Figure 1
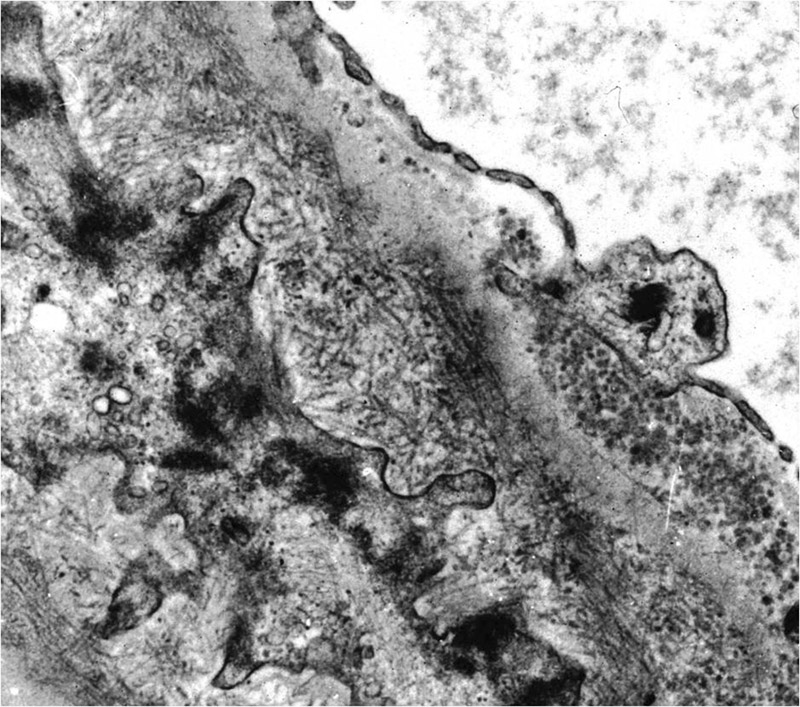
Electron microscopy: peripheral basement membrane with randomly arranged fibrillary deposits.
DOI: https://doi.org/10.4414/smw.2012.13578
A retrospective study
In 1977 Rosenmann and Eliakim described a glomerulopathy with amyloid-like fibrillary material which did not stain with Congo red [1]. Following this publication, there were a few similar case reports [2–6]. According to the criteria of Rosenstock [7] FGN is characterised by randomly arranged fibrillary deposits with a diameter of less than 30 nm (fig. 1). No hollow centres should be identifiable at magnifications of less than 30,000x. Congo-red staining has to be negative, while the immunofluorescence for immunoglobulines has to be positive. Deposits are often polyclonal and mostly made up of IgG4 in contrast to immunotactoid glomerulopathy (IT) in which deposits are almost always monoclonal and do not contain Ig4. FGN is a rare disease diagnosed in about 0.6 to 1% of all native kidney biopsies [7–10]. FGN has to be distinguished from IT, which likely represents a different clinical and pathologic entity [8, 11, 12]. FGN is usually not associated with monoclonal gammopathy or lymphoproliferative disorder.
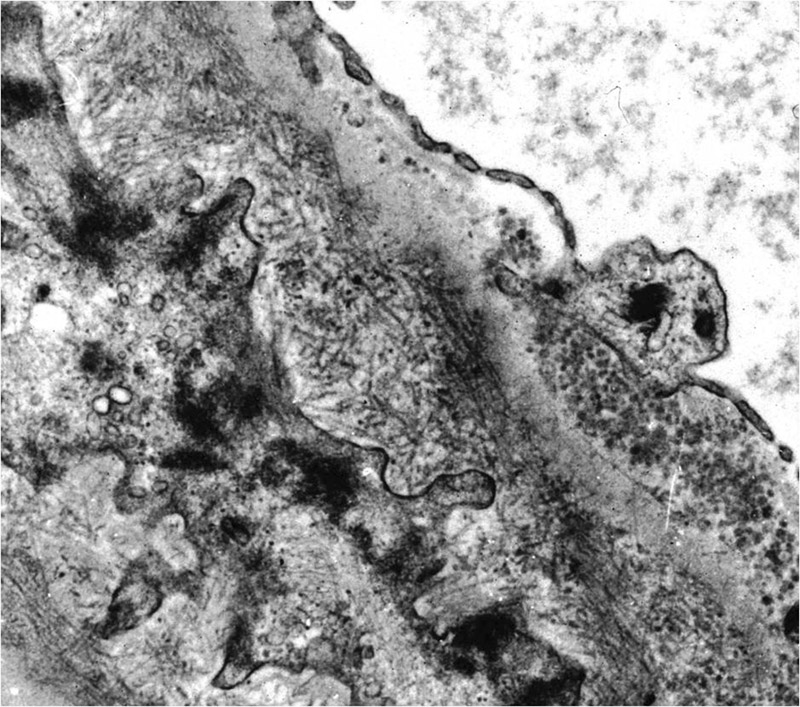
Figure 1
Electron microscopy: peripheral basement membrane with randomly arranged fibrillary deposits.
Most of the patients present with nephrotic proteinuria. Concomitant diseases e.g. hepatitis C viral infection [13], diabetes mellitus type 2 [14], hypocomplementemia [15] or HIV-infection [16] are rare, except in the recent study by Nasr [17] reporting one third of cases attended with malignancy (most commonly carcinoma) or autoimmune diseases (Crohn’s disease, systemic lupus erythematodes, Graves’ disease, and idiopathic thrombocytopenic purpura).
There are only few studies [7, 8, 11, 17] considering the clinical outcome of patients with FGN. In one study by Iskandar et al. [8] 15 (54%) of 28 patients with FGN developed ESRD during an average follow-up of 24 months. Fogo et al. reported 26 patients with FGN, 44% developed ESRD during a mean follow up of 23 months [9]. In study by Rosenstock 25 (45%) out of 56 patients with FGN developed ESRD during a mean follow up of also 23 months [7]. In a recent study by Nasr 29 out of 66 patients or 44% developed ESRD [17].
None of these studies showed a better outcome in patients treated with immunosuppressive drugs [7, 8, 11, 17]. Patients in these studies received various immunosuppressants: steroids, cyclophosphamide, mycophenolate mofetil, azathioprine and cyclosporine. In a previous retrospective study with three patients, we observed a favourable course when an early steroid treatment was begun [18]. None of the three patients reached end stage renal disease (ESRD). Therefore, we decided to assess the long term follow up of all the patients with FGN diagnosed since 1992 at the Institute for Pathology Basel. This retrospective study was designed to provide more comprehensive data regarding the outcome of patients with FGN.
We performed a retrospective surveillance study to examine the clinical course and the outcome of FGN.
All native kidney biopsies examined by light and electron microscopy at the Basel Institute for Pathology, Switzerland, were evaluated for FGN from 1992 until 2007. All cases of FGN were carefully reviewed using the diagnostic criteria for FGN published by Rosenstock et al. [7] (i) randomly oriented glomerular deposition of fibrils with a lack of hollow centers at magnifications of <30,000x, (ii) fibril diameter less than 30nm (iii) negative Congo red-staining. Only biopsies with a positive staining for immunoglobulin in the immunofluorescence were included. The patients previously reported [18] were included into the analysis.
A questionnaire was mailed to all physicians of the identified cases of FGN asking for the following variables: death of any cause, onset of ESRD and applied renal replacement therapy, quantitative protein in the urine, serum creatinine, creatinine clearance (measured or estimated), concomitant diseases, pharmacological treatment of FGN. Serum creatinine and creatinine clearance were asked for at the time of kidney biopsy and at the time of last follow up. Estimated GFR was calculated using the abbreviated formula of modification of diet in renal disease (MDRD) [19].
All data are reported as mean/median, range. Statistical analyses were performed using the JMP 8.02 statistics package ( http://www.jmp.com ). For all analyses, differences were considered statistically significant for p-values <0.05. Mann-Whitney-U-Test and Wilcoxon-signed rank test were used to determine significance for numerical data, Fisher’s exact test was used to assess the significance for categorical data. One-way ANOVA was used to compare among multiple groups.
From 1992 to 2007 a diagnosis of FGN was made in 20 out of 4,990 native kidney biopsies analysed by electron microscopy representing 0.4% of all native kidney biopsies and 0.65% of all cases with a diagnosis of glomerulonephritis (GN) examined at the Basel Institute of Pathology. Sixteen cases could be analysed in detail. The questionnaire was not answered in three cases (15%), and FGN was diagnosed post-mortem in one case. Demographic data and characteristics of the 16 patients at the time of diagnosis are shown in table 1. The mean eGFR (MDRD) was 49.3 ml/min/1.73 m2 with a broad range from 103 to 5 ml/min/1.73 m2. Sixty-three percent (n = 10) of the patients had an eGFR below 60 ml per minute and 68.8% (n = 11) had proteinuria in the nephrotic range. Seven patients (43.8%) had hypertension at the time of diagnosis. Diabetes mellitus and rheumatoid arthritis was found in one and two patients respectively. Three patients (18.8%) suffered from lymphoproliferative disease: myelodysplastic syndrome, Non Hodgkin lymphoma, and osteomyelofibrosis. All of them received an immunosuppressive treatment. The patient with osteomyelofibrosis had a stem cell transplant.
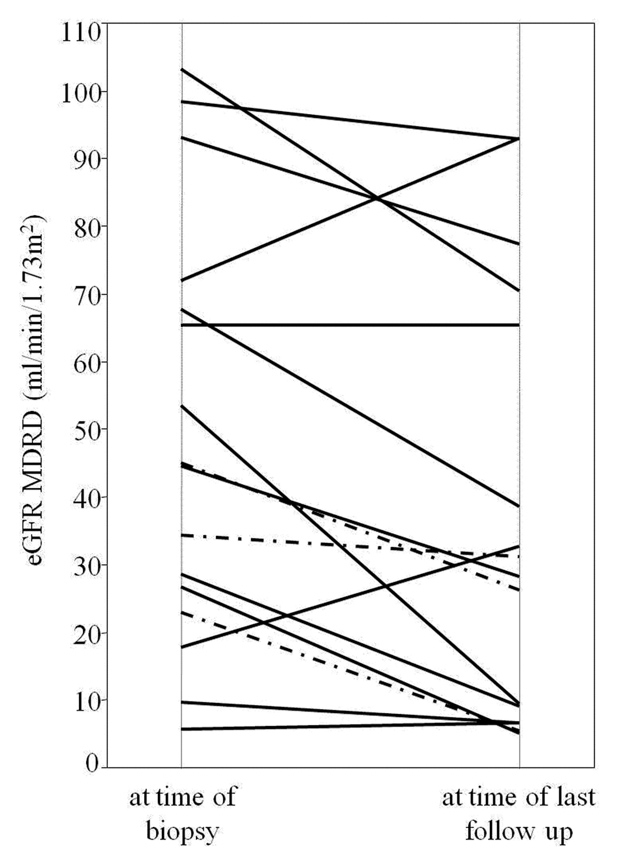
Figure 2
Each solid line shows the course of eGFR of a patient with immunosuppressive treatment, each dashed line shows the course of eGFR of a patient without immunosuppressive treatment.
56.2% (n = 9) of the patients had a histological pattern of membranous glomerulonephritis (MGN), 31.3% (n = 5) of membranoproliferative glomerulonephritis (MPGN) and 12.5% (n = 2) of mesangial proliferative/sclerosing glomerulonephritis (MES). Crescents in the biopsy were found in 50% (n = 8). Thirteen out of 16 patients received any immunosuppressive therapy after a diagnosis of FGN was made: All 13 patients received steroids, five (38%) were additionally treated with cyclophosphamide and one patient (7.7%) received cyclosporine following the treatment with cyclophosphamide.
Three patients did not receive immunosuppressive treatment. Two because their serum creatinine was stable during several months and one because of suspected endocarditis.
The mean follow up was 35 months (1–115.1, median 25.4). Follow up data are shown in table 2. Six patients died (37.5%), three without having ESRD, two died while on hemodialysis, and one patient died in uremia at the age of 84 years without having renal replacement therapy. Six patients (37.5%) reached ESRD, five of them started hemodialysis.
Patients without nephrotic syndrome at the time of biopsy and patients with eGFR >60 ml/min tend to have a lower risk to proceed to ESRD but have to be carefully interpreted as the analyzed number is very small (table 2). Angiotensin converting enzyme inhibitors or angiotensin II receptor antagonists were given in 62.5 percent of all patients. None of the six patients treated with immunosuppressive agents at a time when their kidney function was normal experienced ESRD and patients treated with immunosuppression had a tendency of delayed decrease of GFR over time (–8.3 vs. –13.9 ml/min). Delta eGFR from the time of diagnosis to the end of follow up is shown in figure 2. Five of the 13 patients with immunosuppressive treatment received cyclophosphamide and two of them suffered ESRD in contrast to three of eight patients in the group treated with steroids alone. Due to the small number of cases no reliable results were obtained. Patients with MGN and non nephrotic proteinuria had a better outcome as compared to MPGN, and MES (table 3)
| Table 1: Patient characteristics at time of biopsy; n = 16 mean/median (range). | |
| Age (years) | 60/59.9 (33–84.4) |
| Female/male | 7/9 (43.8%/56.2%) |
| eGFR MDRD (ml/min/1.73 m2) | 49.3/44.9 (5.7–103.3) |
| eGFR <60 ml/min/1.73 m2 | 10 (63%) |
| Proteinuria mg/day | 7,300/7,900 (500–18,400) |
| Patients with nephrotic syndrome | 11 (68.8%) |
| Concomitant diseases: | |
| – Hypertension | 7 (43.8%) |
| – Diabetes mellitus | 1 (6.3%) |
| – Lymphoproliferative disease | 3 (18.8%) |
| – Rheumatoid disease | 2 (12.5%) |
| Light microscopic findings: | |
| Membranoproliferative GN (MPGN) | 9 (56.2%) |
| Mesangioproliferative GN (MES) | 5 (31.3%) |
| Membranous GN (MGN) | 2 (12.5%) |
| Glomerular crescents | 8 (50.0)% |
| Table 2: Data at time of biopsy and on last follow up stratified according to treatment regimen mean (range). | ||
| Immunosuppressive therapy | With therapy (n = 13) | Without therapy (n = 3) |
| At time of biopsy: | ||
| Age (years) | 58.6 (33–84.4) | 66.0 (54.4–78.8) |
| Female / Male | 5/8 (38.5%/ 61.5%) | 2/1 (66.7%/33.3%) |
| eGFR MDRD (ml/min/1.73 m2) | 52.85 (5.7–103.3) | 34.2 (23–45.1) |
| eGFR <60 ml/min/1.73 m2 | 7 (53.8%) | 3 (100%) |
| Proteinuria mg/day | 6,900 (500–18,400) | 9,300 (880–15,000) |
| With nephrotic syndrome | 9 (69.2%) | 2 (66.7%) |
| Outcome: | ||
| – Deaths / time to death (months) | 4 (30.8%) / 24.6 | 2 (66.7%) / 29.7 |
| – ESRD / time to ESRD (months) | 5 (38.5%) / 11.6 | 1 (33.3%) / 8.6 |
| – Dialysis* | 4 (30.8%) | 1 (33.4%) |
| – Proteinuria <1000 mg/day | 7 (53.8%) | 1 (33.4%) |
| – Improvement of eGFR | 2 (15.4%) | 0 (0%) |
| – Δ GFR/year (ml/min/year) | –8.3 | –13.9 |
| – Mean follow up (months) | 37 (1–115) | 27 (11.6–47.7) |
| Light microscopic findings: | ||
| Membranoproliferative GN (MPGN) | 9 (69.2%) | 0 (0%) |
| Mesangioproliferative GN (MES) | 2 (15.3%) | 3 (100%) |
| Membranous GN (MGN) | 2 (15.4%) | 0 (0%) |
| Glomerular crescents | 8 (61.5%) | 0 (0%) |
| * One patient denied hemodialysis therapy. | ||
| Table 3: Outcome with regard to the observed type of glomerulonephritis: at time of biopsy (Bx) / last follow up (LFU). | ||||
| Mean eGFR ml/min Bx / LFU | Mean proteinuria mg/day Bx / LFU | Crescents (%) | ESRD (%) | |
| MPGN (n = 9) | 52 / 45 | 6,500 / 4,600 | 7 (77.8) | 3 (33.3) |
| MES (n = 5) | 31.6 / 15.4 | 7,700 / 8,100 | 1 (20) | 3 (60) |
| MGN (n = 2) | 80.5 / 58.0 | 9,900 / 500 | 0 (0) | 0 (0) |
| Table 4: Summary of all studies concerning fibrillary Glomerulonephritis with more than 10 patients and clinical outcome data [7, 8, 11, 17]. | ||||||
| Iskandar 1992 | Fogo 1993 | Rosenstock 2003 | Nasr 2011 | Kalbermatter 2012 | Total | |
| Patients with FGN | 28 | 26 | 61 | 66 | 16 | 197 |
| MGN (%) | n/a | n/a | 4 (7) | 1 (2) | 2 (12.5) | 7/143 |
| MPGN (%) | n/a | n/a | 27 (44) | 61 (91) | 9 (56.2) | 107/143 |
| MES (%) | n/a | n/a | 30 (49) | 4 (7) | 5 (31.3) | 39/143 |
| Mean follow up | 24 | 23 | 23 | 52 | 35 | 30.8 |
| Nephrotic (%) | n/a | 20 (77) | 32 (52) | 35 (55%) | 11 (68.8) | 98/169 |
| Mean proteinuria | 6,000 | 5,450 | 6,480 | 5,620 | 7,300 | |
| Mean serum creatinine | 3.7 | 3.2 | 3.1 | 2.1 | 2.4 | |
| Crescents % | 19 | 27 | 39 | 17 | 50 | 34.4 |
| IS | 6 | 4 | 20 | 29 | 13 | 72/197 |
| ESRD | 15 (52%) | 11 (44%) | 25 (41%) | 29 (44%) | 6 (38%) | 57/131 |
FGN is a heterogeneous disease associated with significant risk of ESRD. The data presented confirms the poor prognosis of FGN. About one third of patients rapidly developed ESRD in a mean time of 8 months. But the outcome depends on the type of glomerulonephritis by light microscopy and the amount of proteinuria at the time of diagnosis. FGN in the context of MGN seems to have a more favourable prognosis as compared to MES and MPGN and nephrotic range proteinuria is associated with poor outcome. The group without immunosuppressive therapy was too small to compare the outcome with the group with immunosuppressive treatment. None of the six patients, however, who were treated with immunosuppressive agents at a time when their kidney function was normal experienced ESRD over a mean follow up of 46 months, a finding that supports our hypothesis [18], that early immunosuppressive treatment can improve the outcome and delay the decrease of kidney function. – It can also explain the more favourable results as compared to Rosenstock and colleagues [7] who observed no benefit of steroid treatment alone or in combination with cyclophosphamide or cyclosporine in 20 out of 56 patients with FGN. The mean serum creatinine was higher (3.1 mg/dl (0.5–14)) than in our cohort (2.4 mg/dl (0.7–8.5)). We had a higher percentage of MGN (12.5%) than the group of Rosenstock (7%). Our collective may tend to have earlier stages of renal disease and less severe light microscopic findings. However the percentage of patients with nephrotic syndrome was higher in our cohort (68.8%) than in the cohort of Rosenstock (52%). See also table 4.
The success of immunosuppressive therapy may also depend on the type of glomerulonephritis seen by light microscopy. Whether steroid therapy is superior to other immunosuppressants cannot be answered. None of our patients were treated with rituximab which plays a potential role in the treatment of FG as supported by a recent study [20].
The current study is limited by its multicentre, retrospective and observational character. Neither treatment nor follow-up were standardised and there may be a bias due to missing data caused by unanswered questionnaires. Nevertheless, it provides additional information about this rare disease.
In conclusion: Fibrillary glomerulonephritis is a heterogeneous disease associated with significant risk of ESRD and mortality. The course of the disease may be influenced by the histological type of the glomerulonephritis and the time of therapy.
1 Rosenmann E, Eliakim M. Nephrotic syndrome associated with amyloid-like glomerular deposits. Nephron. 1977;18(5):301–8.
2 Sturgill BC, Bolton WK, Griffith KM. Congo red-negative amyloidosis-like glomerulopathy. Human Pathology. 1985;16(3):220–4.
3 Duffy JL, Khurana E, Susin M, Gomezleon G, Churg J. Fibrillary renal deposits and nephritis. Am J Pathol. 1983;113(3):279–90.
4 Korbet SM, Schwartz MM, Rosenberg BF, Sibley RK, Lewis EJ. Immunotactoid glomerulopathy. Medicine. 1985;64(4):228–43.
5 Alpers CE, Rennke HG, Hopper J, Biava CG. Fibrillary glomerulonephritis – an entity with unusual immunofluorescence features. Kidney Int. 1987;31(3):781–9.
6 Churg J, Venkataseshan VS. Fibrillary glomerulonephritis without immunoglobulin deposits in the kidney. Kidney Int. 1993;44(4):837–42.
7 Rosenstock JL, Markowitz GS, Valeri AM, Sacchi G, Appel GB, D’Agati VD. Fibrillary and immunotactoid glomerulonephritis: Distinct entities with different clinical and pathologic features. Kidney Int. 2003;63(4):1450–61.
8 Iskandar SS, Falk RJ, Jennette JC. Clinical and pathological features of fibrillary glomerulonephritis. Kidney Int. 1992;42(6):1401–7.
9 Fogo A, Qureshi N, Horn RG. Morphologic and clinical-features of fibrillary glomerulonephritis versus immunotactoid glomerulopathy. Am J Kidney Dis. 1993;22(3):367–77.
10 Hvala A, Ferluga D, Vizjak A, Koselj-Kajtna M. Fibrillary noncongophilic renal and extrarenal deposits: A report on 10 cases. Ultrastructural Pathology. 2003;27(5):341–7.
11 Fogo A, Qureshi N, Horn RG. Morphologic and clinical-features of fibrillary glomerulonephritis versus immunotactoid glomerulopathy. Am J Kidney Dis. 1993;22(5):757.
12 Bridoux F, Hugue V, Coldefy O, Goujon JM, Bauwens M, Sechet A, et al. Fibrillary glomerulonephritis and immunotactoid (microtubular) glomerulopathy are associated with distinct immunologic features. Kidney Int. 2002;62(5):1764–75.
13 Markowitz GS, Cheng JT, Colvin RB, Trebbin WM, D’Agati VD. Hepatitis c viral infection is associated with fibrillary glomerulonephritis and immunotactoid glomerulopathy. J Am Soc Nephrol. 1998;9(12):2244–52.
14 Gielen GAL, Wetzels JFM, Steenbergen EJ, Muddle AH. Fibrillary glomerulonephritis in a patient with type 2 diabetes mellitus. Netherlands Journal of Medicine. 2006;64(4):119–23.
15 Suzuki S, Konta T, Koizumi R, Nishida W, Abiko H, Kubota I. Fibrillary glomerulonephritis with hypocomplementemia. Internal Medicine. 2003;42(8):719–22.
16 Haas M, Rajaraman S, Ahuja T, Kittaka M, Cavallo T. Fibrillary/immunotactoid glomerulonephritis in HIV-positive patients: a report of three cases. Nephrology Dialysis Transplantation. 2000;15(10):1679–83.
17 Nasr SH, Valeri AM, Cornell LD, Fidler ME, Sethi S, Leung N, Fervenza FC. Fibrillary glomerulonephritis: A report of 66 cases from a single institution. Clin J Am Soc Nephrol. 2011;6(4):775–84.
18 Dickenmann M, Schaub S, Nickeleit V, Mihatsch M, Steiger J, Brunner F. Fibrillary glomerulonephritis: Early diagnosis associated with steroid responsiveness. Am J Kidney Dis. 2002;40(3):E9.
19 Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. Modification Diet Renal Dis Study G. A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Ann Intern Med. 1999;130(6):461‒70.
20 Collins M, Navaneethan SD, Chung M, Sloand J, Goldman B, Appel G, Rovin BH. Rituximab treatment of fibrillary glomerulonephritis. Am J Kidney Dis. 2008;52(6):1158–62.
Acknowledgements: Denes Kiss, MD, Department of Nephrology, Kantonsspital Liestal, Switzerland; Zsusanna Varga, MD, Department of Pathology University Hospital Zurich, Switzerland; Piero Sandoz, MD, Department of Nephrology, Bürgerspital Solothurn, Switzerland; Hans Jakob Gloor, MD, Department of Nephrology, Kantonsspital Schaffhausen, Switzerland.
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article was reported.