Underreporting of needlestick and sharps injuries among healthcare workers in a Swiss University Hospital
DOI: https://doi.org/10.4414/smw.2012.13523
Cathy
Voide, Katharine Elizabeth
Darling, Alain
Kenfak-Foguena, Véronique
Erard, Matthias
Cavassini, Catherine
Lazor-Blanchet
Summary
OBJECTIVES: To determine 1) rates of needlestick and sharps injuries (NSSIs) not reported to occupational health services, 2) reasons for underreporting and 3) awareness of reporting procedures in a Swiss university hospital.
MATERIALS AND METHODS: We surveyed 6,367 employees having close clinical contact with patients or patient specimens. The questionnaire covered age, sex, occupation, years spent in occupation, history of NSSI during the preceding twelve months, NSSI reporting, barriers to reporting and knowledge of reporting procedures.
RESULTS: 2,778 questionnaires were returned (43.6%) of which 2,691 were suitable for analysis. 260/2,691 employees (9.7%) had sustained at least one NSSI during the preceding twelve months. NSSIs were more frequent among nurses (49.2%) and doctors performing invasive procedures (IPs) (36.9%). NSSI rate by occupation was 8.6% for nurses, 19% for doctors and 1.3% for domestic staff. Of the injured respondents, 73.1% reported all events, 12.3% some and 14.6% none. 42.7% of doctors performing invasive procedures (IPs) underreported NSSIs and represented 58.6% of underreported events. Estimation that transmission risk was low (87.1%) and perceived lack of time (34.3%) were the most common reasons for non-reporting. Regarding reporting procedures, 80.1% of respondents knew to contact occupational health services.
CONCLUSION: Doctors performing IPs have high rates of NSSI and, through self-assessment that infection transmission risk is low or perceived lack of time, high rates of underreporting. If individual risk analyses underestimate the real risk, such underreporting represents a missed opportunity for post-exposure prophylaxis and identification of hazardous procedures. Doctors’ training in NSSI reporting merits re-evaluation.
Abbreviations
NSSIs needlestick and sharps injuries
Introduction
Healthcare workers (HCWs) are at risk of occupational blood-borne infections, notably hepatitis B virus (HBV), hepatitis C virus (HCV) and human immunodeficiency virus (HIV), if percutaneous or mucocutaneous exposure to blood and other body fluids should occur [1–3]. More than three million HCWs worldwide are exposed to HBV, HCV or HIV each year as a result of needlestick and sharps injuries (NSSIs) [4]. In the year 2000, 16,000 HCV, 66,000 HBV and 1,000 HIV infections may have occurred worldwide among HCWs following such events [5].
In Switzerland, 8,602 occupational injuries with exposure to blood or other body fluids were notified to the national health reference centres between 2001 and 2008 [6]. This report showed an increase in NSSI cases during this period (on average 1,146 cases reported per year) compared to the period between 1997 and 2000 (average of 671 cases reported per year). The authors of this report suggest that the increase observed may be due to a real increase in the rate of NSSIs, improved rates of reporting or greater risk appreciation among HCWs. Of the source patients associated with the 8602 NSSI events reported between 2001 and 2008 who were tested, 2.2% were positive for HBV (HBV serology performed only when the HCW sustaining the NSSI is not immune), 12.3% were positive for HCV, and 6.5% for HIV.
The risk of HBV, HCV and HIV transmission after exposure to blood and body fluids (respectively 6–30%, 0.5% and 0.3%) [7, 8] increases with increasing viral load of the source patient and the amount of blood exposure [9]. Blood exposure may be significant for HCWs performing invasive procedures (IPs), those procedures which involve the use of sharp instruments and/or where there is a risk of contact between a patient’s blood or body fluids and the blood of the HCW.
When NSSIs occur, reporting is important for reasons of treatment and prevention. For the injured individual, NSSI reporting instigates evaluation of the need for post-exposure prophylaxis, allows early detection of seroconversion and helps to decrease anxiety. More generally, injury reporting allows identification of hazardous devices or procedures and so serves to diminish the risk of future injuries. Preventive strategies such as HCW education, increased use of universal precautions and implementation of safety devices have been shown to significantly reduce NSSIs [10–13].
In our hospital, a telephone hotline managed by the occupational health service is in place, and all staff are encouraged to report every NSSI involving blood and body fluids. In spite of this, a proportion of NSSIs goes unreported. Indeed, the incidence of NSSIs observed from prospective studies or retrospective questionnaires may be as much as 10-fold higher than that derived from standard reporting systems [14, 15]. The purpose of this study was to determine the rate of NSSI underreporting to our occupational health service, to examine the reasons for underreporting, and to assess awareness of reporting procedures in a Swiss university hospital.
Methods
Ethics statement
Participation in this study was voluntary and completion of the survey implied consent for study participation. The study, including the consent procedure, was granted ethical approval by the university ethics committee of our institution (protocol 244/08, Centre Hospitalier Universitaire Vaudois and University of Lausanne, Lausanne, Switzerland) and complied with the guidelines of the Declaration of Helsinki.
Setting
The study was conducted in the University Hospital of Lausanne, Switzerland, a 1,300-bed teaching hospital with 10,000 employees, of whom 1,667 (17%) are doctors (surgeons, anaesthetists, radiologists, obstetricians, gynaecologists, paediatricians and internal physicians) and 3,972 (40%) are nurses and domestic staff.
Procedure
In February 2009, an anonymous 20-item questionnaire was sent to all employees routinely having close clinical contact with patients and/or patient specimens. This group included all doctors and nurses, other HCWs such as physiotherapists, occupational therapists and radiographers, laboratory staff, porters and domestic staff (cleaners). All doctors and senior nurses received the questionnaire by email (n = 1,985); the other employees received a paper copy by post (n = 4,382). For those who received the questionnaire by email, 2 reminder emails were sent 5 weeks after the initial questionnaire.
Questionnaire
The questionnaire was developed in the infectious diseases and occupational medicine services of the hospital and distributed to the HCWs after initial pilot testing.
The questionnaire informed the HCWs of the purpose of the study and suggested an approximate time that the questionnaire would take to complete (10 minutes). The first part of the questionnaire covered demographics: age, gender, occupation, department and number of years in the present occupation. The questionnaire sent to doctors differed from that sent to all other employees in a single respect in that doctors were asked to state whether they considered themselves to be ‘interventional’ (routinely performing IPs), or ‘non-interventional’ (not performing IPs). Respondents were categorised as follows: doctors performing IPs, doctors not performing IPs, nurses, domestic staff and ‘others’: laboratory staff, physiotherapists, radiographers, porters, occupational therapists, pathology assistants, and ‘administrative staff’ (respondents listed as nurses who were working outside the clinical context at the time of the questionnaire).
The second part of the questionnaire examined the number of NSSIs sustained during the preceding twelve months and explored reporting practices and possible barriers to reporting. We focused on percutaneous (as opposed to mucocutaneous) injuries because they represent more than 85% of occupational blood and body fluids exposures in our teaching hospital (unpublished data). If one or more NSSIs had occurred during the preceding twelve months, we asked each respondent if the event(s) had been reported to the occupational health service (always, certain cases or not reported). Injured respondents who had not reported all NSSIs were invited to give reasons for underreporting from the following choice: ‘I considered the blood low risk’; ‘I did not have time’; ‘I did not know I have to report NSSIs’ and, ‘I did not know where to report the NSSI’.
The final part of the questionnaire examined respondents’ awareness of reporting procedures for NSSIs in our hospital. They had to choose one of the following options: ‘I find out about the risks associated with the blood involved’, ‘I report the event to my direct superior’, ‘I dial the telephone number designated for this type of issue’ and, ‘I do not know’.
Data regarding details of exposure injuries (devices used, circumstances surrounding the NSSI, infection status of the source patient, use of protective equipment, knowledge of standard protections) were not collected in this study. These data have been collected since 1989 and have been previously analysed in a Swiss national survey [6].
Statistical analysis
Data were entered into a database and all analyses were performed using Stata 10 (StataCorp LP). We performed descriptive and multivariate analyses. Observed frequencies were compared using the Chi-squared test, where P<0.05 was considered to be statistically significant.
Results
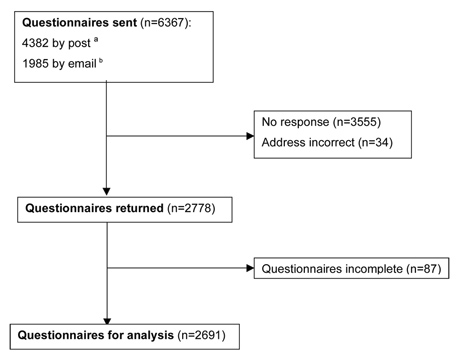
The response rate was 43.6% (2,778 of 6,367). Of the returned questionnaires, 87 (3.1%) were incomplete and so were excluded from the study, leaving 2,691 questionnaires (42.3%) for analysis (fig. 1). The response rate for each HCW category is shown in table 1.
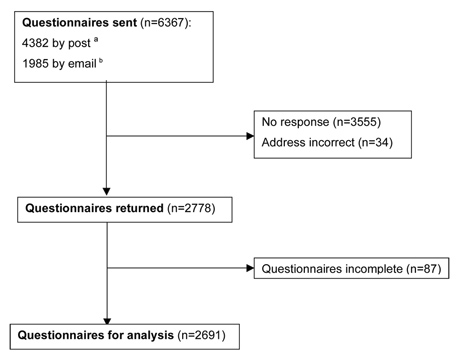
Figure 1
Study scheme of patients included in the analysis. a 3,201 nurses, 447 domesic staff, 388 laboratory staff, 123 physiotherapists, 108 radiographers, 51 porters, 41 occupational therapistes, 14 pathology assistants, 3 adminstrative staff. b 1,667 doctors, 318 nurses.
Of the 2691 HCWs analysed, the majority were female (n = 1,965, 73%), mean age 40.2 years (sd 10.6 years). Two hundred and sixty respondents (9.7%) had sustained at least one NSSI during the preceding twelve months. Of these, 171 (65.8%) had sustained one NSSI, 60 (23.1%) had sustained two and 29 (11.1%) more than two. The number of NSSIs per respondent varied from 1 to 10, with a total number of NSSIs sustained of 386 (data not shown).
Of the 260 injured HCWs, the highest rate of NSSI was observed in nurses (49.2%), followed by doctors routinely performing IPs (36.9%); 7.7% of NSSIs occurred in doctors not routinely performing IPs, 0.7% in domestic staff and 5.4% in the ‘others’ category. Descriptive characteristics of the 260 HCWs who sustained one or more NSSIs are shown in table 2.
With respect to reporting rates, 190 (73.1%) of injured HCWs had reported all NSSIs to the occupational health service. By age, HCWs aged between 16 and 25 years had the highest rates of NSSI reporting (90.9%, data not shown). By occupation, 83.6% of nurses and 85.7% of ‘others’ reported all NSSIs, compared to only 59.5% of doctors (57.3% of doctors performing IPs) (table 3).
Multivariate analysis showed that the difference in underreporting between doctors and nurses was significant (67.1% underreporting in doctors versus 30% in nurses, OR 3.29, CI (95%) 1.59–6.79, P= 0.001) (table 4). Doctors performing IPs underreported more NSSIs than doctors not performing IPs (87.2% versus 12.8%, OR 1.47, CI (95%) 0.5–4.27) although this difference was not significant (P= 0.481). Finally, underreporting was significantly higher among employees who had worked in their occupation for 10 years or more (57.1% versus 42.9%, OR 0.35, CI (95%), P = 0.014) (table 4).
Of the 70 HCWs who had not reported all NSSIs to the occupational health service, 32 (45.7%) had reported only certain events and 38 (54.3%) had reported none. Twenty-six out of thirty-eight (68.4%) of the HCWs who had reported none of their NSSIs were doctors performing IPs. We observed an inverse relationship between the number of NSSIs sustained and the likelihood to report among HCWs who had sustained over two NSSIs during the period surveyed: among HCWs who sustained 2 or fewer NSSIs (n = 231, 88.8%), 79.6% reported all events; among those who sustained 3 or more NSSIs (n = 29, 11.2%), only 20.7% reported all events. Regarding barriers to reporting, the principal reasons for not reporting were 1) self estimation that the NSSI was low risk with respect to blood-borne virus transmission (87.1%) and 2) perceived lack of time (34.3%) (table 5). None of the respondents listed lack of knowledge that reporting was required nor lack of knowledge about reporting procedures as reasons for not reporting (table 5).
With respect to respondents’ awareness of NSSI reporting procedures (n = 2691), 80.1% stated they should telephone the occupational health service, 71.1% stated they should report the injury to their superior and 52.9% stated they should seek advice on infection transmission risk. Only 0.8% of all respondents stated they did not know what to do in the event of NSSI.
|
Table 1: Response rate by occupation. |
|
Occupation
|
Questionnaires sent, n
|
Questionnaires returned *, n (%)
|
| Nurses |
3,525 |
1,489 (42.2) |
| Doctors |
1,667 |
612 (36.7) |
| Domestic staff |
447 |
157 (35.1) |
| Others †
|
728 |
433 (59.5) |
| Total |
6,367 |
2,691 (42.3) |
| * Questionnaires returned and suitable for analysis.
† Others = laboratory staff (388), physiotherapists (123), radiographers (108), porters (51), occupational therapists (41), pathology assistants (14), administrative staff (3). |
|
Table 2: Descriptive characteristics of the 260 healthcare workers who sustained one or more needlestick and sharps injury (NSSI). |
|
Occupation
|
n (%)
|
| Doctors performing IPs |
96 (36.9) |
| Doctors not performing IPs |
20 (7.7) |
| Nurses |
128 (49.2) |
| Domestic staff |
2 (0.7) |
| Others |
14 (5.4) |
|
Female sex (n = 157)
|
|
| Doctors performing IPs |
27 (17.2) |
| Doctors not performing IPs |
8 (5.1) |
| Nurses |
110 (70.1) |
| Domestic staff |
1 (0.6) |
| Others |
11 (7) |
|
Age
|
|
| 16–35 years |
130 (50) |
| 36–55 years |
106 (40.8) |
| >55 years |
24 (9.2) |
|
Work department
|
|
| Surgery |
93 (35.8) |
| Anaesthetics |
42 (16.2) |
| Intensive care |
10 (3.8) |
| Internal medicine and paediatrics |
52 (20) |
| Emergency medicine |
17 (6.5) |
| Psychiatry |
11 (4.2) |
| Laboratory and radiology |
6 (2.3) |
| Domestic service |
2 (0.7) |
| Other or not specified |
27 (10.4) |
|
Years in occupation
|
|
| <10 years |
142 (54.6) |
| ≥10 years |
118 (45.4) |
| Abbreviations: IPs, invasive procedures. |
|
Table 3: Rate of needlestick and sharps injury (NSSI) per occupation and proportion of NSSIs reported or not reported to the occupation health service. |
|
|
Respondents injured
n (%)
|
Respondents reporting all injuries
n (%)
|
Respondents reporting some or no injuries
n (%)
|
| All employees
(n = 2,691) |
260 (9.7) |
190/260 (73.1) |
70/260 (26.9) |
| Doctors performing IPs
(n = 252) |
96 (38.1) |
55/96 (57.3) |
41/96 (42.7) |
| Doctors not performing IPs
(n = 360) |
20 (5.6) |
14/20 (70) |
6/20 (30) |
| Nurses
(n = 1,489) |
128 (8.6) |
107/128 (83.6) |
21/128 (16.4) |
| Domestic staff
(n = 157) |
2 (1.3) |
2/2 (100) |
|
| Others
(n = 433) |
14 (3.2) |
12/14 (85.7) |
2/14 (14.3) |
| Abbreviations: IPs, invasive procedures. |
|
Table 4: Multivariate analysis of demographic and occupational factors associated with underreporting. |
| |
All NSSI reported
n (%)
|
Not all NSSIs reported
n (%)
|
Odds ratio
|
CI (95%)
|
P
|
| Total HCWs injured, n = 260 |
190 |
70 |
|
|
|
| Male
Female
|
64 (33.7)
126 (66.3) |
39 (55.7)
31 (44.3) |
1.29 |
0.64–2.62 |
0.476 |
| Doctors (all)
– Doctors performing IPs
– Doctors not performing IPs
Nurses |
69 (36.3)
55
14
107 (56.3) |
47 (67.1)
41
6
21 (30) |
1.47
3.29 |
0.50–4.27
1.59–6.79 |
0.481
0.001 |
| Domestic staff
Others |
2 (1.1)
12 (6.3) |
0
2 (2.9) |
|
|
|
| Age at NSSI:
<35 years
≥35 years |
100 (52.6)
90 (47.4) |
30 (42.9)
40 (57.1) |
1.18 |
0.49–2.78 |
0.708 |
| Years worked in occupation:
<10 years
≥10 years |
112 (58.9)
78 (41.1) |
30 (42.9)
40 (57.1) |
0.35 |
0.15–0.80 |
0.014 |
| Abbreviations: NSSIs, needlestick and sharps injuries; IPs, invasive procedures; CI, confidence interval. |
|
Table 5: Reasons for not reporting NSSIs (more than one response permitted). |
| |
Total
n (%)
|
Doctors
n (%)
|
Nurses
n (%)
|
Others
n (%)
|
| “I considered the blood low risk” |
61 (87.1%) |
40 (85.1%) |
19 (90.5%) |
2 (100%) |
| “I did not have time” |
24 (34.3%) |
17 (36.2%) |
7 (33.3%) |
|
| “I did not know that I have to report NSSIs” |
|
|
|
|
| “I did not know where to report the NSSI” |
|
|
|
|
Discussion
In our retrospective study of HCWs in a Swiss university hospital, 260/2,691 respondents (9.7%) sustained one or more NSSI during the preceding twelve months. Among these individuals, the rates of NSSI were highest in nurses and doctors at 49.2% and 44.6% respectively. 73.1% of HCWs reported all NSSIs sustained. While doctors had among the highest rates of NSSI, they also had the highest rate of underreporting (67.1%), a level significantly higher than that of nurses (P <0.001). In the subgroup of doctors performing IPs, the rate of underreporting was 42.7%.
Our large study considering all HCWs at risk of percutaneous injury shows that the individuals most injured are also those most exposed (doctors performing IPs and nurses). However, among these groups, doctors, specifically those performing IPs, have the highest rate of underreporting. Underreporting rates of 22 to 82% have been reported in the literature [1, 3, 15, 16] and our observation that doctors report NSSIs less frequently than other HCW categories is also consistent with previous studies [17, 18].
Against our findings among doctors, we found that HCWs classed as, ‘others’ and domestic staff, making up the occupational groups with the lowest rates of NSSI, had the lowest rates of underreporting, at 0 to 14.3%. These low rates of underreporting could be explained by a number of factors: better information at the time of engagement; continuous education throughout the time of employment; perhaps more time allocated within their daily activities to facilitate reporting. The converse finding in our study, that higher numbers of NSSIs sustained are associated with reduced reporting has been described elsewhere, with reporting rates of 84% for a single percutaneous injury reducing to 24% when more than five NSSIs were sustained [3, 16]. A further possibility therefore for low underreporting among ‘others’ and domestic staff and high underreporting among doctors is a phenomenon of desensitisation: the more a HCW is exposed to NSSI-prone activities and the more NSSIs are sustained, the more relaxed the HCW becomes with respect to reporting.
With this in mind, the reasons for underreporting are of interest. We found that the chief reason for not reporting NSSIs was that the HCWs we questioned considered the blood to be low risk for viral infection transmission. We cannot tell from our questionnaire whether this opinion was derived from previous visits to the occupational health service following previous NSSIs, whether it came from personal literature interpretation or from colleague hearsay. It is also possible that HCWs make their own evaluation of the source patient in terms of blood-borne virus risk if the patient’s social and medical history is well known to them. Whatever the basis of a HCW’s opinion that transmission risk is low, several studies among doctors have shown that self-evaluation of transmission risk following NSSI frequently underestimates the real risk. Only 34% of anaesthetists correctly recognised the risk of seroconversion of HIV following a NSSI [19]. In a survey of 768 active surgeons regarding knowledge of seroconversion rates following exposure to blood infected with HIV, HBV and HCV, Patterson et al. reported correct responses in respectively 50.5%, 14.2% and 19.4% of individuals [20]. If self-assessment of blood-borne virus transmission risk underestimates the real risk, this has implications for post-exposure prophylaxis evaluation and delivery.
The second most frequent reason for not reporting was that of perceived lack of time. The perception of lack of time could serve to compound the notion that a NSSI is low-risk: if an injury is ‘probably’ low risk but the HCW has plenty of time, that person is more likely to report the incident than if time is limited. Perceived lack of time as a reason for not reporting has been described elsewhere [21] and merits exploration within different hospital settings. One factor unlikely to be responsible for underreporting is the lack of awareness of hospital reporting procedures, with 80.1% respondents stating they should telephone the occupational health service. Only 0.8% of all respondents stated they did not know what to do in the event of NSSI. It is hoped that individuals answering that they would report to their superior or seek advice on infection transmission risk would ultimately be directed to the occupational health service.
Our study has several limitations. First, the results we report are derived from the 43.6% of employees who responded and we should apply these with caution when considering the hospital workforce as a whole. Against this limitation, the NSSI rate we observed – 29.7 injuries per 100 licensed beds – is similar to rates described elsewhere of 11.8 to 25.4 per 100 licensed beds [22, 23] and within the range of those reported in other Swiss university hospitals of 23.6 to 31.4 per 100 licensed beds [24].
Although the rate of underreporting among doctors seems high, the rate of reporting of all NSSIs when all the HCWs were grouped together was 73.1%. Selection (volunteer) bias is a possible reason for this figure, where individuals who had previously sustained and reported a NSSI may be more likely to complete the questionnaire than those who had not. We do not have the demographic characteristics of people who did not respond to the survey. Potential selection (nonrespondent) bias is particularly relevant for domestic staff (lowest response rate, possibly explained by a high proportion of people who are not native French speakers). From our NSSI data, it would seem that domestic staff rarely sustains an injury, suggesting that hospital policy and precautions taken to prevent NSSIs in this HCW category are effective. If the low response rate among domestic staff was due to linguistic factors regarding the questionnaire rather than the fact that relatively few individuals had sustained a NSSI, the idea that hospital policy is effective among this HCW group may be inaccurate.
The implementation of reminder emails for doctors and senior nurses (the HCWs who received the initial questionnaire by email) may have skewed the response rate in these groups. However, given that doctors had the second lowest response rate after domestic staff, it seems unlikely that the reminder emails served to disproportionately favour doctor participation in our study. Although 73% of all respondents were female, this reflects the representation of female staff in our hospital of 69% at the time this study was conducted (human resources office annual report, 2009).
Another limitation is the retrospective design of the survey. HCWs were asked to give the number of NSSIs sustained during the preceding twelve months. Individuals sustaining a significant NSSI are likely to remember the event, particularly if there is associated anxiety, and so the number of false negatives is likely to be low. However, the precise number of injuries sustained during the period in question may be open to recall bias.
In summary, this study allowed us to determine 1) the rate of NSSI underreporting to the occupational health service in our hospital (26.9%) and 2) the perceived barriers to reporting. Work on NSSI prevention has been carried out in our centre, with the implementation of universal precautions and the use of safer devices. We must now direct efforts towards training and educating HCWs, in particular doctors performing IPs, and stress the importance of reporting NSSIs as a means of maximally reducing the risk of blood-borne infections. Training should be provided to newly employed HCWs, and updated throughout their time of engagement, and HCWs must be reminded that self-assessment of the transmission risk is not reliable. Facilitating the reporting process, notably the time taken to report a NSSI, is another approach that merits consideration at local level. Taken together, these measures to optimise reporting should enhance occupational health care delivery to the HCWs who require it most.
References
1 Tarantola A, Abiteboul D, Rachline A. Infection risks following accidental exposure to blood or body fluids in health care workers: a review of pathogens transmitted in published cases. Am J Infect Control. 2006;34:367–75.
2 Wicker S, Jung J, Allwinn R, Gottschalk R, Rabenau HF. Prevalence and prevention of needlestick injuries among health care workers in a German university hospital. Int Arch Occup Environ Health. 2008;8:347–54.
3 Schmid K, Schwager C, Drexler H. Needlestick injuries and other occupational exposures to body fluids amongst employees and medical students of a German university: incidence and follow-up. J Hosp Infect. 2007;65:124–30.
4 White SM . Needlestuck. Anaesthesia. 2007;62:1199–201.
5 Pruss-Ustun A, Rapiti E, Hutin Y. Estimation of the global burden of disease attributable to contaminated sharps injuries among health-care workers. Am J Ind Med. 2005;48:482–90.
6 Colombo C, Ledergerber F, Zysset F, Francioli P, Cavassini M, Lazor-Blanchet C, et al. Exposition au risque infectieux VIH, VHB et VHC chez le personnel des établissements de soins en Suisse de 2001 à fin juin 2008. BAG Bulletin. 2010;3:36–42.
7 Deisenhammer S, Radon K, Nowak D, Reichert J. Needlestick injuries during medical training. J Hosp Infect. 2006;63:263–7.
8 Trim JC, Elliott TS. A review of sharps injuries and preventative strategies. J Hosp Infect. 2003;53:237–42.
9 Cardo DM, Culver DH, Ciesielski CA, Srivastava PU, Marcus R, Abiteboul D, et al. A case-control study of HIV seroconversion in health care workers after percutaneous exposure. Centers for Disease Control and Prevention Needlestick Surveillance Group. N Engl J Med. 2007;337:1485–90.
10 Cullen BL, Genasi F, Symington I, Bagg J, McCreaddie M, Taylor A. Potential for reported needlestick injury prevention among healthcare workers through safety device usage and improvement of guideline adherence: expert panel assessment. J Hosp Infect. 2006;63:445–51.
11 Mendelson MH, Lin-Chen BY, Solomon R, Bailey E, Kogan G, Goldbold J. Evaluation of a safety resheathable winged steel needle for prevention of percutaneous injuries associated with intravascular-access procedures among healthcare workers. Infect Control Hosp Epidemiol. 2003;24:105–12.
12 Adams D, Elliott TS. Impact of safety needle devices on occupationally acquired needlestick injuries: a four-year prospective study. J Hosp Infect. 2006;64:50–5.
13 Azar-Cavanagh M, Burdt P, Green-McKenzie J. Effect of the introduction of an engineered sharps injury prevention device on the percutaneous injury rate in healthcare workers. Infect Control Hosp Epidemiol. 2007;28:165–70.
14 Lee JM, Botteman MF, Xanthakos N, Nicklasson L. Needlestick injuries in the United States. Epidemiologic, economic, and quality of life issues. AAOHN. 2005;J 53:117–33.
15 Elder A, Paterson C. Sharps injuries in UK health care: a review of injury rates, viral transmission and potential efficacy of safety devices. Occup Med (Lond). 2006;56:566–74.
16 Doebbeling BN, Vaughn TE, McCoy KD, Beekmann SE, Woolson RF, Ferguson KJ, et al. Percutaneous injury, blood exposure, and adherence to standard precautions: are hospital-based health care providers still at risk? Clin Infect Dis. 2003;37:1006–13.
17 Nelsing S, Nielsen TL, Nielsen JO. Percutaneous blood exposure among Danish doctors: exposure mechanisms and strategies for prevention. Eur J Epidemiol. 1997;13:387–93.
18 Tan L, Hawk JC 3rd, Sterling ML. Report of the Council on Scientific Affairs: preventing needlestick injuries in health care settings. Arch Intern Med. 2001;161:929–36.
19 Diprose P, Deakin CD, Smedley J. Ignorance of post-exposure prophylaxis guidelines following HIV needlestick injury may increase the risk of seroconversion. Br J Anaesth. 2000;84:767–70.
20 Patterson JM, Novak CB, Mackinnon SE, Patterson GA. Surgeons’ concern and practices of protection against bloodborne pathogens. Ann Surg. 1998;228:266–72.
21 Au E, Gossage JA, Bailey SR. The reporting of needlestick injuries sustained in theatre by surgeons: are we under-reporting? J Hosp Infect. 2008;70:66–70.
22 Patrick DL, Murray TP, Bijby J, Auerbach J, Davis LK, et al. Sharps injuries among hospital workers in Massachusetts. Findings from the Massachusetts Sharps Injury Surveillance System. 2007. Massachusetts Department of Public Health Occupational health Surveillance Programme 2009.
23 Hernandez Navarrete MJ, Campins Marti M, Martinez Sanchez EV, Ramos Perez F, Garcia de Codes Ilario A, Arribas Llorente JL. Occupational exposures to blood and biological material in healthcare workers. EPINATEC Project 1996–2000. Med Clin. 2004;122:81–6.
24 Colombo C, Masserey V, Ruef C. Incidence of needlestick injuries and other sharps exposures in Swiss acute care hospitals: results of a sentinel surveillance study. J Hosp Infect. 2011;6:181–3.