Management and outcome of severely elevated blood pressure in primary care
DOI: https://doi.org/10.4414/smw.2012.13507
Christoph
Merlo, Klaus
Bally, Benedict
Martina, Peter
Tschudi, Andreas
Zeller
Summary
OBJECTIVE: In primary care the management of patients with acute severely elevated blood pressure (BP) is challenging. The aim of the study was to evaluate the initial management and outcome of patients presenting to their general practitioner (GP) with severe high blood pressure.
METHODS: Twenty five general practitioners prospectively identified 164 patients presenting with severely elevated blood pressure (systolic BP >180 mm Hg and/or diastolic BP >110 mm Hg). At baseline, patients were categorised as having a hypertensive emergency, urgency or asymptomatic BP elevation. The therapeutic approach of the GPs was assessed and patient outcome at 12 month follow-up was analysed.
RESULTS: Median age of 164 patents was 71 (range 22 to 97) years, 60 (37%) were male and 107 (65%) had pre-existing hypertension. Mean baseline systolic BP was 198 ± 16 (range 145 to 255) mm Hg, mean baseline diastolic BP was 101 ± 15 (range 60 to 130). In total, 99 (60%) of patients had asymptomatic BP elevation, 50 (31%) had hypertensive urgency, and 15 (9%) had a hypertensive emergency. Only around two thirds (61%) of patients were given immediate blood pressure lowering medication (most frequently calcium antagonists). Ten patients (6%) were immediately admitted to hospital. Systolic and diastolic BP declined significantly (p <0.01) between one and six hours after study inclusion (drop of systolic and diastolic BP, 24 ± 9 and 10 ± 1, respectively) and were significantly lower (p <0.01) at three month follow-up compared to the initial measurement (drop of systolic and diastolic BP, 37 ± 6 and 14 ± 4, respectively). On average systolic BP was still above target values after three months (148 ± 21). During 12 months of follow-up patients with hypertensive emergency, hypertensive urgency, and asymptomatic BP elevation experienced a cardiovascular event in 27% vs. 6% vs. 16%, of cases respectively (p = 0.17).
CONCLUSION: The majority of 164 patients who presented with acutely and severely elevated blood pressure (BP >180 +/or >110 mm Hg) to their GPs was asymptomatic, had pre-existing hypertension and was managed in GP’s office unless a hypertensive emergency was present. At three month follow-up mean systolic BP was still above target values.
A prospective observational study
Introduction
Hypertension is one of the most common chronic medical conditions affecting approximately 27% of the adult population in Europe [1]. It is estimated that approximately one to two percent of patients treated for hypertension will experience acute and severe blood pressure elevation at some point in their lifetime [2–4]. Severely high BP values are generally considered as a hypertensive crisis and categorised as either a hypertensive emergency or a hypertensive urgency [5, 6]. The management of hypertensive crisis depends on the presence or absence of acute end organ tissue damage [5–7]. Urgent cases are usually managed in an outpatient setting with oral antihypertensive agents and appropriate follow up within 24 hours to several days depending on individual patient characteristics. Emergencies almost always require an immediate reduction of BP mostly with a titratable short acting intravenous antihypertensive agent to prevent or limit progressive end organ damage.
In a general practitioner’s daily clinical practice the management of patients with severely elevated BP is challenging. The evidence on the prevalence and outcome of patients who experience a hypertensive crisis in general is sparse [2]. To our best knowledge data from patients primarily managed in general practices are currently lacking in the literature.
Thus, the aim of the present study was to prospectively evaluate the characteristics, real-life management and outcome of patients presenting to their general practitioners with severely elevated BP.
Methods
Study design
The study uses a prospective observational design. In order to optimise our methodological procedure we proceeded according to the STROBE guidelines (Strengthening the Reporting of Observational Studies in Epidemiology: guidelines for reporting observational studies) [8].
Participants
Participants were recruited prospectively from 25 general practices in the greater agglomerationof the cities Lucerne and Basel, Switzerland. The study was approved by the local Ethical Committee of the University of Basel.Written informed consent was obtained from all subjects. Between March 2008 and July 2009 patients presenting with markedly elevated blood pressure were screened for inclusion during their routine consultation in the general practice. Inclusion criteria were: (a) age ≥18 years, and (b) presenting to their GP with systolic blood pressure >180 mm Hg and/or diastolic blood pressure >110 mm Hg. Patients were excluded if one or more of the following were present: (a) inability to provide informed consent or (b) refusal to participate.
Definition of variables
We allocated the study population to (a) patients presenting with a hypertensive emergency, (b) patients presenting with a hypertensive urgency, and (c) patients presenting severe blood pressure elevation who were asymptomatic according to the presence or absence of acute target organ involvement.
A hypertensive emergency was defined as severe systolic BP elevation of more than 180 mm Hg and/or more than 110 mm Hg for diastolic BP, respectively, with evidence of on-going or progressive target organ damage, i.e. dysfunction of the central nervous system (e.g., focal neurological deficits, apathy, gait disturbances), the cardiovascular system (e.g., dyspnoea, angina pectoris) and/or the renal system (acute kidney injury) [5, 6].
For the present study the definition of hypertensive urgency was the presence of severe BP elevation (systolic or diastolic BP more than 180 mm Hg and/or more than 110 mm Hg, respectively) accompanied by non-specific symptoms such as headache, dizziness, malaise and/or palpitations (impending acute target organ damage) [5, 6].
The term hypertensive crisis is used to indicate either a hypertensive urgency or emergency.
When planning the study we assumed that GPs would also encounter patients who were completely asymptomatic despite severely elevated blood pressure values (systolic BP more than 180 mm Hg and/or diastolic than 110 mm Hg). Those patients not meeting the criteria for hypertensive emergency or urgency were defined as having asymptomatic BP elevation.
Procedure
During an 18 month period in total 172 patients with severely elevated blood pressure were identified, of whom eventually 164 individuals agreed to participate. Patients were recruited during routine consultations. They were asked to participate by their GP if eligible according to inclusion and exclusion criteria. Blood pressure was measured according to current guidelines [5, 6]. Blood pressure was measured by the GP twice in a sitting position after five minutes rest. Validated devices (auscultatory or oscillometric) were used and large cuffs were applied in patients with arm circumference more than 33 cm.
Study patients were categorised as patients with a hypertensive emergency, a hypertensive urgency, or asymptomatic blood pressure elevation. Follow up BP readings were obtained one, six, and twelve hours after initial presentation, after 2 (±1) days, and after 3 (±1) months Patients included in the study were observed for at least one hour in the practice unless urgent hospitalisation was needed due to a hypertensive emergency. One hour after initial presentation first follow-up blood pressure was measured in the practice. After discharge from the practice patients were asked to self-report their blood pressure six and twelve hours after initial presentation. Patient blood pressure was reassessed after 2 (±1) days and 3 (±1) months by the GP in the practice. Twelve months after initial presentation GPs were asked whether their patients had experienced a cardiovascular event (acute coronary syndrome, acute congestive heart failure, transient ischaemic attack or stroke).
Statistical analysis
The results are presented as descriptive statistics, i.e. proportions, means, and standard deviations (SD), unless otherwise specified. Categorical data are given as absolute numbers and percentages of the study population respectively. For continuous paired-traits, Mann-Whitney U-statistics were calculated. To evaluate potential differences in terms of systolic and diastolic blood pressure between the three study groups, a one way analysis of variance (ANOVA) was performed. Analysis of categorical data was performed by chi-square tests. In small samples (e.g. subgroups) Fischer’s exact test was used. A p value of <0.05 was considered to be statistically significant. All data were analysed by using Stata (Stata Statistical Software, 2005; Stata Corp., College Station, USA).
Results
Data of 164 primary care outpatients presenting with severely elevated BP were available. The baseline characteristics are given in table 1. A vast majority (88%) of patients with pre-existing hypertension were already on antihypertensive treatment and 61% of patients presented with severely elevated blood pressure for the first time to their GP.
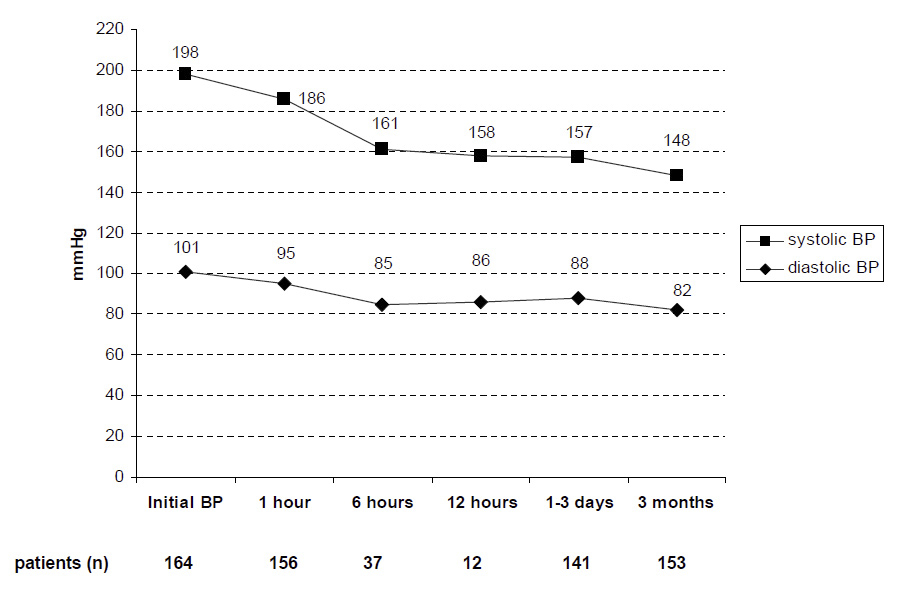
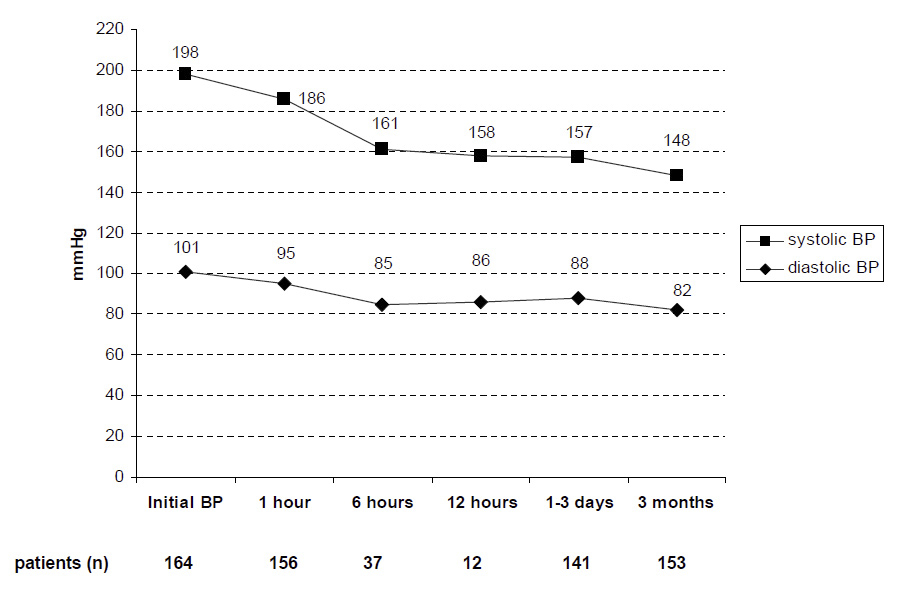
Figure 1
Blood pressure values of all patients (n = 164) presenting with BP >180 mm Hg and/or 110 mm Hg at study entry (initial BP) and follow-up over 3 months. On average, systolic and diastolic BP declined significantly (p <0.01) between one and six hours after initial readings and between 1 to 3 days and three months.
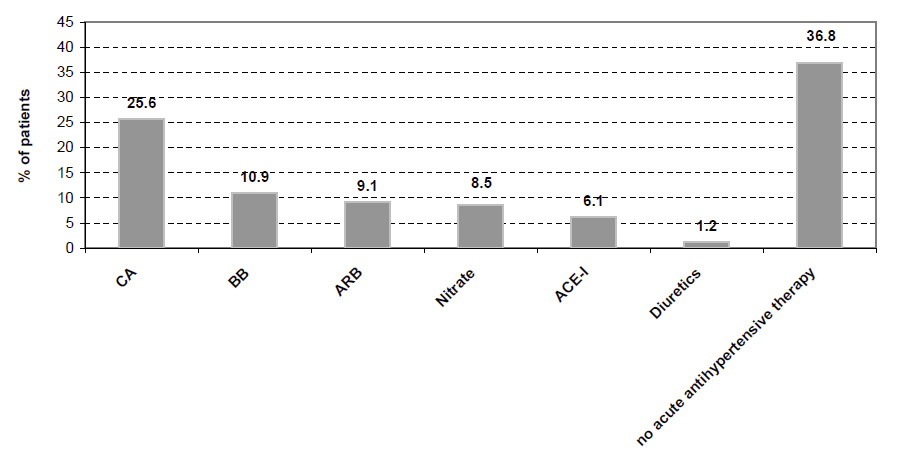
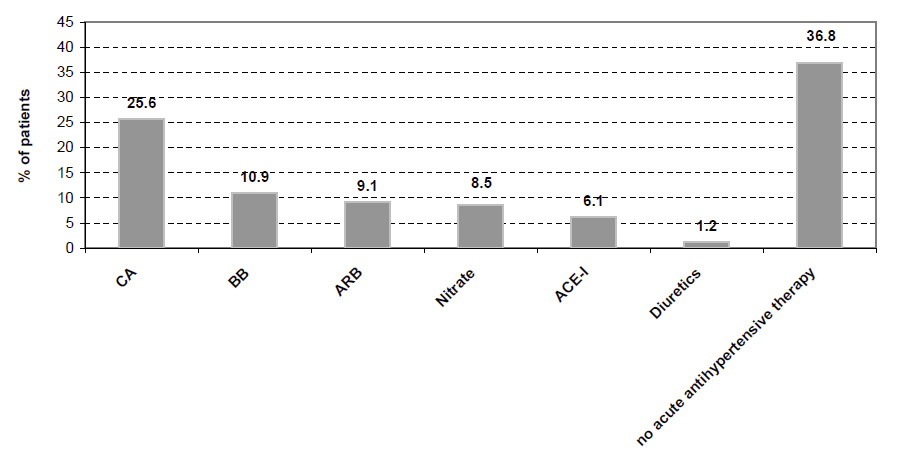
Figure 2
General practitioners’ choice of antihypertensive agent to acutely treat patients presenting with severely elevated blood pressure. CA, BB, ARB, ACE-I refer to calcium channel blockers, beta-blockers, Angiotensin receptor blockers and Angiotensin converting enzyme inhibitors.
Mean initially blood pressure values were 198 ± 16 mm Hg (range 145–255) for systolic and 101 ± 15 mm Hg (range 60–130) for diastolic BP. A majority of patients (n = 105, 64%) were included due to isolated systolic blood pressure elevation (>180 mm Hg), in 18% (n = 29) systolic and diastolic blood pressure were elevated and 5% (n = 8) of subjects had isolated diastolic blood pressure elevation (>110 mm Hg). Systolic and diastolic BP declined significantly (p <0.01) between one and six hours after the initial measurement (drop of systolic and diastolic BP, 24 ± 9 and 10 ± 1, respectively) and compared to initial readings BP values were significantly lower (p <0.01) after a follow-up of three months (drop of systolic and diastolic BP, 37 ± 6 and 14 ± 4, respectively). After 12 hours, one to three days, and three months systolic BP was still hypertensive on average (148 ± 21), whereas diastolic BP remained normotensive (fig. 1).
Overall, 15 (9%), 50 (31%), and 99 (60%) individuals were classified as having a hypertensive emergency, urgency and asymptomatic BP elevation, respectively. Mean initial BP values in patients with hypertensive emergency, urgency and asymptomatic BP elevations were 211 ± 17 mm Hg, 195 ± 18 mm Hg and 197 ± 14 mm Hg for systolic, and 106 ± 15 mm Hg, 101 ± 15 mm Hg and 99 ± 14 mm Hg, respectively. The differences between the three study groups for initial measured BP was significant for diastolic BP (p = 0.002) but not for systolic BP (p = 0.057). After three months no significant difference between emergencies (138/79 ± 14/9 mm Hg), urgencies (146/83 ± 21/9 mm Hg) and asymptomatic patients (152/82 ± 23/12 mm Hg) was present. Headache and dizziness were the most common complaints in hypertensive urgencies (in 77%). Agitation, nausea, palpitations and malaise were less frequent in descending order. In hypertensive emergencies central nervous symptoms (focal neurological deficits, apathy, gait disturbances) were most frequent (in 53%), followed by dyspnoea (20%), angina pectoris (20%) and diplopia (7%).
Figure 2 shows the pharmacological treatment initially given by GPs to patients presenting with severely elevated blood pressure. Around 40% of patients did not receive acute antihypertensive medication. Nearly two thirds of patients (63.2%) immediately received blood pressure lowering medication. Calcium antagonists were given most frequently (nifedipine 20 mg) and 37% of patients initially received a combination therapy (≥ two antihypertensive drug classes). Patients with hypertensive urgency or emergency received significantly more frequently prompt blood pressure lowering medication than asymptomatic patients presenting without symptoms (OR 7.9, CI95% 3.4 to 18.2, p <0.0001). No difference in terms of administering acute antihypertensive therapy was found between subjects with hypertensive urgency and emergency. Calcium channel blockers were the most frequent (25.6%), notably nifedipine. Overall, 10 (6%) patients were immediately admitted to hospital, mostly subjects with hypertensive emergency (n = 8). All asymptomatic patients were managed at the GP’s office.
Follow-up data for 140 (85.4%) patients at 12 month follow-up were available for analysis. Overall, 23 subjects (16.4%) experienced a cardiovascular event such as acute congestive heart failure (n = 8, 35%), stroke (n = 6, 26%) or transient ischaemic attack (n = 1, 4%), symptomatic peripheral arterial occlusion (n = 5, 22%) or acute coronary syndrome (n = 3, 13%). Amongst the patients with asymptomatic blood pressure elevation one out of ten (n = 10, 11%) experienced a documented cardiovascular event. The difference between asymptomatic patients and subjects with hypertensive urgency and/or emergency regarding the occurrence of cardiovascular events was not significant (p = 0.17). Seven patients died during follow-up, mostly of congestive heart failure. Cardiovascular risk factors were not more frequent among patients presenting with hypertensive emergency compared to patients with hypertensive urgency and/or asymptomatic blood pressure elevation. In addition no differences between the occurrence of hypersensitive emergency, urgency and asymptomatic hypertension were found in patients with pre-existing or newly documented hypertension.
|
Table 1: Baseline characteristics of the study population (n = 164). *Values refer to BP (average of two readings) and pulse initially measured when patients presented to the GP’s office; SD refers to standard deviation; bpm refers to beats per minute. |
|
Characteristic
|
Description
|
| Median age (years) ( SD |
71 (15) |
| Male gender, n |
62 (38%) |
| Diabetes, n |
36 (22%) |
| Dyslipidaemia, n |
62 (38%) |
| Smoking cigarettes, n |
30 (18%) |
| Obesity (BMI >30 kg/m2), n |
50 (30%) |
| Pre-existing hypertension, n |
117 (71%) |
| Mean systolic BP* (mm Hg) ± SD |
198 ± 16 |
| Mean diastolic BP* (mm Hg) ± SD |
101 ± 15 |
| Mean pulse frequency * (bpm) ± SD |
78 ± 15 |
Discussion
Approximately 1 to 2% of patients treated for hypertension will experience acute and severe blood pressure elevation at some point in their lifetime [2–4]. Therefore general practitioners should expect to see patients with severely elevated blood pressure in their clinical practice.
In the present study a majority of patients had asymptomatic acute raises in blood pressure (60%). Hypertensive urgencies were observed more frequently (31%) than hypertensive emergencies (9%). In the medical literature the clinical problem of acutely and severely elevated blood pressure is discussed sparsely and most studies have been conducted in patients managed in hospital settings. These studies are usually old [9, 10] and have been carried out in specific populations [11]. Some information is available on patients with hypertensive crisis managed in emergency unit settings (in-hospital). Zampaglione and colleagues reported on 1,634 patients presenting with hypertensive crisis (defined as a diastolic blood pressure ≥120 mm Hg) to an emergency department in Northern Italy [7]. The authors found a prevalence of hypertensive crises of 3% and nearly one quarter (24%) of these patients were considered to have hypertensive emergencies with on-going target damage. In our population from primary care the proportion of hypertensive emergencies is considerably lower (9%) This seems to be realistic because patients with more serious symptoms usually seek medical advice from hospital services. On the other hand, it is noteworthy that among patients presenting to their GPs with asymptomatic severely elevated blood pressure, 11% experienced a cardiovascular event during a follow-up of one year, most frequently acute congestive heart failure (35%). This finding underlines the point that in asymptomatic patients with severely elevated blood pressure (>180 +/or 110 mm Hg) adequate adaptation to the antihypertensive medication and close clinical follow-up on an outpatient basis must be guaranteed. Studies on the quality of treatment modifications and follow-up by GPs are lacking in the literature. However, some data is available from hospital settings. These studies suggest that a majority (71%) of patients treated for hypertensive crisis in urban emergency departments did not receive adequate medical regimen modification or discharge instructions to follow up with the GP [12]. In addition, in the present study blood pressure control after three month was insufficient. Mean systolic blood pressure was still above target values whereas mean diastolic blood pressure decreased to normal. One explanation for this could be that GPs did not modify antihypertensive therapy aggressively enough. Indeed, it has been shown that physicians appear to overestimate their adherence to guidelines regarding treatment of hypertensive patients [13]. Recent data from Switzerland showed that control rates for complicated hypertension, particularly diabetes-associated, have not improved over time [14].
Only a minority of patients included in our study had unknown hypertension (25%), indicating that hypertensive crisis seems to occur more frequently in patients with known hypertension. This finding is in line with evidence from previous studies assessing patients with hypertensive crises treated in emergency units of university-affiliated hospitals [7, 15]. Furthermore, a majority of patients with pre-existing hypertension were on blood pressure lowering medication before presenting with severely elevated blood pressure to their GP. These data confirm previous studies reporting that insufficient adherence to antihypertensive therapy or inadequate therapy may play a decisive role regarding the aetiology of hypertensive crises [16–19]. As a matter of fact, in a recent study assessing potential risk factors non-adherence was the most important risk factor and significantly associated with hypertensive crisis [18]. In another study, 15–50% of patients presenting to an emergency department with a hypertensive emergency were not adherent to their antihypertensive medication regimen in the preceding week [19].
In our study around 40% of patients presenting with severely high blood pressure did not receive any antihypertensive therapy and these were notably asymptomatic patients. Nearly two thirds of participants were treated with at least one antihypertensive drug, most frequently calcium channel blockers, particularly nifedipine. There is an obvious lack of trial evidence that asymptomatic patients with severe hypertension (not fulfilling the criteria of hypertensive crisis) benefit from acute lowering of blood pressure. Not providing antihypertensive agents to patients with severely elevated blood pressure in the absence of acute target organ damage does not imply that these patients are treated inadequately. One influential editorial described such situations “pseudo-emergencies” and characterised aggressive medical therapy for asymptomatic severely blood pressure elevation as primarily cosmetic, intended to calm the patient and physician without substantive medical benefit for the patient [20].
The primary limitation of this study is its observational nature and we are aware of the fact that ascertainment bias might have precluded precise information on the number of hypertensive urgencies or emergencies among patients with severely elevated BP. However, our intent was to document the management of patients with severely elevated blood pressure in GP practices and therefore we could not mandate standardised blood pressure measuring techniques. We chose this design to ascertain real-life conditions in GP offices. We also decided to incorporate patient self-reported blood pressure readings (follow-up measurements after six and twelve hours) to reflect real-life conditions in daily practice. As a consequence we were able to analyse GP acute real-life management of severely elevated blood pressure. The selection of the participating general practitioners may have influenced the results of management quality. It is possible that those physicians willing to collaborate are those who are more likely to be guideline adherent. Furthermore, the number of participating GPs was small and GPs were recruited only from two areas in Switzerland which limits the generalisability of the results.
In summary, we conclude that the majority of patients presenting with severely elevated blood pressure (>180/110 mm Hg) to their GP are asymptomatic, have pre-existing hypertension and can be managed in the GP’s office unless a hypertensive emergency is present. Furthermore, our data show an inadequate systolic blood pressure control after a three-month follow up which necessarily implies a more aggressive modification of blood pressure lowering treatment by the GP. Further studies are required to determine and improve the quality of GP management of asymptomatic severely hypertensive patients in terms of adequate treatment modifications of and appropriate clinical follow-up.
Acknowledgments: We are grateful to all participating GPs for their highly appreciated work, participation and professional contribution.
Lucerne: Dres. Andreas Bitzi, Martina Buchmann, Jürg Fritschi, Beni Estermann, Urs Gübelin, Bernhard Häfliger, Andreas Imobersteg, Aldo Kramis, Heidi und Benedikt Kuster, Andreas Lischer, Franz Maurer, Christoph Merlo, Werner Messerli, Heini Rosner, Annemarie Scherrer, Edith Schwegler-Frey, Christian Studer, Maria Widmer, Kurt Züsli. Basel: Klaus Bally, Béatrice Kaufmann, Louis Litschgi, Edy Riesen, Silvana Romerio, Peter Sigg
References
1 Wolf-Maier K, Cooper RS, Banegas JR, Giampaoli S, Hense HW, Joffres M, et al. Hypertension prevalence and blood pressure levels in 6 european countries, canada, and the united states. JAMA. 2003;289(18):2363–9.
2 Cherney D and Straus S. Management of patients with hypertensive urgencies and emergencies: A systematic review of the literature. J Gen Intern Med. 2002;17(12):937–45.
3 Marik PE, Varon J. Hypertensive crises: challenges and management. Chest. 2007;131(6):1949–62.
4 Varon J, Marik PE. The diagnosis and management of hypertensive crises. Chest. 2000;118(1):214–27.
5 Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, et al. 2007 guidelines for the management of arterial hypertension: The task force for the management of arterial hypertension of the european society of hypertension (esh) and of the european society of cardiology (esc). J Hypertens. 2007;25(6):1105–87.
6 Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr. et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: The jnc 7 report. JAMA. 2003;289(19):2560–72.
7 Zampaglione B, Pascale C, Marchisio M and Cavallo-Perin P. Hypertensive urgencies and emergencies. Prevalence and clinical presentation. Hypertension. 1996;27(1):144–7.
8 von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC and Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (strobe) statement: Guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–9.
9 Kincaid-Smith P, Mc MJ and Murphy EA. The clinical course and pathology of hypertension with papilloedema (malignant hypertension). Q J Med. 1958;27(105):117–53.
10 Bechgaard P, Kopp H and Nielsen J. One thousand hypertensive patients followed from 16–22 years. Acta Med Scand Suppl. 1956;312:175–84.
11 Brizio-Molteni L, Molteni A, Cloutier LC, Rainey S. Incidence of post burn hypertensive crisis in patients admitted to two burn centers and a community hospital in the united states. Scand J Plast Reconstr Surg. 1979;13(1):21–8.
12 Karras DJ, Kruus LK, Cienki JJ, Wald MM, Chiang WK, Shayne P, et al. Evaluation and treatment of patients with severely elevated blood pressure in academic emergency departments: A multicenter study. Ann Emerg Med. 2006;47(3):230–6.
13 Steinman MA, Fischer MA, Shlipak MG, Bosworth HB, Oddone EZ, Hoffman BB, et al. Clinician awareness of adherence to hypertension guidelines. Am J Med. 2004;117(10):747–54.
14 Brenner R, Waeber B, Allemann Y. Medical treatment of hypertension in switzerland. The 2009 swiss hypertension survey (swisshype). Swiss Med Wkly. 2011;141(w13169.
15 Martin JF, Higashiama E, Garcia E, Luizon MR, Cipullo JP. Hypertensive crisis profile. Prevalence and clinical presentation. Arq Bras Cardiol. 2004;83(2):131–6; 25–30.
16 Wu PH, Yang CY, Yao ZL, Lin WZ, Wu LW, Chang CC. Relationship of blood pressure control and hospitalization risk to medication adherence among patients with hypertension in taiwan. Am J Hypertens. 2010;23(2):155–60.
17 Tisdale JE, Huang MB and Borzak S. Risk factors for hypertensive crisis: Importance of out-patient blood pressure control. Fam Pract. 2004;21(4):420–4.
18 Saguner AM, Dur S, Perrig M, Schiemann U, Stuck AE, Burgi U, et al. Risk factors promoting hypertensive crises: Evidence from a longitudinal study. Am J Hypertens. 2010;23(7):775–80.
19 Tumlin JA, Dunbar LM, Oparil S, Buckalew V, Ram CV, Mathur V, et al. Fenoldopam, a dopamine agonist, for hypertensive emergency: A multicenter randomized trial. Fenoldopam study group. Acad Emerg Med. 2000;7(6):653–62.
20 Grossman E, Messerli FH, Grodzicki T and Kowey P. Should a moratorium be placed on sublingual nifedipine capsules given for hypertensive emergencies and pseudoemergencies? JAMA. 1996;276(16):1328–31.