
Figure 1
Simplified model of the relationships of stressors, resources and consequences for employees and for the hospital.
DOI: https://doi.org/10.4414/smw.2012.13532
At present, the demands on and challenges to the quality of health care are growing. This affects not only the purely medical or scientific elements of quality, but also the level of care that is provided to patients [1]. Accordingly, from the patient perspective, the quality of care is coming increasingly under scrutiny. For instance, a recent study by Comparis [2] provides an analysis of various aspects of patient satisfaction in Swiss hospitals. The results show that there are considerable differences in the evaluation of hospitals in Switzerland. Given a background of increasing competition, differences in perceived patient satisfaction in hospitals will gain significance over time. Simultaneously, in the health care system, the pressure to reduce costs is growing. As in other countries, system reform is the subject of constant debate and controversy in the media and political circles.

Figure 1
Simplified model of the relationships of stressors, resources and consequences for employees and for the hospital.
Cost savings have some awkward implications for the work situation and thus for the health of employees and quality of care provided. Studies indicate that a high level of stress jeopardises the health of employees as well as work efficiency [3–4].
The relationship between working conditions and employee health is generally evaluated on the basis of stress and action theory [5, 6]. According to these approaches, stressors jeopardise employee health (see fig. 1) [7, 8]. Such stressors include regulation hindrances and hindrances caused by capacity-overtaxing. Regulation hindrances constrain the achievement of work objectives. One example is that of informational impediments, such as a lack of information (e.g. data in the patient records) that is necessary for the effective performance of work. Another example of regulation hindrances are constant interruptions while employees work on complex tasks (e.g. while they are writing discharge letters, physicians are interrupted with questions concerning the treatment of patients). Hindrances through capacity overtaxing include time pressure over an extended period of time.
Health-related problems can occur at the physiological, psychological or social levels [9] and exert an impact over the short, medium or longer term [10]. Examples of such health problems are psychosomatic disorders, irritability or chronic illness. Moreover, stressors at work have negative consequences for the organisation. Thus, regulation hindrances reduce work efficiency, because they require constant additional effort (which could in fact be avoided), such as having to obtain missing information or again focusing one's attention on the work after an interruption [8]. Frequent time pressure overloads employees and impacts also on both health and efficiency [4].
On the other hand, resources at work yield positive relationships with employee health. Moreover, the appropriate provision of resources seems to assist in overcoming stress factors. Control and social support are important work-related resources [6].
The postulated relationships between stressors, resources and health have been demonstrated in numerous studies in different branches including the health services [4, 9, 11]. Longitudinal studies [e.g. 8] have shown that stressors do really cause health problems.
Especially for employees in interactive service work, such as the provision of health services, health problems in the form of burnout can develop and lead to an aversion to patients [12]. Research shows that burnout is triggered very substantially by stressors such as constant time pressure [3, 4]. A study of hospitals in the USA reveals that each additional patient per hospital nurse increases the likelihood of burnout by 23% [13]. In order to study effects of rationing of care in greater detail, an instrument for measuring the implicit rationing of care was developed (the Basel Extent of Rationing of Nursing Care, BERNCA). A study in Switzerland, based on this instrument, showed that burnout is clearly associated with the implicit rationing of care [RICH-Nursing Study, 14]. Furthermore, current studies demonstrate that characteristics of interactions between employees and patients, such as dealing with those with particularly high expectations [15], with difficult personalities [16], as well as aggressive patients [11], are associated with burnout. Simultaneously, in a hospital setting, aspects of employee burnout are negatively correlated with the completeness of the health service itself and the quality of life of patients [17] as well as their satisfaction [18].
The organisational framework and associated conditions also constitute a fundamental basis of service quality perceived by patients or customers [19]. Evidence of such effects can be found in the research on service climate, which can be defined as "the employee perceptions of the practices, procedures, and kinds of behaviours that get rewarded and supported in a particular setting" [20, p.151]. Empirically, service climate was investigated in different areas. A study of employees in the hotel and hospitality sector revealed that the relationship between organisational resources (such as support from superiors or the quality of available internal services), employee performance and customer loyalty was mediated through employee commitment and the service climate [21]. Thus, customer-oriented work is not determined solely by the personal competence and attitudes of employees, but also by the conditions prevailing in the organisation.
Similar results are found in the hospital. A review of international data provides evidence that low nurse staffing and low skill mix levels, as well as negative characteristics of the nursing work environment are related to patient outcomes (e.g., higher complications and mortality rates) [22]. The RICH-Nursing study also revealed that several outcomes (nosocomial infections, pressure ulcers and patient satisfaction) were especially sensitive to rationing [23].
While these studies focus on the organisation as a whole, aspects of working conditions at the individual work places might also be relevant for the quality of care provided at the hospital. Research on employee working conditions (stressors and resources at individual workplaces) has so far concentrated on the relationship to employee health. A study on 351 physicians' assistants in 106 medical practices, by contrast, had the objective of investigating the relationship of working conditions in the interaction with customers (particularly of resources) with the service orientation [24]. The results indicate that patient-oriented control explains additional variance in the service climate1 and in the personal service orientation beyond the more familiar organisational resources. It is assumed that the importance of patient-oriented control lies mainly in its enabling employees to react flexibly, particularly when unanticipated customer needs arise.
1 The authors of this study use the term "organisational service orientation" instead of "service climate" and the study is based on individual data instead of aggregated data.
The related findings show that stressors and resources of employees in different occupational fields are associated with the health of employees. Moreover, for physicians' assistants, it was shown that resources in the interaction with patients (patient-oriented control) are associated with the personal service orientation of employees.
Based on these findings, the present study was intended to evaluate the role of working conditions in the interaction with patients, for employees of different occupational groups in a hospital. The aim of the study was to investigate stressors and resources which are present in the interactions of employees with patients at an orthopaedic clinic of a Swiss cantonal hospital and to analyse their relationship to the health of employees and their patient orientation. The following hypotheses formed the basis of the study:
1. Stressors in the interaction with patients are positively associated with physical complaints, emotional exhaustion and an aversion to patients on the part of employees.
2. Stressors in the interaction with patients are negatively associated with an employee's patient orientation.
3. Patient-oriented control is positively associated with an employee's patient orientation.
The study was conducted by the University of Applied Sciences Northwestern Switzerland at the Orthopaedic Clinic of the Cantonal Hospital of Olten. The main objective of the Orthopaedic Clinic was to analyse working conditions and the health of employees at the clinic and to develop measures for work redesign, based on this analysis. The background was the generally difficult situation at the clinic. The number of operations that had been conducted over the past few years had increased markedly and with a simultaneous reduction in the average length of patient stays in the hospital. However, there was no funding for a corresponding increase in personnel. The aim of the study was therefore to find ways to use the available resources optimally and to reduce additional effort resulting from regulation hindrances.
The study was cross-sectional and the written survey took place between the end of March and the beginning of April 2008 at a cantonal hospital. The hospital has 240 beds and includes the extended basic care of an area of about 100,000 people. Almost 1,000 employees work at the hospital.
The study included the physicians, nurses and the secretarial staff of the orthopaedic clinic. In addition, the sample included the interfaces between the clinic and the broader hospital organisation. These interface areas entailed OP nurses, physiotherapy, ergotherapy, anaesthesia and other organisational units.
| Table 1: Overview of use of available and newly developed scales. | |||
| Scale | Source | Items | Cronbach's α |
| Impediments in the interaction with patients | New | 4 | 0.77 |
| Barriers to patient-oriented work | New | 5 | 0.77 |
| Patient-oriented control | Adapted version of scale of customer-oriented latitude [24] | 5 | 0.82 |
| Physical complaints | Scale from iafob [4] | 11 | 0.82 |
| Emotional exhaustion | BHD [12] | 12 | 0.87 |
| Aversion to patients | BHD [12] | 5 | 0.90 |
| Patient orientation | Adapted version of a scale of personal service orientation [24] | 2 | 0.87 |
| Quantitative Overload | Short version of scale from SALSA [27] | 3 | 0.78 |
| Presenteeism | Items from iafob [4] | 1 | - |
| Intention to leave the hospital | Items from iafob [4] | 1 | - |
The variables include stressors and resources in the interaction with patients, aspects of employee health and the employees' patient orientation (see table 1).
Two forms of stressors in the interaction with patients were assessed, namely impediments in the interaction with patients and barriers to patient-oriented work. In order to capture these stressors, two new scales were developed. These refer to psychological action regulation theory and to the results of a qualitative study on characteristic stressors at work among nurses [25 and 26]. A first version of the scales with nine items (barriers to patient-oriented work) and six items (impediments in the interaction with patients) was generated. It was pre-tested for appropriateness and comprehensibility in interviews with two nurses who worked in Swiss hospitals. As a result, adapted versions of the scales with five items (barriers to patient-oriented work) and four items (impediments in the interaction with patients) were compiled. Scale characteristics were tested in the study presented here (see below).
Impediments in the interaction with patientsrefer to the concept of regulation hindrances [8]. They are defined as stressors that result from additional effort, when employees have to look after patients whose cooperation is constrained or problematic. This may be the case when patients have difficulty understanding information about their illness, as is common with older patients or those whose knowledge of German is poor. The same applies to those with little motivation to do anything themselves to improve their condition. Impediments in the interaction with patients are considered as stressors because there is usually no compensation for the additional effort that is necessary to cope with such events. An example of a question for determining impediments in the interaction with patients is: "In this department, one has to work with patients who have difficulties understanding information about their illness."
Barriers to patient-oriented work may be assigned to the concept of regulation hindrances [8]. They are defined as organisational barriers that occur in interactions with patients. This is the case, for example, if the information needed to advise patients is not available, or if there are constant interruptions during important discussions with patients. Because of its assumed effect on employee attitudes towards work, we refer to such stressors as barriers to patient-oriented work. An example of a question for determining barriers to patient-oriented work is: "How often are you interrupted during important conversations with patients?"
Patient-oriented control was measured by means of an adapted version of a scale originally designed to measure customer-oriented control [24]. Patient-oriented control is defined as the leeway that employees have to make in their own decisions in order to act in a patient-oriented manner.
Physical complaints cover various different health complaints, such as headaches, sleep disorders, back pain or vertigo. They were assessed using an 11 item scale from iafob [4].
Two aspects of burnout were assessed (emotional exhaustion and aversion to patients), based on the BHD (Screening the Demands of Humanitarian Services [12]). Emotional exhaustion is defined as the feeling of being emotionally overextended. Aversion to patients is defined as a possible extreme consequence of emotional exhaustion and inequality in social exchange between employee and patient.
The patient orientation was determined from an adapted version of a scale for a personal service orientation [24]. Patient orientation is defined as the employee's wish to respond individually to patient preferences or needs.
The BHD [12], as well as the scale for patient orientation, have seven-point scales. All other instruments have five-point scales.
Quantitative overload was introduced in the analysis as a possible confounder. Quantitative overload means that the work load is too high. It is measured from the SALSA-Instrument [27].
For a further analysis, "presenteeism" (a decrease in productivity caused by employees who are present at the workplace, although they are suffering from health problems), and the employee's intention to leave the hospital were evaluated with items from iafob [4].
The questionnaire for the clinic personnel was both web-based and made available in a paper version, as not all the relevant employees had access to a computer. On average, it took 25 minutes to complete the questionnaire.
In order to validate the quantitative analyses a supplementary qualitative analysis was conducted. A total of six workplace analyses of different professional groups and hierarchy levels were conducted on the basis of observational interviews, with the aid of the procedure of contrastive task analysis [28]. These yielded a series of specific examples of the stressors and resources which were analysed in the questionnaire-based study.
The study is based on a questionnaire survey that measures employee perceptions of their working conditions and their health, as well as their attitudes to the patient orientation. Bias in the evaluation of employees cannot thus be excluded. For example, an overestimation of the relationships between stressors and health problems may occur. Respondents who are basically optimistic and satisfied could underestimate both the burdens and their impact on health. Those who see the world somewhat more negatively may thus overestimate both factors. In order to minimise such distortions, the questions on working conditions were formulated in such a manner that personal evaluations do not form the focus ("the work is hard"), but rather specific occurrences that have actually been experienced ("there are occasions on which information that is necessary for advising patients is not available").
For all scales, the frequencies, means, standard deviations and reliability coefficients (internal consistency measured by Cronbach's Alpha) were calculated. Exploratory factor analysis (principal component analysis with varimax rotation and two factors) was conducted to explore the factorial structure of the newly developed items for the analysis of stressors in the interaction with patients. In order to test the hypotheses, Pearson correlations and regression analyses were calculated. Multiple regressions were calculated to test for possible confounders. Possible differences in results for pairwise and listwise exclusion of missing items were tested for correlations. There were only minimal differences. Missing items were excluded pairwise for correlations and listwise for factor analysis and regression.
All in all, 252 individuals were invited to participate at the study. A total of 188 questionnaires were returned. Two were excluded, because data were inconsistent. This resulted in 186 valid questionnaires which corresponded to a purged return rate of 73.8%. As not all of the participants of the study worked with patients, those who did not were excluded from this study (the questionnaires of these employees were used for the project on occupational health management that we conducted at the clinic, but not for the analysis presented here). This resulted in a final sample of N = 162 employees. The demographic data of the final sample are presented in table 2.
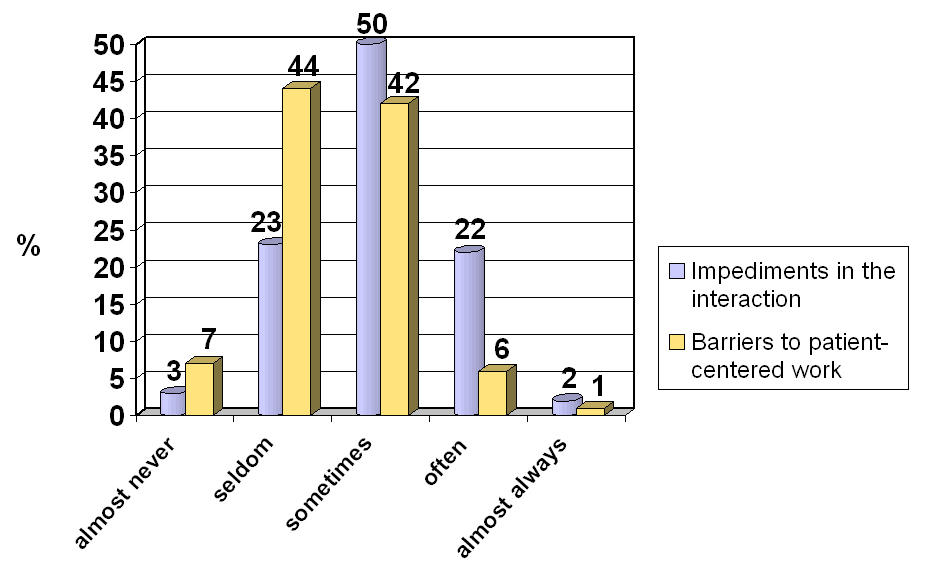
Figure 2
Frequency of impediments in the interaction with patients (N = 161) and of barriers to patient-oriented work (N = 151).
The internal consistency of the available scales yielded satisfactory to very good values for Cronbach's α between .78 and .90 (see table 1). Both newly developed scales for determining the stressors in interactions with patients yielded satisfactory Cronbach's α values of .77 (see also table 1). The exploratory factor analysis of the items of both scales revealed that a solution with two factors explained 57% of the variance. The first factor explained 29 % and the second factor 28%. The pattern of item loadings on the two components confirmed the postulated scales. The loadings ranged between 0.61 and 0.84.
The initial descriptive evaluation revealed that stressors in interactions with patients occur frequently in the investigated clinic (see table 3). The mean value for impediments in the interaction with patients was 2.81. The five-point scale ranged from almost never (1) to almost always (5). Nearly a quarter of all employees (24%) stated that they "often" or "almost always" experienced problems in dealing with patients (see fig. 2).2 50% experience such problems "sometimes". The most heavily affected were the physicians, of whom 44% responded with "often" or "almost always" with respect to encountering such stressors.
2 To calculate the frequencies of stressors and resources, scale values were recoded, so as to obtain easily interpreted graphic image of frequencies. Values from 1 to 1.49 were recoded to 1, values from 1.5 to 2.49 were recoded to 2, values from 2.5 to 3.49 were recoded to 3, values from 3.5 to 4.49 were recoded to 4 and values from 4.5 to 5 were recoded to 5.
The mean for barriers to patient-oriented work was 2.48 on the five-point scale (see table 3). This scale again ranged from almost never (1) to almost always (5). A look at the frequencies reveals that 7% of employees "often" or "almost always" encounter barriers to patient-oriented work (see fig. 2). 42% "sometimes" have such problems. When the individual items on this scale are considered, it is evident that barriers in the form of interruptions to discussions with patients are particularly common. 26% of respondents reported experiencing such interruptions "often" or "almost always". Again, the most heavily affected were the physicians at 37% followed by the nurses at 27%.
A large proportion of employees have at least some patient-oriented control, with a mean of 3.56 on the five-point scale (see table 3). All in all, 54% of respondents report having such control "often" or "almost always". Patient-oriented control was highest for the group of "others", where 73% indicated having patient-oriented control "often" or "almost always", followed by the physicians with 52%.
| Table 2: Summary of demographic data for the sample. | ||
| N | 162 | |
| Sex (%) | Female | 71.1 |
| Male | 28.9 | |
| Age (mean) | 37.2 | |
| Occupation (%) | Physicians | 18.1 |
| Nurses Ward | 41.6 | |
| Nurses OP | 13.4 | |
| Secretaries | 6.7 | |
| Others | 20.1 | |
| Job tenure at the clinic (mean years) | 6.9 | |
| Table 3: Means and standard deviations of working conditions in the interaction with patients. | ||
| Stressors and latitude | Mean | Standard deviation |
| Impediments in the interaction with patients | 2.81 | 0.75 |
| Barriers to patient-oriented work | 2.48 | 0.66 |
| Patient-oriented control | 3.56 | 0.79 |
The results show that working conditions in interactions with patients are indeed associated with health and the patient orientation. These relationships are particularly evident in the form of barriers to patient-oriented work. Below, the results for the individual hypotheses are presented.
In the first step, correlations and regression analyses were calculated to be able to analyse relationships between individual stressors and resources and each of the outcomes.
Impediments in the interaction with patients correlate significantly with emotional exhaustion and with aversion to patients (see table 4). However, there is no significant relationship with physical complaints. The regression analysis also shows that impediments in the interaction with patients are a significant predictor of emotional exhaustion and aversion to patients (see tables 5 and 6, univariate analyses).
Barriers to patient-oriented work correlate significantly with emotional exhaustion, aversion to patients and physical complaints (see table 4). The regression analysis indicates that barriers to patient-oriented work are a significant predictor of those outcomes (see table 5, 6 and 7).
There is no significant correlation between impediments in the interaction with patients and the patient orientation (see table 4). However, barriers to patient-oriented work correlate significantly negatively with the patient orientation. The regression analysis also shows that barriers to patient-oriented work are a significant predictor of patient orientation.
The correlation between patient-oriented control and the patient orientation of employees is significant (see table 4). This relationship is confirmed by the regression analysis (see table 8).
| Table 4: Relationships between working conditions, health of employees and patient orientation. | ||||
| Emotional exhaustion | Aversion to patients | Physical complaints | Patient orientation | |
| Impediments in the interaction with patients | 0.174* | 0.266** | 0.007 | –0.067 |
| Barriers to patient-oriented work | 0.374** | 0.329** | 0.320** | –0.191* |
| Patient-oriented control | –0.281** | –0.223** | 0.072 | 0.195** |
| * The correlation is significant at the 0.05 level/ ** The correlation is significant at the 0.01 level (one-sided), N = 143‒161. | ||||
In the next step, multiple regression analyses were conducted to test if the relationships between each of the working conditions and the outcomes remained significant, even if all significant predictors were tested together. Moreover, quantitative overload was introduced as a possible confounder, because the lack of time might mediate the relationships between working conditions in the interaction with patients and the outcomes.
The results show that in the multiple regression analysis, impediments in the interaction with patients are not a significant predictor of emotional exhaustion, but they still significantly predict aversion to patients (see tables 5 and 6).
Barriers to patient-oriented work remain a significant predictor of all outcomes in the multiple regression analyses (see tables 5, 6, 7 and 8).
If barriers to patient-oriented work and quantitative overload are included in the multiple regression analysis, patient-oriented control is no longer a significant predictor of patient orientation (p = 0.070, see table 8).
| Table 5: Regression analyses of emotional exhaustion. | |||||||
| Univariate | Multivariate | ||||||
| β | t | p | R2 | β | t | p | |
| Impediments in the interaction with patients | 0.174 | 2.189 | 0.030 | 0.030* | 0.100 | 1.255 | 0.212 |
| Barriers to patient-oriented work | 0.374 | 4.800 | 0.000 | 0.140** | 0.217 | 2.433 | 0.016 |
| Quantitative overload | 0.261 | 3.026 | 0.003 | ||||
| R2 | 0.199** | ||||||
| * p <0.05 / ** p <0.01 | |||||||
| Table 6: Regression analyses of aversion to patients. | |||||||
| Univariate | Multivariate | ||||||
| β | t | p | R2 | β | t | p | |
| Impediments in the interaction with patients | 0.266 | 3.409 | .001 | 0.071** | 0.170 | 2.064 | 0.041 |
| Barriers to patient-oriented work | 0.329 | 4.151 | .000 | 0.108** | 0.232 | 2.512 | 0.013 |
| Quantitative overload | 0.094 | 1.060 | 0.291 | ||||
| R2 | 0.140** | ||||||
| * p <0.05 / ** p <0.01 | |||||||
| Table 7: Regression analysis of physical complaints. | |||||||
| Univariate | Multivariate | ||||||
| β | t | p | R2 | β | t | p | |
| Barriers to patient-oriented work | 0.320 | 4.022 | 0.000 | 0.102** | 0.221 | 2.496 | 0.014 |
| Quantitative overload | 0.213 | 2.413 | 0.017 | ||||
| R2 | 0.138** | ||||||
| * p <0.05 / ** p <0.01 | |||||||
| Table 8: Regression analyses of patient orientation. | |||||||
| Univariate | Multivariate | ||||||
| β | t | p | R2 | β | t | p | |
| Barriers to patient-oriented work | –0.191 | –2.314 | 0.022 | 0.037* | –0.254 | –2.597 | 0.010 |
| Patient-oriented control | 0.195 | 2.405 | 0.017 | 0.038* | 0.155 | 1.829 | 0.070 |
| Quantitative overload | 0.206 | 2.242 | 0.027 | ||||
| R2 | 0.090** | ||||||
| * p <0.05 / ** p <0.01 | |||||||
The descriptive statistics suggest that there are differences between professions, with respect to working conditions. We therefore also calculated correlations between working conditions, health and patient orientation, by professions. The results generally seem to indicate that impediments in the interaction with patients are related to the health of nurses at the ward more closely than to the health of other professions. Barriers to patient-oriented work seem to have the strongest relationship to health and the patient orientation of nurses in the operating theatre, and yield relatively low correlations with the health and patient orientation of physicians. On the other hand, correlations between patient-oriented control and patient orientation are higher for physicians than for other professions. However, the number of cases per profession is small. Therefore, the results of the analyses should be interpreted with caution.
Supplementary qualitative evaluations demonstrate how exactly working conditions relate to various aspects of the patient orientation. For example, the time pressure devolving on physicians leads to waiting times for patients to be released from hospital and that there is then little time available for this final discussion. It also became clear that stressors in different analytical categories may occur together. For example, a lack of time, as a barrier to patient-centred work, occurs in combination with impediments in the interaction with patients, when older patients have difficulty understanding information on how they can contribute to their own health after release from the hospital.
For the hospital as an organisation, stressors in the interaction with patients may result in a number of negative consequences, including absence from work, "presenteeism" (a decrease in productivity caused by employees who are present at the workplace, although they are suffering from health problems) and high employee turnover rates. Further analysis revealed that, in the clinic under investigation, 19% of the respondents indicated that they came frequently or even very frequently to work, even when feeling unwell. Furthermore, the respondents revealed a comparatively common intention to terminate their employment at the hospital. 37% of the respondents indicated that they had thought at least once of resigning over the past year. By comparison, in the RICH-Nursing Study, 26% of 1,338 responding nurses intended to change jobs over the next year [14]. However, these figures are obviously only comparable to a limited degree, as they were not obtained by identical methods.
This study evaluated working conditions in the interaction with patients, and their relationship to the health of employees and their patient orientation. The sample consisted of 162 employees of the Orthopaedic Clinic at the Cantonal Hospital in Olten. It was assumed that stressors in the interaction with patients are positively associated with physical complaints, emotional exhaustion and aversion to patients on the part of employees (hypothesis 1) and negatively associated with an employee's patient orientation (hypothesis 2). By contrast, a positive association was postulated between patient-oriented control and patient orientation (hypothesis 3). The results of the study demonstrate that stressors in the interaction with patients do indeed predict health problems, as well as the quality of health service provided. Especially stressors in the form of barriers to patient-oriented work are significant predictors of emotional exhaustion, aversion to patients, physical complaints and a (lower) patient orientation of employees. These effects remain significant for all outcomes, even when other significant predictors and quantitative overload, as a possible confounder, are included in the regression analysis. Stressors in the form of impediments in the interaction with patients and resources in the form of patient-oriented control are significantly correlated with some of the outcomes. In the multiple regression analyses however, only the relationship between impediments in the interaction with patients and the aversion to patients remained significant.
The results underline the relevance of working conditions for the health of employees, as revealed in many other studies. They also show that for interactive work in the hospital, especially stressors in the form of barriers to patient-oriented work predict aspects of burnout and physical complaints.
Moreover, the results of other studies indicating a relationship between working conditions in the interaction with patients and patient-orientation, were confirmed. However, while a study on physicians' assistants showed that patient-oriented control predicts the level of patient-orientation, our study found that in the hospital, this relationship seems to be confounded by stressors (barriers to patient-oriented work and quantitative overload). Barriers to patient-oriented work, however, seem to predict patient orientation, even if other working conditions are included in the multiple regression analysis (patient-oriented control and quantitative overload).
From the perspective of action regulation theory, the relationship of barriers to patient-oriented work with the outcomes can be explained by the fact that regulation hindrances constrain the achievement of work objectives and cause additional effort. If such barriers occur during interactive service work at a hospital, it is quite likely that hindrances not only affect the employees' health, but also their patient orientation. One example of barriers to patient-oriented work are informational impediments in the interaction with patients (e.g., data in the patient records are not available). In this case, extra effort (investing time to obtain the information) is absolutely necessary.
For impediments in the interaction with patients, it seems that their effect might depend to a greater extent on employee competence and on the situation on hand. For example, if a nurse is well trained in caring for patients with dementia, she might experience less emotional strain than other employees caring for a similar patient.
The results concerning patient-oriented control seem to indicate that it is necessary to analyse in greater depth, possible relationships between patient-oriented control and stressors, and their relevance to a patient-orientation. It is also possible that in the hospital, patient-oriented control is less important than other forms of control (e.g., interactive control [29]). Interactive control does not focus on the latitude in fulfilling the patients' needs, but on latitude in arranging the interaction with patients, according to the needs of the employees themselves. In our recent study of geriatric care, we found that in this setting, interactive control is more important than patient-oriented control [30].
From a methodological perspective, the study is subject to a number of limitations. It entails a case study in one clinic within a hospital. It would, however, be desirable to test the results on a larger sample in other hospitals. The study is cross-sectional, so that no statements can be made as to the direction of causation of the observed relationships. Moreover, the different occupational groups could moderate the relationship between working conditions and the outcomes. Because of the relatively small sample, such moderation effects could not be tested in this study. It could also be argued that the relationships between working conditions, employee health and patient orientation are quite week (e.g., in this study, significant correlations ranged from 0.174 to 0.374). However, Zapf, Dormann and Frese show that correlations higher than r = 0.3 are not often found. This is, among other reasons, due to the fact that employee health and attitudes are influenced by many factors besides working conditions [31]. Mohr and Semmer also argue that even relatively small effect sizes are relevant, if we consider the relative risks that are associated with those effects [32].
Further research is needed to enhance our understanding of the relationship between working conditions in the interaction with patients, the health and patient orientation of employees. Other aspects of control (e.g., interaction control) should be included in empirical research on this topic. Longitudinal studies are necessary to draw causal conclusions. Moreover, larger samples with different occupational groups would provide insight into possible differences between these groups.
The identification of risks that are present in working conditions in the interaction with patients is of great interest, because this forms a basis for measures in the field of occupational health and might also help to improve the quality of care. As a consequence of our study, "health circles", in which all occupational groups in the study participated, have been implemented in the hospital where we conducted our investigation. Moderated by the School for Applied Psychology of the University of Applied Sciences Northwestern Switzerland, the employees developed a series of specific measures for improving working conditions. The focus of these measures was the reduction of barriers to patient-oriented work. Based on the suggestions made by the employees, the management team decided upon a list of measures for reducing the stressors with which the employees had to contend. These measures are currently being implemented.
Acknowledgments:The study was conducted with the financial support of the Orthopaedic Clinic of the Cantonal Hospital of Olten. We thank the participating employees very much for their commitment to the investigation. Particular thanks are due to Elisabeth Baumann for her outstanding support in organising the project. Ellen Laupper and Marco Schröder receive our thanks for their excellent support with the statistical procedures and evaluation. We thank Dr. Brian Bloch for his accurate and articulate translation of the manuscript. We would also like to thank the anonymous reviewers for their very helpful and constructive comments.
1 Büssing A, Glaser J. Mitarbeiter- und Klientenorientierung im Gesundheitswesen. Zeitschrift für Arbeits- und Organisationspsychologie 2003;47(4):222–8.
2 Eisler R. Patientenzufriedenheit in Schweizer Spitälern 2007. Available from: http://www.comparis.ch/Krankenkassen/spitalfuehrer/dokument/Studie_Patientenzufriedenheit_2007.pdf
3 Biaggi P, Peter S, Ulich E. Stressors, emotional exhaustion and aversion to patients in residents and chief residents – what can be done? Swiss Med Wkly. 2003;133:339–46.
4 Ulich E, Wülser M. Gesundheitsmanagement in Unternehmen. Arbeitspsychologische Perspektiven. 4rd ed. Wiesbaden: Gabler; 2010.
5 Schabracq M, Cooper C, Travers C, von Maanen D. Occupational Health Psychology: the Challenge of Workplace Stress. Chichester: Wiley-Blackwell; 2002.
6 Bamberg E, Busch C, Ducki A. Stress- und Ressourcenmanagement: Strategien und Methoden für die neue Arbeitswelt. Bern: Huber; 2003.
7 Greiner BA, Krause N, Ragland DR, Fisher JM. Objective Stress factors, accidents, and absenteeism in transit operators: A theoretical framework and empirical evidence. J Occup Health Psychol. 1998;3(2):130–46.
8 Leitner K, Resch MG. Do the effects of job stressors on health persist over time? A longitudinal study with observational measures. J Occup Health Psychol. 2005;10(1):18–30.
9 Semmer N, Udris I. Bedeutung und Wirkung von Arbeit. In: Schuler H, ed. Lehrbuch Organisationspychologie. Berne: Huber; 2004.
10 Udris I, Frese M. Belastung und Beanspruchung. In: Graf Hoyos C, Frey D, Stahlberg D ed. Angewandte Psychologie. Weinheim: Psychologie Verlags Union; 1999.
11 Glaser J, Hornung S. Interaction, work characteristics, and mental health in nursing. Proceedings of the 2nd International Conference on Applied Human Factors and Ergonomics (AEI 2008). Las Vegas, NV: AEI; 16th of july, 2008.
12 Hacker W, Reinhold S. Beanspruchungsscreening bei Humandienstleistungen BHD-System. Frankfurt a.M.: Swets Tests Services; 1999.
13 Aiken LH, Clarke SP, Sloane DM, Schochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288(16):1987–93.
14 Schubert M, Schaffert-Witvliet B, De Geest, S, Aiken, L, Sloane, DM, Clarke, S, Abraham, I. RICH-Nursing Study. Rationing of nursing care in Switzerland. Effects of rationing of nursing care in Switzerland on patients' and nurses' outcomes. Basel: Basel Institute for Clinical Epidemiology; 2005.
15 Wallace JE, Lemaire J. Determinants of Physician Well Being: Results from the physician Survey. Stage Two Report. Calgary: University of Calgary; 2009.
16 Glaser J. Analysis and design of nursing work – a decade of research in different fields of health care. In: Korunka C, Hoffmann P, eds. Change and quality in human service work. München: Hammp; 2005: 13–31.
17 Büssing A, Glaser J. Mitarbeiter- und Patientenorientierung – Konzept und Evaluation von Qualität im Krankenhaus. In: Büssing A, Glaser J, eds. Dienstleistungsqualität und Qualität des Arbeitslebens im Krankenhaus. Göttingen, Hogrefe; 2003: 247–70.
18 Garmann AN, Corrigan PW, Morris S. Staff burnout and patient satisfaction. Evidence at the care unit level. J Occup Health Psychol. 2002;7(3):235–41.
19 Nerdinger FW, Blickle G, Schaper N. Arbeits- und Organisationspsychologie. 2nd ed. Berlin: Springer; 2011.
20 Schneider B, White S, Paul MC. Linking service climate and customer perceptions of service quality: Test of a causal model. J Appl Psychol. 1998;83(2):150–63.
21 Salanova M, Agut S. Linking organizational resources and work engagement to employee performance and customer loyalty: The mediation of service climate. J Appl Psychol. 2005;90(6):1217–27.
22 Schubert M, Schaffert-Witvliet B, De Geest S. Auswirkungen von Kosteneinsparungsstrategien und Stellenbesetzung auf die Ergebnisse von Patienten und Pflegefachpersonen. Eine Literaturübersicht. Pflege, 18, 2005: 320–8.
23 Schubert M, De Geest, S, Glass, T, Schaffert-Witvliet B, Clarke S. Prevalence, correlates and threshold levels of implicit rationing of nursing care in Swiss acute care hospitals. Int J Nurs Stud. 2009;46:884–93.
24 Dormann C, Spethmann K, Weser D, Zapf D. Organisationale und persönliche Dienstleistungsorientierung und das Konzept des kundenorientierten Handlungsspielraums. Zeitschrift für Arbeits- und Organisationspsychologie. 2003;47:194–207.
25 Rieder, K. Zwischen Lohnarbeit und Liebesdienst. Belastungen in der Krankenpflege. Weinheim: Juventa; 1999.
26 Rieder K. Dialogische Dienstleistungsarbeit in der Krankenpflege: Konzepte für die Analyse von Belastungen und Anforderungen. In: Ulich E, Herausgeber. Arbeitspsychologie in Krankenhaus und Arztpraxis. Berne: Huber; 2003: 151–67.
27 Rimann M, Udris J. SAA und SALSA: Zwei Fragebögen zur subjektiven Arbeitsanalyse. In: Dunckel H, Herausgeber: Handbuch psychologischer Arbeitsanalyseverfahren. Zürich: vdf Hochschulverlag; 1999: 397–420.
28 Dunckel H, Pleiss C, Herausgeber. Kontrastive Aufgabenanalyse. Grundlagen, Entwicklungen und Anwendungserfahrungen. Zürich: vdf; 2007.
29 Büssing A, Giesenbauer B, Glaser J, Höge T. Arbeitsbedingungen, Interaktionsarbeit und Qualität der Arbeit in der stationären Altenpflege. Berichte aus dem Lehrstuhl für Psychologie der TU München (Bericht Nr. 58). München: Technische Universität; 2001.
30 Rieder, K, Herms, I, Schröder M, Hausen A. Service-orientiertes Seniorenzentrum – Arbeitsbedingungen und Dienstleistungsqualität in der Altenpflege. Tagung Professionalisierung Interaktiver Arbeit, Munich, 15th of July 2010.
31 Zapf, D, Dormann, C, Frese, M. Longitudinal studies in organizational stress research: a review of the literature with reference to methodological issues. J Occup Health Psychol. 1996;1(2):145–69.
32 Mohr, G, Semmer, NK. Arbeit und Gesundheit: Kontroversen zu Person und Situation. Psychologische Rundschau. 2002;53(2):77–84.
Funding / potential competing interests: The present study was conducted at the University of Applied Sciences Northwestern Switzerland in Olten, with the financial support of the Orthopaedic Clinic of the Olten Cantonal Hospital.