Perception of non-invasive ventilation in adult Swiss intensive care units
DOI: https://doi.org/10.4414/smw.2012.13551
Igor
Salvadè, Guido
Domenighetti, Philippe
Jolliet, Marco
Maggiorini, Hans-Ueli
Rothen
Summary
The real utilisation scenario of non-invasive ventilation (NIV) in Swiss ICUs has never been reported. Using a survey methodology, we developed a questionnaire sent to the directors of the 79 adult ICUs to identify the perceived pattern of NIV utilisation.
We obtained a response rate of 62%. The overall utilisation rate for NIV was 26% of all mechanical ventilations, but we found significant differences in the utilisation rates among different linguistic areas, ranging from 20% in the German part to 48% in the French part (p <0.01). NIV was mainly indicated for the acute exacerbations of COPD (AeCOPD), acute cardiogenic pulmonary edema (ACPE) and acute respiratory failure (ARF) in selected do-not-intubate patients. In ACPE, CPAP was much less used than bi-level ventilation and was still applied in AeCOPD. The first line interface was a facial mask (81%) and the preferred type of ventilator was an ICU machine with an NIV module (69%).
The perceived use of NIV is generally high in Switzerland, but regional variations are remarkable. The indications of NIV use are in accordance with international guidelines. A high percentage of units consider selected do-not-intubate conditions as an important additional indication.
Abbreviations:
NIV = noninvasive ventilation;
ICU = intensive care unit;
AeCOPD = acute exacerbation of chronic obstructive pulmonary disease;
ACPE = acute cardiogenic pulmonary edema;
CAP = community acquired pneumonia;
ARF = acute respiratory failure
Introduction
Non-invasive ventilation (NIV) has emerged as an important respiratory modality in critical care. Its role in the management of acute respiratory failure has been clarified in recent years by many clinical trials [1, 2]. In selected groups of patients, current evidence demonstrates that NIV therapy reduces the need for endotracheal intubation and the mortality rate; this is true for the acute respiratory failure in patients with COPD exacerbations [AeCOPD], cardiogenic pulmonary edema [ACPE] and during episodes of hypoxaemic respiratory failure associated with pneumonia in immunocompromised patients [3–6]. Moreover, a growing body of evidence supports the use of NIV as a prevention of post-extubation respiratory failure and as a weaning bridge in difficult-to-wean COPD-patients [7–10]. Interestingly, studies of NIV utilisation in the acute care setting have found that major disparities may exist between different health care providers. This is rather surprising, considering the evidence supporting its use and the consensus of opinions. Major reasons reported for low utilisation rates include lack of physician knowledge, weakly trained staff and inadequate equipment [11].
Two different studies demonstrated that NIV utilisation may vary widely among different Institutions. An European study showed that NIV was poorly applied as a primary form of ventilation in patients in whom mechanical ventilation was indicated, while a second study demonstrated that 52% of 264 hospitals surveyed in the UK didn’t use this technique at all [12, 13].
To date there are no data reporting on NIV utilisation in adult ICUs in Switzerland. By using an ad hoc designed questionnaire, we explored the attitudes concerning NIV and its applications in common clinical settings.
Material and methods
We used a questionnaire consisting of 43 relevant items. Questions were generated based on earlier surveys and perceived areas of specific interest: type of ICU, geographical location, numbers of beds and patients treated in 2008, years of experience with NIV and percentage of total mechanical ventilation and NIV utilisation. Additional fields were: validated NIV indications, selection of patients for NIV, monitoring, interfaces used, type of ventilators, modes of ventilation and timing of ventilation, degree of satisfaction and possible improvement suggestions. Since 2007, the Swiss Society of Intensive Care Medicine requires from each ICU that a minimal data set of information be generated on-line; this structured set of information allowed a more precise response format as multiple choice options and scales. The questionnaire was mailed to the directors of all the adult certified Swiss ICUs in 2009. The recruitment was performed between January and June 2009. Non-responders were further contacted by mail or phone. Centres were recruited in all the linguistic parts of Switzerland (German and Romansh, French, Italian). In order to obtain representative data we planned to enrol ICUs from at least 4 tertiary, 10 secondary and 20 primary hospitals. To enhance participation, we decided to compensate the time spent to fill a questionnaire with 80 Swiss francs. Considering the nature of the study, an approval from the Ethics Committee was not required.
Statistical methods
Data are expressed as the mean ± SD for continuous variables and as the frequency for nominal variables. Continuous variables were compared using at-test. The Mann-Whitney U test was employed for variables with a distribution that was not normal. Analysis was performed using Systat 12 (Systat Software Inc, San José, CA).
Results
Response rate, characterisation of the ICUs and NIV utilisation
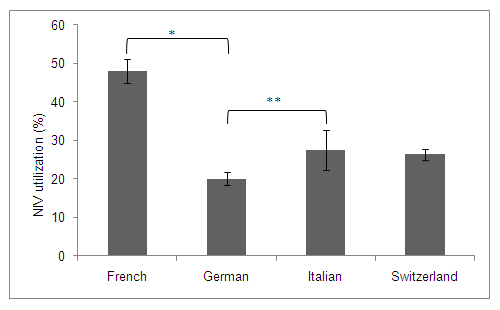
We obtained replies from 49 out of 79 contacted certified adult ICUs, which corresponds to a response rate of 62%. Six university ICUs (2 from Basel, 2 from Zurich, Bern and Geneva), 15 middle-sized hospitals and 28 regional hospitals responded to the questionnaire. This sample greatly exceeded the expectations outlined above. Geographically, all the regions of the country were represented in this survey. 34 replies came from the German and Romansh parts (=57.6% of all German Units with all German University centres, representing a total of 37,666 patients admitted during 2008), 10 from the French part (66.6% of the French Units with 1 University centre, representing a total of 10,298 admitted patients) and 5 from the Italian part of Switzerland (100% of the units of this region, representing a total of 3,442 patients). The majority of units was multidisciplinary (n = 40; 82%), five were exclusively surgical (10%) and four exclusively medical (8%; table 1). The directors were asked to provide data regarding the use of NIV as the most likely percentage of all patients receiving ventilator assistance. Figure 1 shows the perceived percentage of NIV utilisation in function of all ventilated patients: as shown on this graph, 19 of the ICUs reported a non-invasive ventilation in less than 20% of their mechanically ventilated patients; a similar number of units used NIV in 20–40% of all ventilated patients. Only few centres ventilated in more than 40% of cases. The latter were mostly units of tertiary teaching hospitals having a long experience in NIV utilisation.

Figure 1
Perceived percentage of NIV utilisation. The y-axis shows the number of responses (= number of units). On the x-axis, the perceived percentage of non invasive ventilation (NIV) in function of all ventilated patients for a given unit, is shown.
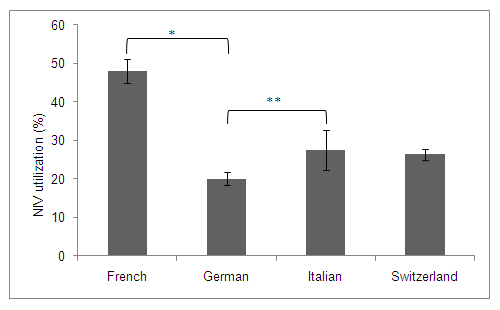
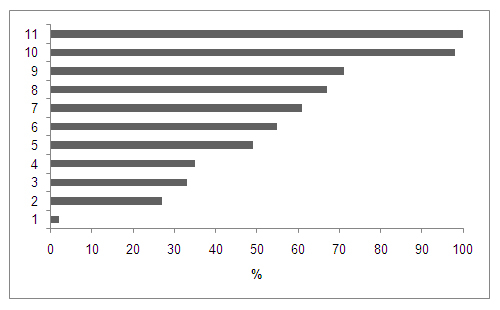
Figure 2
NIV utilisation in the different geographical areas.
*p <0.001 ; **p = 0.47
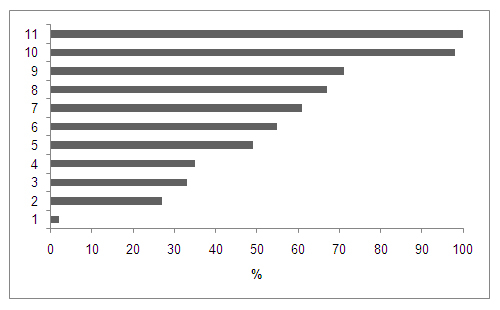
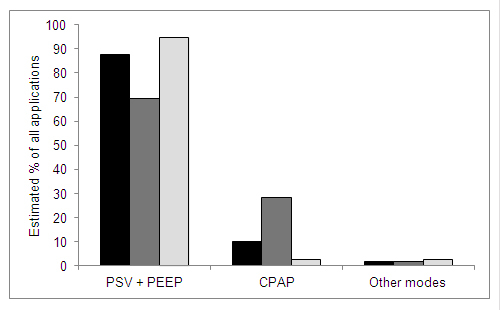
Figure 3
Estimated declaration of NIV applications according to current clinical recommendations.
1: others; 2: ALI/ARDS; 3: weaning failure in COPD; 4: asthma exacerbation; 5: severe community acquired pneumonia; 6: respiratory failure in immune compromised states; 7: postoperative respiratory failure; 8: extubation failure; 9: respiratory failure in a do-not-intubate patient; 10: acute cardiogenic pulmonary edema; 11: COPD exacerbation
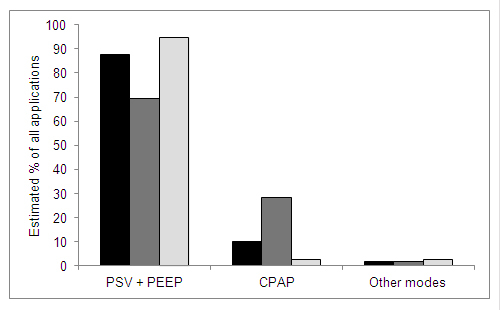
Figure 4
Reported modes of ventilation in COPD exacerbation (black), Cardiogenic pulmonary edema (dark grey) and CAP/ALI/ARDS (light grey). PSV = Pressure Support Ventilation; CPAP = Continuos Positive Airway Pressure; PEEP = Positive End Expiratory Pressure; CAP = Community Acquired Pneumonia.
The overall estimated utilisation rate for NIV in Switzerland was 26.4% [CI: 25.0–27.8%] of all patients in whom therapy with mechanical ventilation was initiated in the setting of acute respiratory failure. As shown in figure 2, there is a marked variation in utilisation of NIV between the French and the German part (p <0.001): concomitantly, there was a significant difference (p = 0.013) in the years of previous experience between the French and the German part (table 1). Overall, the mean duration of experience with NIV in Switzerland was of 10.2 years [CI: 8.9–11.5]. The NIV utilisation rates between university and non-university hospitals didn't demonstrate a significant difference (p = 0.76). The utilisation rate was similar (p: NS) between small-sized (less than 8 beds), medium-sized (8–12 beds) and large-sized (more than 12 beds) units.
Indications for NIV
The main indications for NIV utilisation were AeCOPD and ACPE (fig. 3). A lower utilisation was shown for other evidence-based indications, specifically pneumonia in the immunocompromised patient, weaning failure in COPD patients and extubation failure in high-risk patients. Severe community acquired pneumonia (CAP) and ALI/ARDS were less frequent indications. A high percentage of units [n = 35; 71%] considered a “do-not-intubate” status as a good indication for NIV. Concerning the contraindications for NIV, the assembled data matched the current guidelines; however, the presence of abundant secretions in the airways (22% of the units) and an agitated patient (24% of the units) were not considered an absolute contraindication for NIV.
Site of the initiation of NIV and monitoring
The study showed that the preferred location of NIV initiation in the acute hospital is the ICU (86%). Only few centres applied NIV in the emergency department (14%). The general ward has not been reported as a site for NIV initiation. The initial response to NIV was normally checked after 30 min (65% of responses), latest after 1 hour (94%); arterial blood gas measurements, continuous SpO2 and respiratory rate, represented the main parameters applied for monitoring. The main criteria adopted for deciding the duration of NIV were patient’s tolerance (40%) and the severity of acute respiratory failure (40%). The decision to stop NIV was carried out by the attending physician (86%). Only few ICUs (14%) used pre-defined local protocols for initiating, performing and discontinuing NIV.
Interfaces and modes of ventilation
The most used interface was the oro-nasal facemask. Important reasons reported for this choice were avoidance of side effects, patient comfort, simplicity of fitting and nurse confidence. Very few centres used the helmet (2%) for ACPE. The specific NIV indications didn’t influence the choice of the interface for the majority of ICUs (70%). During an AeCOPD the preferred machine was an ICU ventilator with NIV module in 74% of all applications. Here, the acute respiratory failure was approached with a bi-level mode of ventilation (PSV + PEEP) in 88% of all applications; few centres (10%) still used CPAP for this indication (fig. 4). For centres using the bi-level mode, the mean initial setting of the inspiratory pressure was 10 ± 0.5 cm H2O and the mean initial end-expiratory pressure (PEEP) was 5.1 ± 0.2 cm H2O.
In ACPE, the ICU ventilator with NIV module was the preferred type of ventilator in 69% of all applications. CPAP, which is considered equivalent to bi-level ventilation in terms of effectiveness during ACPE, was much less used than expected (29%; fig. 4). For those using the bi-level mode, the initial setting of the ventilator was a mean inspiratory pressure level of 9.0 ± 1.1 cm H2O and a mean PEEP of 6.65 cm H2O (±0.08).
Finally, in CAP and ALI/ARDS, bi-level ventilation (fig. 4) was the leading NIV strategy, with an ICU ventilator used in 82% of all applications. The initial setting was a mean inspiratory pressure level of 10.4 ± 1.2 cm H2O and a PEEP of 6.2 ± 0.1 cm H2O.
Degree of satisfaction and suggestions
The directors of the ICUs were asked about the reasons of low utilisation rates and about their general experience, satisfaction and suggestions. The majority of them reported a high degree of satisfaction. For those reporting moderate or low degree of satisfaction, almost from ICUs located in the German and Italian part of Switzerland, the reasons were lack of knowledge about NIV and lack of adequate equipment, typically the interface; as a consequence, more practical teaching was a frequent request in the field of improvement suggestions. By attributing a numerical value to the satisfaction degree, this was significantly higher in the French than in the German part of Switzerland (p = 0.032). Moreover and in general, centres with low utilisation rates expressed a significantly lower degree of satisfaction than did the centres where NIV was more frequently applied (p = 0.023).
|
Table 1: Respondents’ characteristics according to different geographical areas. |
| |
French
|
German
|
Italian
|
|
ICUs
|
|
|
|
| Universitary n
|
1 |
5 |
|
| Non-universitary n
|
9 |
29 |
5 |
|
Type of ICU
|
|
|
|
| Surgical n
|
|
5 |
|
| Medical n
|
1 |
3 |
|
| Interdisciplinary n
|
9 |
26 |
5 |
|
Number of beds
|
109 |
378 |
38 |
| Patients treated [2008] n
|
10,298 |
37,666 |
3,442 |
|
Previous practice withNIV
years
|
13.1 ± 2.5* |
9.0 ± 1.6* |
12.6 ± 3.9 |
| *p = 0.013 |
Discussion
This survey demonstrates that NIV utilisation is substantially important in the Swiss ICUs. As represented in figures 1 and 2, the utilisation rate is variable and heterogeneously spread throughout the different areas of the country. For instance, a minority of the ICUs reported a NIV utilisation rate substantially higher than 40% of all ventilatory applications; also, there was a significant regional difference in the use of NIV between the French and German speaking parts of Switzerland. On the whole, general Swiss utilisation rate (26%), albeit similar to that reported in a recent French ICU survey (23%; 14), is higher than that detailed in other reports including a multinational cohort observational study (15), a German study (16) and a survey performed in New England-USA acute-care hospitals (20%; 11), indicating that NIV is increasingly used in the acute setting in Switzerland. Even though not entirely comparable with our study, Crimi et al. recently conducted an interesting survey in a cohort of selected pneumologists and intensive care physicians, aiming to identify the perceived pattern of NIV utilisation in Europe for different indications (17). This study showed that the NIV utilisation rate during AeCOPD, which is considered the most common indication, was considerably elevated (48%), corroborating our results for a constant increase of NIV utilisation during an acute respiratory condition such as the AeCOPD. In the Crimi et al. study, the utilisation rate was higher for pulmonologists than for intensive care physicians. However, it must be noted that the real expertise for mechanical ventilation practice in acute hospitals is quite different between European countries and Switzerland: the ICU, managed by intensivists, is the primary work facility for ventilation practices in our country, while in wards or in most semi-intensive respiratory units in European hospitals, pulmonologists are the primary suppliers of ventilation techniques. Another interesting finding is represented by the absence of a wide variation in the utilisation of NIV between university and non-university hospitals; this result demonstrates that, in the ICUs, the certified education in intensive care of the directors is quite homogeneous in our country and that the dissemination of similar practical skill principles during the dedicated curriculum in intensive care medicine is performed appropriately.
Compared to the German-speaking part of Switzerland, the French-speaking area has an increased penetration rate of NIV (fig. 2). An even higher rate is observed in the Italian-speaking part of Switzerland. This could be attributed to various reasons, including the presence of more experienced physicians in the French-and Italian-speaking areas, and an enduring French and Italian tradition in noninvasive ventilation [1–3]. Also, the satisfaction degree was higher in the French than in the German part of Switzerland. In detailing the lower degree of satisfaction, directors of ICUs at the institutions reporting low utilisation rates, identified a number of reasons explaining their perceived disappointment: the most important arguments were a lack of physician knowledge or inadequate staff training and, surprisingly, the need for better interfaces. We hypothesise that this last assertion was likely related to the lack of general experience with NIV during the different acute indications. In fact, the tolerance of patients to NIV, (and, therefore, its success) is directly associated to the mask comfort which, in turn, is linked to the amount of air leaks [18]. Oro-nasal masks, which seem to be much more efficient than the nasal masks in terms of leaks [19], were the most widely used interfaces in our survey; in these circumstances, a low degree of satisfaction (linked to the NIV failure) could be explained by other factors such as lack of dedicated NIV platforms with NIV modules or failure to recognise the presence of patient-ventilator asynchronies especially during the very first phases of NIV. As reported in the survey, all these reasons underscored the need for more education and practical training of all caregivers.
The directors were asked to provide data regarding the etiologies of respiratory failure primarily treated with NIV, after exclusion of potential candidates for invasive mechanical ventilation.In agreement with previously published work [20], the vast majority of applications were for patients with AeCOPD (acute hypercapnic respiratory failure) and ACPE. Other appropriate, but inhomogeneously distributed applications were pneumonia in the immunocompromised patient, post-extubation failure in high risk patients and weaning failure from invasive mechanical ventilation in COPD-patients [8, 6, 21]. An unpredictably high percentage of units considered a “do-not-intubate” (DNI) condition as a good indication for NIV. In patients with various end-stage lung diseases, in patients reluctant to accept invasive ventilation, in those with a DNI order or in very old patients considered poor candidates for intubation, NIV is now recognised as an emergent treatment of acute respiratory failure to treat the acute condition itself and to improve “the quality of dying” in selected patients [22–24]. This result highlights two important aspects: the first is that selected end-stage lung disease patients and “end of life” patients in our country are mainly supported with NIV in the ICU; the second is that contrary to other European countries [23], many Swiss acute hospitals don’t have intermediate or high dependency units where the use of NIV is a common practice.
During the AeCOPD, respiratory failure is approached with the bi-level mode in the great majority of all applications. Yet, we were surprised to realise that some centres still used a non evidence-based technique, i.e. CPAP, for this indication. According to our survey, we believe that this inappropriate application is linked to a lack of physician knowledge about NIV utilisation, suggesting that an appropriate use becomes unlikely unless physicians are aware of the scientific evidence. This observation is strengthened by the fact that CPAP which is in terms of effectiveness the standard of care or equivalent to positive pressure ventilation during the ACPE, was much less reported than expected. Even though bi-level ventilation may represent a wise methodology once ACPE is associated with a COPD or presents with a respiratory acidosis, different studies have demonstrated that either CPAP or bi-level ventilation, when associated with the conventional medical therapy, are similar in terms of reducing the need of intubation and of improving the outcome compared with the conventional oxygen therapy and medical care [25, 26].
A substantial number of primary applications of NIV were for patients with severe pneumonia but few were for ALI/ARDS-patients. NIV in patients with severe pneumonia still remains a controversial indication. The only study supporting NIV as a treatment modality in severe pneumonia was the study of Confalonieri et al. [27]. However, the post-hoc analysis of this study demonstrated that the overall success rate correlated with the presence of a subgroup of patients with a concomitant COPD. We cannot comment on the appropriateness of this indication in our survey, but, on the other hand, we know that in Switzerland few centres have collected a significant clinical experience in the NIV of patients with pneumonia [28, 29] and that staffing and experience may allow in these Institutions to consider non-invasive ventilation to be attempted even in controversial conditions.
This survey has limitations. The questionnaires were mainly based on perception of NIV use; only 7.5% of responses were the result of recorded data. Therefore, our results may rather underestimate actual practice variations. We only surveyed directors of ICUs, excluding other health care professionals. However, the ICU specialist is appropriate to provide competent information on the use of ventilation. Further, allowing only one respondent to participate could be also seen as an advantage, as repetitive answers from the same unit are avoided. Other limitations could include the lack of a process to validate the questionnaire and the retrospective nature of the survey. Major strengths of this survey include high response rates and a complete response to all the questions asked. Also, the survey is representative for all regions in Switzerland providing valuable information and characteristics of the different traditions in NIV practice.
In conclusion, this is the first survey that characterises Swiss physicians’ behaviour and perceptions towards NIV and demonstrates that the NIV practice is quite high in Switzerland, especially in the French and Italian parts of the country. NIV is used indiscriminately in university and non-university hospitals. The indications of the NIV use are in accordance with international guidelines, but a high percentage of units consider selected do-not-intubate conditions as a normal indication for NIV. The variability of NIV application among the different institutions and some erroneous applications suggest that more education and training of physicians, nurses and therapists are needed to improve the overall utilisation of NIV in acute care hospitals.
Acknowledgements:The authors thank all the Swiss ICU Directors who agreed to participate in this survey. Their commitment has been greatly appreciated.
References
1 Ambrosino N, Vagheggini G. Noninvasive positive pressure ventilation in the acute care setting: where are we? Eur Respir J. 2008;31:874–86.
2 Nava S, Hill N. Non-invasive ventilation in acute respiratory failure. Lancet. 2009;374:250–9.
3 Brochard L, Mancebo J, Wysocki M, Lofaso F, Conti G, Rauss A, et al. Noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease. N Engl J Med. 1995;333:817–22.
4 Plant PK, Owen JL, Elliott MW. One-year period prevalence study of respiratory acidosis in acute exacerbations of COPD: implications for the provision of non-invasive ventilation and oxygen administration. Thorax. 2000;55:550–4.
5 Masip J, Betbese A, Paez J, Vecilla F, Cañizares R, Padró J, et al. Non-invasive pressure support ventilation versus conventional oxygen therapy in acute cardiogenic pulmonary edema: a randomised trial. Lancet. 2000;356:2126–32.
6 Hilbert G, Gruson D, Vargas F, Valentino R, Gbikpi-Benissan G, Dupon M, et al. Noninvasive ventilation in immunosuppressed patients with pulmonary infiltrates, fever and acute respiratory failure. N Engl J Med. 2001;344:481–7.
7 Ferrer M, Sellarés J, Valencia M, Carrillo A, Gonzalez G, Badia JR, et al. Non-invasive ventilation after extubation in hypercapnic patients with chronic respiratory disorders: randomised controlled trial. Lancet. 2009;374:1082–8.
8 Nava S, Gregoretti C, Fanfulla F, Squadrone E, Grassi M, Carlucci A, et al. Noninvasive ventilation to prevent respiratory failure after extubation in high-risk patients. Crit Care Med. 2005;33:2465–70.
9 Nava S, Ambrosino N, Clini E, Prato M, Orlando G, Vitacca M, et al. Noninvasive mechanical ventilation in the weaning of patients with respiratory failure due to chronic obstructive pulmonary disease. A randomized, controlled trial. Ann Intern Med. 1998;128:721–8.
10 Trevisan CE, Vieira SR. Noninvasive mechanical ventilation may be useful in treating patients who fail weaning from invasive mechanical ventilation: a randomized clinical trial. Crit Care. 2008;12:R51. doi: 10.1186/cc6870
11 Maheshwari V, Paioli D, Rothaar R, Hill NS. Utilization of noninvasive ventilation in acute care hospitals: a regional survey. Chest. 2006;129:1226–33.
12 Carlucci A, Richard J, Wysocki M, Lepage E, Brochard L. Noninvasive versus conventional mechanical ventilation: an epidemiologic survey. Am J Respir Crit Care Med. 2001;163:874–80.
13 Doherty M, Greenstone M. Survey of non-invasive ventilation (NIPPV) in patients with acute exacerbations of chronic obstructive pulmonary disease (COPD) in the UK. Thorax. 1998;53:863–6.
14 Demoule A, Girou E, Richard JC, Taillé S, Brochard L. Increased use of non-invasive ventilation in French intensive care units. Intensive Care Med. 2006;32:1747–55.
15 Esteban A, Ferguson ND, Meade MO, Frutos-Vivar F, Apezteguia C, Brochard L, et al. Evolution of mechanical ventilation in response to clinical research. Am J Respir Crit Care Med. 2008;177:170–7.
16 Kumle B, Haisch G, Suttner SW, Piper SN, Maleck W, Boldt J. Current status of non-invasive ventilation in German ICUs: a postal survey. Anasthesiol Intensivmed Notfallmed Schmerzther. 2003;38:32–7.
17 Crimi C, Noto A, Princi P, Esquinas A, Nava S. A European survey of noninvasive ventilation practices. Eur Respir J. 2010;36:362–9.
18 Prinianakis G, Delmastro M, Carlucci A, Ceriana P, Nava S. Effect of varying the pressurisation rate during noninvasive pressure support ventilation. Eur Respir J. 2004;23:314–20.
19 Girault C, Briel A, Benichou J, Hellot M, Dachraoui F, Tamion F, et al. Interface strategy during noninvasive positive pressure ventilation for hypercapnic acute respiratory failure. Crit Care Med. 2009;37:124–31.
20 Nava S, Hill N. Non-invasive ventilation in acute respiratory failure. Lancet. 2009;374:250–9.
21 Ferrer M, Sellares J, Valencia M, Carrillo A, Gonzalez G, Badia JR, et al. Non-invasive ventilation after extubation in hypercapnic patients with chronic respiratory disorders: a randomised controlled trial. Lancet. 2009;374:1082–8.
22 Nava S, Sturani C, Hartl S, Magni G, Ciontu M, Corrado A, et al. End-of-life decision-making in respiratory intermediate care units: a European survey. Eur Respir J. 2007;30:156–64.
23 Curtis JR, Cook DJ, Sinuff T, White D, Hill N, Keenan S, et al. Noninvasive positive pressure ventilation in critical and palliative care settings: understanding the goals of therapy. Crit Care Med. 2007;35:932–9.
24 Nava S, Grassi M, Fanfulla F, Domenighetti G, Carlucci A, Perren A, et al. Non-invasive ventilation in elderly patients with acute hypercapnic respiratory failure: a randomised controlled trial. Age Ageing. 2011;40:444–50.
25 Park M, Sangean MC, Volpe Mde S, Feltrim MI, Nozawa E, Leite PF, et al. Randomized, prospective trial of oxygen, continuous positive airway pressure and bilevel positive airway pressure by face mask in acute cardiogenic pulmonary edema. Crit Care Med. 2004;32:2407–15.
26 Bellone A, Vettorello M, Monari A, Cortellaro F, Coen D. Noninvasive pressure support ventilation vs continuous positive airway pressure in acute hypercapnic pulmonary edema. Intensive Care Med. 2005;31:807–11.
27 Confalonieri M, Potena A, Carbone G, Porta R, Tolley E, Meduri U. Acute respiratory failure in patients with severe community-acquired pneumonia. A prospective randomized evaluation of noninvasive ventilation. Am J Respir Crit Care Med. 1999;160:1585–91.
28 Jolliet P, Abajo B, Pasquina P, Chevrolet JC. Noninvasive pressure support ventilation in severe community-acquired pneumonia. Intensive Care Med. 2001;27:812–21.
29 Domenighetti G, Gayer R, Gentilini R. Noninvasive pressure support ventilation in non-COPD patients with acute cardiogenic pulmonary edema and severe community-acquired pneumonia: acute effects and outcome. Intensive Care Med. 2002;28:1226–32.