Morbidity in surgery: impact of the 50-hour work-week limitation in Switzerland
DOI: https://doi.org/10.4414/smw.2012.13506
Reto
Kaderli, Adrian
Businger, Antoine
Oesch, Ulrich
Stefenelli, Urban
Laffer
Summary
PRINCIPLES: Work-hour regulations for residency programmes in Switzerland, including a 50-hour weekly limit, were set in on 1 January 2005. Patient safety was one of the major arguments for the implementation. As the effect of the restriction of residency work hours on patient care in Switzerland has not yet been evaluated on objective data, the aim of the present study was to assess its impact by comparing the patients‘ morbidity and mortality before (2001–2004) and after (2005–2008) the implementation.
METHODS: Retrospective analysis of records of the Spitalzentrum Biel AG, a large referral center classified according to the Swiss Medical Association, collected in the database of the Association for Quality Assurance in Surgery (AQC), a prospective database of consecutive patients undergoing surgical procedures in Switzerland. A selection of 2,686 patients with common surgeries, operated on by residents, was performed.
RESULTS: There were 1,259 (46.9%) patients meeting our inclusion criteria who were admitted during the period before introduction of work-hour limitation and 1,427 (53.1%) patients after introduction. The in-hospital mortality and postoperative surgical complication rate were significantly higher after the reform (p <0.05 and p <0.01, respectively). No significant differences could be found concerning the overall intraoperative (p = 0.61) and postoperative medical complication frequencies (p = 0.08).
CONCLUSIONS: The work-hour limitation implemented in Switzerland was not associated with surgical patient safety measure improvement for common surgeries (i.e., morbidity and mortality rate). Further research on a nationwide basis is needed to assess the value of the higher surgical complication and mortality rate.
Introduction
Whereas in other occupational settings, such as commercial aviation, strict work-hour regulations and rest periods have been taken for granted since 1940, work-hour limitation for all residency programmes in Switzerland were only set on 1 January 2005 by the Swiss government [1, 2].The new requirements include a 50-hour weekly limit with a maximum overtime of 2 hours per day and 140 hours per year, respectively, and at least 11 hours of rest between duty periods. Overtime per day may exceed 2 hours during work-free business days or in emergency cases. Daily rest time may be reduced to 9 hours several times a week, as long as the resting time amounts to 12 hours, averaged over 2 weeks.
Traditionally, surgical skills were attained during extended work shifts by performing every aspect of patient care, observing, and assisting according to the Halsted paradigm of total dedication to surgery and patients [3–5]. Residents were expected literally to live in hospitals [6].
As sleep deprivation might result in reduced alertness and jeopardised patient safety, there was a growing public demand for work-hour limitations [4, 7]. Potential negative effects of fatigue due to extended shift duration and long work hours on performance in general [8], lack of quality patient care with serious medical errors [9–12], worse performance during operations [13], and simulated surgical procedures in particular are well documented but still often contradictory [14, 15].
However, there is little evidence of an improvement in patient safety by the restriction of resident work hour regarding morbidity or mortality [16–18]. On the contrary, US studies showed that the 80-hour work-week limitation has not resulted in a deterioration in patient outcomes [19–21]. The reasons for the lack of an amelioration are unclear. It has been argued that discontinuity of care can be more dangerous than sleep deprivation, particularly during night-time cross-coverage and in academic health centers [22–25]. Furthermore, restrictions in the United States exclude attending physicians and are applied to resident physicians only [26].
Patient safety was, besides the improvement of work-life balance of physicians, one of the major arguments for the implementation of a 50-hour work-week limitation for residents and senior physicians in Switzerland. Lifestyle, in the sense of time, is a main impediment for choosing a surgical career and, on the other hand, the high prevalence of work/life conflicts among physicians has been found as an explanation for a high prevalence of poor self-rated health [27–29]. Chief physicians and department heads are excluded from the restriction on working time. Nevertheless, the effect of the restriction of resident work hours on patient care in Switzerland has not yet been evaluated based on objective data. In a nationwide survey in Switzerland a subjective improvement of residents’ quality of life with a negative effect on surgical training and quality of patient care was found [30]. The aim of the present study was to assess the impact of the 50-hour work-week limitation in Switzerland by comparing the patients’ morbidity and mortality in common surgeries done by residents before and after the implementation.
Methods
Study design
This analysis utilised the records of the Spitalzentrum Biel AG, a large referral center classified according to the Swiss Medical Association [31], collected in the database of the Association for Quality Assurance in Surgery (AQC), a prospective database of consecutive patients undergoing surgical procedures in Switzerland [32]. Overall, 47 hospitals participated in the AQC, all of which were teaching hospitals. This database is complete, although only 47/96 of Swiss surgical departments enroll their patients.
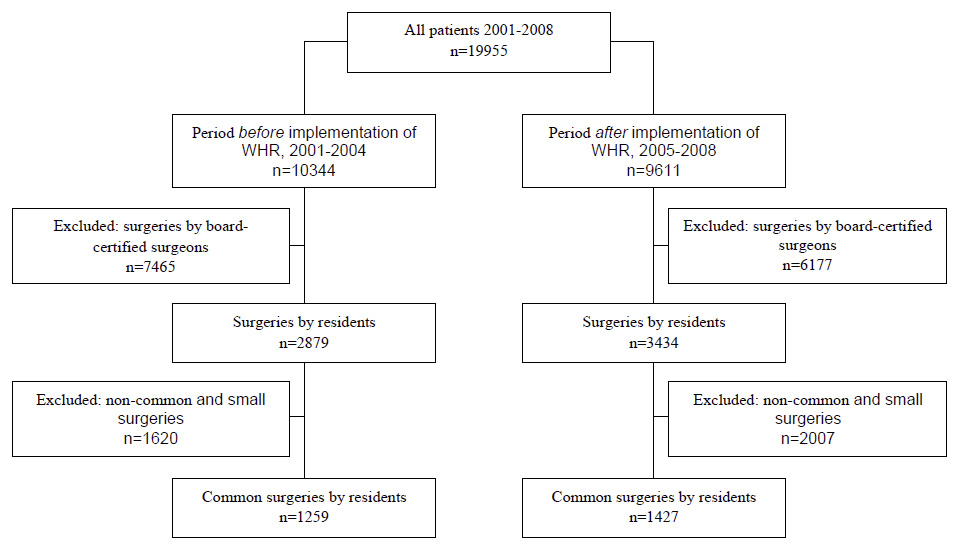
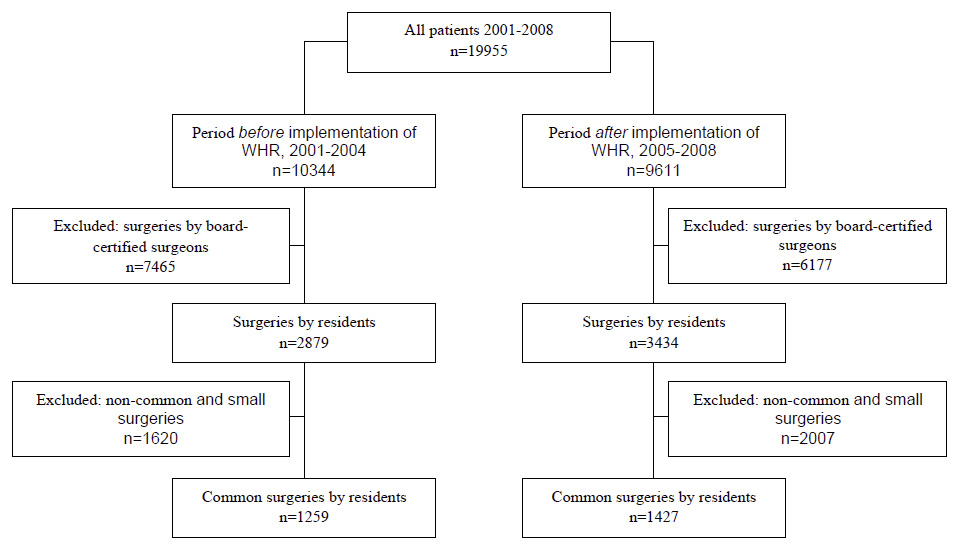
Figure 1
Study design. WHR: work-hour restrictions; non-common surgeries: mammary and thoracic operations, large abdominal and vessel surgeries, surgeries of the genitourinary system, treatment of hand injuries; small surgeries: excision of lymphnodes, metal removals, fracture fixations with Kirschner wires, small amputations, operations on tendons and ligaments and arthroscopies; common surgeries: herniotomy, cholecystectomy, appendectomy, thyroid surgery, proctological interventions, varicose vein operations, colorectal and small intestine surgery, and fracture fixation without Kirschner wire.
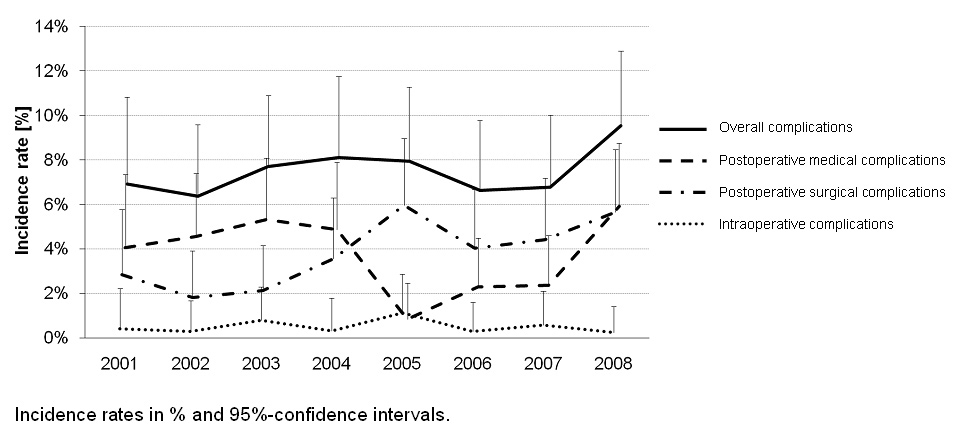
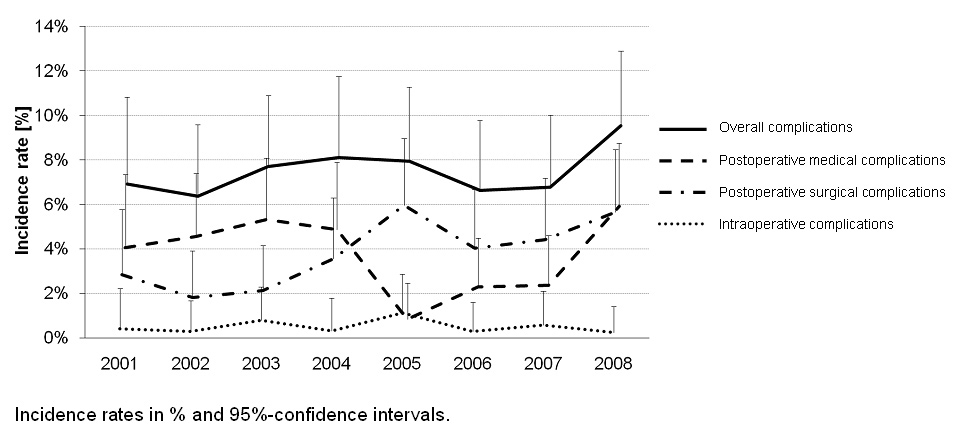
Figure 2
Rate of complications between 2001-2008.
For the purposes of this study, we considered patients admitted from January 2001 to December 2008 to the Spitalzentrum Biel AG. We examined two time periods: The time before introduction of work-hour limitations (January 2001 to December 2004) and after introduction (January 2005 to December 2008). Demographic data were collected including age, sex, body mass index, American Society of Anesthesiologists fitness score, malignant neoplasia, and time of surgery (emergency vs. elective) for comparison of baseline characteristics between patients in the two time groups.
Primary endpoints were intraoperative complications (e.g., bowel injury, vessel injury, and other), postoperative surgical complications (e.g., wound dehiscence, bleeding, surgical site infection, intraabdominal abscess, anastomotic leakage, fistula, peritonitis and other), and medical complications (e.g., myocardial infarction, cardiac arrhythmia, pneumonia, pulmonary embolism, deep vein thrombosis, renal insufficiency, septicemia, multiple organ failure, apoplectic insult, urinary tract infection, and other) and outcome measures (e.g., length of hospital and intensive care unit stay, required mechanical ventilation, number of transfusions and complications per patient). The secondary endpoint was in-hospital mortality.
The average residents’ weekly working time was calculated based on the daily clocking-in times recorded by themselves, as usual in Switzerland, and verified monthly by the head of department.
The study was exempt from approval by the ethical committee, as data were kept anonymous and the purpose of the AQC database is a quality assessment tool.
Selection of patients
Of all 19,955 surgeries performed by residents and board-certified surgeons, 13,642 (68.4%) operations performed by the latter were excluded (fig. 1). Furthermore, a selection of common surgeries was performed (herniotomy, cholecystectomy, appendectomy, thyroid surgery, proctological interventions, varicose vein operations, colorectal and small intestine surgery, and fracture fixation without use of Kirschner wire), which made up 13.5% (2,686/19,955) of the total number of operations.
In Switzerland surgical residents have to perform a list of surgical operations, consisting of 545 surgeries divided into three degrees of difficulty to become board-certified surgeons. Our selection represents the most common surgical procedures of residents. In every case residents’ operations were supervised by a board-certified surgeon during the intervention. Non-common surgeries (220/545; 40.4%), which are usually performed by board-certified surgeons, and small surgeries (55/545; 10.1%), which only hardly contribute to an increase of the patients’ morbidity or mortality statistics, were excluded. The exclusion comprised mammary and thoracic operations, large abdominal (gastric and pancreatic) and vessel surgeries, surgeries of the genitourinary system, treatment of hand injuries, and small surgeries (excision of lymphnodes, metal removals, fixations with Kirschner wires, small amputations, operations on tendons and ligaments, as well as arthroscopies). In all, 270/545 (49.5%) surgical operations of the above-mentioned list were included.
Statistical analysis
All statistical computations were performed by an experienced statistician (US).
Collected data were analysed by using SPSS version 17.0 (SPSS Inc.; Chicago, USA) and SAS version 9.0 (SAS Institute Inc.; Heidelberg, Germany). On the basis of multiple logistic regression models the changes between 2001 and 2004 and those between 2005 and 2008 were assessed. All predictor variables were entered into the model at the same time, since not only the predictors by themselves, but their inter-correlations were used to improve the prediction of the dependent variable. Chi-square test was used to assess contrasts between groups and Mann-Whitney U test to examine intergroup differences.
Continuous data with a normal distribution were expressed as mean (standard deviation) or median (range), and dichotomous data were expressed as frequencies and percentages.
Levels of statistical significance were defined as P <0.05. All tests were two-sided.
Results
The residents’ weekly work hours decreased from 52.5 (SD 0.7) hours before the limitations (2001–2004) to 49.7 (SD 0.7) hours after introduction of the limitations (2005–2008), (p = 0.11).
Patient characteristics
There were 1,259 (46.9%) patients meeting our inclusion criteria who were admitted during the period before introduction of work-hour limitation (2001–2004) and 1,427 (53.1%) patients after introduction (2005–2008). Baseline characteristics for these two groups are shown in table 1. They did not differ significantly with regard to age, sex, body mass index, American Society of Anesthesiologists fitness score, and malignant neoplasia. The group after introduction of the 50-hour work-week limitation contained significantly fewer elective admissions and showed a significantly longer duration of surgery. To facilitate the interpretation of the results, the two groups were assumed to be similar because of the small absolute differences.
Univariate analysis
A comparison of intraoperative and postoperative complication rates revealed a significantly higher postoperative surgical complication rate after the reform (p <0.01), whereas no significant difference could be found concerning the overall intraoperative (p = 0.61) and postoperative medical complication rate (p = 0.08). Table 2 shows a detailed list of intraoperative and postoperative surgical and medical complications.
Furthermore, univariate analysis showed a statistically significant shorter hospital length of stay after introduction of work-hour regulations (p = 0.01). The implementation of work-hour limitations was not associated with a higher overall complication rate per patient (p = 0.62).
An additional evaluation of all patients with common surgeries operated by board-certified surgeons and residents revealed a significant increase in the postoperative surgical complication rate after the reform, as well (p <0.01).
Multivariate analysis
Intraoperative and postoperative complication rates were further analysed with multiple logistic regression models (table 3), except for low complication rates, to predict the independent effect of the work-hour limitations on each category of complication: “Surgical site infection” and “other postoperative surgical complications” were independently associated with higher rates of postoperative surgical complications after enforcement of the 50-hour work-week limitation (p = 0.04 and p <0.01, respectively).
The statistically significant shorter hospital length of stay after introduction of work-hour regulations, which was found with univariate analysis, was not confirmed by multiple logistic regression models (p = 0.09). The percentage of intubated patients in intensive care units was significantly lower after the reform (p = 0.02).
In contrast to univariate analysis, the logistic regression analysis showed a significant increase of the in-hospital mortality after the reform (p <0.05).
An additional evaluation of all patients with common surgeries operated by board-certified surgeons and residents revealed a significant increase in the in-hospital mortality rate, as well (OR 1.63; 95% CI 1.06–2.50; p = 0.03).
|
Table 1: Baseline characteristics of patients (n = 2,686). |
|
Characteristic
|
Before reform
(2001–2004)
(n = 1,259)
|
After reform
(2005–2008)
(n = 1,427)
|
P-value
|
| Age, median (range), y |
52 (16–95) |
50 (16–97) |
0.07 |
| Sex, No. (%) |
|
|
|
| Male |
700 (55.6) |
833 (58.4) |
0.15 |
| Female |
559 (44.4) |
594 (41.6) |
|
| BMI, median (range), kg/m2
|
25 (16–55) |
25 (15–51) |
0.14 |
| ASA score ≥III, No. (%) |
112 (9.2) |
123 (8.6) |
0.64 |
| Malignant neoplasia, No. (%) |
30 (2.4) |
25 (1.8) |
0.25 |
| Elective admission, No. (%) |
818 (65.9) |
846 (60.9) |
0.01 |
| Duration of surgery, median (range) h |
1.2 (0–5.2) |
1.3 (0–13.8) |
<0.01 |
| BMI = body mass index; ASA = American Society of Anesthesiologists. |
|
Table 2: Univariate analysis of intraoperative, postoperative surgical and medical complications and outcome measures (n = 2,686). |
|
Characteristic
|
Before reform
2001–2004
(n = 1,259)
No. (%)
|
After reform
2005–2008
(n = 1,427)
No. (%)
|
P-Value
|
| Complications: |
|
|
|
| Intraoperative complications |
|
|
|
| No intraoperative complications |
1,253 (99.5) |
1,419 (99.4) |
0.76 |
| Bowel injury |
1 (0.1) |
0 (0.0) |
0.29 |
| Vessel injury |
2 (0.2) |
2 (0.1) |
0.90 |
| Other (e.g., splenic, vesical, hepatic injury) |
3 (0.2) |
6 (0.4) |
0.42 |
| Postoperative surgical complications |
|
|
|
| No postoperative surgical complications |
1,227 (97.5) |
1,355 (95.0) |
<0.01 |
| Wound dehiscence |
2 (0.2) |
1 (0.1) |
0.49 |
| Bleeding |
5 (0.4) |
3 (0.2) |
0.38 |
| Surgical site infection |
2 (0.2) |
11 (0.8) |
0.02 |
| Intraabdominal abscess |
3 (0.2) |
1 (0.1) |
0.26 |
| Anastomotic leakage |
1 (0.1) |
0 (0.0) |
0.29 |
| Fistula |
1 (0.1) |
1 (0.1) |
0.93 |
| Peritonitis |
0 (0.0) |
0 (0.0) |
NC |
| Other (e.g., abdominal incision dehiscence, wound edge necrosis, residual gallstone, compartment syndrome) |
18 (1.4) |
55 (3.9) |
<0.01 |
| Postoperative medical complications |
|
|
|
| No postoperative medical complications |
1,199 (95.2) |
1,385 (97.1) |
0.01 |
| Myocardial infarction |
0 (0.0) |
2 (0.1) |
0.18 |
| Pneumonia |
2 (0.2) |
3 (0.2) |
0.76 |
| Pulmonary embolism |
0 (0.0) |
1 (0.1) |
0.35 |
| Deep vein thrombosis |
0 (0.0) |
0 (0.0) |
NC |
| Renal insufficiency |
2 (0.2) |
0 (0.0) |
0.13 |
| Septicemia |
1 (0.1) |
1 (0.1) |
0.93 |
| Multiple organ failure |
1 (0.1) |
1 (0.1) |
0.93 |
| Apoplectic insult |
0 (0.0) |
1 (0.1) |
0.35 |
| Urinary tract infection |
5 (0.4) |
2 (0.1) |
0.19 |
| Other (e.g., cardiac or respiratory insufficiency, ileus, fever of unknown origin, allergic reaction, electrolyte imbalance) |
40 (3.2) |
29 (2.0) |
0.06 |
| |
|
|
|
| Outcome measures: |
|
|
|
| Length of hospital stay, median (range), d |
3 (1–196) |
3 (1–162) |
0.01 |
| Length of ICU stay, mean (SD), h |
2 (±12.6) |
3 (±26.2) |
0.61 |
| ICU stay, intubated, No. (%) |
18 (1.4) |
12 (0.8) |
0.15 |
| Transfusions, No. (%) |
11 (0.9) |
8 (0.6) |
0.34 |
| Complications per patient, mean (SD) |
0.1 (±0.3) |
0.1 (±0.3) |
0.62 |
| Died during hospitalisation, No. (%) |
5 (0.4) |
14 (1.0) |
0.07 |
| NC = not calculated. ICU = intensive care unit. |
|
Table 3: Multivariate analysis of intraoperative, postoperative surgical and medical complications and outcome measures (n = 2,686). |
|
Characteristic
|
Odds ratio
|
95% CI
|
P-Value
|
| Complications:
Intraoperative complications |
|
|
|
| No intraoperative complications |
0.85 |
0.29–2.46 |
0.76 |
| Vessel injury |
0.88 |
0.12–6.27 |
0.90 |
| Other (e.g., splenic, vesical, hepatic injury) |
1.77 |
0.44–7.08 |
0.42 |
| Postoperative surgical complications |
|
|
|
| No postoperative surgical complications |
0.49 |
0.32–0.75 |
<0.01 |
| Bleeding |
0.53 |
0.13–2.22 |
0.38 |
| Surgical site infection |
4.88 |
1.08–22.07 |
0.04 |
| Intraabdominal abscess |
0.29 |
0.03–2.83 |
0.29 |
| Other (e.g., abdominal incision dehiscence, wound edge necrosis, residual gallstone, compartment syndrome) |
2.76 |
1.61–4.73 |
<0.01 |
| Postoperative medical complications |
|
|
|
| No postoperative medical complications |
1.65 |
1.10–2.47 |
0.02 |
| Pneumonia |
1.32 |
0.22–7.94 |
0.76 |
| Urinary tract infection |
0.35 |
0.07–1.82 |
0.21 |
| Other (e.g., cardiac or respiratory insufficiency, ileus, fever of unknown origin, allergic reaction, electrolyte imbalance) |
0.63 |
0.39–1.03 |
0.06 |
| |
|
|
|
| Outcome measures: |
|
|
|
| Length of hospital stay |
0.99 |
0.98–1.00 |
0.09 |
| Length of ICU stay |
1.01 |
1.00–1.02 |
0.02 |
| ICU stay, intubated |
0.26 |
0.08–0.84 |
0.02 |
|
Transfusions
|
0.62
|
0.23–1.73
|
0.36
|
| Complications per patient |
1.19 |
0.87–1.61 |
0.28 |
| Died during hospitalisation |
3.61 |
1.01–12.93 |
<0.05 |
| CI = confidence interval. ICU = intensive care unit. Due to small case counts, some complications were excluded in the multiple logistic regression analysis. |
Discussion
The present report describes a study among patients with common surgeries at a large referral Swiss hospital performed by residents to examine the impact of the 50-hour work-week limitation. It showed a significantly higher postoperative surgical complication and in-hospital mortality rate after the reform. No differences could be found concerning the overall intraoperative and postoperative medical complication frequencies. Thus, an improvement in patient safety was not found.
The finding of equal intraoperative complication rates before and after the reform is similar to a study in New York State teaching hospitals, where resident work-hour limits were not associated with improvements in surgical patient safety measures and even worsening trends observed in accidental puncture or laceration [33]. It is known that work-hour limitations may jeopardise resident education and patient care by worsening surgical training [23]. On the other hand, it has been shown that manual skills and operative performance in surgical residents may be affected by sleep deprivation [13]. Two simulated laparoscopy studies found significantly more errors and longer time to perform procedures on post-call mornings [15, 34]. They suggest an affect of sleep deprivation on psychomotor performance. Horne and Pettitt demonstrated that the overall situation is more complex than merely the performance of tasks, as sleep deprivation can be overcome by an incentive for better performance [35].
The higher postoperative surgical complication rate could not be confirmed by the results of previous publications. In a study on the frequency of postoperative surgical complications for residents who had been on call the previous night, no statistically significant difference was found [36]. Regarding the impact of fatigue, the results differ in the literature. Impaired performance equivalent to alcohol intoxication and alterations in mood have been described [8, 37]. On the other hand, it has been shown that eliminating interns’ extended work shifts and reducing the number of hours interns work per week can reduce serious medical errors in the intensive care unit [38, 39].
Although with the introduction of work-hour limitations concerns were expressed about less resident responsibility for the patient and about the development of a shift work mentality [6, 25], in agreement with others we did not find a significant change in the overall postoperative medical complication rate after the reform [17, 41, 42].
A possible reason for the lack of negative impact on the medical complication rate might be that errors due to transfer of care were counterbalanced by a decrease of complications due to less fatigue [17, 30].
The negative effect of transfers of care on complication frequencies has been shown by Laine et al. They found that restricted resident work hours in internal medicine were associated with delayed test ordering and higher rates of in-hospital complications [43]. Similarly, Petersen et al. showed that the patients’ risk for potentially preventable adverse events was increased when the patients were cross-covered by physicians from another team, particularly when the cross-covering physician was an intern [22].
As we found a higher in-hospital mortality rate after implementation of work-hour limitations, our results differ from those of previous studies, which found no conclusive evidence of a change in mortality rates [16, 17]. On the contrary, among high-risk medical patients in U.S. teaching hospitals the work-hour regulations were even associated with decreased short-term mortality [17]. The reasons behind the higher mortality rate remain elusive. The possibility that resident work-hour limit enforcement impaired the patient care cannot be ascertained.
A strength of this study is the quality assurance database of a large referral center as source of records. Swiss Hospitals may participate voluntarily in registering patients in this database. Data are used as a quality assessment tool and to identify their own strengths. Due to the high and continually growing number of participating hospitals, the database is complete. Assessing the quality of healthcare has become increasingly important around the world in the last decade [44].
As the present study is based on a database, there are several limitations. As the complication rates were recorded by residents, intra- and postoperative complication rates might be higher than indicated in our study [45]. Additionally, the AQC database is lacking on information about the level of training of the residents, which might influence the surgical care of patients. Furthermore, it does not provide information on the length of work shifts of residents and the operative exposure, respectively. As the work hours are indicated on a self-reporting basis, underreporting is probable, so we lack objective data [46]. This might affect the slight decrease of residents’ weekly work hours after introduction of the limitations, which is comparable to the findings of Zuckerman et al. [47–49]. The patients’ preoperative morbidity was compared in terms of age, sex, body mass index, American Society of Anesthesiologists fitness score, and malignant neoplasia. A further breakdown of preoperative co-morbidities was not performed. A selection bias due to more elective admissions before introduction of work-hour limitations cannot be excluded. A correlation of a higher postoperative morbidity with other factors after implementation of work hour limitations cannot be excluded. Additionally, as the absolute numbers regarding the complication and morbidity rates were low, a national study is essential. A link between cause and effect of the higher postoperative surgical complication and in-hospital mortality rate cannot be conclusively made. The AQC database is deficient in information about the 30-day mortality and re-hospitalisation rate in correlation with specific patients. Like any other retrospective analysis, this study has limitations, such as a selection and detection bias due to the manner in which data were originally collected. Finally, a performance bias due to an increase in patient turnover, fast-track surgery, perioperative nutritional considerations, and changes in the use of antibiotics cannot be excluded [50–52].
While most of surgeries were done by board-certified surgeons, in our study we analysed surgeries performed by residents only. We could show that neither the trend of the postoperative surgical complication rate nor that of the mortality rate differed between the two groups.
To our knowledge, this is the first study conducted to elucidate the effect of a 50-hour work-week limitation. It provides initial data that resident work hour limitations enforced in Switzerland were not associated with surgical patient safety measure improvement in common surgeries. Although the mortality and postoperative surgical complication rate were higher after introduction of the 50-hour work-week limitation, the mandated restriction of resident work hours had no measurable positive effect on the quality of patient care regarding the overall intra- and postoperative medical complication rates. Further research on a nationwide basis is needed to assess the value of the higher mortality and postoperative surgical complication rate and to verify the steady complication rates. To improve patient safety it seems to be crucial to better understand the conditions minimizing the possible negative effects of more frequent physician cross-coverings, while maximizing the benefits of reduced fatigue.
Acknowledgments: We thank Phillip Hendrickson, Ph.D., Basel, Switzerland, for critical reading of the manuscript.
References
1 SECO Web site. Application of the labour law to residents working in public hospitals [homepage on the internet]; c2007 [cited 2011 Nov 20]. Available from: http://www.seco.admin.ch/aktuell/00277/01164/01980/index.html?lang=de&msg-id=9333.
2 Pilot flight time and rest: fact sheet. Federal Aviation Administration, 2010 [homepage on the internet]; [cited 2011 Nov 20]. Available from: http://www.faa.gov/news/fact_sheets/news_story.cfm?newsId=6762.
3 Halsted WS. The training of the surgeon. Bull Johns Hopkins Hosp. 1904;15:267–75.
4 Wallack MK, Chao L. Resident work hours: the evolution of a revolution. Arch Surg. 2001;136:1426–32.
5 Drazen JM, Epstein AM. Rethinking medical training – the critical work ahead. N Engl J Med. 2002;347:1271–2.
6 Dawson D, Zee P. Work hours and reducing fatigue-related risk: good research vs good policy. JAMA. 2005;294:1104–6.
7 Philibert I, Friedmann P, Williams WT. New requirements for resident duty hours. JAMA. 2002;288:1112–4.
8 Dawson D, Reid K. Fatigue, alcohol and performance impairment [scientific correspondence]. Nature. 1997;388:235.
9 Firth-Cozens J, Greenhalgh J. Doctors’ perceptions of the links between stress and lowered clinical care. Soc Sci Med. 1997;44:1017–22.
10 Landrigan CP, Rothschild JM, Cronin JW, Kaushal R, Burdick E, Katz JT, et al. Effect of reducing interns’ work hours on serious medical errors in intensive care units. N Engl J Med. 2004;351:1838–48.
11 Weinger MB, Ancoli-Israel S. Sleep deprivation and clinical performance. JAMA. 2002;287:955–6.
12 Bernstein M, Etchells EE. Does reducing interns’ work hours reduce the rate of medical errors? CMAJ. 2005;172:474.
13 Goldman LI, McDonough MT, Rosemond GP. Stresses affecting surgical performance and learning. I. Correlation of heart rate, electrocardiogram, and operation simultaneously recorded on videotapes. J Surg Res. 1972;12:83–6.
14 Taffinder NJ, McManus IC, Gul Y, Russell RC, Darzi A. Effect of sleep deprivation on surgeons’ dexterity on laparoscopy simulator. Lancet. 1998;352:1191.
15 Grantcharov TP, Bardram L, Funch-Jensen P, Rosenberg J. Laparoscopic performance after one night on call in a surgical department: prospective study. BMJ. 2001;323:1222–3.
16 Volpp KG, Rosen AK, Rosenbaum PR, Romano PS, Even-Shoshan O, Wang Y, et al. Morality among hospitalized Medicare beneficiaries in the first 2 years following ACGME resident duty hour reform. JAMA. 2007;298:975–83.
17 Shetty KD, Bhattacharya J. Changes in hospital mortality associated with residency work-hour regulations. Ann Intern Med. 2007;147:73–80.
18 Rosen AK, Loveland SA, Romano PS, Itani KM, Silber JH, Even-Shoshan OO et al. Effects of resident duty hour reform on surgical and procedural patient safety indicators among hospitalized Veterans Health Administration and Medicare patients. Med Care. 2009;47:723–31.
19 Morrison CA, Wyatt MM, Carrick MM. Impact of the 80-hour work week on mortality and morbidity in trauma patients: an analysis of the National Trauma Data Bank. J Surg Res. 2009;154:157–62.
20 Gopaldas RR, Chu D, Dao TK, Huh J, LeMaire SA, Coselli JS, Bakaeen FG. Impact of ACGME work-hour restrictions on the outcomes of coronary artery bypass grafting in a cohort of 600,000 patients. J Surg Res. 2010;163:201–9.
21 De Virgilio C, Yaghoubian A, Lewis RJ, Stabile BE, Putnam BA. The 80-hour resident workweek does not adversely affect patient outcomes or resident education. Curr Surg. 2006;63:435–39.
22 Petersen LA, Brennan TA, O’Neil AC, Cook EF, Lee TH. Does housestaff discontinuity of care increase the risk for preventable adverse events. Ann Intern Med. 1994;121:866–72.
23 Whang EE, Mello MM, Ashley SW, Zinner MJ. Implementing resident work hour limitations: lessons from the New York State experience. Ann Surg. 2003;237:449–55.
24 Fischer JE. Continuity of care: a casualty of the 80-hour work week. Acad Med. 2004;79:377–8.
25 Hutter MM, Kellogg KC, Ferguson CM, Abbott WM, Warshaw AL. The impact of the 80-hour resident workweek on surgical residents and attending surgeons. Ann Surg. 2006;243:864–71.
26 Payette M, Chatterjee A, Weeks WB. Cost and workforce implications of subjecting all physicians to aviation industry work-hour restrictions. Am J Surg. 2009;197:820–5.
27 Kaderli R, Buser C, Stefenelli U, Businger A. Students’ interest in becoming a general surgeon before and after a surgical clerkship in German-speaking Switzerland. Swiss Med Wkly. 2011 Aug 15;141:w13246. doi: 10.4414/smw.2011.13246.
28 Buddeberg-Fischer B, Stamm M. The medical profession and young physicians’ lifestyles in flux: challenges for specialty training and health care delivery systems. Swiss Med Wkly. 2010;140:w13134. doi: 10.4414/smw.2010.13134.
29 Knecht M, Bauer GF, Klaghofer R, Buddeberg-Fischer B, Stamm M, Hämmig O. Work-life conflicts and health among Swiss physicians – in comparison with other university graduates and with the general Swiss working population. Swiss Med Wkly. 2010;140:w13063. doi: 10.4414/smw.2010.13063.
30 Businger A, Guller U, Oertli D. Effect of the 50-hour workweek limitation on training of surgical residents in Switzerland. Arch Surg. 2010;145:558–63.
31 Weiterbildungsstätten – qualitätsorientierte Kriterien. Swiss Medical Association (FMH) [homepage on the internet]; c2011 [cited 2011 Nov 20]. Available from: http://www.fmh.ch/files/pdf6/wbs_chirurgie.pdf.
32 AQC Web site [homepage on the internet]; c2011 [cited 2011 Nov 20]. Available from: http://www.aqc.ch/Willkommen-bei-der-AQC.aspx.
33 Poulose BK, Ray WA, Arbogast PG, et al. Resident work hour limits and patient safety. Ann Surg. 2005;241:847–56.
34 Taffinder N. Better surgical training in shorter hours. J R Soc Med. 1999;92:329–31.
35 Horne JA, Pettitt AN. High incentive effects on vigilance performance during 72 hours of total sleep deprivation. Acta Psychol (Amst). 1985;58:123–39.
36 Haynes DF, Schwedler M, Dyslin DC, Rice JC, Kerstein MD. Are postoperative complications related to resident sleep deprivation? South Med J. 1995;88:283–9.
37 Bartle EJ, Sun JH, Thompson L, Light AI, McCool C, Heaton S. The effects of acute sleep deprivation during residency training. Surgery. 1988;104:311–6.
38 Landrigan CP, Rothschild JM, Cronin JW, Kaushal R, Burdick E, Katz JT, et al. Effect of reducing interns' work hours on serious medical errors in intensive care units. N Engl J Med. 2004;351:1838–48.
39 Lockley SW, Cronin JW, Evans EE, Cade BE, Lee CJ, Landrigan CP, et al. Effect of reducing interns’ weekly work hours on sleep and attentional failures. N Engl J Med. 2004;351:1829–37.
40 Warshaw AL, Sarr MG. The now and future world of restricted work hours for surgeons. Surgery. 2003;134:1–2.
41 Ellman PI, Law MG, Tache-Leon C, Reece TB, Maxey TS, Peeler BB, et al. Sleep deprivation does not affect operative results in cardiac surgery. Ann Thorac Surg. 2004;78:906–11.
42 Kaafarani HM, Itani KM, Petersen LA, Thomby J, Berger DH. Does resident hours reduction have an impact on surgical outcomes? J Surg Res. 2005;126:167–71.
43 Laine C, Goldman L, Soukup JR, Hayes JG. The impact of a regulation restricting medical house staff working hours on the quality of patient care. JAMA. 1993;269:374–8.
44 Groene O, Skau JK, Frølich A. An international review of projects on hospital performance assessment. Int J Qual Health Care. 2008;20:162–71.
45 Dindo D, Hahnloser D, Clavien PA. Quality assessment in surgery: riding a lame horse. Ann Surg. 2010;251:766–71.
46 Mache S, Kelm R, Bauer H, Nienhaus A, Klapp BF, Groneberg DA. General and visceral surgery practice in German hospitals: a real-time work analysis on surgeons’ work flow. Langenbecks Arch Surg. 2010;395(1):81–7.
47 Macgregor JM, Sticca R. General surgery residents’ view on work hours regulations. J Surg Educ. 2010;67:376–80.
48 Todd SR, Fahy BN, Paukert JL, Mersinger D, Johnson ML, Bass BL. How accurate are self-reported resident duty hours? J Surg Educ. 2010;67:103–7.
49 Zuckerman JD, Kubiak EN, Immerman I, Dicesare P. The early effects of code 405 work rules on attitudes of orthopaedic residents and attending surgeons. J Bone Joint Surg Am. 2005;87(4):903–8.
50 Wilmore DW, Kehlet H. Management of patients in fast track surgery. BMJ. 2001;322:473–6.
51 Paillaud E, Bories PN, Le Parco JC, Campillo B. Nutritional status and energy expenditure in elderly patients with recent hip fracture during a 2-month follow up. Br J Nutr. 2000;83:97–103.
52 Kanter G, Connelly NR, Fitzgerald J. A system and process redesign to improve perioperative antibiotic administration. Anesth Analg. 2006;103:1517–21.