Figure 1
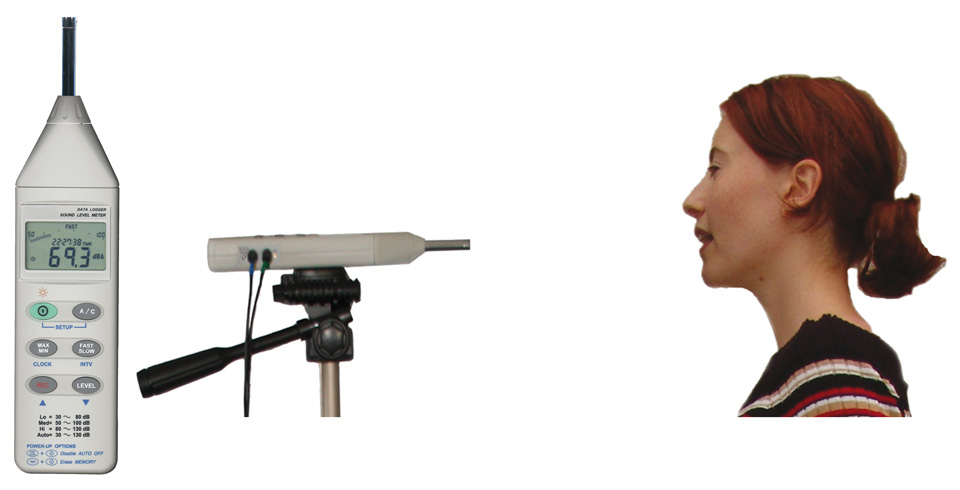
Equipment set-up for data collection: Sound level meter; standardised record. (Reprinted with permission from WEVOSYS.)
DOI: https://doi.org/10.4414/smw.2012.13534
The human voice is a (non-linguistic) component of body language [1–2] and the volume of one's vocalisation has been identified as a key factor of body expression. Furthermore, the voice appears to be an essential tool in many social contexts, such as the doctor-patient relation [3–4]. Based on a speaker's voice, diverse socially relevant information such as interpersonal distance, emotional state, vocal pleasantness, conviction, attractiveness or authority may be transferred during different routine verbal clinical activities (e.g., in taking a history, reporting a diagnosis, ordering further diagnostic examinations, medical visits, patient care). A proper use of voice has been regarded as crucial for the doctor-patient communication, well-being and patient satisfaction [5–7]. Even an influence of the physician's nonverbal behaviour on health outcomes is reported [8].
Serber [9] detected the acoustic-perceptual voice feature 'speech loudness' (also named 'vocal loudness' or 'loudness of phonation') as one of six variables involved in interactive behaviour. It is defined as "the sound level produced by the voice and perceived by the listener" [10; p. 30]. A subject's default sound level, used for the majority of her or his vocalisations is called 'habitual loudness' – "the perceptual correlate to the most frequently produced vocal intensity" [11; p. 176]. Listeners usually prefer a medium loudness [12]. Experts in acoustics and phoniatrics are typically concerned with the reduction of habitual loudness as a sign of a voice and/or speech disorder [11]. Seen from a perspective of social psychology, a low voice volume may suggest insecurity, submissive behaviour or vulnerability whereas a loud voice may be a sign of strength, assertive behaviour [13–14] or social dominance. In an older telephone study, the patient's perception of the doctor's dominance was positively correlated with increased amplitude and rate of speech [15]. While a louder voice belongs to the gender role of the male physician [6], female physicians with a louder voice are perceived as particularly dominant [16], because they tend to have a more emotional and less dominant communication style [17].
It is, however, unknown whether the period of medical education has an impact on a possible change of voice loudness. No previous study investigated the effect of curricular education on loudness or other voice parameters in medical students. Further, the evidence base to support larger investigations such as cohort studies is slim because as yet there are no observational data underlining an association between medical socialisation and voice loudness. Therefore, we wanted to test the hypothesis that medical students talk louder than their non-medical peers and, if so, to find out whether they commence their studies with a loud voice, representing a characteristic of admission, or whether sound pressure level changes during education, reflecting model learning.
In this quasi-longitudinal experimental study, we compared the voice loudness of medical and non-medical students at 2 points of time. The study was approved by the local Ethics Committee.
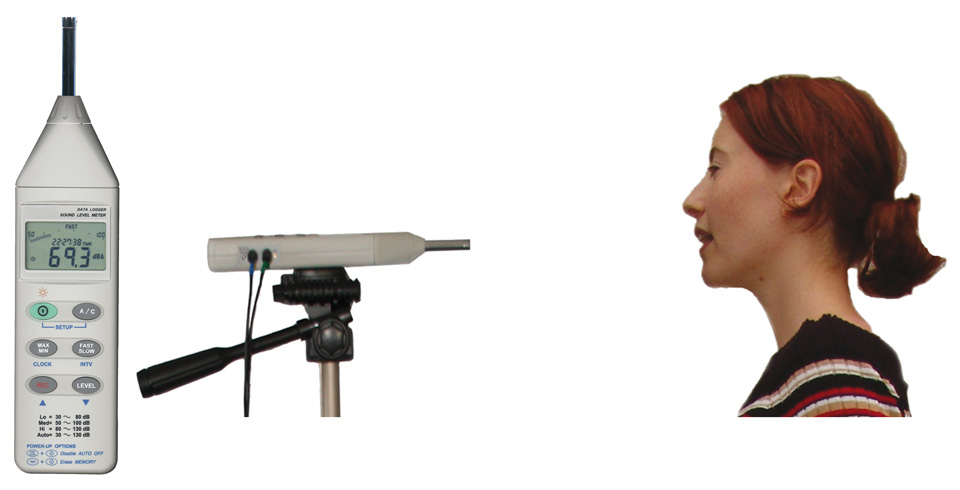
Figure 1
Equipment set-up for data collection: Sound level meter; standardised record. (Reprinted with permission from WEVOSYS.)
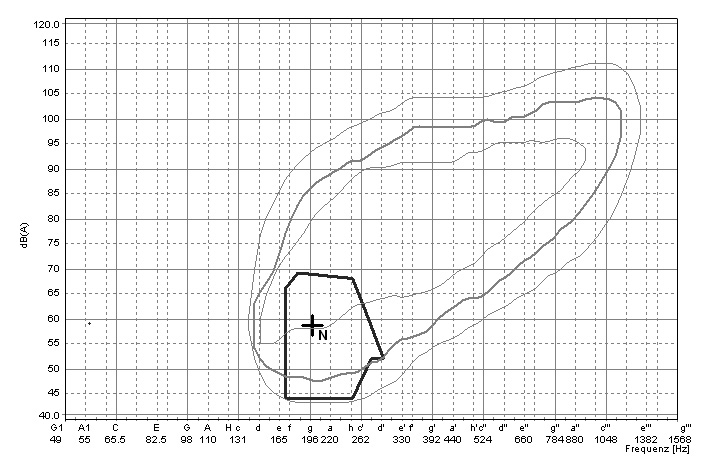
Figure 2
Voice range profile (example). The cross symbolises the averaged dB value for 1 of the 2 tasks. (Reprinted with permission from WEVOSYS.)
We randomly recruited freshmen and fifth-year students from Göttingen Medical School (= medicine), and a broad mix of other faculties of the university (= non-medicine). We recruited the latter students especially at the schools for law, business, biology, chemistry and social sciences and addressed them as well as the medical students in lecture halls and the cafeteria. A total of 206 students (117 females) between 18 and 32 years of age gave written informed consent to participate in the study. They were only informed that we recorded their voice as part of a comparative voice study. We strictly avoided any information about the loudness parameter of the study.
The participants had no voice disorders, respiratory problems and no formal training in singing or speaking. All demonstrated normal hearing (auditory impression) and, at the time of the interview, all were healthy and free from colds, laryngitis and hoarseness. The age-sex mix in the 4 groups of students was comparable (table 1). The slight over-representation of women is in accordance with the higher percentage of female students at Göttingen University Medical School (57.4%; 2009; http://www.uni-goettingen.de/de/24666.html). The percentage of women in the other faculties where students were recruited ranged between 34% and 67%. For a comparable gender mix, we tried to address especially female students at the non-medical faculties during the last period of recruitment.
The target outcome of the study was the student's habitual loudness. Since common microphones have technical limitations for sound pressure measurements [18], we used the standardised lingWAVES sound level meter for measurement of the frequency-weighted sound pressure level, displayed in dB (A) [19]. Measurement took place in a silent room in a quiet environment. As recommended from the producer, the sound level meter was kept at a distance of approximately 30 cm (12 inches) from the speaker's mouth during the recording (fig. 1). The distance was controlled by a special mark on the floor for the position of the speaker's chair, the students were asked to sit as calmly as possible.
The accuracy of measurement with the sound level meter is reported as ± 1.5 dB (Ingolf Franke, personal communication). Due to external changes (e.g., weather; time of day) or internal processes (e.g., health status) as well as due to unknown effects of familiarity, a valid assessment of retest-reliability in voice measurement is difficult to realise. Or in other words: a difference in sound pressure level values between two measurements of the same person is not necessary a sign of low reliability. However, since we were interested in a sort of internal quality control of our own measurements, we tried to arrange a retest with at least a small sample of students that was invited to a second measurement about 4 weeks later.
Present in the room were the student and the examiner. To avoid an effect of the task on the sound pressure level, all subjects had to produce two different tasks: (1) reading aloud a short story consisting of 113 words composed of a title and 6 sentences, a standard text in German in order to measure voice parameters ("Der Nordwind und die Sonne" = "The Borealis and The Sun" [Aesop]); (2) spontaneous speech, elicited through 2 interview questions about the experience of students in Göttingen. Data collection took approximately 5 minutes per student. The average loudness of a speaker for one task, expressed in dB values, is represented by a cross in the display (fig. 2). Habitual loudness was calculated, as recommended by Zraick et al. [11], as the averaged dB value elicited by the 2 tasks.
| Table 1: Sample characteristics. | ||||
| Medical students | Non-medical students | |||
| Characteristics | Freshmen | Fifth-year students | Freshmen | Fifth-year students |
| Sample; n (%)* | 51 (49) | 53 (51) | 50 (49) | 52 (51) |
| Females; n (%)** | 28 (55) | 29 (55) | 29 (58) | 31 (60) |
| Age; m (SD) | 20.9 (2.0) | 25.6 (1.8) | 20.4 (1.4) | 25.7 (1.7) |
| * The percentages refer to the distribution between freshmen and fifth-year students ** The percentages refer to the share of females in the sample | ||||
We calculated the mean sound pressure level values (and their standard deviation [SD]) for the 4 groups of students under study. We also compared the values of female and male students. Differences between freshmen and fifth-year medical students were first investigated by a t-test for two independent samples, including the 95%-confidence interval (CI) for the mean difference. The main hypothesis was tested in a 2-way analysis of variance, with year of study (first vs. fifth year) and field of study (medicine vs. non-medicine) as main factors. Since it was an unbalanced design, we used the type III sum of squares to determine F and its respective p-value [20]. Prior to this analysis, the distribution of the dependent variable in all 4 groups was checked for normality, using the Shapiro-Wilk test with a cut-off of p = 0.05.
Retest-reliabilty was determined by Pearson's coefficient of correlation between first and second measurement. Additionally, the signed-rank test for dependent samples was used to test whether the differences between first and second measurement were different from zero.
All analyses were performed using the statistical software SAS, version 9.2.
For 5 of the 206 students, we obtained a second loudness reading. Only one student's measurement differed widely from the first measurement (4.15 dB) First and second reading of the 5 students correlated at 0.79 (Pearson's R). The averaged difference between both measurements (1.34) did not significantly differ from zero (p = 0.3125).
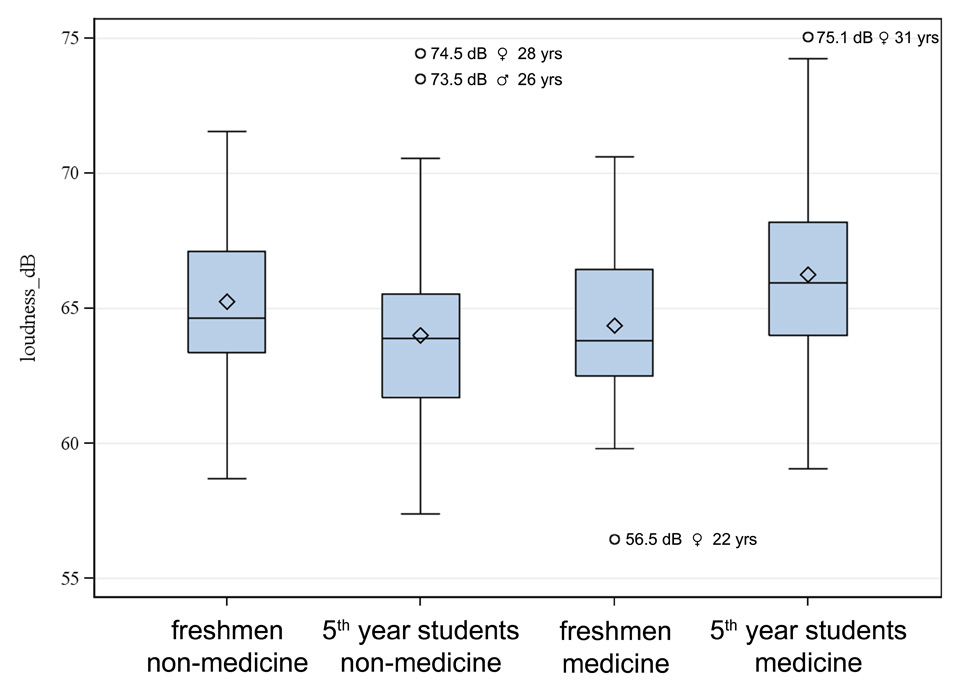
Figure 3
Habitual loudness of freshmen and fifth-year students.
The mean sound pressure level of freshmen in medicine was, on average, 64.4 dB (SD 3.0), that of fifth-year medical students, 66.3 dB (3.7). The respective scores of non-medical students were 65.2 (SD 2.7) for freshmen and 64.0 (3.4) for fifth-year students. When considered separately, men and women displayed the same tendency: The mean scores of first semester women in medicine were 64.2 (SD 3.1) and 65.9 (3.7) for fifth-year women in medicine, that of men 64.5 (SD 2.9) and 66.7 (3.7), respectively. The respective scores in non-medicine students were 65.3 (SD 2.2) and 64.2 (3.2) for women and 65.2 (3.3) and 63.7 (3.8) for men.
We first performed a t-test for the difference in sound pressure level between medical freshmen and fifth-year medical students. The difference was significant (difference between the 2 points in time: 1.906; 95%-CI: 0.605 to 3.206; p = 0.0045).
The box plots in figure 3 show the distribution of the values in the 4 groups. In 1 subgroup (non-medical students, fifth year), the hypothesis of a normal distribution was rejected (p = 0.026; Shapiro-Wilk test), probably because of several outliers. Two of the outliers (see fig. 3) were somewhat older (28 and 31 yrs) than the average fifth-year student (26.5 yrs). We log-transformed the values of the students' sound pressure level in all 4 groups.
On basis of the log-transformed values, we then performed a 2-way analysis of variance with "field of study", "years of study" and "gender" as main factors and the students' sound pressure level as dependent variable. All three factors were non-significant individually (F values for "field of study" = 2.46, for "years of study" = 0.46, for "gender" = 0.18) but the interaction (field of study x years of study) proved to be highly significant (F = 12.7; p = 0.0005). We repeated this analysis but deleted the 4 outliers that can be seen in figure 3. The F-value for the interaction of "field of study" and "years of study" even increased (15.0; p <0.0001) and the factor "field of study" became significant with a rather low F-value of 4.3 (p = 0.039).
This paper presents some evidence that medical students, in contrast to their non-medical peers, learn to raise vocal loudness during their education in medical school. Prima facie, the higher mean dB values in fifth-year medical students might appear in line with vocal sound pressure levels of the normal population. For example, in their study of 100 healthy persons between the age of 19 to 32 years, Pérez Álvarez and Hacki [21] found, for the average intensity, sound pressure levels of 66.1 dB (SD 3.6) for men and 65.1 dB (SD 3.6) for women. However, it should be considered that dB values refer to a logarithmic scale so that an increase of 1 dB is already audible; to produce an increase of 3 dB demands a doubling of a speaker's sound power. The increase in loudness in our study of nearly 2 dB therefore seems remarkable and can be interpreted (1) by theories of social learning, (2) as a means of status cueing or (3) a gain in self-confidence.
(1) It is to be assumed that tendencies to produce higher sound pressure levels during medical education are conditioned by social learning or – as Hafferty [22] puts it – by the hidden and powerful curriculum of medical schools. That is to say that most values, attitudes, beliefs and related behaviours, deemed important within medicine, are taught and internalised in a latent curriculum, often antithetical to the goals and content of official medical courses [23]. Since students often learn the values and ideology of the profession by observing those in the position to which they aspire [24], their vocal behaviour is therefore likely to be acquired by the observation of, and in informal interactions with, teachers, consultants and senior residents in medical schools.
(2) Loudness is not irrelevant to socio-cultural status cueing. Perhaps medical students, after successfully completing their studies, know they will belong to a high-status group and, therefore, adopt features like vocal loudness to compliment a social identity, positively valued by that social group and the population at large. High loudness levels may play a role in the cueing of authority, competence or social dominance orientation. A loud voice is a means of dominating conversation and demonstrates (vocal) power. Peng et al. [25] found that vocal loudness universally conveyed power in American and Korean male speakers. This may also explain why our medical male students in the fifth year spoke the loudest.
(3) A louder voice may reflect a gain in self-confidence. Older medical students learn, perhaps more intensively and more systematically than their non-medical peers, to present themselves in seminars or during bedside-teaching as competent partners and may tend to express this competency via a louder voice that helps to control the audience and the environment conditions (Edelbert Schaffert, personal communication).
We should emphasise that these results may be differently interpreted from experts in acoustics and phoniatrics. They would probably take into account factors such as speech intensity, vocal fundamental frequency air flow, and air pressure.
There is a wealth of studies on patient-centred vs. doctor-centred behaviours, typically assessed by the use or non-use of specific interview techniques such as closed questions, active or passive interview style, emotional reassurance or information giving besides others [3; 26]. Voice parameters such as habitual loudness usually play no role in such studies. And if the voice is considered important for the doctor-patient relation there is a sort of naivety as can be exemplarily seen in a Canadian article on the power of a dentist's voice. The author recommends a strong, confident voice for effective interpersonal communication to project an image of confidence and professionalism [27]. In some contrast to such recommendations, patients seem to prefer a warm and slow voice and to dislike a loud and aggressive voice; at least patients treated by psychotherapists [28]. According to the results of our study, a 'strong' voice seems to be the result of a socialisation process where to gain professional dominance is, still nowadays, often more important than to empathise with the patient [24]. A louder voice may be an important, powerful – and largely unconscious – component of the medical profession or, to speak with Pierre Bourdieu, may be part of the embodied nature of the medical habitus [29; p 59].
The study has some limitations. First, cross-sectional data at a single point in development may be misleading. Although the interaction of years of study and field of study was statistically strong and the increase of medical students' loudness seems plausible, other factors than those investigated may be the actual – or a likewise important – cause of this development. Second, the present study took only notice of one acoustic parameter of the voice: the habitual loudness in speaking. Other features, such as pitch or frequency spectrum, may give additional insight into the voice development of students. Third, a 'loud voice' is a complex construct, not only 'produced' by a speaker but also 'perceived' by a listener. For a pilot study, however, the sound pressure level may be an adequate indicator of whether or not the students' vocal loudness increased during their education.
While the sound pressure meter seems reliable, our test of retest-reliability was only performed with a very small sample of students that may not be considered a valid assessment. It only ensured some minimum standard of quality control.
After the second year of medical education all students have to undergo a communication course with simulated patients in Göttingen. In brief, this programme aims at the improvement of communication skills considering verbal as well as non-verbal aspects of communication. Use and modulation of voice are also part of the structured feedback, students receive after the training. All medical students of the fifth year who participated in our study have passed this training 2.5 years ago. Should have this communication training influenced the results of our study, it should be considered that the voice differences between first year and fifth year students might be even more significant without the communication training mentioned above.
An increased habitual loudness at the end of medical studies may be an important carrier signal to understand how this profession gains dominance. Furthermore, it could represent one quality the possession of which is necessary for those persons beginning their career as a medical professional. If further research, using a longitudinal design and also eliciting the perceived loudness confirm our results, habitual loudness as one prerequisite to a medical career, should receive more attention.
Studies about communication behaviour in medical consultations could also benefit from a more systematic consideration of the voice as an effective tool to configurate the relation to the patient as Haskard and collegues [5] showed in their studies on the effects of a provider's voice tone on patient satisfaction and treatment adherence.
According to Buddeberg-Fischer and Stamm [30] who recommend changes in postgraduate training in order to address the medical profession's changing profile, further studies could investigate whether the medical students' habitual loudness decreases, or even increases, during the postgraduate training period.
While medical sociologists are especially concerned with processes of power and subsequent risks for the patient, we should also consider a risk for those who acquire a louder voice: hoarseness and an (occupational) dysphonia by stressing the voice through a high loudness phonation. This may be a risk not only for medical students but also for physicians, if they are additionally engaged in medical teaching.
Acknowledgements:The authors would like to thank Carmen Illgner and Lisa Manhart for their help with data collection. Ryan David Mullins gave valuable comments on former drafts of the paper. Norbert Scheer, M.Sc., established the sound measurement procedure, ensured the quality of the measurement process and helped with the graphic display of the results.
1 Scherer KR. On the symbolic functions of vocal affect expression. J Lang Soc Psychol. 1988;7(2):79–100.
2 Scherer KR. Expression of emotion in voice and music. J Voice. 1995;9(3):235–48.
3 Street RL Jr, Gordon H, Haidet P. Physicians' communication and perceptions of patients: It is how they look, how they talk, or is it just the doctor? Soc Sci Med. 2007;65(3):586–98.
4 Teutsch C. Patient-doctor communication. Med Clin North Am. 2007;87(5):1115–45.
5 Haskard KB, Wiliams SL, DiMatteo R, Heritage J, Rosenthal R. The provider's voice: patient satisfaction and the content-filtered speech of nurses and physicians in primary medical care. J Nonverbal Behav. 2008;32(1):1–20.
6 Mast MS, Hall JA, Köckner C, Choi E. Physician gender affects how physician nonverbal behaviour is related to patient satisfaction. Med Care. 2008;46(12):1212–8.
7 Ong LML, De Haes JCJM, Hoos AM, Lammes, FB. Doctor-patient communication: A review of the literature. Soc Sci Med. 1995;40(7):903–18.
8 Schmid Mast, M. On the importance of nonverbal communication in the physician-patient interaction. Patient Educ Couns. 2007;67(3):315–8.
9 Serber, M. Teaching the nonverbal components of assertive training. J Behav Ther Exp Psychiat. 1972;3(3):179–83.
10 Case J. Clinical management of voice disorders. 4th ed. Austin, TX: Pro-Ed; 2002.
11 Zraick RI. Marshall W. Smith-Olinde L. Montague JC. The effect of task on determination of habitual loudness. J Voice. 2004;18(2):176–82.
12 Hollien H, Gelfer MP, Carlson T. Listening preferences for voice types as a function of age. J Commun Disord. 1991;24(2):157–71.
13 Eisler RM, Miller PM, Hersen M. Components of assertive behavior. J Clin Psychol. 1973;29(3):295–9.
14 Rose YJ, Tryon WW. Judgements of assertive behaviour as a function of speech loudness, latency, content, gestures, inflection, and sex. Behav Modif. 1979;3(1):112–23.
15 Harrigan JA, Gramata JF, Lucic KS, Margolis C. It's how you say it: physicians' vocal behavior. Soc Sci Med. 1989;28(1):87–92.
16 Schmid Mast M, Hall, JA, Cronauer, CK, Cousin G. Perceived dominance in physicians: Are female physicians under scrutiny? Patient Educ Couns. 2011;83(2):174–9.
17 Cronauer CK, Schmid Mast, M. Gender-specific aspects of the physician-patient interaction. Rehabilitation (Stuttg). 2010;49(5):308–14.
18 Svec JG, Granqvist S. Guidelines for selecting microphones for human voice production research. Am J Speech Lang Pathol. 2010;19(4):356–68.
19 LingWAVES, Voice Diagnostic Center. [http://www.wevosys.com/products/lingwaves/lingwaves_voice_diagnostic_center.html] (last accessed 2011/06/01).
20 Walker GA. Common statistical methods for clinical research. 2nd ed. Cary, NC: SAS Institute, 2002.
21 Pérez Álvarez JC, Hacki T. Norm-Stimmparameter beim Standardlesetext [Norms for the voice parameters when reading a standard text]. In Aktuelle phoniatrisch-pädaudiologische Aspekte 1999/2000, vol. 7 [Current phoniatric-pedaudiologcal aspects]. Ed. Gross M. Heidelberg: Median; 2000;78–81.
22 Hafferty FW. The hidden curriculum, ethics, teaching and the structure of medical education. Acad Med. 1994;69(11):861–71.
23 Hafferty FW. Beyond curriculum reform: confronting medicine's hidden curriculum. Acad Med. 1998;73(4):403–7.
24 White CB, Kumagai AK, Ross PT, Fantone JC. A qualitative exploration of how the conflict between the formal and informal curriculum influences student values and behaviors. Acad Med. 2009;84(5):597–603.
25 Peng Y, Zebrowitz LA, Lee HK. The impact of cultural background and cross-cultural experience on impressions of American and Korean male speakers. J Cross Cult Psychol.1993;24(2):203–20.
26 Del Piccolo L, Mazzi M, Saltini A, Zimmermann C. Inter and intra individual variations in physicians' verbal behaviour during primary care consultations. Soc Sci Med. 2002;55(10):1871–85.
27 McCoy LA. The power of your vocal image. J Can Dent Assoc. 1996;62(3):231–4.
28 Bauer S, Tomicic A, Martinez C, Reinoso A, Schäfer A, Peukert A, Frangkouli A. The significance of the voice and voice tone during psychotherapy seen from the patient perspective (in German). Psychoanal Körper. 2010;9(2):27–50.
29 Brosnan C. Pierre Bourdieu and the theory of medical education. Thinking 'relationally' about medical students and medical curricula. In: Handbook of the Sociology of Medical Education. Eds. Brosnan C, Turner BS. NY: Routledge; 2009;51–68.
30 Buddeberg-Fischer B, Stamm M. The medical profession and young physicians' lifestyles in flux: challenges for specialty training and health care delivery systems. Swiss Med Wkly. 2010;140:w13134.
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article was reported.