Psychosocial stress and cardiovascular risk – current opinion
DOI: https://doi.org/10.4414/smw.2012.13502
Summary
Cardiovascular disease (CVD) is a major cause of morbidity and mortality worldwide. Epidemiologic research of the last half-century has clearly shown that psychosocial factors related to the social environment, personality characteristics, and negative affect increase the risk of incident CVD and also impact prognosis of cardiac patients. Several mechanisms may explain this link, including a genetic predisposition, poor lifestyle choices, low adherence to health recommendations, and direct pathophysiologic perturbations. The latter include alteration of the hypothalamic-pituitary adrenal axis and autonomic dysfunction resulting in endothelial dysfunction, inflammation, and a prothrombotic state further downstream. Screening for psychosocial factors seems appropriate as part of the standard history and based on the clinician's knowledge of the patient and the purpose of the visit. Psychological interventions generally alleviate distress in cardiac patients, but whether they reduce the risk of hard cardiovascular endpoints and all-cause mortality is less evident. Cardiac patients with more severe depression may particularly profit from antidepressant medications. Due to their pharmacologic properties, selective serotonin reuptake inhibitors were shown to improve cardiovascular outcome. The most effective psychosocial treatment is multicomponent therapy that combines elements of cognitive behaviour therapy (“stress management”) and changes in health behaviours, including the adoption of a regular exercise regimen. Gender-specific issues should probably be considered. The field of behavioural cardiology has accumulated a wealth of epidemiological, mechanistic and clinical knowledge that undoubtedly has furthered our understanding about the important role of psychosocial risk factors in patients with a heart disease.
Introduction
Cardiovascular disease (CVD) continues to be the most frequent cause of mortality in developed as well as in low/mid income countries. For instance, 37.4% of Swiss deaths in 2005 were due to CVD, whereby coronary heart disease (CHD) (15.3%), including myocardial infarction (MI), cerebrovascular disease (6.7%), and other heart diseases (8.2%), including chronic heart failure (CHF), presented the most frequent death causes [1]. Several modifiable risk factors for CVD explain about half of the risk of CVD. Findings from the world-wide conducted INTERHEART case-control study suggest that an additional one third of the population attributable risk of MI can be assigned to psychosocial factors, including major life events, lack of control over life, depression, as well as stress at work, in the family, and with financial issues [2]. Numerous prospective studies have demonstrated that psychosocial factors may contribute to incident CVD and impact prognosis in patients with manifest CVD [3]. The majority of this research refers to CHD events and outcomes. However, the importance of psychosocial factors for both quality of life and prognostic outcome is also increasingly acknowledged in patients with heart failure [4] and in those who underwent cardiac interventions such as coronary bypass surgery [3] and implantation of a cardioverter defibrillator [5]. The prevalence of takotsubo cardiomyopathy (i.e., the “broken heart syndrome”) in patients clinically presenting with a putative MI is typically observed in the wake of intense emotional stress, whereby a spillover of stress hormones seems to literally stun the myocardium [6]. Even though the stressed heart patient is the focus of this literature, it should not be forgotten that stress levels are also high in partners who have to adapt to new challenges they face as a consequence of the patient’s CVD [7].
This article aims to provide an overview on the role psychosocial risk factors and stress play in CVD, with a particular focus on CHD. However, it is out of the scope of this article to provide a systematic review and meta-analysis on epidemiologic, mechanistic and clinical aspects of psychosocial stress in CVD, but to rather highlight important concepts and up-todate discussions that have emerged from the ever-increasing literature on this topic. For instance, by September 2009, there already was an impressive number of 130 prospective studies from 87 cohorts examining depression as a predictor of risk of incident CHD or poor prognosis in patients with established CHD. Each of these cohorts studied more than 500 participants and all used established measures of depression. This literature has been summarised in at least 200 editorials, review articles, and meta-analyses [8].
A scientific understanding of “stress” for behavioural cardiology
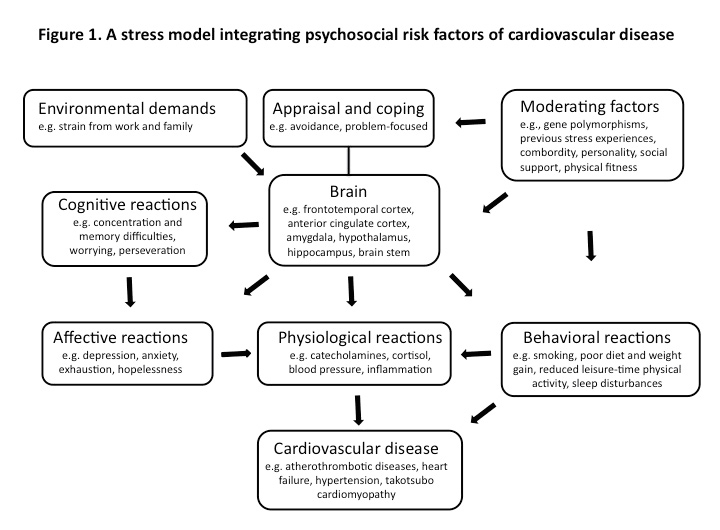
Stress is a vague term for many clinicians and patients alike. The ostensible lack of operationalisation of “stress” as opposed to laboratory cut-off measure based definitions of CVD risk factors like hypertension and dyslipidemia is one important reason for why knowledge from behavioural cardiology is still struggling these days to make its way in clinical routine. Moreover, the terms “stress” and “psychosocial factor” are sometimes used as if they were mutually exchangeable. This experience calls for a delineation of a scientific concept of stress that is presented in figure 1.
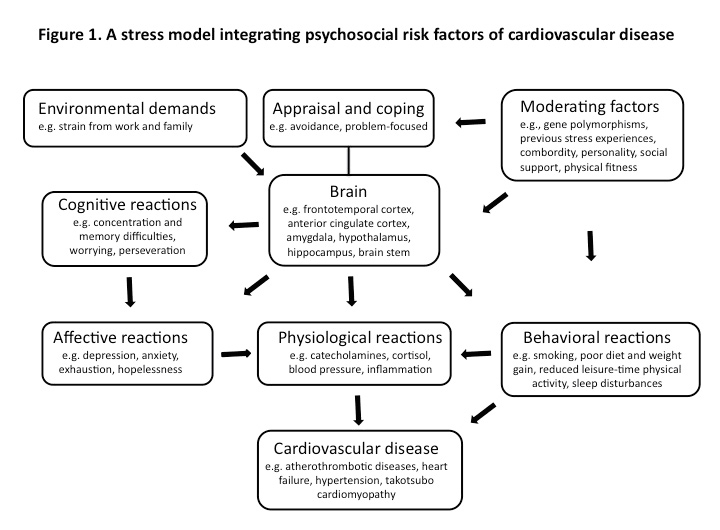
Figure 1
Depending on appraisal, coping resources, and several moderating factors, environmental demands trigger a neurobiologically driven stress reaction across cognitive, affective, behavioural, and physiological domains, all contributing directly and/or indirectly to cardiovascular disease.
Clearly, a distinction should be made between demanding environmental situations termed “stressors”, a person’s perception of such situations in the form of “distress”, and the person’s situational response termed “stress reaction” [9]. As a consequence of differences in the genetic make-up, personality, social support, and other moderating variables of stress perception and response, not all individuals are equally vulnerable to experience distress and harmful stress reactions during times of increased demands [10]. Moreover, life circumstances attain the status of psychosocial stressors if a person perceives an amount of threat and challenge that he or she appraises to overwhelm coping resources [11]. The accompanying neurobiological, neuroendocrine and autonomic activation patterns shape the stress response to elicit a wide range of initially adaptive cognitive, affective, behavioural and physiological changes in an attempt to maintain homeostasis. However, if exaggerated or sustained, stress reactions may become maladaptive, thereby bringing forward cognitive impairment and dysfunctional cognitions, negative affect, poor life style habits, and biological changes pertinent to CVD [12]. The delineated stress concept purports an integrated model of psychosocial risk factors of CVD as each of these can seamlessly be assigned to either one level of the outlined cascade leading from “stressors” to “distress” and eventually “stress reactions”. Based on this model, clinicians who are not behavioural specialists may better understand why for instance not only negative life events (e.g., unemployment, partner loss) but also negative affect like depression and hopelessness, which may arise from stressful events, have emerged as risk factors of CVD in their own right [3].
Psychosocial risk factors of cardiovascular disease
General lessons learned
Didactically, psychosocial risk factors for the initiation and progression of atherothrombotic CVD can be categorised into three domains referring to the social environment, personality traits, and negative affect (table 1). In addition, intense negative affect, such as anger and depression, as well as traumatic stress experiences related to natural disasters and war-related activities have clearly been shown to trigger acute coronary syndromes as well as fatal arrhythmias and sudden death, particularly in patients with preexisting atherosclerosis [13, 14].
Psychosocial factors co-occur with CVD at rates that exceed co-morbidity by chance. As an example, 40% of patients with CHD have a clinically relevant form of depression, whereas the prevalence of depression in the general population is 5–10%. The World Health Organization projects that in the year 2030 depression and CHD will rank among the three leading causes of global burden of disease [15]. Because of the apparent link between depression and CVD, some experts recommend that burden of disease estimates should include major depressive disorder as a risk factor for CHD [16].
Psychosocial risk factors often co-occur in the same cardiac patient (e.g., depression and low social support or job stress and exhaustion). Nonetheless, when applying factor analysis, the individual constructs are generally maintained, suggesting they constitute distinct psychological concepts [17]. Psychosocial risk factors also co-occur with many of the traditional risk factors for CVD, understandably so because part of an individual’s chronic response to stress may result in poor health behaviors and metabolic perturbations (fig. 1). Accordingly, several psychosocial factors discussed here have been associated with the development of the metabolic syndrome that is a strong predictor of CHD [18]. Individual components of the metabolic syndrome such as elevated fasting glucose and insulin sensitivity have also been associated with psychosocial factors, including hostility and anger-proneness [19, 20].
In epidemiologic studies, psychosocial risk factors and traditional CVD risk factors seem to equally strong predict cardiac risk, whereby the total cardiac risk of an individual patient is reflected by the additive effect of the sum of psychosocial and traditional CVD risk factors [21]. Although sometimes attenuated when statistically controlled for traditional cardiovascular risk factors, many studies found the link between psychosocial risk factors and an increased risk of CVD to be partly independent of demographic factors, hypertension, adiposity, diabetes, smoking, and physical activity. There is evidence for a gender aspect in that among women relative to men, depression and stress from family relationships seem more consistently associated with elevated CHD risk than hostility and job stress [22].
|
Table 1: Categories of psychosocial risk factors of cardiovascular disease. |
|
Social environment
|
Personality
|
Negative affect
|
| Low socioeconomic status |
Anger-proneness |
Depression |
| Life events, incl. adverse childhood experiences |
Hostility |
Anxiety |
| Family stress |
Type D personality |
Exhaustion |
| Job stress |
Neuroticism |
Hopelessness |
| Low social support |
Overcommitment to work |
Bereavement |
Social environment
Socioeconomic status: Low socioeconomic status (SES) as defined by low level of education, occupational position, and income is associated with shortened life expectancy and there is a particularly strong social gradient in CHD risk [23]. Moreover, those with a low SES are 1.7-times more likely to have a stroke with traditional vascular risk factors only explaining part of this risk [24]. Rather, lack of autonomy and low social participation of those low in their social hierarchy explain the social gradient in cardiovascular health [23]. This notion is supported by the observation that mortality from CHD is greatest in countries with the greatest income inequality to suggest a process of social comparison between people plays a role in CVD in wealthy and poor areas of the world [25].
Life events: The Copenhagen City Heart Study found a 1.4-fold and 1.5-fold increased risk of incident stroke (but not of MI) for more than one event in childhood and adulthood, respectively. There also was a dose-response relationship between accumulated major life events and stroke risk [26]. In a retrospective cohort survey on more than 17,000 individuals, adverse childhood experiences like sexual abuse, neglect, and household dysfunction increased the risk to develop CHD in adult life by 1.5-fold. The CHD risk was even 3.6-fold increased when seven or more adversities had been experienced during childhood. Depressive mood and anger-proneness appeared to be more important mediators of this relationship than traditional CVD risk factors [27].
Family stress: The Stockholm Female Coronary Risk Study followed up on women with an acute coronary syndrome for five years and found marital stress to be associated with a 2.9-fold increased risk of a recurrent coronary event after adjustment for age, SES, traditional CVD risk factors, cardiac function, and estrogen status [28]. Stress related to family strain is also pertinent to informal caregivers. Compared with women with no caregiving responsibilities, women providing care for at least nine hours per week to a disabled or ill spouse had a 1.8-fold higher risk of incident CHD during four years of follow-up when controlling for age and a range of CHD risk factors [29]. Caregiver burden is associated with elevated levels of psychological distress, whereby greater depressive symptoms and distress from patient problem behaviours shortened the time to onset of CVD over an 18-month period in spousal dementia caregivers [30]. In turn, relative to a wait list control condition, video-based coping skills training combined with telephone coaching calls decreased depressive symptoms, anxiety and perceived stress, as well as resting blood pressure in caregivers of a relative with Alzheimer’s disease [31].
Job stress:In addition to perceived injustice at work through for instance intransparent decision-making and unfairness by supervisors, two models of stress at work have gained particular attention as they allow clinicians and researchers alike to operationalise the relationship between work characteristics and CVD risk. Firstly, the job strain model postulates that a combination of high psychological demands with low control at work is a stressful experience. Low social support from supervisors or coworkers increases overall strain at the workplace [32]. Psychological demands include high workload and time constraints, while low decision latitude comprises a person’s inability to influence his or her own work. Secondly, the effort-reward imbalance model posits that an inequity between high effort spent and low rewards received in the form of wages, career opportunities and recognition creates a distressful work environment [33]. Overcommitted workers are particularly prone to experience effort-reward imbalance as they put themselves under time pressure and fail to sufficiently withdraw from working obligations. A previous meta-analysis of 14 prospective cohort studies with more than 100,000 employees found an approximately 1.5-fold higher adjusted relative risk of incident CHD for high versus low job strain, for a combination of high efforts and low rewards, and for organisational injustice at work [34]. Although still few in numbers, studies suggest that job stress also adversely impacts post-MI prognosis in male and female workers [35]. The relationship between job stress and CVD risk seems stronger in men than in women and in younger than in older workers (i.e., those >55 years of age). The latter may reflect a healthy worker survivor effect as the less healthy workers might develop CVD outcomes earlier.
Social support:Two broad domains of social support are commonly distinguished. Functional support refers to the aid and encouragement that is provided to a person by the social network; important subcategories are instrumental support (e.g., help getting tasks done) and emotional support (e.g., feelings of being loved). Structural support refers to the characteristics of the network of people surrounding a person and his/her interaction with this network. Important aspects are the number and frequency of contacts. Performing a meta-analysis of totally 25 prospective studies, we found low functional support – but not low structural support – to be associated with an increased risk of incident CHD [36]. In patients with manifest CHD, low functional support increased the risk of cardiac and all-cause mortality by 1.6-fold, even after adjustment for other prognostic factors. The data on the prognostic impact of structural support in CHD patients were comparably less conclusive [36]; however, some studies suggest that low structural support is also associated with increased cardiovascular mortality in CHD patients [37]. Low social support is a psychosocial risk factor of CVD in its own right, but there are likely complex interactions between social support and other psychosocial risk factors [38].For instance, individuals acting hostile in relationships and depressed patients who withdraw themselves from social participation seem less able to profit from “stress buffering” supportive environments and, therefore, may show more intense stress reactions.
Personality
Anger-proneness and hostility: Anger-proneness and hostility have emerged as the two “cardiotoxic” components of the type A coronary-prone behaviour pattern that was originally described in the 1950s [39]. Individuals with a Type A personality were typically characterised as being highly ambitious, aggressive, hostile, competitive, and under constant time pressure. Interestingly enough, the aforementioned personality style of overcommitment of a person to his/her work is characterised by traits that apparently overlap with Type A behaviour.
Hostility can primarily be viewed as a cognitive attitude of cynical and suspicious thinking about others, whereas anger describes variously intense states of negative affect. It seems didactically helpful to distinguish “anger-proneness” as a personality trait from “anger” as a negative affect. Hostility and anger-proneness show important differences, but are often used interchangeably, as the affective and behavioural components of hostility may include for instance angry feelings and verbal aggressiveness, respectively. Meta-analyses have taught us that, while Type A personality can no longer be claimed as a risk factor of CHD [40], there is now convincing evidence for anger-proneness and hostility to predict CHD outcomes with a 1.2-fold increased risk in healthy individuals and in those with established CHD [41]. The association between anger and anger-proneness, respectively, and CHD risk can be observed across different anger constructs, including outbursts of anger, anger-in style, anger-out style, and trait anger. In healthy populations, the harmful effects of hostility and anger constructs on CHD events seems greater in men than in women [41].
Type D personality: Type D (“distressed”) personality confers trait characteristics of experiencing negative affect, which a person avoids to express in social interactions to prevent disapproval by others [42]. In other words, the combined high level of the two dimensions “negative affectivity” and “social inhibition” of Type D designates a general propensity to distress [43]. The prevalence of Type D personality in the general population and in cardiac populations is between 20% and 30%. However, there is a debate whether Type D is a dimensional or categorical construct (i.e., Type D vs. non-type D persons) and whether the construct is stable across time [44].
Several meta-analysis and systematic reviews on the impact of Type D personality in CVD have been published with similar results. Pooled effect sizes across patients with CHD, CHF, and peripheral arterial disease showed type D personality to be associated with a more than 3-fold increased risk of poor long-term prognosis in terms of (cardiac) mortality, recurrent events, and revascularisations [43]. This effect is largely independent of depression, although it may be of questionable value to statistically control Type D effects for other constructs of negative affect, as they are so central to the dimension of “negative affectivity” of Type D personality [44]. Another meta-analysis on patients with CVD found an association between Type D personality and greater risk of major adverse cardiovascular events, whereas health-related quality of life was decreased in Type D persons [45]. Notably, several studies on type D personality in CVD populations stem from the same research group, whereas some recent studies from other groups failed to replicate the significant associations, likely for reasons that may include differences in methodology and study designs [44].
There is much overlap between the negative affectivity dimension of type D (i.e., the tendency to experience dysphoria, anxiety, irritability, and other negative feelings across time and situations) with the nearly identical personality trait neuroticism [44] that, by itself, predicted increased risk of death from CVD in a 21-year prospective cohort study [46].
Negative affect
Depression: Depression is arguably the most extensively studied psychosocial risk factor of CVD. As previously summarised, meta-analysis concerned with the role of depression in the development of CHD report effect sizes from approximately 1.5 to 2.7 depending on the definition of CHD, the measure of depression, and control variables. For studies investigating the predictive value of depression in patients with diagnosed CHD, effect sizes range between 1.6 and 2.2 depending on the original cardiac diagnosis, length of follow-up, definition of prognosis, measure of depression, and covariates controlled [8]. Meta-analytic reviews further show that depression is associated with a 1.3-fold increased risk for incident stroke after adjustment for potential confounding factors [47] and with a 2.1-fold greater risk for death and secondary events in patients with CHF [48].
Depression is a heterogenous concept that is made up of a range of different symptoms. Therefore, attempts are increasingly made to dismantle the depression concept in terms of its “cardiotoxic” components. Major findings and recent trends from the depression-CHD literature are as follows [8, 49]: a) there is a dose-response relationship between depression and CHD severity; b) the mortality risk seems to increase with longer follow-up time; c) first-time depression after MI seems more toxic for cardiac prognosis than recurrent depression; d) in patients after an acute coronary syndrome, treatment resistant depression is associated with a particularly high risk of mortality or recurrent cardiac events; and e) somatic/affective depressive symptoms (e.g., fatigability, appetite and sleep disturbance, pain) are of greater cardiac harm than cognitive/affective ones (e.g., lack of interest, guilt, suicidal thoughts). Somatic/affective depression resembles an atypical depression phenotype and might reflect part of a “sickness behaviour” triggered by proinflammatory cytokines originating from atherosclerotic vessels. Via compromising serotoninergic neurotransmission, chronic signaling of cytokines to the brain may induce a pattern of behavioural and affective changes, including social withdrawal, sleep disturbance, and depressive mood [49, 50].
Anxiety: About 30% of cardiac patients have increased levels of anxiety symptoms. A meta-analysis of 20 studies on totally 250,000 individuals pooled the effects of anxiety across different constructs, including generalised anxiety disorder, panic disorder, social phobia and posttraumatic stress disorder on incident CHD [51]. After a mean follow-up of 11 years anxious persons showed a respectively 1.3-fold and 1.5-fold increased risk of CHD and cardiac mortality, independent of other prognostic factors. In another meta-analysis on 12 papers, a total of 5,750 post-MI patients were followed up for an average of 2.6 years [52]. Anxious patients had poorer prognosis than non-anxious ones. Specifically, risks with anxiety were increased 1.5-fold for all-cause mortality, 1.2-fold for cardiac mortality, and 1.7-fold for new cardiac events. Surviving a heart attack can be a traumatic experience to patients. In fact, between 10% and 20% of post-MI patients will develop clinically relevant levels of posttraumatic stress attributable to MI, such as re-experiencing aspects of the heart attack in thoughts or dreams [53]. We recently showed that MI-triggered posttraumatic stress predicts an increased risk of CVD-related rehospitalisations over a follow-up of three years [54].
Anxiety shows high comorbidity with depression, whereby the association between anxiety and post-MI prognosis seems smaller for anxiety than for depression. Study findings about whether anxiety predicts cardiac outcome independent of depression are mixed. There is little information on associations between individual anxiety disorders and cardiac outcome. Moreover, most studies used questionnaires to assess symptom levels of anxiety (disorders) instead of a structured diagnostic interview. Some studies even suggest a protective effect of anxiety, perhaps because anxious heart patients have greater health alertness and thus seek more often health care than non-anxious ones [52].
Vital exhaustion: Vital exhaustion has been conceptualised as a state of profound mental fatigue, demoralisation and irritability consequent to maladjustment to ongoing psychological stressors [55]. Several studies have shown that vital exhaustion predicts risk of incident MI and CHD mortality as well as recurrent cardiac events in patients after successful coronary angioplasty. Sleeping difficulties (i.e., trouble falling asleep, waking up at night, and waking up unrefreshed) are also part of the vital exhaustion concept and similar insomnia complaints were shown to positively predict the risk of incident CVD in their own right [56]. Overtime work was observed as a principal psychosocial stressor leading to feelings of vital exhaustion [55] and working 11 hours or more compared to 7–8 hours per day predicted incident CHD events over a median follow-up of 12 years in British civil servants [57]. These data are particularly intriguing as emotional exhaustion is also the key dimension of the burnout syndrome due to prolonged stress at work. In the Finnish Health 2000 Study, burnout was associated with an increased prevalence of CVD [58] and predicted overall mortality after a follow-up of 10 years in workers below 45 years of age [59].
A unifying model has been proposed according to which negative affect are part of a biologically driven conservation-withdrawal reaction that occurs if a psychosocial emergency (i.e., fight-flight) situation overwhelms a person and cannot be resolved within a critical time period [60]. Giving up of the organism will set in together with accompanying negative affect, particularly so depression, exhaustion, hopelessness and bereavement.
Hopelessness: As part of the Kupio Ischemic Heart Disease Risk Factor Study, middle-aged men answered two items about whether they felt the future was hopeless and reaching their goals would be impossible [61]. Those reporting high hopelessness had greater progression of carotid atherosclerosis, as measured by intima-media thickness, over 4 years than men reporting low to moderate levels of hopelessness. Moreover, the effects of hopelessness were stronger among men with more severe atherosclerosis at baseline.
Bereavement: Bereavement increases mortality in men more than in women (i.e., 1.3-fold vs. 1.15-fold) within the first two years after the death of the spouse. The risk to die from cardiac causes seems particularly increased [62]. As a substantial portion of bereaved spouses develops depression after spousal death, depressive symptoms are thought to be important mediators of the link between bereavement and CHD.
Positive affect
With the advent of positive psychology research, increasing attempts have been made to identify factors that keep people healthy. Positive affective traits (e.g., optimism, cheerfulness) and states (e.g., happiness, joy, enthusiasm) are gaining considerable attention in behavioural cardiology. Meta-analytic findings suggest that, in healthy populations, positive affect are associated with a 19% and 29% reduction in mortality from all causes and from CVD, respectively; in patients with preexisting CVD, positive affect had no effect on mortality [63]. Nonetheless, a more recent study found that independently of disease severity, depression, and social support, CHD patients with more optimistic expectations of being able to cope with their disease experienced significantly lower total and cardiovascular mortality over a 15-year follow-up period [64]. Of note, the protective effects of positive affect are independent of negative affect [63]. This supports the notion that positive affect is not the mere opposite of negative affect, but that the two constructs rather behave as independent affect systems.
Mechanisms that link psychosocial factors to cardiovascular disease risk
Psychosocial factors may impact cardiovascular health by several pathways and mechanisms, some of which are rather complex [3, 21]. Psychosocial stress is generally associated with more adverse health behaviours. This helps to explain the clustering of psychosocial factors with the established cardiovascular risk factors. For instance, in CHD patients attending outpatient cardiac rehabilitation, the prevalence of abdominal obesity was higher in patients with low SES relative to those with high SES [65]. Psychosocial stress and particularly depression are also associated with lower adherence of CHD patients to recommendations for a healthy heart and cardiac therapy, including regular intake of medications and participation in cardiac rehabilitation programs. There might be a common genetic background to explain the increased life-time co-occurrence of psychosocial stress and CVD. For instance, a twin study showed a genetic correlation between depressive symptoms and CHD that explained 18% of the mutual variance [66]. An index of low central nervous system serotonin levels has also been associated with the clustering of psychosocial risk factors, including hostility, and cardiometabolic risk factors [67]. Also, a polymorphism in the promoter region of the serotonin transporter gene is associated with both an exaggerated hemodynamic reactivity to acute psychosocial stress and an increased risk of MI [68]. This finding is in line with a recent meta-analysis showing that increased cardiovascular responses, including blood pressure and heart rate reactivity, to laboratory stressors predict future risks of hypertension, subclinical atherosclerosis, and CVD events [69]. Epigenetic processes have been proposed as an important mechanism leading from early life environmental stress (e.g., maternal stress) to an increased risk of CVD in adult life. Exposure to increased cortisol levels in utero during maternal stress may affect patterns of gene expression in the fetus, for instance via methylation of the gen that encodes for the glucocorticoid receptor. Fetal programming of a hyperactive stress response system may carry over to adulthood, thereby setting the stage for an increased disease risk [70].
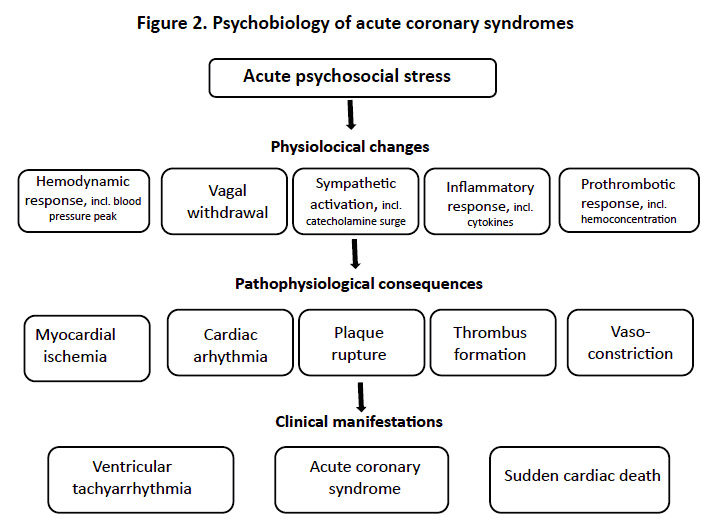
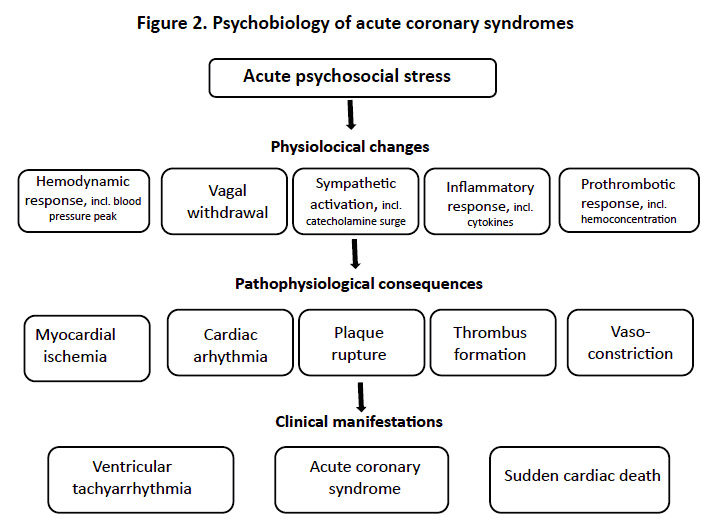
Figure 2
The scheme shows the cascade from physiological cardiovascular changes to pathophysiological alterations and eventually the clinical manifestation of cardiovascular disease in response to acute psychosocial stress.
There is an abundant literature on direct pathophysiologic links between psychosocial factors and CVD [3, 71, 72]. In terms of atherothrombotic diseases, psychosocial factors interact with virtually all of the biological steps leading from atherosclerosis intitiation and progression to clinically manifest CHD. Much of this knowledge has been accumulated from studies measuring circulating biomarkers of endothelial dysfunction, cellular adhesion, inflammation, and a prothrombotic state, all viewed as intermediate endpoint measures of an increased CVD risk. Table 2 summarises these pathologies with their respective measurements. As is described in more detail elsewhere [71–73], chronic stress-related changes in hypothalamic-pituitary-adrenal axis activity and the autonomic nervous system exert regulatory function for both the immune and hemostasis system, thereby resulting in enhanced inflammation, coagulation activation, and reduced fibrinolytic capacity. Figure 2 shows the cascade of events involved in acute coronary syndromes (e.g., fatal or non-fatal MI) as triggered by acute psychosocial stress (e.g., intense affect or trauma stress) [19, 74].
|
Table 2: Psychobiological mechanisms in atherothrombotic diseases. |
|
Pathology
|
Major findings with chronic psychosocial stress
|
| Altered hypothalamic-pituitary adrenal axis activity |
Hypercortisolism, hypocortisolism that is accompanied by downregulated or desensitised glucocorticoid receptors |
| Autonomic dysfunction |
Norepinephrine↑, epinephrine↑, heart rate variability↓, heart rate recovery after exercise↓, baroreflex sensitivity↓ |
| Endothelial dysfunction |
von Willebrand factor↑, endothelin-1↑,
flow-mediated dilation↓, nitric oxide production↓ |
| Upregulated cellular adhesion |
Soluble intercellular-adhesion molecule-1↑, soluble vascular-cellular adhesion molecule-1↑ |
| Increased inflammation |
High-sensitivity C-reactive protein↑, interleukin-6↑, tumor necrosis factor-α↑, interleukin-1β↑, anti-inflammatory cytokines↓, white blood cell count↑ |
| Prothrombotic state |
Fibrinogen↑, clotting factor VII↑, D-dimer ↑, plasminogen activator inhibitor-1↑, platelet hyperactivity |
Clinical practice
Screening for psychosocial risk factors
In 2004, a task force on practice guidelines for the treatment of acute MI patients issued by the American College of Cardiology/AmericanHeart Association (AHA) recommended that the psychosocialstatus of the patient should be evaluated, including inquiriesregarding symptoms of depression, anxiety, or sleep disordersand the social support environment [75]. More recently, the AHA Science Advisory advocated a) routine screening for depression in patients with CHD in various settings, including the hospital, physician’s office, clinic, and cardiac rehabilitation center and b) that patients with positive screening results should be evaluated by a professional qualified in the diagnosis and management of depression [76]. However, not all experts support routine screening for depression, as no trial to date has tested whether the screen and refer paradigm would improve depression outcomes for cardiac patients compared to usual care. They anticipate problematic misdiagnosis or overdiagnosis and inappropriate labeling, adverse effects and costs of inappropriate or unnecessary treatment (e.g., antidepressant treatment in patients with mild depression), as well as unjustified resource allocation [77]. With this debate in mind, it seems appropriate if the clinician inquires about history and symptoms of depression and other psychosocial factors as part of the standard history and physical examination, as appropriate and based on the clinician’s knowledge of the patient and the purpose of the visit [77]. Single item questions as presented in table 3 are a good start for this purpose [78–81]. For instance, if a patient’s answer is “yes” to one or two of the depression items, sensitivity was 90% and specificity was 69% for major depression. A “no” response to both items effectively rules out depression and no further screening is necessary [79]. However, if the screening test is positive (i.e., at least one “yes” answer), the low specificity calls for further diagnostic steps, particularly so if the patient shows significant functional impairment. Depending upon the clinical setting and the clinician’s competence with psychosocial issues, the single item question screening approach (yes/no answers) may be supplemented with broader psychosocial evaluation (e.g., of work place characteristics) and/or with easy-to-administer psychosocial questionnaires (e.g., the Hospital Anxiety and Depression Scale [78]). However, referral to a qualified professional for clinical evaluation, including a structured interview, may be warranted right away. In many countries, cardiology departments now routinely collaborate with behavioural cardiologists, clinical psychologists, or psychosomatic/ psychiatric consultation-liaison services. These “psychocardiologists” are familiar with the psychosocial needs of cardiac patients and patients at risk of CVD [82].
|
Table 3: Single item screening questions for psychosocial risk factors. |
|
Construct
|
Questions to be asked (yes/no answers)
|
| Low socioeconomic status |
Do you have mandatory education? Are you a manual worker? |
| Family stress |
Do you have serious problems with your partner? |
| Job stress |
Do you have enough control over how to meet the demands at work? Is your reward appropriate for your effort? |
| Low social support |
Are you living alone? Do you lack a close confidant? Do you lack any person to help you in case of illness? |
| Anger-proneness and hostility |
Do you frequently feel angry over little things? If someone annoys you, do you regularly let him know? Do you often feel annoyed about habits other people have? |
| Depression |
During the past month, have you often been bothered (i) by feeling down, depressed, or hopeless? (ii) by little interest or pleasure in doing things? |
| Panic-like anxiety |
During the past month, have you had an anxiety attack, i.e., suddenly feeling fear or panic? |
| Posttraumatic stress |
During the past month, have you experienced your heart disease (i) that you had nightmares about it or thought about it when you did not want to? (ii) tried hard not to think about it or to avoid situations that reminded you of it? |
| Exhaustion |
During the past month, have you experienced exhaustion and/or undue fatigue? Was your sleep bad during the last month? |
| A “yes” answer to any of these questions designates a potential psychosocial problem area and further clinical evaluation may be needed. |
Treatment of psychosocial risk factors
Psychotherapy, antidepressant medications, and behavioural interventions, particularly adopting a regular exercise regimen, are the key therapeutic elements. A most recent Cochrane analysis included 24 studies from 51 publications in which psychosocial interventions for CHD patients were evaluated in randomised controlled trials. Studies were only included if trained staff had delivered treatment and effects of the psychological interventions were distinguishable from those of other treatments [83]. Psychological interventions resulted in small-to-moderate improvements of depression and anxiety, while effects on health-related quality of life were not superior over those of usual care. Interventions aimed at treating anger and hostility were most effective in improving depressive mood. There was no strong evidence that psychological interventions reduced all-cause mortality, risk of revascularisation, or non-fatal MI. However, a positive effect could be observed for a reduction of cardiac mortality risk by 1.3-fold. The CVD outcome data partially contrast with another meta-analysis in which a 1.4-fold reduction of all-cause mortality risk was reported for CHD patients in the first two years after the psychological intervention [84]. Sensitivity analyses showed that mortality benefits were greatest when treatment was initiated at least two months after the cardiac event, but were only significant in men. It has been argued that psychosocial treatments for women with CVD should probably consider more gender specific topics (e.g., relationship stress, balancing family and career) to effectively reduce mortality risk [85]. A similar coping skills intervention study was performed in separate groups of men and women with CHD and resulted in reduced fatal and nonfatal recurrent CVD events, including MI, during a mean follow-up of 8 years [86]. A third meta-analysis also found positive effects on all-cause mortality and non-fatal MI in patients with CHD [87]. However, the authors included studies that had combined psychological treatments with exercise training. By itself, 30 minutes of jogging at 70–85% of maximum heart rate three times per week is a means to reduce both negative affect and adverse outcomes in patients with CVD [88].
Several key elements of successful psychosocial intervention programmes for patients with CHD have been identified [89]. The intervention should apply proven principles of cognitive behaviour therapy and is preferably delivered in a group setting for a limited number of about eight sessions. The primary focus lies on the training and practicing of social and coping skills. These ought to enable patients to better handle and resist stressful situations and reduce negative affect. From a terminological point of view, “stress management”, such as offered in cardiac rehabilitation, often refers to multicomponent treatments that also include relaxation methods [85, 86]. Although research is still limited, stress management may favourably affect biological mechanisms involved in atherothrombotic diseases, like vascular endothelial function and cardiac autonomic control [90], which is crucial for psychosocial interventions to improve prognosis of CVD. In addition to reducing depression and anger as well as increasing life-satisfaction, a psychosocial skills training workshop decreased blood pressure and heart rate both at rest and during an anger recall challenge in patients who had undergone coronary bypass surgery [91]. Outpatient cardiac rehabilitation programmes now regularly comprise psychosocial and life style interventions. A 12-week rehabilitation programme in CHD patients was shown to improve depressive symptoms and this effect was maintained after a follow-up of 4 years [92].
In terms of pharmacologic interventions, randomised clinical trials have demonstrated that the two selective serotonin reuptake inhibitors (SSRIs) sertraline and citalopram are safe for patients with CHD and thus the first-line antidepressant drugs in cardiac patients [76]. A recent meta-analysis of SSRI trials showed a reduction in depressive symptoms that did not reach statistical significance at six months follow-up after an acute coronary syndrome [93]. However, subjects treated with antidepressant medications showed a significantly lower rate of re-hospitalisations from all causes compared to usual care. In fact, intrinsic pharmacologic properties of SSRIs might exert favourable cardiovascular effects, such as reduction in platelet hyperactivity and improvement in endothelial function that are independent from SSRI effects on depressive mood [94]. No SSRI seems to be more effective than any other to improve mood [79]. However, as most patients take multiple medications for CVD, interaction effects with some of the SSRIs need to be considered. The most commonly reported adverse effects of SSRIs are insomnia or somnolence, nausea, diarrhea, and sexual dysfunction, most of which may diminish in the first month of treatment. Because of their cardiotoxic side effects, tricyclic antidepressants and monoamine oxidase inhibitors are contraindicated for many patients with heart diseases [76], especially for those with unstable angina, cardiac conduction disorders, and significant ventricular arrhythmias. Other commonly prescribed antidepressants have side effects, which may be of concern in cardiac patients; i.e., systolic hypertension with venlafaxine, weight gain and orthostatic hypotension with mirtazapine, and orthostatic hypotension and ventricular tachycardia with trazadone. Duloxetine and bupropion seem to have a more favourable cardiovascular profile, although bupropion may increase blood pressure [95]. The current notion is that antidepressant medications may reduce depressive symptoms for some CHD patients (i.e., those with more severe depression); for other patients, however, medication fails to clinically meaningfully relieve depressive symptoms and may perform no better than placebo [77, 88]. Therefore, treatment with an SSRI alone will often not meet good clinical practice for cardiac patients with depression. The efficacy of exercise appears generally comparable with antidepressant medication and both tend to be better than placebo in patients with major depression [88].
Concluding remarks
Well-operationalised psychosocial risk factors for CVD with effects of similar magnitude as for established cardiovascular risk factors have been identified over the last half-century. In these studies, CHD seems to be the most often investigated endpoint of interest. However, whether psychosocial risk factors are differently associated with the onset of specific CHD phenotypes (e.g., stable CHD vs. MI vs. unstable angina) as well as specific CVD endpoints (e.g., CHD vs. stroke) has not systematically been investigated. Biobehavioural mechanisms that may link psychosocial stress with CVD risk are plausible, but more psychosocial intervention studies trying to favourably change biological mechanisms that play a role in atherothrombotic diseases are clearly needed. While psychosocial treatments seem to generally reduce distress in cardiac patients, the evidence for a favourable effect on hard cardiovascular endpoints is less convincing. The tailoring of psychosocial, pharmacologic, and behavioural interventions to the individual mental and physical needs of heart disease patients, within a multicomponent and interdisciplinary treatment regimen, bears the potential for even more effective treatments in the future.
References
1 Zahlen und Daten über Herz-Kreislauf-Krankheiten in der Schweiz. Schweizerische Herzstiftung. Ausgabe 2008, Tabelle 2.4.1 (Todesursachen in der Schweiz 2005), p. 38.
2 Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364(9438):937–52.
3 Rozanski A, Blumenthal JA, Davidson KW, Saab PG, Kubzansky L. The epidemiology, pathophysiology, and management of psychosocial risk factors in cardiac practice: the emerging field of behavioral cardiology. J Am Coll Cardiol. 2005;45(5):637–51.
4 Friedmann E, Thomas SA, Liu F, Morton PG, Chapa D, Gottlieb SS; Sudden Cardiac Death in Heart Failure Trial Investigators. Relationship of depression, anxiety, and social isolation to chronic heart failure outpatient mortality. Am Heart J. 2006;152(5):940.e1-8.
5 Matchett M, Sears SF, Hazelton G, Kirian K, Wilson E, Nekkanti R. The implantable cardioverter defibrillator: its history, current psychological impact and future. Expert Rev Med Devices. 2009;6(1):43–50.
6 Wittstein IS, Thiemann DR, Lima JA, Baughman KL, Schulman SP, Gerstenblith G, et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med. 2005;352(6):539–48.
7 Van Den Broek KC, Habibović M, Pedersen SS. Emotional distress in partners of patients with an implantable cardioverter defibrillator: a systematic review and recommendations for future research. Pacing Clin Electrophysiol. 2010;33(12):1442–50.
8 Frasure-Smith N, Lespérance F. Depression and cardiac risk: present status and future directions. Heart. 2010;96(3):173–6.
9 von Känel R. Psychological distress and cardiovascular risk: what are the links? J Am Coll Cardiol. 2008;52(25):2163–5.
10 Cacioppo JT, Berntson GG, Malarkey WB, Kiecolt-Glaser JK, Sheridan JF, Poehlmann KM, et al. Autonomic, neuroendocrine, and immune responses to psychological stress: the reactivity hypothesis. Ann N Y Acad Sci. 1998;840:664–73.
11 Lazarus RS, Folkman S. Stress, Appraisal, and Coping. New York, NY: Springer, 1984.
12 McEwen BS, Gianaros PJ. Central role of the brain in stress and adaptation: links to socioeconomic status, health, and disease. Ann N Y Acad Sci. 2010;1186:190–222.
13 Leor J, Poole WK, Kloner RA. Sudden cardiac death triggered by an earthquake. N Engl J Med. 1996;334(7):413–9.
14 Steinberg JS, Arshad A, Kowalski M, Kukar A, Suma V, Vloka M, et al. Increased incidence of life-threatening ventricular arrhythmias in implantable defibrillator patients after the World Trade Center attack. J Am Coll Cardiol. 2004;44(6):1261–4.
15 Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(11):e442.
16 Charlson FJ, Stapelberg NJ, Baxter AJ, Whiteford HA. Should global burden of disease estimates include depression as a risk factor for coronary heart disease? BMC Med. 2011;9:47.
17 Kudielka BM, von Känel R, Gander ML, Fischer JE. The interrelationship of psychosocial risk factors for coronary artery disease in a working population: do we measure distinct or overlapping psychological concepts? Behav Med. 2004;30(1):35–43.
18 von Känel R, Mausbach BT, Dimsdale JE, Mills PJ, Patterson TL, Ancoli-Israel S, et al. Regular physical activity moderates cardiometabolic risk in Alzheimer’s caregivers. Med Sci Sports Exerc. 2011;43(1):181–9.
19 Surwit RS, Williams RB, Siegler IC, Lane JD, Helms M, Applegate KL, et al. Hostility, race, and glucose metabolism in nondiabetic individuals. Diabetes Care. 2002;25(5):835–9.
20 Shen BJ, Countryman AJ, Spiro A 3rd, Niaura R. The prospective contribution of hostility characteristics to high fasting glucose levels: the moderating role of marital status. Diabetes Care. 2008;31(7):1293–8.
21 Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation. 1999;99(16):2192–217.
22 Low CA, Thurston RC, Matthews KA. Psychosocial factors in the development of heart disease in women: current research and future directions. Psychosom Med. 2010;72:842–54.
23 Marmot G. Status syndrome: a challenge to medicine. JAMA. 2006;295(11):1304–7.
24 Kerr GD, Slavin H, Clark D, Coupar F, Langhorne P, Stott DJ. Do vascular risk factors explain the association between socioeconomic status and stroke incidence: a meta-analysis. Cerebrovasc Dis. 2011;31(1):57–63.
25 Wilkinson RG, Pickett KE. Income inequality and socioeconomic gradients in mortality. Am J Public Health. 2008;98(4):699–704.
26 Kornerup H, Osler M, Boysen G, Barefoot J, Schnohr P, Prescott E. Major life events increase the risk of stroke but not of myocardial infarction: results from the Copenhagen City Heart Study. Eur J Cardiovasc Prev Rehabil. 2010;17(1):113–8.
27 Dong M, Giles WH, Felitti VJ, Dube SR, Williams JE, Chapman DP, et al. Insights into causal pathways for ischemic heart disease: adverse childhood experiences study. Circulation. 2004;110(13):1761–6.
28 Orth-Gomér K, Wamala SP, Horsten M, Schenck-Gustafsson K, Schneiderman N, et al. Marital stress worsens prognosis in women with coronary heart disease: The Stockholm Female Coronary Risk Study. JAMA. 2000;284(23):3008–14.
29 Lee S, Colditz GA, Berkman LF, Kawachi I. Caregiving and risk of coronary heart disease in U.S. women: a prospective study. Am J Prev Med. 2003;24(2):113–9.
30 Mausbach BT, Patterson TL, Rabinowitz YG, Grant I, Schulz R. Depression and distress predict time to cardiovascular disease in dementia caregivers. Health Psychol. 2007;26(5):539–44.
31 Williams VP, Bishop-Fitzpatrick L, Lane JD, Gwyther LP, Ballard EL, Vendittelli AP, et al. Video-based coping skills to reduce health risk and improve psychological and physical well-being in Alzheimer’s disease family caregivers. Psychosom Med. 2010;72(9):897–904.
32 Theorell T, Karasek RA. Current issues relating to psychosocial job strain and cardiovascular disease research. J Occup Health Psychol. 1996;1(1):9–26.
33 Siegrist J. Adverse health effects of high-effort/low-reward conditions. J Occup Health Psychol. 1996;1(1):27–41.
34 Kivimäki M, Virtanen M, Elovainio M, Kouvonen A, Väänänen A, Vahtera J. Work stress in the etiology of coronary heart disease--a meta-analysis. Scand J Work Environ Health. 2006;32(6):431–42.
35 Aboa-Éboulé C, Brisson C, Maunsell E, Bourbonnais R, Vézina M, Milot A, et al. Effort-reward imbalance at work and recurrent coronary heart disease events: a 4-year prospective study of post-myocardial infarction patients. Psychosom Med. 2011;73(6):436–47.
36 Barth J, Schneider S, von Känel R. Lack of social support in the etiology and the prognosis of coronary heart disease: a systematic review and meta-analysis. Psychosom Med. 2010;72(3):229–38.
37 Williams RB, Barefoot JC, Califf RM, Haney TL, Saunders WB, Pryor DB, et al. Prognostic importance of social and economic resources among medically treated patients with angiographically documented coronary artery disease. JAMA. 1992;267(4):520–4.
38 Lett HS, Blumenthal JA, Babyak MA, Strauman TJ, Robins C, Sherwood A. Social support and coronary heart disease: epidemiologic evidence and implications for treatment. Psychosom Med. 2005;67(6):869–78.
39 Friedmann M, Rosenman RH. Association of specific overt behavior pattern with blood and cardiovascular findings; blood cholesterol level, blood clotting time, incidence of arcus senilis, and clinical coronary artery disease. J Am Med Assoc. 1959;169(12):1286–96.
40 Myrtek M. Meta-analyses of prospective studies on coronary heart disease, type A personality, and hostility. Int J Cardiol. 2001;79(2-3):245–51.
41 Chida Y, Steptoe A. The association of anger and hostility with future coronary heart disease: a meta-analytic review of prospective evidence. J Am Coll Cardiol. 2009;53(11):936–46.
42 Denollet J. DS14: standard assessment of negative affectivity, social inhibition, and type D personality. Psychosom Med. 2005;67(1):89–97.
43 Denollet J, Schiffer AA, Spek V. A general propensity to psychological distress affects cardiovascular outcomes: evidence from research on the type D (distressed) personality profile. Circ Cardiovasc Qual Outcomes. 2010;3(5):546–57.
44 Smith TW. Toward a more systematic, cumulative, and applicable science of personality and health: lessons from type D personality. Psychosom Med. 2011;73(7):528–32.
45 O’Dell KR, Masters KS, Spielmans GI, Maisto SA. Does type-D personality predict outcomes among patients with cardiovascular disease? A meta-analytic review. J Psychosom Res. 2011;71(4):199–206.
46 Shipley BA, Weiss A, Der G, Taylor MD, Deary IJ. Neuroticism, extraversion, and mortality in the UK Health and Lifestyle Survey: a 21-year prospective cohort study. Psychosom Med. 2007;69(9):923–31.
47 Dong JY, Zhang YH, Tong J, Qin LQ. Depression and risk of stroke: a meta-analysis of prospective studies. Stroke. 2012;43(1):32–7.
48 Rutledge T, Reis VA, Linke SE, Greenberg BH, Mills PJ. Depression in heart failure a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol. 2006;48(8):1527–37.
49 Ormel J, de Jonge P. Unipolar depression and the progression of coronary artery disease: toward an integrative model. Psychother Psychosom. 2011;80(5):264–74.
50 Dantzer R, O’Connor JC, Freund GG, Johnson RW, Kelley KW. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat Rev Neurosci. 2008;9(1):46–56.
51 Roest AM, Martens EJ, de Jonge P, Denollet J. Anxiety and risk of incident coronary heart disease: a meta-analysis. J Am Coll Cardiol. 2010;56(1):38–46.
52 Roest AM, Martens EJ, Denollet J, de Jonge P. Prognostic association of anxiety post myocardial infarction with mortality and new cardiac events: a meta-analysis. Psychosom Med. 2010;72(6):563–9.
53 Guler E, Schmid JP, Wiedemar L, Saner H, Schnyder U, von Känel R. Clinical diagnosis of posttraumatic stress disorder after myocardial infarction. Clin Cardiol. 2009;32(3):125–9.
54 von Känel R, Hari R, Schmid JP, Wiedemar L, Guler E, Barth J, et al. Non-fatal cardiovascular outcome in patients with posttraumatic stress symptoms caused by myocardial infarction. J Cardiol. 2011;58(1):61–8.
55 Appels A. Exhaustion and coronary heart disease: the history of a scientific quest. Patient Educ Couns. 2004;55(2):223–9.
56 Phillips B, Mannino DM. Do insomnia complaints cause hypertension or cardiovascular disease? J Clin Sleep Med. 2007;3(5):489–94.
57 Kivimäki M, Batty GD, Hamer M, Ferrie JE, Vahtera J, Virtanen M, et al. Using additional information on working hours to predict coronary heart disease: a cohort study. Ann Intern Med. 2011;154(7):457–63.
58 Honkonen T, Ahola K, Pertovaara M, Isometsä E, Kalimo R, Nykyri E, et al. The association between burnout and physical illness in the general population--results from the Finnish Health 2000 Study. J Psychosom Res. 2006;61(1):59–66.
59 Ahola K, Väänänen A, Koskinen A, Kouvonen A, Shirom A. Burnout as a predictor of all-cause mortality among industrial employees: a 10-year prospective register-linkage study. J Psychosom Res. 2010;69(1):51–7.
60 Buerki S, Adler RH. Negative affect states and cardiovascular disorders: a review and the proposal of a unifying biopsychosocial concept. Gen Hosp Psychiatry. 2005;27(3):180–8.
61 Everson SA, Kaplan GA, Goldberg DE, Salonen R, Salonen JT. Hopelessness and 4-year progression of carotid atherosclerosis. The Kuopio Ischemic Heart Disease Risk Factor Study. Arterioscler Thromb Vasc Biol. 1997;17(8):1490–5.
62 Williams JR Jr. Depression as a mediator between spousal bereavement and mortality from cardiovascular disease: appreciating and managing the adverse health consequences of depression in an elderly surviving spouse. South Med J. 2005;98(1):90–5.
63 Chida Y, Steptoe A. Positive psychological well-being and mortality: a quantitative review of prospective observational studies. Psychosom Med. 2008;70(7):741–56.
64 Barefoot JC, Brummett BH, Williams RB, Siegler IC, Helms MJ, Boyle SH, et al. Recovery expectations and long-term prognosis of patients with coronary heart disease. Arch Intern Med. 2011;171(10):929–35.
65 Binder RK, Barth J, Schmid JP, Saner H. Burden of abdominal obesity in cardiac rehabilitation patients: Results from the Swiss CaRe study. Swiss Med Wkly. 2011;141:w13153.
66 Scherrer JF, Xian H, Bucholz KK, Eisen SA, Lyons MJ, Goldberg J, et al. A twin study of depression symptoms, hypertension, and heart disease in middle-aged men. Psychosom Med. 2003;65(4):548–57.
67 Williams RB, Surwit RS, Siegler IC, Ashley-Koch AE, Collins AL, Helms MJ, et al. Central nervous system serotonin and clustering of hostility, psychosocial, metabolic, and cardiovascular endophenotypes in men. Psychsom Med. 2010;72(7):601–7.
68 Brummett BH, Siegler IC, Ashley-Koch A, Williams RB. Effects of 5HTTLPR on cardiovascular response to an emotional stressor. Psychosom Med. 2011;73(4):318–22.
69 Chida Y, Steptoe A. Greater cardiovascular responses to laboratory mental stress are associated with poor subsequent cardiovascular risk status: a meta-analysis of prospective evidence. Hypertension. 2010;55(4):1026–32.
70 Kuzawa CW, Sweet E. Epigenetics and the embodiment of race: developmental origins of US racial disparities in cardiovascular health. Am J Hum Biol. 2009;21(1):2–15.
71 Hänsel A, Hong S, Cámara RJ, von Känel R. Inflammation as a psychophysiological biomarker in chronic psychosocial stress. Neurosci Biobehav Rev. 2010;35(1):115–21.
72 von Känel R, Mills PJ, Fainman C, Dimsdale JE. Effects of psychological stress and psychiatric disorders on blood coagulation and fibrinolysis: a biobehavioral pathway to coronary artery disease? Psychosom Med. 2001;63(4):531–44.
73 von Känel R, Orth-Gomér K. Autonomic function and prothrombotic activity in women after an acute coronary event. J Womens Health. 2008;17(8):1331–7.
74 Steptoe A, Brydon L. Emotional triggering of cardiac events. Neurosci Biobehav Rev. 2009;33(2):63–70.
75 Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, et al. American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction). ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction – executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction). Circulation. 2004;110(5):588–636.
76 Lichtman JH, Bigger JT Jr, Blumenthal JA, Frasure-Smith N, Kaufmann PG, Lespérance F, et al. American Heart Association Prevention Committee of the Council on Cardiovascular Nursing; American Heart Association Council on Clinical Cardiology; American Heart Association Council on Epidemiology and Prevention; American Heart Association Interdisciplinary Council on Quality of Care and Outcomes Research; American Psychiatric Association. Depression and coronary heart disease: recommendations for screening, referral, and treatment: a science advisory from the American Heart Association Prevention Committee of the Council on Cardiovascular Nursing, Council on Clinical Cardiology, Council on Epidemiology and Prevention, and Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Psychiatric Association. Circulation. 2008;118(17):1768–75.
77 Ziegelstein RC, Thombs BD. Is routine screening a parachute for heart disease patients with depression? J Psychosom Res. 2011;71(1):3–5.
78 Albus C, Jordan J, Herrmann-Lingen C. Screening for psychosocial risk factors in patients with coronary heart disease-recommendations for clinical practice. Eur J Cardiovasc Prev Rehabil. 2004;11(1):75–9.
79 Whooley MA. Depression and cardiovascular disease: healing the broken-hearted. JAMA. 2006;295(24):2874–81.
80 Löwe B, Gräfe K, Zipfel S, Spitzer RL, Herrmann-Lingen C, Witte S, et al. Detecting panic disorder in medical and psychosomatic outpatients: comparative validation of the Hospital Anxiety and Depression Scale, the Patient Health Questionnaire, a screening question, and physicians’ diagnosis. J Psychosom Res. 2003;55(6):515–9.
81 Prins A, Ouimette PC, Kimerling R, Cameron RP, Hugelshofer DS, Shaw-Hegwer J, et al. The Primary Care PTSD Screen (PC-PTSD): development and operating characteristics. Primary Care Psychiatry. 2003;9(1):9–14.
82 Herrmann-Lingen C. Steps towards integrated psychosomatic medicine – the example of psychocardiology. J Psychosom Res. 2011;70(2):111–5.
83 Whalley B, Rees K, Davies P, Bennett P, Ebrahim S, Liu Z, et al. Psychological interventions for coronary heart disease. Cochrane Database Syst Rev. 2011;(8):CD002902.
84 Linden W, Phillips MJ, Leclerc J. Psychological treatment of cardiac patients: a meta-analysis. Eur Heart J. 2007;28(24):2972–84.
85 Orth-Gomér K, Schneiderman N, Wang HX, Walldin C, Blom M, Jernberg T. Stress reduction prolongs life in women with coronary disease: the Stockholm Women’s Intervention Trial for Coronary Heart Disease (SWITCHD). Circ Cardiovasc Qual Outcomes. 2009;2(1):25–32.
86 Gulliksson M, Burell G, Vessby B, Lundin L, Toss H, Svärdsudd K. Randomized controlled trial of cognitive behavioral therapy vs standard treatment to prevent recurrent cardiovascular events in patients with coronary heart disease: Secondary Prevention in Uppsala Primary Health Care project (SUPRIM). Arch Intern Med. 2011;171(2):134–40.
87 Welton NJ, Caldwell DM, Adamopoulos E, Vedhara K. Mixed treatment comparison meta-analysis of complex interventions: psychological interventions in coronary heart disease. Am J Epidemiol. 2009;169(9):1158–65.
88 Blumenthal JA. New frontiers in cardiovascular behavioral medicine: Comparative effectiveness of exercise and medication in treating depression. Cleve Clin J Med. 2011;78(Suppl 1):S35–43.
89 Williams RB. Psychosocial and biobehavioral factors and their interplay in coronary heart disease. Annu Rev Clin Psychol. 2008;4:349–65.
90 Blumenthal JA, Sherwood A, Babyak MA, Watkins LL, Waugh R, Georgiades A, et al. Effects of exercise and stress management training on markers of cardiovascular risk in patients with ischemic heart disease: a randomized controlled trial. JAMA. 2005;293(13):1626–34.
91 Bishop GD, Kaur D, Tan VL, Chua YL, Liew SM, Mak KH. Effects of a psychosocial skills training workshop on psychophysiological and psychosocial risk in patients undergoing coronary artery bypass grafting. Am Heart J. 2005;150(3):602–9.
92 Koçer O, Wachter M, Zellweger M, Piazzalonga S, Hoffmann A. Prevalence and predictors of depressive symptoms and wellbeing during and up to nine years after outpatient cardiac rehabilitation. Swiss Med Wkly. 2011;141:w13242.
93 Mazza M, Lotrionte M, Biondi-Zoccai G, Abbate A, Sheiban I, Romagnoli E. Selective serotonin reuptake inhibitors provide significant lower re-hospitalization rates in patients recovering from acute coronary syndromes: evidence from a meta-analysis. J Psychopharmacol. 2010;24(12):1785–92.
94 von Känel R. Platelet hyperactivity in clinical depression and the beneficial effect of antidepressant drug treatment: how strong is the evidence? Acta Psychiatr Scand. 2004;110(3):163–77.
95 Vieweg WV, Julius DA, Fernandez A, Wulsin LR, Mohanty PK, Beatty-Brooks M, et al. Treatment of depression in patients with coronary heart disease. Am J Med. 2006;119(7):567–73.