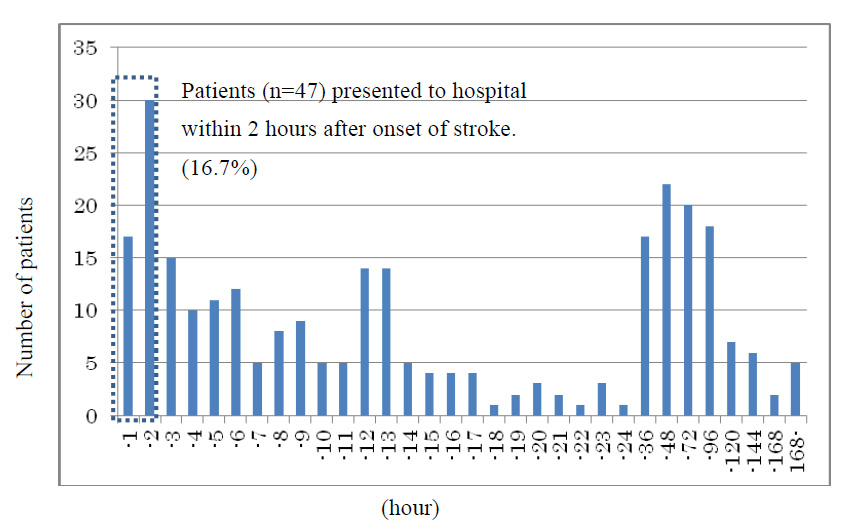
Figure 1
Distribution of time to presenting to hospital from onset of stroke symptoms.
DOI: https://doi.org/10.4414/smw.2011.13296
A hospital-based study in Japan
Despite the fact that use of recombinant tissue plasminogen activator (rt-PA) for intravenous thrombolytic treatment of acute stroke was approved in 1996 in the United States, its approval was delayed by 9 years (until 2005) in Japan. Therapy with rt-PA is highly effective for treating stroke but is only available to patients within 3 hours after onset of stroke symptoms. Because of this 3-hour treatment window, according to Nakagawara et al., only around 2–3% of stroke patients are treated with rt-PA in Japan [1]. One of the reasons for this delayed treatment is the shortage of medical institutions that are open for acute treatment 24 hours a day [1]. The approval of rt-PA has therefore shown the need for an increase in the number of trained specialists capable of treating hyperacute stroke and the establishment of stroke care systems and facilities, such as 24-hour medical institutions, stroke care units, and similar facilities, as well as a regional acute stroke care network [2]. In addition, previous studies performed outside Japan have shown that patient social factors, such as insufficient awareness of stroke symptoms [3], absence of a witness of stroke onset [4–6], past history [7], and poor accessibility to an appropriate hospital [8–9], are associated with the delayed initiation of stroke treatment.
To date, however, such epidemiologic studies in Japan are limited. This study aims to investigate multifaceted factors that constrain early stroke treatment, from both clinical and social standpoints, by using the data of patients who were presented to a particular hospital.
Subjects were all stroke patients who were hospitalised at the Center for Stroke and Neuroscience of Southern Tohoku General Hospital (Koriyama City, Fukushima Prefecture) between October 2009 and March 2010. Koriyama City is situated in the center of Fukushima Prefecture and is a hub of the high-speed traffic network with about 338,000 people living in a 760-km2 area. The total number of beds at this general hospital is 449. The Center for Stroke and Neuroscience, comprising the Neurosurgery Department and the Neurology Department, received 2,512 inpatient admissions and had 200 mean daily outpatient visits in 2009.
The following relevant characteristics and clinical details of patients were extracted retrospectively from electronic medical records kept at both departments and from hospital forms filled in by patients or their family on arrival at the hospital: age; gender; household composition (including age of occupants); risk factors for stroke (smoking history, hypertension, dyslipidemia, diabetes, stroke history and atrial fibrillation); medical history (kept by the hospital); time of onset of stroke symptoms; type of presentation to hospital (emergency or non-emergency) after the most recent stroke; stroke severity according to the Japan Coma Scale (JCS) and the National Institutes of Health Stroke Scale (NIHSS); major clinical category; infarct territory; treatment provided; and outcome after stroke according to the Modified Rankin Scale (mRS). The distance between the hospital and the residence of each patient was obtained using an address-based internet distance calculator on the Mapfan website [10]. The time to presenting to hospital was defined as the difference between the last known time without stroke symptoms and the time of arrival as noted in electronic medical records.
rt-PA is only considered for treating stroke patients within 3 hours of onset. Considering that roughly 1 hour is required for several examinations (i.e., computed tomography (CT), magnetic resonance imaging (MRI), and blood testing) before starting rt-PA administration [8], we used an onset-to- presentation time of 2 hours as the admission window to meet the 3-hour window for rt-PA treatment. Thus, in this study, the 2-hour window for hospital presentation was used as an outcome variable in multiple logistic regression analysis, which was performed using the data of all patients and that of a subset of patients with their first stroke who lived within a 32-km (20-mile) radius of the hospital and could thus potentially access the hospital within 2 hours.
Statistical analysis was performed using SPSS 17.0J software. Statistically significant variables (p value <0.05) were further examined by multiple logistic regression analysis. This study was approved by the Ethics committees of Fukushima Medical University (registration number 1111) and the Southern Tohoku General Hospital (registration number 68).
The mean age of the 287 patients was 74.4 years, and 59.6% were male. The distribution of time to presenting to hospital was multimodal (fig. 1) with a median value of 12 hours (range, 0.4–347 hours). When the last known time without stroke symptoms was uncertain (133 cases), a time of 0:00, 6:00, 12:00, or 18:00 was chosen, whichever was closest to the approximate recorded time, which is a useful approach when presumed stroke onset was “at dawn“ or “during the evening”. Forty-seven patients (16.7%) presented to the hospital within the 2-hour window. Atherothrombotic brain infarction was the most common clinical category and found in 44.3% (n = 127) of the patients. A total of 163 patients (56.8% of total) were in a clear conscious state (JCS = 0), and most of them complained only of paralysis.
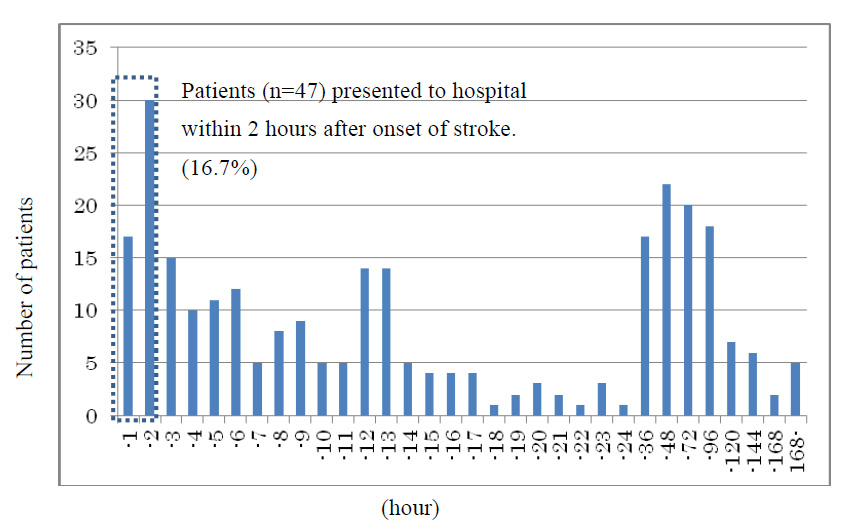
Figure 1
Distribution of time to presenting to hospital from onset of stroke symptoms.
Table 1 shows the results of univariate analysis performed using the data of all patients. The time to presenting to hospital beyond the 2-hour window showed an association (p <0.1) living with a spouse (odds ratio (OR) = 0.53), admission history (OR = 0.50), road or air ambulance service (OR = 0.12), history of stroke (OR = 0.54), cardiogenic cerebral embolism (OR = 0.28), and a JCS score of ≥1 (OR = 0.4). Multivariate analysis showed a significant level of association with a JCS score of ≥1 (OR = 0.41) and cardiogenic cerebral embolism (OR = 0.36) (table 2). When treatment given and outcome after a stroke were examined, the proportion of patients treated with rt-PA (p = 0.00), those with a mRS score of ≥2 (p = 0.04), and those in a rehabilitation hospital/long-term care ward or who died (p = 0.00) was significantly higher among patients who presented to the hospital within the 2-hour admission window than in those who missed this window (table 3).
Table 4 shows the results of multivariate analysis performed similarly and using the data of the first stroke of the subset of patients who lived within a 32-km (20-mile) radius from the hospital. Cardiogenic cerebral embolism and a JCS score of ≥1 showed a significant association with the time to presenting to hospital. When treatment given and outcome after a stroke, were examined, the proportion of patients treated with rt-PA was significantly higher while that of patients discharged was significantly lower in the patients who presented to hospital within the 2-hour window than in those who missed this window. These results are consistent with the findings of multivariate analysis using the data of all patients (table 5).
| Table 1: Association between time to presenting to hospital and patient characteristics: Univariate analysis using data of all patients. | |||||||
| Time to presenting to hospital from stroke onset: N (%) a | |||||||
| <120 min N = 47 | ≥120 min N = 235 | p-value d | Exp(B) f | 95%CI g | |||
| Basic characteristics | |||||||
| Age (≥65 years) | 38 (80.9) | 179 (76.2) | 0.49 | 0.76 | 0.35 | – | 1.66 |
| Gender (male) | 33 (70.2) | 136 (70.2) | 0.12 | 1.72 | 0.87 | – | 3.38 |
| Household composition | |||||||
| Live with a spouse | 31 (72.1) | 131 (58.0) | 0.09 | 0.53 | 0.26 | – | 1.09 |
| Live with somebody | 41 (93.2) | 197 (87.2) | 0.27 | 0.50 | 0.15 | – | 1.71 |
| Live with somebody ≥20 years old | 29 (65.9) | 156 (69.0) | 0.68 | 1.15 | 0.58 | – | 2.29 |
| Hospital admission related | |||||||
| Previous admission(s) to the hospital | 21 (45.7) | 69 (29.5) | 0.03 | 0.50 | 0.26 | – | 0.95 |
| Means of transport to the hospital (emergencyb) | 37 (80.9) | 91 (38.7) | 0.00 | 0.12 | 0.05 | – | 0.27 |
| Address within a 32-km radius of the hospitalc | 38 (82.6) | 181 (77.4) | 0.43 | 1.39 | 0.61 | – | 3.16 |
| Lifestyle | |||||||
| Smoking history | 11 (26.8) | 88 (39.8) | 0.12 | 1.81 | 0.86 | – | 3.79 |
| Medical history | |||||||
| Hypertension | 35 (74.5) | 159 (67.9) | 0.38 | 0.73 | 0.36 | – | 1.48 |
| Dyslipidemia | 12 (25.5) | 48 (20.5) | 0.45 | 0.75 | 0.36 | – | 1.56 |
| Diabetes | 12 (25.5) | 51 (21.8) | 0.58 | 0.81 | 0.39 | – | 1.68 |
| Stroke | 21 (44.7) | 71 (30.3) | 0.06 | 0.54 | 0.29 | – | 1.02 |
| Atrial fibrillation | 13 (27.7) | 46 (19.7) | 0.22 | 0.64 | 0.31 | – | 1.31 |
| Clinical category | |||||||
| Major clinical category | |||||||
| Atherothrombotic brain infarction | 14 (29.8) | 113 (48.1) | 1.00 | ||||
| Lacunar infarction | 8 (17.0) | 47 (19.1) | 0.80 | 0.87 | 0.30 | – | 2.50 |
| Cardiogenic cerebral embolism | 18 (38.3) | 42 (17.9) | 0.00 | 0.28 | 0.12 | – | 0.65 |
| Other | 7 (14.9) | 35 (14.9) | 0.81 | 1.18 | 0.31 | – | 4.50 |
| Infarct territorye | |||||||
| IC | 1 (2.1) | 6 (2.6) | 0.86 | 1.21 | 0.14 | – | 10.25 |
| ACA | 5 (10.6) | 13 (5.5) | 0.20 | 0.49 | 0.17 | – | 1.45 |
| MCA | 31 (66.0) | 155 (66.0) | 1.00 | 1.00 | 0.52 | – | 1.94 |
| PCA | 5 (10.6) | 26 (11.1) | 0.93 | 1.05 | 0.38 | – | 2.88 |
| BA-VA | 4 (8.5) | 38 (16.2) | 0.19 | 2.07 | 0.70 | – | 6.12 |
| JCS stroke severity level | |||||||
| JCS = 0 | 18 (38.3) | 143 (60.9) | 1.00 | ||||
| JCS ≥1 | 29 (61.7) | 92 (39.1) | 0.01 | 0.40 | 0.21 | – | 0.76 |
| a Column values for some items do not add up to the total number indicated in the top row because of missing data. b Emergency transport includes that by means of road or air ambulance service, while non-emergency transport is by family car or taxi and includes in-hospital onset. c The distance between each patient’s residence and the hospital was calculated, and a 32-km distance was used as a cut-off value to reach the hospital within 60 min6). d The time to presenting to hospital was used as the independent variable, and patient characteristics were used as explanatory variables for logistic regression analysis. e Because some patients had infarct in multiple territories, infarct territories were individually analysed. f Odds ratio g 95% confidence interval | |||||||
| Table 2: Association between time of arrival to hospital from onset and patient characteristics: Multivariate analysis using data of all patients. | |||||
| p-value a | Exp(B) b | 95%CI c | |||
| Live with a spouse | 0.06 | 0.48 | 0.22 | – | 1.02 |
| Previous admission to the hospital | 0.08 | 0.48 | 0.21 | – | 1.08 |
| Previous onset of stroke symptoms | 0.66 | 1.21 | 0.52 | – | 2.81 |
| JCS score of ≥1 | 0.02 | 0.41 | 0.20 | – | 0.86 |
| Major clinical category: cardiogenic cerebral embolism | 0.02 | 0.36 | 0.15 | – | 0.85 |
| a The time to presenting to hospital was used as the independent variable and patient characteristics at p <0.1 in table 1 were used as explanatory variables for multiple logistic regression analysis. Means of transport to the hospital was not included as an explanatory variable because the time taken to make a decision for an emergency visit is almost equivalent to a visit within 120 minutes. b Odds ratio c 95% confidence interval | |||||
| Table 3: Outcome of all patients in relation with time to presenting to hospital. | |||
| Time of admission to hospital N(%) a | |||
| <120 min N = 47 | ≥120 min N = 235 | p-value a | |
| Drugs used for treatmentb | |||
| rt-PA | 9 (19.1) | 0 (0.0) | 0.00 |
| Argatroban | 9 (19.1) | 61 (26.0) | 0.36 |
| Ozagrel Na | 12 (25.5) | 86 (36.6) | 0.18 |
| Heparin | 21 (44.7) | 83 (35.3) | 0.25 |
| Edaravone | 31 (66.0) | 119 (50.6) | 0.06 |
| Outcome | |||
| mRS | |||
| 0–1 | 15 (31.9) | 114 (48.5) | 0.04 |
| 2–6 | 32 (68.1) | 121 (51.5) | |
| Discharged toc: | |||
| Home | 19 (40.4) | 162 (68.9) | 0.00 |
| Rehabilitation hospital | 14 (29.8) | 42 (17.9) | |
| Long-term care ward | 11 (23.4) | 22 (9.4) | |
| Death | 3 (6.4) | 9 (3.8) | |
| a Chi square test or Fisher’s exact test was used. b Because multiple drugs were used in some patients, drugs were individually analysed. c p value for the discharge site was calculated by dichotomising the variable into home or others. | |||
| Table 4: Time to presenting to hospital and patient characteristics: Multivariate analysis using data of patients with a first stroke within a 32-km radius. | |||||||
| Time of admission to hospital N(%) a | |||||||
| <120 min N = 21 | ≥120 min N = 121 | p-value a | Exp(B) b | 95%CI c | |||
| Major clinical category | |||||||
| Atherothrombotic brain infarction | 6 (28.6) | 58 (47.9) | 1.00 | ||||
| Lacunar infarction | 4 (19.0) | 29 (24.0) | 0.63 | 0.77 | 0.26 | – | 2.25 |
| Cardiogenic cerebral embolism | 9 (42.9) | 20 (16.5) | 0.01 | 0.34 | 0.14 | – | 0.80 |
| Others | 2 (9.5) | 14 (11.6) | 0.72 | 1.29 | 0.33 | – | 5.00 |
| JCS(≥1) | 14 (66.7) | 43 (35.5) | 0.02 | 0.41 | 0.19 | – | 0.89 |
| a The time to presenting to hospital was used as the independent variable and patient characteristics with p <0.1 in table 1 were used as explanatory variables for multiple logistic regression analysis. A means of transport to the hospital was not included in explanatory variables, because the time taken to make a decision for an emergency visit is almost equivalent to a visit within 120 minutes. b Odds ratio c 95% confidence interval | |||||||
| Table 5: Outcome of patients with a first stroke within a 32-km radius. | |||
| Time to presenting to hospital N(%) a | |||
| <120 min N = 21 | ≥120 min N = 121 | p-value a | |
| Drugs used for treatmentb | |||
| rt-PA | 7 (100.0) | 0 (0.0) | 0.00 |
| Argatroban | 4 (19.0) | 34 (28.1) | 0.59 |
| Ozagrel Na | 5 (23.8) | 46 (38.0) | 0.32 |
| Heparin | 10 (47.6) | 39 (32.2) | 0.22 |
| Edaravone | 15 (71.4) | 65 (53.7) | 0.16 |
| Outcome | |||
| mRS | |||
| 0–1 | 7 (33.3) | 56 (46.3) | 0.34 |
| 2–6 | 14 (66.7) | 65 (53.7) | |
| Discharged toc: | |||
| Home | 7 (33.3) | 82 (67.8) | 0.00 |
| Rehabilitation hospital | 7 (33.3) | 25 (20.7) | |
| Long-term care ward | 6 (28.6) | 10 (8.3) | |
| Death | 1 (4.8) | 4 (3.3) | |
| a Chi square test or Fisher’s exact test was used. b Because multiple drugs were used in some patients, drugs were individually analysed. c p value for the discharge site was calculated by dichotomising the variable into home or others. | |||
| Table 6: Summary of findings related to the time to presenting to hospital from the onset of stroke symptoms. | |||
| Country | Sample size | Results | Reference |
| Japan | 287 | Mean time to reach hospital was 725 min (12 h). To compare with other studies, the proportion of patients who reached hospital within 2, 3, and 6 h was 16.7%, 22.0%, and 33.7%, respectively. | This study |
| Japan | 130 | Mean time was 7.5 h (min. 2.0, max. 31.8), and 30% visited hospitals within 2 h. | 11) |
| Japan | 16922 | 36.8% visited hospitals within 3 h, and 49.5 within 6 h. | 12) |
| Sweden | 329 | Mean time was 5.1 h among stroke patients, and 4.0 h among TIA patients. | 13) |
| Finland | 363 | 43% visited hospitals within 6 h. | 14) |
| Australia | 198 | Mean time to call an ambulance was 53 min (min. 15, max. 251), and mean time to reach hospital was 99 minutes (min. 59, max. 309). | 7) |
| United States | 151 | Average time to reach hospital was 5.7 h (min. 1.8, max. 21.4). | 15) |
It is noteworthy that only 16.7% of stroke patients in this study presented to hospital within the 2-hour window. This figure is lower than that found in previous studies carried out in Japan and overseas (table 6). Besides the analysed patient characteristics, hospital characteristics may have also contributed to this low figure. Southern Tohoku General Hospital is the core hospital for the treatment of stroke in the region and offers MRI examinations 24 hours a day to all stroke patients, except those with a pacemaker. Because MRI can detect minor strokes that cannot be detected by CT, it is likely that our inpatients include those with more minor strokes and who have a low degree of sensory dysfunction and minor difficulties in daily activities and who, therefore, tend to delay a hospital visit, when compared with those at hospitals using only CT [8, 12]. Furthermore, with Japan’s universal medical care insurance system that provides all citizens access to adequate medical care, more stroke patients without difficulties in daily activities are likely to visit a hospital and undergo MRI examination in Japan than such patients in other countries. According to a study carried out in the United States, 5% of patients with transient ischemic attack (TIA) underwent an MRI examination at an emergency outpatient department, and only 54% were hospitalised for treatment of TIA [16]. On the other hand, we perform MRI in all patients with suspected TIA and minor stroke, unless contraindicated, and offer inpatient treatment to these patients, albeit with a shorter hospital stay than that required for the treatment of severe stroke. Indeed, our findings with respect to stroke outcome (table 3) reflect a high proportion of minor stroke in patients with delayed presentation to hospital.
As described above, the absence of major difficulties in everyday activities is one of the reasons for delayed hospitalisation among patients with minor stroke. One may argue that hospitalisation is not necessary for some of these patients; however, given the possible aggravation of symptoms, the benefits of urgent treatment for TIA and minor stroke have already been demonstrated [17, 18]. Indeed, 36% of patients in this study who had a clear conscious state (JCS = 0) at the time of presentation became handicapped (mRS of 2–6) following stroke. Risk factors for aggravation of symptoms after TIA and minor stroke include the following: >65 years of age; diabetes; hypertension; hemiplegia; speech disorders; and prolonged TIA symptoms of >1 hour [19]. When such risk factors exist, it is important that stroke patients, even those with minor symptoms, are admitted promptly for evaluation to ensure that inpatient treatment is received. All suspected stroke patients in this study, except those with a pacemaker, were examined by MRI, resulting in a high detection rate of minor stroke which has little impact on everyday life. Although therapy similar to that for stroke is so far favoured [18–20], a detailed risk factor assessment is needed to proactively treat patients with minor but potentially serious symptoms without unnecessary hospitalisation.
It has been shown that patients with cardiogenic cerebral embolism, who presented with acute onset of symptoms, visited a hospital at the early stage after onset (tables 2 and 4). This finding is consistent with the results shown in a previous study [5] and indicates that obvious sudden onset of paralysis, disturbances of consciousness, and dysarthria encourages these patients to go to a hospital sooner rather than later.
Several studies have indicated that the time of hospital admission after stroke onset tends to be longer in patients who live alone than in those who live with somebody [4–6]. However, no association between the time to presenting to hospital and household composition was found in this study. Koriyama City is located in the northern part of Japan and has a traditional community structure, and only 32 of 287 patients (11.1%) in this study lived alone. In addition, this close-knit society is more prominent in agricultural regions than in populated regions, and thus stroke symptoms may be detected at an early stage after onset in the region investigated in this study, regardless of household composition. Nevertheless, in the future more residents are expected to live alone, even in Japanese agricultural regions. Therefore, it is important to monitor the influence of household composition on the time to presenting to hospital.
There are three limitations regarding the present study. First, the study subjects were inpatients at one hospital in northern Japan, and findings only reflect the household situation of that particular region. Secondly, this is an observational study using retrospectively collected data, and thus information on some factors associated with patient health, such as history of alcohol consumption and existing medications, was not available. Also, the type of informant was not recorded, and we could not assess the extent of misclassification that occurred based on family member reports of patient information, including the outcome indicator of timing of onset. Lastly, despite the NIHSS being the internationally recognised scale for evaluating stroke severity [21], medical records often did not contain NIHSS-related information. Thus, the JCS, the most commonly used scale in Japan, was used. Given the above limitations, the results from the multivariate analysis do not definitively identify associations, but rather are only suggestive of associations. A multicenter study that employs a more detailed questionnaire, which is designed for a prospective data collection, and involves stroke patients living in both urban and agricultural regions is necessary in the future.
The time to presenting to hospital from the onset of stroke symptoms was investigated at a core hospital in Koriyama City, Fukushima Prefecture. Although our results are preliminary; given their limited generalisability and the retrospective nature of data collection, it is noteworthy that only 16.7% of stroke patients presented to hospital within 2 hours of onset. Multivariate analysis revealed that, rather than social factors, medical factors related to a low severity of a stroke which does not disturb a clear conscious state is significantly associated with presenting to hospital more than 2 hours after onset. Because minor stroke symptoms can be aggravated, it is important to promote the earliest possible admission to hospital after stroke.
Acknowledgement: We thank Drs. Teiji Yamamoto and Shinya Shimoji and the hospital staff at Southern Tohoku General Hospital for their help in data collection. We are also grateful to ThinkSCIENCE K.K., Tokyo, for providing language support.
1 Nakagawara J. Present state of stroke emergency in Japan. Brain Nerve. 2010;62(1):25–34.
2 Stop! Stroke. http://www.jsa-web.org/ (in Japanese)
3 Pancioli AM, Broderick J, Kothari R, Brott T, Tuchfarber A, Miller R, et al. Public perception of stroke warning signs and knowledge of potential risk factors. JAMA. 1998;279(16):1288–92.
4 Casetta I, Granieri E, Gilli G, Lauria G, Tola MR, Paolino E. Temporal trend and factors associated with delayed hospital admission of stroke patients. Neuroepidemiology. 1999;18(5):255–64.
5 Moser DK, Kimble LP, Alberts MJ, Alonzo A, Croft JB, Dracup K, et al. Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke: a scientific statement from the American Heart Association Council on cardiovascular nursing and stroke council. Circulation. 2006;114(2):168–82. Epub 2006 Jun 26.
6 Tanaka Y, Nakajima M, Hirano T, Uchino M. Factors influencing pre-hospital delay after ischemic stroke and transient ischemic attack. Intern Med. 2009;48(19):1739–44. Epub 2009 Oct 1.
7 Mosley I, Nicol M, Donnan G, Patrick I, Dewey H. Stroke symptoms and the decision to call for an ambulance. Stroke. 2007;38(2):361–6. Epub 2007 Jan 4.
8 Scott PA, Temovsky CJ, Lawrence K, Gudaitis E, Lowell MJ. Analysis of Canadian population with potential geographic access to intravenous thrombolysis for acute ischemic stroke. Stroke. 1998;29(11):2304–10.
9 Kleindorfer D, Xu Y, Moomaw CJ, Khatri P, Adeoye O, Hornung R. US geographic distribution of rt-PA utilization by hospital for acute ischemic stroke. Stroke. 2009;40(11):3580–4. Epub 2009 Oct 1.
10 Increment P Corporation. MapFan Web. http://www.mapfan.com/routemap/routeset.cgi
11 Iguchi Y, Wada K, Shibazaki K, Inoue T, Ueno Y, Yamashita S, Kimura K. First impression at stroke onset plays an important role in early hospital arrival. Intern Med. 2006;45(7):447–51. Epub 2006 May 1.
12 Kimura K, Kazui S, Minematsu K, Yamaguchi T. Japan Multicenter Stroke Investigator's Collaboration. Analysis of 16,922 patients with acute ischemic stroke and transient ischemic attack in Japan. A hospital-based prospective registration study. Cerebrovasc Dis. 2004;18(1):47–56. Epub 2004 Jun 1.
13 Wester P, Rådberg J, Lundgren B, Peltonen M. Factors associated with delayed admission to hospital and in-hospital delays in acute stroke and TIA: a prospective, multicenter study. Seek- Medical-Attention-in-Time Study Group. Stroke. 1999;30(1):40–8.
14 Fogelholm R, Murros K, Rissanen A, Ilmavirta M. Factors delaying hospital admission after acute stroke. Stroke. 1996;27(3):398–400.
15 Kothari R, Jauch E, Broderick J, Brott T, Sauerbeck L, Khoury J, Liu T. Acute stroke: delays to presentation and emergency department evaluation. Ann Emerg Med. 1999;33(1):3–8.
16 Edlow JA, Kim S, Pelletier AJ, Camargo CA Jr. National study on emergency department visits for transient ischemic attack, 1992–2001. Acad Emerg Med. 2006;13(6):666–72. Epub 2006 Apr 11.
17 Rothwell PM, Giles MF, Chandratheva A, Marquardt L, Geraghty O, Redgrave JN, et al. Early use of Existing Preventive Strategies for Stroke (EXPRESS) study. Effect of urgent treatment of transient ischaemic attack and minor stroke on early recurrent stroke (EXPRESS study): a prospective population-based sequential comparison. Lancet. 2007;370(9596):1432–42.
18 Luengo-Fernandez R, Gray AM, Rothwell PM. Effect of urgent treatment for transient ischaemic attack and minor stroke on disability and hospital costs (EXPRESS study): a prospective population-based sequential comparison. Lancet Neurol. 2009;8(3):235–43. Epub 2009 Feb 4.
19 Johnston SC, Rothwell PM, Nguyen-Huynh MN, Giles MF, Elkins JS, Bernstein AL, et al. Validation and refinement of scores to predict very early stroke risk after transient ischaemic attack. Lancet. 2007;369(9558):283–92.
20 Lavallée PC, Meseguer E, Abboud H, Cabrejo L, Olivot JM, Simon O, et al. A transient ischaemic attack clinic with round-the-clock access (SOS-TIA): feasibility and effects. Lancet Neurol. 2007;6(11):953–60.
21 Nedeltchev K, Renz N, Karameshev A, Haefeli T, Brekenfeld C, Meier N, et al. Predictors of early mortality after acute ischaemic stroke. Swiss Med Wkly. 2010;140(17-18):254–9.
Funding / potential competing interests:We confirm that there are no known conflicts of interest associated with this publication and that no significant financial support that could have influenced the outcome of our study has been received.
Authors’ contribution: CK designed the study, collected data, performed statistical analysis, and wrote the manuscript. AG gave insightful comments in relation to the study design and statistical analysis, and contributed in finalising the manuscript. SY supervised the study and gave insightful comments in relation to statistical analysis and manuscript writing.