Figure 1
Unit’s patient safety climate (n = 120).
DOI: https://doi.org/10.4414/smw.2012.13501
Today’s hospital-based healthcare is highly complex and despite high quality standards adverse events (AEs) occur every day. Internationally, between 2.9% and 16.6% of hospitalised patients are affected by AEs, such as surgical (peri- and postoperative) complications, medication errors, healthcare-associated infections or patient falls [1–6]. Healthcare is often delivered in a high risk and dynamic environment, involving a vast array of technology and many individual decisions and judgments by healthcare professionals. Most AEs do not result from individual recklessness [7], but from faulty systems/processes that provide conditions that lead people to make mistakes or fail to prevent them [8].
According to international experts, the development of a so-called “culture of safety” within healthcare organisations appears to be a systemic and fruitful approach to better understanding of patient safety mechanisms and protecting patients from harm due to AEs [9, 10]. Patient safety culture is defined as a “subset of organizational culture, which relates specifically to values and beliefs concerning patient safety within healthcare organizations” [11, p. 312]. In high-risk industries such as aviation or nuclear power a common approach to the evaluation and improvement of the safety culture is the use of workforce surveys designed to assess and monitor the safety climate (i.e. the perceived safety culture of a particular place at a particular time) [12].
Measuring the patient safety climate (PSC) in healthcare organisations provides insight into the safety of healthcare environments [10]. Such results, in turn, can help to identify problematic areas/issues and lead to the development of adequate counter measures [13–16]. Recent studies investigated the PSC within hospitals and its various clinical areas. The results showed that employees’ perceptions of the PSC varied between and within hospitals [17]. Personnel in specialised areas where patients may be at higher risk for AE, such as emergency departments, perceived lower PSC than those in other hospital wards. Nurses had an on the whole lower perception of the PSC than other disciplines (e.g. physicians) and frontline workers perceived a lower PSC than management [18–20]. Studies have identified problematic PSC issues in intensive care units [21–23] and operating rooms [24–27], such as poor communication and teamwork [25].
Despite increasing interest in studying the PSC in healthcare organisations in recent years, most research on this topic was carried out in the US and few studies have been conducted in European healthcare systems [15, 28, 29], including Switzerland [30]. In addition, although the perception of PSC has been found to differ between various healthcare professionals, little attention has been given to describing nurses’ perceptions of the PSC in depth, which is important considering their key role in delivering patient care and protecting patients from harm [31]. For the first time in Switzerland, we aimed (1) to describe the nurse-reported PSC on general medical, surgical and mixed medical-surgical units in a national hospital sample, (2) to describe nurses’ engagement in specific safety behaviours, and (3) to explore the association between the nurse-reported PSC and characteristics of Swiss acute care hospitals. We hypothesised that there would be differences in nurse-reported PSC based on (a) hospital type (university/cantonal hospital versus regional hospitals), (b) unit type (medical versus surgical units) and (c) language regions (German- versus French- / Italian-speaking).
For this substudy we used nurse survey data from the multicentre-cross sectional Swiss-RN4CAST (Nurse Forecasting: Human Resources Planning in Nursing). The Swiss RN4CAST is part of the 12 European-country RN4CAST study funded by the EU 7th Framework (EU Project number: 223468). Using a cross-sectional design the RN4CAST assessed a number of variables, such as the nurse work environment, nurse staffing and educational level, nurse outcomes (e.g. job satisfaction, burnout) and patient outcomes (e.g., patient satisfaction, risk-adjusted in-hospital mortality) through nurse and patient surveys as well as administrative hospital and patient discharge data. The main aim of the RN4CAST study was to enrich and refine traditional nurse forecasting models with factors that take into account how features of the work environment impact on nurse retention, burnout and patient satisfaction. Thus, it allows simulation of scenarios to illustrate how changes of different nurse-related organisational factors impact on future nursing workforce needs [32].
The sample of this substudy included registered nurses (RNs) working on medical, surgical and mixed medical-surgical units in Swiss acute care hospitals. The sampling method of the Swiss RN4CAST study was a multi-stage sampling approach. In the 1st step we selected acute-care hospitals using quota sampling. For step 1 we obtained a list of all acute-care hospitals (n = 150) from the Swiss Federal Office of Public Health for the year 2005. Hospitals were eligible to participate if they had at least 60 acute care beds and employed at least 50 RNs. We aimed to include a total of at least 30 hospitals and one hospital for each language region and canton. From a total of 150 acute-care hospitals 88 (62 German-, 19 French- and 7 Italian-speaking hospitals) met our eligibility criteria. Based on the number of hospitals per language region and per canton (ranging from 1 to 14 hospitals), 41 hospitals were selected and invited to take part in the study on the basis of research group consensus. From those 41 hospitals, hospital directors and chief nursing officers from 35 hospitals (85%) agreed to participate and gave their written consent to participation in the study, anonymous benchmarking and dissemination of the study results.
In the 2nd step, a total sample of 132 units from the 35 study hospitals was included: 62 general medical, 59 general surgical units and 11 mixed medical-surgical wards (German-speaking region only). Within the participating university and cantonal hospitals units were randomly selected (n = 76 units) whereas in regional hospitals all medical/surgical wards (n = 56 units) had to be included to achieve the planned RNs sample size per hospital. In the 3rd step, within selected units all registered nurses (except those on sick leave, maternity leave or those who were on vacation) were invited to complete the questionnaires.
PSC was measured by the Safety Organising Scale (SOS) [33, see items in table 2]. The SOS measures the extent to which RNs and their colleagues engage in patient safety behaviours and practices on their unit. Its theoretical background lies in the high-risk industry and it was adapted for healthcare organisations to reflect crucial safety behavioural processes (e.g. preoccupation with failures) [33]. The SOS is a one-dimensional instrument, consisting of nine items each assessed by a 7-point Likert scale (1 = not at all, 2 = to a very limited extent, 3 = to a limited extent, 4 = to a moderate extent, 5 = to a considerable extent 6 = to a great extent and 7 = to a very great extent). The SOS score, the average of the single nine items, gives information on the prevailing PSC. The original English version of the SOS has excellent psychometric properties, such as high internal reliability (Cronbach’s alpha = 0.88), convergent validity (e.g., comparative fit index = 0.964, root mean square error of approximation = 0.055, p <0.001 for all factor loadings) and criterion validity (medication error: B = –0.678, p <0.001 and patient falls: B = –0.629, p <0.001) [33].
The SOS was translated into German, French and Italian following a forward-backward translation procedure according to the adapted Brislin’s model [34]. Psychometric evaluation according to the guidelines of the American Educational Research Association (AERA) [35] revealed evidence based on content (S-CVI >0.89), response patterns (e.g. average of missing values across all items = 0.80%), internal structure (e.g. comparative fit indices >0.90, root mean square error of approximation <0.08) and reliability (Cronbach’s alpha >0.79) for all three language versions. Intraclass correlations and within-group agreement demonstrated that the SOS is meaningful at the unit level, which justified aggregation of the individual SOS score at unit level.
The predictor variables, hospital type (university and cantonal = 1, regional = 2), unit type (surgical = 1, medical = 2, medical-surgical = 3) and language region (German-speaking = 1, French- and Italian-speaking = 2) were all categorical variables. As these three variables were inclusion criteria for the national hospital sample, data were retrieved prior and during the sampling strategy from the Swiss Federal Statistics Office (hospital types) and from the hospitals’ chief nursing officers (unit types). According to the Swiss Federal Statistics Office, university and cantonal hospitals in Switzerland are characterised by a higher number of medical specialties, with complex structures and processes, and they provide healthcare services for a larger number of patients and a larger proportion of seriously ill patients than regional hospitals [36].
Sociodemographics and professional characteristics on the participating RN included age (in years), education/training in Switzerland (0 = no, 1 = yes), employment level (10–100%), professional experience as an RN (in years) and professional experience in the hospital where they were currently working (in years) and were collected with a subscale of the nurse questionnaire which has been used in previous outcome studies [37, 38].
Data collection took place from 12 October 2009 to 30 June 2010. For each participating hospital a predefined contact person (e.g. ward nurses, clinical nurse specialists or chief nursing officers) supported us in planning and data collection. All requisite documents, including the nurse survey questionnaire and additional information on the study, were prepared at the Institute of Nursing Science (University of Basel) and sent to the contact persons in each participating hospital. They distributed the questionnaires to all eligible RNs on the selected units. The questionnaires were distributed with prepaid, addressed envelopes for return of the completed questionnaires by the RNs to the research team. Response rates were calculated for each unit, based on the number of questionnaires that were sent out by the research team and sent back by RNs. Units with response rates <70% after two weeks were reminded by the contact person to complete the questionnaires and if necessary again, to improve the response rate, four weeks after distribution of the questionnaires. Completed questionnaires were scanned and data underwent quality control (e.g., 10% of entered questionnaires were randomly selected and checked for data entry errors).
To describe the RN and hospital samples and to detect data anomalies (e.g. outliers, extreme values and missing values) descriptive analyses such as frequencies, means, standard deviations, medians, interquartile ranges, cross-tabulations and graphs were performed. As the missing value rate per item was very low (<1.9%), for descriptive and inferential analyses only SOS questionnaires with complete data were included.
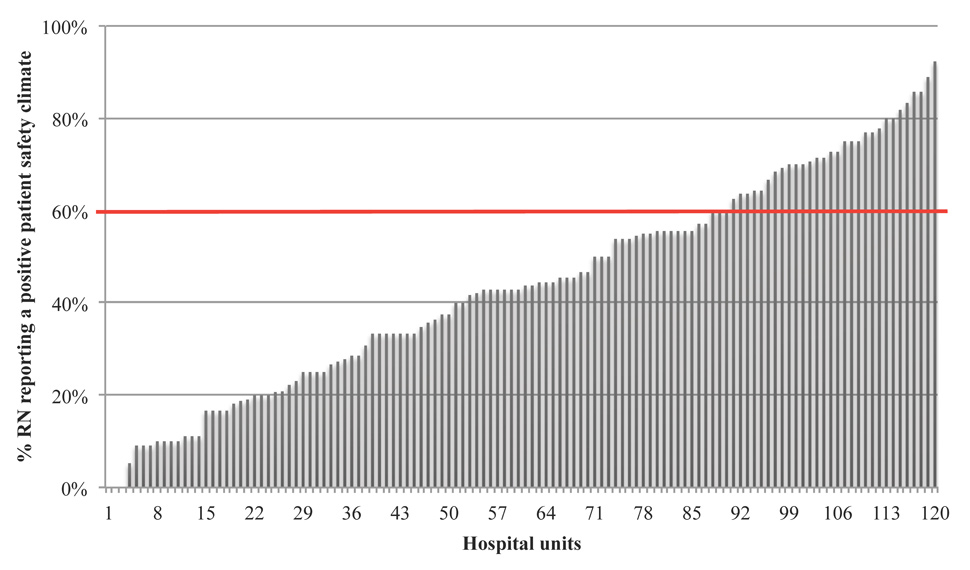
First, to describe the nurse-reported PSC on the hospital units, the SOS total score was calculated as the average of the scores on the nine items. Then the proportion of RNs who reported a positive PSC (SOS score ≥6, “to a great extent”) for their unit was calculated. In this study, units were considered to have a positive PSC if at least 60% of RNs reported an average SOS score ≥6 (consistent with engaging in the measured behaviours to a great or very great extent). Units were only included in these analyses if at least 50% of their eligible RNs completed the survey.
Second, to describe RNs’ perceptions that they and colleagues on their unit are engaged in each of the nine safety behaviours measured by the SOS, we collapsed the 7-point Likert scale to a 3-point Likert scale as follows: not at all (1) and to a very limited (2) and limited (3) extent were recoded as not engaged; to a moderate (4) and considerable (5) extent were recoded as not consistently engaged; and to a great (6) and very great (7) extent were recoded as consistently engaged. We then calculated the number and proportion of RNs who reported that they and colleagues were not engaged, not consistently engaged and consistently engaged in each of the behaviours.
Third, to test our two-sided hypothesis we used regression analyses with the SOS score as dependent variable and language region, hospital size and unit type as independent dichotomous variables (model 1) and adjusted for RN sociodemographics and professional characteristics as possible confounding variables (model 2). We adjusted for the hierarchical data structure (nurses nested within units and units nested within hospital), using multilevel linear modelling with units and hospitals as random effects (model 3). We excluded mixed medical-surgical units from the regression analysis, as they were only present in the German-speaking hospitals and data from RNs working on these units was not comparable to those from RNs working on either medical or surgical units.
The level of significance was set at p <0.05. Descriptive analyses were completed using IBM SPSS Statistics (version 18.0.2; SPSS Inc., Chicago, IL) and Microsoft Office Excel 2011®; for regression analyses we used STATA (version 11.2/SE; StataCorp LP).
The study was approved by all 13 responsible ethical committees of the respective cantons. RNs were surveyed voluntarily and they gave their consent to participate in the study by filling out and sending back the questionnaires. Measures were taken to protect the identity of the nurses and to guarantee the confidentiality of collected data (e.g. pre-coded questionnaires, prepared addressed envelopes, and questionnaires stored under lock and key).
In total, 35 hospitals from the three language regions of Switzerland participated in the RN4CAST study. The hospitals included 4 university, 15 cantonal and 16 regional hospitals varying in size from <200 to >500 acute care beds. Most of the participating hospitals were regional hospitals with fewer than 200 acute-care beds.
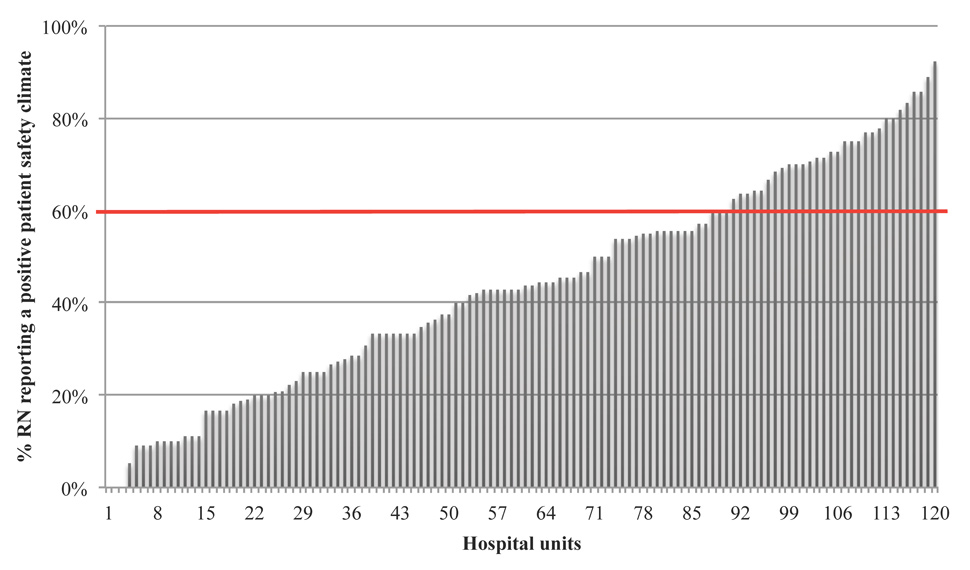
Figure 1
Unit’s patient safety climate (n = 120).
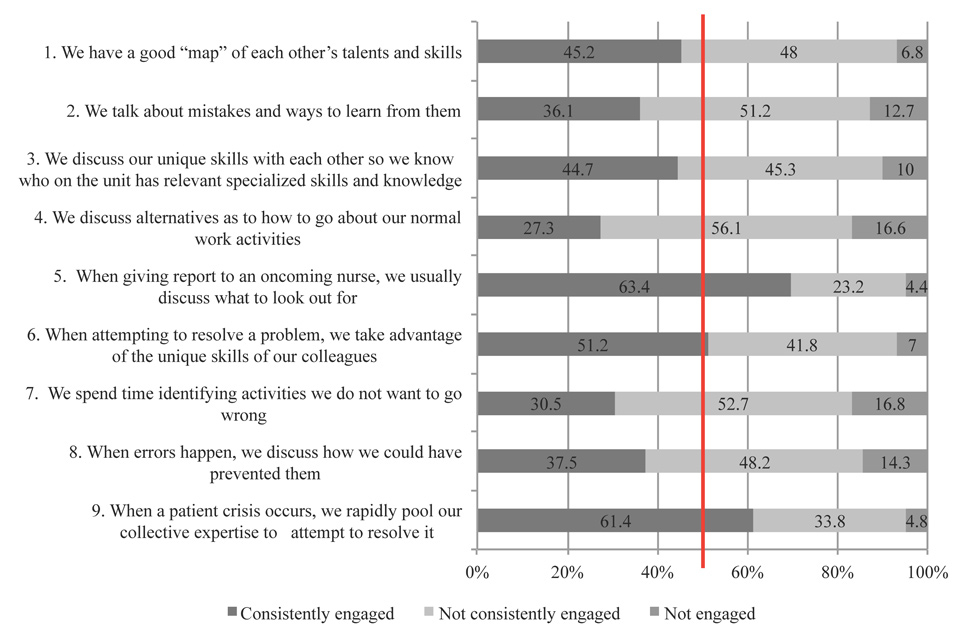
Figure 2
Frequencies (%) of the single items comparing RN’s engagement (“Consistently engaged” = answer categories 6–7, “Not consistently engaged” = answer categories 4–5, “Not engaged” = answer categoreis 1–3) in safety behaviours (n = 1,564).
A total of 1,633 RNs from 132 medical, surgical and mixed medical-surgical units completed the questionnaires, corresponding to an overall response rate of 72%. Response rates at the unit level ranged between 40% and 100%. The majority (91.7%) of RNs were female, 41.7% were aged 20–30 and almost half of the respondents (48.5%) were employed in full-time positions (working >90%). Their median years of “professional experience as a nurse” and the “professional experience as a nurse in the given hospital” were 8 years and 5 years respectively. Two thirds of the respondents (65.9%) were German-speaking. The proportion of RN working on medical units (48.4%) was slightly higher than the proportion on surgical units (44.8%) (table 1).
Most respondents (1,564 of 1,633 RNs; 95.77%) filled out the SOS without omitting items. Overall their perceptions of the extent to which their unit engagement in the listed patient safety behaviours ranged between a moderate (4) to considerable extent (5) for item 4 “We discuss alternatives as to how to go about our normal work activities” (mean = 4.62 [95% CI: 4.56–4.69]) and to a considerable (5) and great (6) extent for item 5 “When giving report to an oncoming nurse, we usually discuss what to look out for” (5.62 [95% CI: 5.57 to 5.68]). The average SOS score on the nine items was 5.11 (95% CI: 5.07–5.16) suggesting that on average RNs perceived that the behaviours measured were practised to a considerable extent on their unit (table 2).
To compare the PSC on the participant medical, surgical and mixed medical-surgical units we computed the proportion of RNs on each unit reporting a positive PSC (defined as a mean SOS score ≥6). From a total of 132 units, 120 units had a response rate >50% and were eligible for this analysis. The proportion of RNs per unit reporting a positive PSC ranged from 0% to 92.31% (mean = 43.84%, 95% CI: 39.67% to 48.01%). The RN-reported PSC was positive on only 33 out of 120 units (27.5%). For three units (2.5%) no RN reported a positive PSC (fig. 1).
Figure 2 shows the proportion of RNs who reported that they and colleagues were not engaged, not consistently engaged and consistently engaged in each of the PSC behaviours based on the collapsed SOS categories. The behaviours that the highest proportion of the participants (63.4% and 61.4% respectively) reported that they and colleagues engaged in consistently were “When giving report to an oncoming nurse, we usually discuss what to look out for” (Item 5) and “When a patient crisis occurs, we rapidly pool our collective expertise to attempt to resolve it” (Item 9). The behaviour that fewest reported engaging in consistently was “We discuss alternatives as to how to go about our normal work activities” (Item 4; 27.3% of participants).
Data from 1,456 RNs were included in regression analysis. In the two naive regression models the unit type and language regions were significantly associated with the nurse-reported PSC with (1) RNs working on medical units expressing higher PSC than RNs working on surgical units and (2) RNs from the French- and Italian-speaking language regions reporting lower PSC than RNs from the German-speaking language region (table 3). For our third variable of interest, hospital type, RNs working in regional hospitals reported higher PSC than those in university and cantonal hospitals, but the results were only borderline statistically significant (see table 3).
Adjusting also for the hierarchical data structure, considering units and hospitals as random effects (regression model 3) we found both significant between-unit variability (variance = 0.100, SE = 0.024, 95% CI: 0.062 to 0.699) and significant between-hospital variability (variance = 0.040, SE = 0.022, 95% CI: 0.014 to 0.118). In this fully adjusted model only language regions remained a significant predictor for nurse-reported PSC. When we included socio-demographic and professional characteristics as potential confounding variables (Model 2 and 3), we observed a significant negative relationship between RNs’ total years of experience in the participating hospital and PSC, but we did not find significant relationships for age, educational level, employment level or professional experience in the hospital where RNs were currently working and PSC (table 3).
| Table 1: Characteristics of hospitals and RN. | |||
| Hospital characteristics | RN4CAST hospital sample(n = 35) | Swiss acute-care hospital population* (n = 150) | |
| n (%) | n (%) | ||
| Hospitals per language region | |||
| German-speaking | 20 (57.0) | 105 (70.0) | |
| French-speaking | 11 (31.5) | 34 (22.7) | |
| Italian-speaking | 4 (11.5) | 11 (7.3) | |
| Hospital type | |||
| University hospital | 4 (11.0) | 5 (3.3) | |
| Cantonal hospital | 15 (43.0) | 23 (15.4) | |
| Regional hospital | 16 (46.0) | 122 (81.3) | |
| Hospital size | |||
| Large (>500 acute-care beds) | 6 (17.0) | 9 (7.6)** | |
| Medium (200–500 acute-care beds) | 11 (31.0) | 29 (24.4)** | |
| Small (<200 acute-care beds) | 18 (52.0) | 81 (68.0)** | |
| RN characteristics (n = 1633) | Median (IQR) | n (%) | |
| Female | 1,466 (91.7) | ||
| Age in years | |||
| 20–30 | 652 (41.7) | ||
| 31–40 | 437 (27.9) | ||
| 41–50 | 321 (20.5) | ||
| >50 | 155 (9.9) | ||
| Nursing education in Switzerland | 1275 (78) | ||
| Employment | |||
| >90% | 766 (48.5) | ||
| 51–90% | 515 (32.6) | ||
| 10–50% | 299 (18.9) | ||
| Professional experience in years, | |||
| as a nurse | 8 (15) | ||
| in this hospital | 5 (10) | ||
| RN per language region | |||
| German-speaking | 1,074 (65.9) | ||
| French-speaking | 401 (24.6) | ||
| Italian-speaking | 155 (9.5) | ||
| RN per unit type | |||
| Surgical units | 731 (44.8) | ||
| Medical units | 789 (48.4) | ||
| Mixed medical/surgical units (only German-speaking region) | 110 (6.7) | ||
| Number of RN per unit | 12 (5) | ||
| * Characteristics on the Swiss acute-care hospital population (without psychiatric and rehabilitation clinics) were retrieved from the annual hospital statistics 2005 of the Swiss Federal Office of Public Health ( http://www.bag.admin.ch/ ) ** Data available only on 109 of 150 acute-care hospitals | |||
| Table 2: Mean, 95% confidence interval (CI), standard deviation (SD), median and interquartile range (IQR), for the single nine items and the SOS score (n = 1,564). | ||
| Items of the SOS [33] | Mean (95% CI) ± SD | Median (IQR) |
| We have a good “map” of each other’s talents and skills | 5.23 (5.17 to 5.28) ± 1.073 | 5 (1) |
| We talk about mistakes and ways to learn from them | 4.92 (4.86 to 4.98) ± 1.251 | 5 (2) |
| We discuss our unique skills with each other so we know who on the unit has relevant specialised skills and knowledge | 5.13 (5.07 to 5.19) ± 1.237 | 5 (2) |
| We discuss alternatives as to how to go about our normal work activities | 4.62 (4.56 to 4.69) ± 1.270 | 5 (2) |
| When giving report to an oncoming nurse, we usually discuss what to look out for | 5.62 (5.57 to 5.68) ± 1.071 | 6 (1) |
| When attempting to resolve a problem, we take advantage of the unique skills of our colleagues | 5.30 (5.25 to 5.36) ± 1.154 | 6 (1) |
| We spend time identifying activities we do not want to go wrong | 4.71 (4.64 to 4.77) ± 1.330 | 5 (2) |
| When errors happen, we discuss how we could have prevented them | 4.91 (4.84 to 4.97) ± 1.305 | 5 (2) |
| When a patient crisis occurs, we rapidly pool our collective expertise to attempt to resolve it | 5.58 (5.53 to 5.64) ± 1.060 | 6 (1) |
| SOS-score | 5.11 (5.07 to 5.16) ± 0.913 | 5 (1) |
| Table 3: Association between the nurse-reported PSC and characteristics of Swiss acute care hospitals (n = 1,456). | ||||||
| Variables | Model 1 (naive, unadjusted) | Model 2 (naive, adjusted) | Model 3 (multilevel, adjusted) | |||
| Coefficient (p) | 95% CI | Coefficient (p) | 95% CI | Coefficient (p) | 95% CI | |
| Hospital type* | 0.093 (0.059) | –0.004 to 0.189 | 0.091 (0.065) | –0.006 to 0.187 | 0.125 (0.230) | –0.079 to 0.329 |
| Unit type# | 0.104 (0.025) | 0.013 to 0.195 | 0.101 (0.030) | 0.009 to 0.193 | 0.070 (0.346) | –0.076 to 0.217 |
| Language region+ | –0.434 (<0.001) | –0.526 to –0.342 | –0.436 (<0.001) | –0.529 to –0.343 | –0.428 (<0.001) | –0.630 to -0.227 |
| RN age – in years | 0.001 (0.552) | –0.001 to 0.003 | 0.0001 (0.947) | –0.002 to 0.002 | ||
| RN education° | –0.001 (0.597) | –0.170 to 0.068 | –0.002 (0.507) | –0.006 to 0.003 | ||
| Employment level – % | –0.0003 (0.575) | –0.001 to 0.002 | 0.0003 (0.676) | –0.001 to 0.002 | ||
| RN professional experience (total) – in years | –0.003 (0.017) | –0.010 to -0.001 | –0.003 (0.029) | –0.005 to –0.0003 | ||
| RN professional experience (hospital currently working) – in years | 0.002 (0.150) | –0.001 to 0.005 | 0.002 (0.163) | –0.001 to 0.005 | ||
| Constant | 5.441 (<0.001) | 5.210 to 5.671 | 5.409 (<0.001) | 5.152 to 5.666 | 5.433 (<0.001) | 4.952 to 5.915 |
| * Hospital type: university and cantonal hospitals versus regional hospitals # Unit type: surgical units versus medical units + Language region: German-speaking region versus French- and Italian-speaking region ° RN education: education in Switzerland versus education outside Switzerland | ||||||
This is the first study to describe the nurse-reported PSC in a representative national sample of Swiss acute care hospitals. We observed variability in the extent to which RNs reported that they and colleagues engage in the individual safety behaviours measured and the PSC climate across units and hospitals. The three items that the RNs reported they and colleagues consistently engaged in reflected safety behaviours such as nurses’ shift reports and the use of one another’s skills and expertise in critical situations and in resolving problems in patient care. As more than half of the participating RNs reported that personnel of their units consistently engaged in these activities (SOS score ≥6, consistent with “to a great extent”), it may be that these are implicit safety behaviors that are seen as part of their daily business in preventing/protecting patients from harm. Furthermore, results on the use of one another’s skills and expertise in critical situations and in resolving problems (items six and nine) suggest good interprofessional relations and communication among RNs and physicians, essential for high levels of patient safety and quality of care [39].
However, in our sample a high proportion of RNs reported that they and colleagues did not or did not consistently engage in six out of the nine behaviours. Those items reflect important patient safety behaviours such as proactive and preemptive analysis and discussion of possible unexpected events, ability to detect and learn from errors and critical thinking about normal, everyday work activities/processes. Learning from errors and near misses is crucial for patient safety and over the last several years many European countries including Switzerland have invested in patient safety measures, methods and instruments. For example, Critical Incident Reporting Systems (CIRS) have been implemented in healthcare systems [40–43]. However, for the benefits of such well-meant systems to be realized, healthcare professionals must be willing to report and share errors [44], which is known to be problematic. In one study, for example, RNs reported only half of the medication errors that occurred [45]. Despite a blame-free and non-punitive environment [45] the functioning and success of CIRS might depend also on healthcare professionals’ individual capabilities and skills in detecting, reporting, analysing and learning from errors. To strengthen these individual skills and to increase willingness to report and share errors on systemic levels, creating a “positive” PSC at unit level by implementation of appropriate activities, such as root cause analysis, is necessary [46].
In addition to processes responding to errors that occur, proactive analyses of unexpected events and critical analysis of existing work activities/processes are important to avoid errors. The results of our study suggest that these behaviours are not yet “implicit behaviours” to the same extent as other safety behaviours measured by the SOS. Activities addressing these proactive behaviors that have been reported in the scientific literature include tools such as patient safety leadership walking rounds [47], safety briefings [48] and Healthcare Failure Mode and Effect Analysis (HFMEA™) [49]. Such prospective methods, aiming to stimulate healthcare professionals’ safety awareness and to identify and prevent process problems before they occur, may not yet be extensively implemented in Swiss acute care hospitals.
The fact that the majority of RNs reported that they and colleagues did not consistently engage in six out of the nine SOS safety behaviours was also reflected in a low proportion of units with an overall positive PSC. Given that previous research has shown that units and hospitals with a lower PSC have higher rates of AEs, such as medication errors and patient falls [33, 50, 51], these findings should encourage Swiss hospitals to improve their PSC.
Our hypothesis, that there would be differences in nurse-reported PSC based on (a) hospital type, (b) unit type and (c) language regions, was only partially supported, as in our multilevel model only language region significantly related to variability in the nurse-reported PSC. The higher nurse-reported PSC in the German-speaking region could be related to the implementation of several initiatives on patient safety in recent years, such as the “Critical Incident Reporting and Reacting NETwork (CIRRNET)“ in 24 hospitals [52], initiated by the Swiss patient safety foundation first in the German-speaking language region of Switzerland. Recently, CIRRNET and other important initiatives (e.g., “Error & Risk Analysis”) are being extended to the Italian- and French-speaking regions or initiated at national level [52] and may contribute to improvement in PSC at the unit level. In our naïve regression models we found that (1) RNs on surgical units reported lower PSC than nurses on medical units and (2) RN working in regional hospitals expressed higher perceptions of their unit’s PSC than RNs working in cantonal and university hospitals. These results might indicate that greater complexity of structures (university and cantonal hospitals) and a large number of interfaces in the care processes (e.g. peri- and post-operative care) might have a negative impact on the PSC, as it is more difficult for health care professionals, such as RNs, to guarantee patient safety in such environments. However, after statistical adjustment for the nested data structure, these relationships were no longer significant. These results indicate that the PSC variability between units and between hospitals is in general higher than the variability between medical or surgical units and between university/cantonal or regional hospitals.
Even though this study allowed us to form a picture of nurse-reported PSC in the acute care setting, there are some limitations/precautions to consider. The RN4CAST study used a cross-sectional study design, which does not allow assessment of causal relationships between study variables. Since we have not used randomised sampling techniques in all stages of our sampling process, this increases the risk of bias. External validity is restricted to general medical, surgical and mixed medical-surgical units in Swiss acute care hospitals. Since we only included acute-care hospitals with 60 or more beds to achieve a sample size of at least 50 RNs per hospital, regional hospitals were relatively underrepresented in contrast to the total hospital population.
The SOS gives important information on crucial patient safety behaviours and processes at unit level, but other aspects of PSC such as management support for patient safety engagement or a blame-free environment [11, 30] are not measured with the SOS. Hence the SOS may not present a complete picture of the PSC. As the RN4CAST study included only RNs, the PSC perceptions of other healthcare professionals, e.g. physicians, were not captured.
The results of this study provide initial insights on RNs’ perceptions of the extent to which they and colleagues engage in patient safety behaviours and the prevailing PSC on general medical, surgical and mixed medical-surgical units in a national sample of Swiss acute care hospitals. Despite the increasing awareness of patient safety in Switzerland in recent years, our findings show variability in RNs’ perceptions of safety behaviours, as well as significant variability in the prevailing PSC between units, hospitals and language regions, and indicate the potential for improvement. Hospital leaders at various levels should strengthen the PSC at the unit level and support/foster healthcare professionals’ engagement in safety behaviors by implementing safety methods such as root cause analysis, patient safety leadership walk rounds or safety briefings and de-briefings. This could, in turn, improve individual and team skills and awareness concerning discussions on errors, proactive and critical analyses of possible unexpected events and work processes, improve adherence to CIRS and, most importantly, result in better patient safety outcomes. The regular measurement of PSC by the SOS allows evaluation of the impact of implementing such activities and provides a means for ongoing monitoring of the prevailing PSC within hospitals. Linking the PSC with other structural and process indicators (e.g., staffing level, skill mix, leadership abilities, implicit rationing of nursing care) could lead to a better understanding of the complex relationships that impact on the quality of patient care.
Acknowledgements: The authors thank all hospital nursing directors, nurses and patients for participating in the RN4CAST study. Special thanks are due to Mario Desmedt (scientific collaborator RN4CAST) for fruitful discussions, Tracy Glass, PhD (Biostatistician) for her statistical support and Natascha Natum (administrative collaborator RN4CAST) and the key persons in the hospital, for their major efforts during the data collection process.
1 Zegers M, de Bruijne MC, Wagner C, Hoonhout LH, Waaijman R, Smits M, et al. Adverse events and potentially preventable deaths in Dutch hospitals: results of a retrospective patient record review study. Qual Saf Health Care. 2009;18(4):297–302.
2 Aranaz-Andres JM, Aibar-Remon C, Vitaller-Burillo J, Requena-Puche J, Terol-Garcia E, Kelley E, et al. Impact and preventability of adverse events in Spanish public hospitals: results of the Spanish National Study of Adverse Events (ENEAS). Int J Qual Health Care. 2009;21(6):408–14.
3 Soop M, Fryksmark U, Koster M, Haglund B. The incidence of adverse events in Swedish hospitals: a retrospective medical record review study. Int J Qual Health Care. 2009;21(4):285–91.
4 Baker GR, Norton PG, Flintoft V, Blais R, Brown A, Cox J, et al. The Canadian Adverse Events Study: the incidence of adverse events among hospital patients in Canada. CMAJ. 2004;170(11):1678–86.
5 Vincent C, Neale G, Woloshynowych M. Adverse events in British hospitals: preliminary retrospective record review. BMJ. 2001;322(7285):517–9.
6 Thomas EJ, Studdert DM, Burstin HR, Orav EJ, Zeena T, Williams EJ, et al. Incidence and types of adverse events and negligent care in Utah and Colorado. Med Care. 2000;38(3):261–71.
7 Institute of Medicine. Patient safety. Achieving a new standard for care. series QC, editor. Washington D.C.: The National Academies Press; 2004.
8 Vincent C. Understanding and responding to adverse events. N Engl J Med. 2003;348(11):1051–6.
9 Vincent C, Aylin P, Franklin BD, Holmes A, Iskander S, Jacklin A, et al. Is health care getting safer? BMJ. 2008;337:a2426.
10 Reason J. The Human Contribution. Unsafe Acts, accidents and heroic recoveries. Burlington, Surrey: Ashgate; 2008.
11 Feng X, Bobay K, Weiss M. Patient safety culture in nursing: a dimensional concept analysis. J Adv Nurs. 2008;63(3):310–9.
12 Ashkanasy N, Broadfoot L, Falkus S. Questionnaire measures of organizational culture. In: Ashkanasy N, Wilderom C, Peterson M, editors. Handbook of organizational culture and climate. Thousand Oaks, CA: Sage; 2000.
13 Hartmann CW, Meterko M, Rosen AK, Shibei Z, Shokeen P, Singer S, et al. Relationship of hospital organizational culture to patient safety climate in the Veterans Health Administration. Med Care Res Rev. 2009;66(3):320–38.
14 Pringle J, Weber RJ, Rice K, Kirisci L, Sirio C. Examination of how a survey can spur culture changes using a quality improvement approach: A region-wide approach to determining a patient safety culture. Am J Med Qual. 2009;24(5):374–84.
15 Hellings J, Schrooten W, Klazinga N, Vleugels A. Challenging patient safety culture: survey results. Int J Health Care Qual Assur. 2007;20(7):620–32.
16 Nicklin W, Mass H, Affonso DD, O’Connor P, Ferguson-Pare M, Jeffs L, et al. Patient safety culture and leadership within Canada's academic health science centres: towards the development of a collaborative position paper. Nurs Leadersh (Tor Ont). 2004;17(1):22–34.
17 Singer SJ, Hartmann CW, Hanchate A, Zhao S, Meterko M, Shokeen P, et al. Comparing safety climate between two populations of hospitals in the United States. Health Serv Res. 2009;44(5 Pt 1):1563–83.
18 Singer SJ, Falwell A, Gaba DM, Baker LC. Patient safety climate in US hospitals: variation by management level. Med Care. 2008;46(11):1149–56.
19 Singer SJ, Gaba DM, Falwell A, Lin S, Hayes J, Baker L. Patient safety climate in 92 US hospitals: differences by work area and discipline. Med Care. 2009;47(1):23–31.
20 Hartmann CW, Rosen AK, Meterko M, Shokeen P, Zhao S, Singer S, et al. An overview of patient safety climate in the VA. Health Serv Res. 2008;43(4):1263–84.
21 Kho ME, Perri D, McDonald E, Waugh L, Orlicki C, Monaghan E, et al. The climate of patient safety in a Canadian intensive care unit. J Crit Care. 2009;24(3): 469 e467–413.
22 France DJ, Greevy RA, Jr., Liu X, Burgess H, Dittus RS, Weinger MB, et al. Measuring and comparing safety climate in intensive care units. Med Care;48(3):279–84.
23 Huang DT, Clermont G, Sexton JB, Karlo CA, Miller RG, Weissfeld LA, et al. Perceptions of safety culture vary across the intensive care units of a single institution. Crit Care Med. 2007;35(1):165–76.
24 Kaafarani HM, Itani KM, Rosen AK, Zhao S, Hartmann CW, Gaba DM. How does patient safety culture in the operating room and post-anesthesia care unit compare to the rest of the hospital? Am J Surg. 2009;198(1):70–5.
25 Scherer D, Fitzpatrick JJ. Perceptions of patient safety culture among physicians and RNs in the perioperative area. AORN J. 2008;87(1):163–75.
26 Makary MA, Sexton JB, Freischlag JA, Millman EA, Pryor D, Holzmueller C, et al. Patient safety in surgery. Ann Surg. 2006;243(5):628–32; discussion 32-5.
27 Carney BT, Mills PD, Bagian JP, Weeks WB. Sex differences in operating room care giver perceptions of patient safety: a pilot study from the Veterans Health Administration Medical Team Training Program. Qual Saf Health Care. 2010;19(2):128–31.
28 Smits M, Wagner C, Spreeuwenberg P, van der Wal G, Groenewegen PP. Measuring patient safety culture: an assessment of the clustering of responses at unit level and hospital level. Qual Saf Health Care. 2009;18(4):292–6.
29 Saturno PJ, Da Silva Gama ZA, de Oliveira-Sousa SL, Fonseca YA, de Souza-Oliveira AC, Grupo Proyecto Indicadores de Seguridad del P, et al. [Analysis of the patient safety culture in hospitals of the Spanish National Health System]. Med Clin (Barc). 2008;131(Suppl 3):18–25.
30 Pfeiffer Y, Manser T. Development of the German version of the hospital survey on patient safety culture: Dimensionality and psychometric properties. Safety Science. 2010;48(10):1452–62.
31 Hughes LC, Chang Y, Mark BA. Quality and strength of patient safety climate on medical-surgical units. Health Care Manage Rev. 2009;34(1):19–28.
32 Sermeus W, Aiken LH, Van den Heede K, Rafferty AM, Griffiths P, Moreno-Casbas MT, et al. Nurse Forecasting in Europe (RN4CAST): Rationale, design and methodology. BMC Nurs. 2011;10(1):6.
33 Vogus TJ, Sutcliffe KM. The Safety Organizing Scale: development and validation of a behavioral measure of safety culture in hospital nursing units. Med Care. 2007;45(1):46–54.
34 Jones PS, Lee JW, Phillips LR, Zhang XE, Jaceldo KB. An adaptation of Brislin's translation model for cross-cultural research. Nurs Res. 2001;50(5):300–4.
35 American Educational Research Association. Standards for Educational and Psychological Testing1999.
36 Swiss Federal Statistical Office. Krankenhaustypologie. Statistik der stationären Betriebe des Gesundheitswesens. 2006; Available from: http://www.bfs.admin.ch/bfs/portal/de/index/infothek/erhebungen__quellen/blank/blank/kh/02.parsys.0893.downloadList.92145.DownloadFile.tmp/typologieks200611v52afrdv20.pdf
37 Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288(16):1987–93.
38 Schubert M, Glass TR, Clarke SP, Aiken LH, Schaffert-Witvliet B, Sloane DM, et al. Rationing of nursing care and its relationship to patient outcomes: the Swiss extension of the International Hospital Outcomes Study. Int J Qual Health Care. 2008;20(4):227–37.
39 Martin JS, Ummenhofer W, Manser T, Spirig R. Interprofessional collaboration among nurses and physicians: making a difference in patient outcome. Swiss Med Wkly. 2010;140:w13062.
40 Andersen PO, Maaloe R, Andersen HB. Critical incidents related to cardiac arrests reported to the Danish Patient Safety Database. Resuscitation. 2010;81(3):312–6.
41 Dominguez Fernandez E, Kolios G, Schlosser K, Wissner W, Rothmund M. Introduction of a critical incident reporting system in a surgical university clinic. What can be achieved in a short term?. Dtsch Med Wochenschr. 2008;133(23):1229–34.
42 Tighe CM, Woloshynowych M, Brown R, Wears B, Vincent C. Incident reporting in one UK accident and emergency department. Accid Emerg Nurs. 2006;14(1):27–37.
43 Wingenfeld C, Abbara-Czardybon M, Arbab D, Frank D. Patient safety in orthopaedics: implementation and first experience with CIRS and team time-out. Z Orthop Unfall. 2010;148(5):525–31.
44 Mahajan RP. Critical incident reporting and learning. Br J Anaesth. 2010;105(1):69–75.
45 Chiang HY, Lin SY, Hsu SC, Ma SC. Factors determining hospital nurses’ failures in reporting medication errors in Taiwan. Nurs Outlook. 2010;58(1):17–25.
46 Taitz J, Genn K, Brooks V, Ross D, Ryan K, Shumack B, et al. System-wide learning from root cause analysis: a report from the New South Wales Root Cause Analysis Review Committee. Qual Saf Health Care. 2010;19(6):e63.
47 Thomas EJ, Sexton JB, Neilands TB, Frankel A, Helmreich RL. The effect of executive walk rounds on nurse safety climate attitudes: a randomized trial of clinical units[ISRCTN85147255] [corrected]. BMC Health Serv Res. 2005;5(1):28.
48 Menendez MD, Martinez AB, Fernandez M, Ortega N, Diaz JM, Vazquez F. Walkrounds and briefings in the improvement of the patient safety. Rev Calid Asist. 2010;25(3):153–60.
49 Kessels-Habraken M, De Jonge J, Van der Schaaf T, Rutte C. Prospective risk analysis prior to retrospective incident reporting and analysis as a means to enhance incident reporting behaviour: a quasi-experimental field study. Soc Sci Med. 2010;70(9):1309–16.
50 Mardon RE, Khanna K, Sorra J, Dyer N, Famolaro T. Exploring relationships between hospital patient safety culture and adverse events. J Patient Saf. 2010;6(4):226–32.
51 Vogus TJ, Sutcliffe KM. The impact of safety organizing, trusted leadership, and care pathways on reported medication errors in hospital nursing units. Med Care. 2007;45(10):997–1002.
52 Patient Safety Foundation. Annual report 2009. Available from: http://www.patientensicherheit.ch/dms/de/ueber-uns/1114_jahresbericht_2009_d/x1114_jahresbericht_2009_d.pdf
Funding / potential competing interests: None of the authors has a conflict of interest regarding this substudy. The research leading to these results has received funding from the European Union’s Seventh Framework Programme (FP7/2007-2013) under grant agreement n° 223468. For more information on the RN4CAST project, please visit http://www.rn4cast.eu .