.9% [9], whereas patients with a concomitant shock show a very high mortality of up to 56.9% for patients obtaining the same treatment [10]. Our survival rate reflects the heterogenous group of transferred patients concerning the presence of cardiogenic shock.
Interestingly, close to 50% of patients did not receive inotropic medication. Indication for invasive mechanical support may, therefore, be scrutinised. As addressed in the limitations section of the manuscript, questioning the selection of patients and/or indication of IABP (e.g., vs pharmacological) support was not within the focus of our investigation, and emergency physicians involved in the transfer were only made aware of a limited amount of medical information regarding the patient.
Clinical evidence supporting IABP use for cardiogenic shock remains controversial. The SMASH (Swiss Multicentre Evaluation of Early Angioplasty for Shock Following Myocardial Infarction) and TACTICS (Thrombolysis and Counterpulsation to Improve Survival in Myocardial Infarction Complicated by Hypotension and Suspected Cardiogenic Shock) trials had to be stopped before reaching sufficient patient inclusion for the calculated population sizes [11, 12]. Two further early investigations on IABP support were also disappointing [13, 14]. Recent studies [15, 16] as well as current guidelines [17] remain ambiguous with regard to clear recommendations for mechanical circulatory support in cardiogenic shock. Obviously, data on IABP support in cardiac failure are confounded by a systematic negative selection of the patients analysed.
Our data indicate that IABP used as a bridge prior to invasive acute intervention for cardiac failure can be used safely during helicopter transfer between primary care and specialised hospitals. Middle-range outcome data for our patient collective is promising, and IABP use despite all of the above-mentioned limitations has also been supported by a benchmark registry [18] and a recent IABP-shock trial [15]. A current editorial by Ohlmann et al. recommend the routine use of IABP in acute myocardial infarction patients with pre-shock or cardiogenic shock [19].
Costs for helicopter transfer provided by Swiss Air-Rescue (Rega) are calculated based on flight minutes. Our data show that the flight times for IABP patients are average compared with other inter-hospital transfers (22 ± 10 min). In contrast, the time from landing at the referring hospital to taking off with the IABP patient is substantially longer (68 ± 30 min; range: 39–168 min), demonstrating the complexity of patient handling. In addition, installation and removal of the pump in the helicopter require at least 30 additional minutes for each step. In most patients, the time required for safe implementation of IABP transfer exceeds the 90-minute door-to-balloon time recommended for emergency PCI. Therefore, in patients transferred for this procedure, insertion of a mechanical support device with consecutive delay must be balanced against loss of time.
For that reason, a comprehensive understanding of the underlying process and agreement regarding the priorities of patient management is mandatory to facilitate and accelerate handover and overall care of these critically ill patients. Implementation of a specialised team for this purpose has been recommended recently [7]. In addition, a well-defined process increases patient and crew safety. This is why we developed a standard operating procedure (SOP) for the IABP transfers. We communicate the attached SOP (Appendix A) and respective checklist for the referring and receiving hospitals (Appendix B). Rega provides this checklist in English, German, French and Italian for convenience.
This report is purely an observational investigation. Lack of a control group prevents the authors from making any conclusion on the effectiveness of mechanical circulatory support or risk/benefit ratio. One purpose of the manuscript is to provide the readers with some insight into the situation as experienced by emergency physicians responsible for the transfer. Individual cases are discussed in depth between the responsible staff physicians from the transfer-requesting hospital and the patient-receiving colleague at the target hospital. At the point at which the emergency physician becomes a part of the team, everything concerning the patient’s current and future treatment has been decided. As a consequence, the information provided to the helicopter physician is limited, with a focus restricted to what is medically necessary for the transfer. Due to our limited participation in the process as a whole, no specific haemodynamic or echocardiographic parameters or data were collected. In addition, the number of patients included is small. Rare complications will, therefore, remain undetected. Nevertheless, the case series is a consecutive summary of all respective transfers carried out by Rega during this 26-month period.
Inter-hospital transfers are high-risk operations for seriously ill patients. Following a predefined protocol and with well-informed referring and receiving hospitals and a specifically trained team, IABP-dependent patients with cardiac failure can be safely transported by helicopter to highly specialised centres for further invasive interventional or surgical care.
Appendix A: Standard operating procedure (SOP) for inter-hospital transfers of IABP-dependent patients http://www.smw.ch/fileadmin/smw/images/SMW-13552-Appendix-A.pdf (pdf).
Appendix B: Checklist for referring hospitals http://www.smw.ch/fileadmin/smw/images/SMW-13552-Appendix-B.pdf (pdf).
1 Antman EM, Anbe DT, Armstrong PW, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction; A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of patients with acute myocardial infarction). J Am Coll Cardiol. 2004;44:E1–E211.
2 Van de Werf F, Bax J, Betriu A, et al. Management of acute myocardial infarction in patients presenting with persistent ST-segment elevation: the Task Force on the Management of ST-Segment Elevation Acute Myocardial Infarction of the European Society of Cardiology. Eur Heart J. 2008;29:2909–45.
3 Farto e Abreu P, Thomas B, Loureiro J, Roquette J, Ferreira R. Inter-hospital transfer of critically-ill patients for urgent cardiac surgery after placement of an intra-aortic balloon pump. Rev Port Cardiol. 2002;21:1115–23.
4 Sinclair TD, Werman HA. Transfer of patients dependent on an intra-aortic balloon pump using critical care services. Air Med J. 2009;28:40–6.
5 Zeymer U, Thiele H, Zahn R. Einsatz der intraaortalen Ballonpumpe bei Patienten mit kardiogenem Schock. Notfall Rettungsmed. 2011;14:624–9.
6 Cove ME, MacLaren G. Clinical review: mechanical circulatory support for cardiogenic shock complicating acute myocardial infarction. Crit Care. 2010;14:235.
7 Fürnau G, Thiele H. Invasive Kreislaufunterstützungssysteme bei intra- und interhospitalen Transporten. Notfall & Rettungsmedizin. 2011;14:630–4.
8 Francois SJ, Erne P, Urban P, et al. Impact of a normal or non-specific admission ECG on the treatment and early outcome of patients with myocardial infarction in Swiss hospitals between 2003 and 2008. Swiss Med Wkly. 2010;140:w13078.
9 Patel MR, Smalling RW, Thiele H, et al. Intra-aortic balloon counterpulsation and infarct size in patients with acute anterior myocardial infarction without shock: the CRISP AMI randomized trial. JAMA. 2011;306:1329–37.
10 Zeymer U, Bauer T, Hamm C, et al. Use and impact of intra-aortic balloon pump on mortality in patients with acute myocardial infarction complicated by cardiogenic shock: results of the Euro Heart Survey on PCI. EuroIntervention. 2011;7:437–41.
11 Ohman EM, Nanas J, Stomel RJ, et al. Thrombolysis and counterpulsation to improve survival in myocardial infarction complicated by hypotension and suspected cardiogenic shock or heart failure: results of the TACTICS Trial. J Thromb Thrombolysis. 2005;19:33–9.
12 Urban P, Stauffer JC, Bleed D, et al. A randomized evaluation of early revascularization to treat shock complicating acute myocardial infarction. The (Swiss) Multicenter Trial of Angioplasty for Shock-(S)MASH. Eur Heart J. 1999;20:1030–8.
13 Flaherty JT, Becker LC, Weiss JL, et al. Results of a randomized prospective trial of intraaortic balloon counterpulsation and intravenous nitroglycerin in patients with acute myocardial infarction. J Am Coll Cardiol. 1985;6:434–46.
14 O’Rourke MF, Norris RM, Campbell TJ, Chang VP, Sammel NL. Randomized controlled trial of intraaortic balloon counterpulsation in early myocardial infarction with acute heart failure. Am J Cardiol. 1981;47:815–20.
15 Prondzinsky R, Lemm H, Swyter M, et al. Intra-aortic balloon counterpulsation in patients with acute myocardial infarction complicated by cardiogenic shock: The prospective, randomized IABP SHOCK Trial for attenuation of multiorgan dysfunction syndrome. Crit Care Med. 2010;38:152–60.
16 Sjauw KD, Engstrom AE, Vis MM, et al. A systematic review and meta-analysis of intra-aortic balloon pump therapy in ST-elevation myocardial infarction: should we change the guidelines? Eur Heart J. 2009;30:459–68.
17 Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non ST-Elevation Myocardial Infarction): developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons: endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. Circulation. 2007;116:e148–304.
18 Ferguson JJ, 3rd, Cohen M, Freedman RJ, Jr., et al. The current practice of intra-aortic balloon counterpulsation: results from the Benchmark Registry. J Am Coll Cardiol. 2001;38:1456–62.
19 Ohlmann P, Morel O, Kindo M, Radulescu B, Kremer H, Bareiss P. Use of intra-aortic balloon counterpulsation in cardiogenic shock complicating acute myocardial infarction. Do we really need more evidence? Crit Care Med. 2010;38:321–2.
Funding / potential competing interests: All authors work part or full-time with Swiss Air-Rescue (Rega). Roland Albrecht is chief medical director of Swiss Air-Rescue (Rega). No financial support and no other potential conflict of interest relevant to this article were reported.