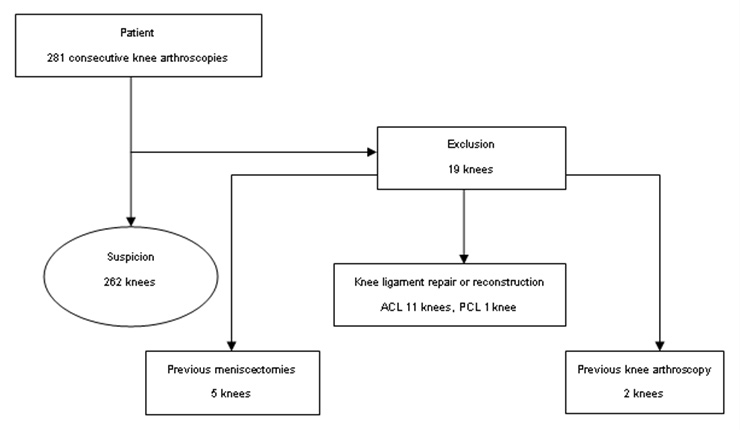
Figure 1
Diagram of patients enrolled in the study.
DOI: https://doi.org/10.4414/smw.2011.13314
Meniscus tears, seen in young and old patients alike, are an extremely common cause of knee pain [1]. Incidental meniscal findings on magnetic resonance imaging (MRI) of the knee are common in the general population and increase with increasing age. Among persons with radiographic evidence of osteoarthritis (Kellgren-Lawrence grade 2 or higher), the prevalence of a meniscal tear was found to be higher than the corresponding prevalence among persons without radiographic evidence of osteoarthritis [2]. Arthroscopic surgery in patients with moderate-to-severe osteoarthritis of the knee provides no additional benefit to optimised physical and medical therapy [3]. It is important to make an accurate diagnosis of meniscus tears so that the appropriate treatment can be given. A detailed history and physical examination can help differentiate patients who have a meniscus tear from those whose knee pain arises from other conditions [4–6]. MRI is the test commonly used on patients with meniscus tears of the knee because of its ability to diagnose meniscal tears [7–9]. MRI is commonly used because various intra-articular lesions historically have had common symptoms, patient history alone is in adequate as a diagnostic tool, and the diagnostic accuracy of clinical tests for meniscal tears has often been questioned. A review of the available literature reveals conflicting results as to their usefulness [10–15]. If the patient had no clinical symptoms, even though MRI showed meniscal tears of a patient, knee arthroscopy was unnecessary. In a high percentage of cases, relying on MRI alone without using clinical judgment may have led to inappropriate treatment. In any case, MRI did not prevent “unnecessary surgery” [16]. The aims of this study were to identify sensitive and specific clinical tests and elements of patients’ history with high predictive value, and to assess the combined diagnostic accuracy of sensitive and specific clinical tests and elements of patients’ history with MRI by using arthroscopy as a gold standard for control.
Institutional review board approval was obtained before beginning the study, allowing a retrospective review of patient records and images without informed consent.
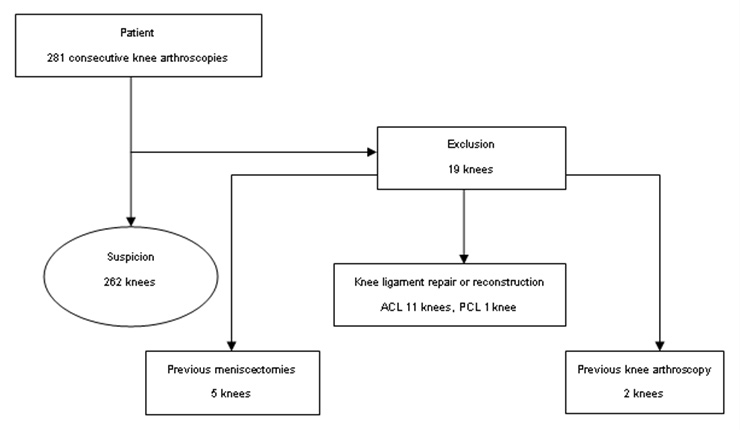
Figure 1
Diagram of patients enrolled in the study.
We retrospectively collected data from 281 consecutive knee arthroscopies performed by 2 experienced knee surgeons between March 2009 and April 2010 to investigate and treat suspected internal knee pathologies [17]. A total of 19 knees which had had previous meniscectomies, knee ligament repair, or reconstruction and knee arthroscopy were excluded from the study (fig. 1). The study group consisted of 262 knees and their medical records were subsequently reviewed for relevant clinical history, MRI reports and operative findings. There were 115 male and 135 female patients in the age group of 7–78 years, with a median age of 41. There were 138 (53%) left knees and 124 (47%) right knees in the study group. The mechanisms of tear for the 262 knees included beyond recall (88 knees, 33.59%), twisting (101 knees, 38.55%), jumping–landing (39 knees, 14.88%), trauma (29 knees, 11.07%), and valgus–varus stress (5 knees, 1.91%).
Clinical data (including patient demographics, waiting period between MRI and arthroscopy), suggestive symptoms (including pain, swelling, limited motion, giving way locking, and clicking), physical examination, mechanism of tear, clinical diagnosis and operative details were reviewed and analysed. Clinical tests included quadriceps atrophy, joint line tenderness test, induration around knee joint, varus or valgus deformity, lack of flexion or extension, floating patella test, Soto-holl test, Apley’s test, McMurray’s test, Kellogg-Speed test, pain on hyperextension and pain on hyperflexion.
All MRI examinations were performed at our institution with a 1.5-T superconducting magnet (Signa, GE Healthcare, USA) and a dedicated knee extremity coil. For most of the examinations, high-resolution FSE proton density–weighted and fat-suppressed, FSE T2-weighted paired sequences were performed in the sagittal and coronal planes. Fat-suppressed, FSE T2-weighted images were also obtained in the axial plane. FSE proton density–weighted sequence parameters were as follows: 2 signals acquired; TR/TE, 2,000/18; echo-train length, 4; receiver bandwidth, 32 kHz; matrix, 256 × 256; field of view, 14–16 cm; and slice thickness, 3 mm. Fat-suppressed, FSE T2-weighted sequence parameters were 2 signals acquired;TR/TE, 4,000/50; echo-train length, 8; receiver bandwidth, 20 kHz; matrix, 256 × 256; field of view, 14–16 cm; and slice thickness, 3 mm. There were 179 knees with suspected meniscal tears that underwent MRI within 6 weeks before arthroscopy. MRI reports of 179 knees with suspected meniscal tears were reviewed and analysed.
Arthroscopies were performed under general anaesthesia and the usual technique by 2 experienced knee surgeons [18, 19]. Arthroscopy findings served as the study’s gold standard.
The composite data was tabulated on a Microsoft Excel spreadsheet and studied for correlation. The diagnostic accuracy of MRI and the sensitive and specific clinical tests and elements of patients’ history with high predictive value for meniscal tears were determined by calculating sensitivity (Se), specificity (Sp), positive predictive value (PPV) and negative predictive value (NPV). Continuous variables were summarised using median values. Categorical variables were summarised using frequency and were compared using the chi-square or McNemar test as appropriate. Logistic regression analysis was used to examine correlations with regard to suggestive symptoms, clinical tests and MRI results associated with meniscal tears. Correlation of the clinical examination and MRI with arthroscopy from the pooled data of 262 knees was expressed as a percentage. All the tests were 2-sided, and a p-value of less than 0.05 was considered to be statistically significant. Analyses were performed using SPSS version 13.0 (SPSS, Chicago, IL, USA).
Of the 262 knees, 189 knees with a meniscal tear were identified at surgery in 180 patients. There were 89 male and 91 female patients in the age group of 7–77 years, with a median age of 41. There were 85 (45%) left knees and 104 (55%) right knees. There were 82 lateral meniscus tears (and 36 discoid lateral meniscus accompanied meniscus tears) and 77 medial meniscus tears. There were 179 knees with a suspected meniscal tear that underwent MRI within 6 weeks before arthroscopy (median = 1.3 weeks). The operative diagnoses of 262 knees were meniscal tear (189), osteoarthritis (134),synovial disease (122), loose body (66) and others (30) as listed in table 1.
Of 179 knees that underwent MRI, the operative diagnoses were meniscal tear (117), osteoarthritis (87), synovial disease (68), and loose body (26). Positive findings of MRI were meniscal tear (112), osteoarthritis (11), synovial disease (3), and loose body (4). Of the 179 knees with an MRI diagnosis of suspected meniscal tears, 112 were confirmed on MRI and arthroscopy (true positive); 47 knees had no evidence of meniscal tear on MRI and arthroscopic procedure (true negative); 15 knees which didn’t have meniscal tears confirmed by arthroscopy were misinterpreted by MRI (false positive); and 5 knees with meniscal tears confirmed by arthroscopy were not diagnosed by MRI (false negative). MRI diagnosis had an accuracy of 88% for meniscal tears (sensitivity 96%, specificity 76%, positive predictive value 88% and negative predictive value 90%) (table 2).
By performing the chi-square test it was found that items such as swelling, giving way, locking, quadriceps atrophy, joint line tenderness test, lack of flexion or extension, Apley’s test, McMurray’s test, Kellogg-Speed test, pain on hyperextension, and pain on hyperflexion were common in meniscus tears (p<0.05). The results of univariate analysis by chi square analysis are given in table 3.
Multivariate logistic regression analysis of those significant clinical variables showed that giving way, locking and McMurray’s test were independent diagnostic factors with a predicted correct percentage of 80.0% (p<0.05) for the diagnosis of meniscal tears found during arthroscopy (table 4).
We knew that MRI was also a diagnostic factor, and multivariate logistic regression analysis of all the significant variables including clinical items and MRI showed that locking, McMurray’s test and MRI were independent diagnostic factors with a higher predicted correct percentage (91.6%) (p<0.05) (table 5).
By using logistic regression analysis of the significant variables (swelling, giving way, locking, quadriceps atrophy, joint line tenderness test, lack of flexion or extension, Apley’s test, McMurray’s test, Kellogg-Speed test, pain on hyperextension, and pain on hyperflexion), giving way, locking and McMurray’s test were independent diagnostic factors for the diagnosis of meniscal tears.
As 179 knees underwent MRI, in order to compare the value of clinical examination and patients’ history with MRI concerning their power to predict a meniscal lesion, we calculated the sensitivity (Se), specificity (Sp), positive predictive value (PPV), negative predictive value (NPV) of giving way, locking, and McMurray’s test of 179 knees with MRI. The diagnostic accuracy of giving way, locking, and McMurray’s test for meniscal tears are listed in table 6.
Giving way, locking and McMurray’s test had the following values, respectively, for the diagnosis of meniscal tears: accuracy, 49.2, 60.9, 76; sensitivity, 43.5, 55.2, 75.8; specificity, 84, 96, 76.9; PPV, 94.4, 98.8, 95.1; and NPV, 19.4, 25.8, 35.1. Combining with MRI, the diagnostic accuracy values of giving way, locking, McMurray’s test for the diagnosis of meniscal tears found during arthroscopy were: accuracy, 88.3,89.9,89.4; sensitivity, 95.7,97.4,97.4; specificity, 74.2,75.8,74.2; PPV, 87.5,88.4, 87.7; and NPV, 90.2,94,93.9 (table 6). When considering a positive clinical history and/or physical examination (i.e., patients who are symptomatic), the combined diagnostic accuracy of positive locking and positive McMurray’s test was: accuracy, 50.8; sensitivity, 43.5; specificity, 96, PPV98.5, and NPV21.6. The combined diagnostic accuracy of positive giving way and positive locking and positive McMurray’s test was: accuracy, 36.3; sensitivity, 26.6; specificity, 96; PPV, 97.6; and NPV, 17.5 (table 6).
| Table 1: Demographic data of 189 knees with meniscus tears and operative diagnoses of 262 knees. | |||||||||
| Knee category | No. of knees | Sex | Median patient age (y) | Lesion location | Median interval (wk) between MRI and surgery | ||||
| Male | Female | left | right | lateral (discoid lateral meniscus) | medial | ||||
| All knees | 262 | 115 | 135 | 41 (7–78) | 138 | 124 | 82 (36) | 77 | 1.3 |
| Meniscal tear Osteoarthritis Synovial disease Loose body Other | 189 134 122 66 30 | 89 | 91 | 41 (7–77) | 85 | 104 | |||
| Table 2: Diagnostic values of MRI for meniscal tears. | |||||||||
| Diagnosis | True positive | True negative | False positive | False negative | Accuracy (%) | Se(%) | Sp(%) | PPV (%) | NPV (%) |
| Meniscal tear | 112 | 47 | 15 | 5 | 88.8 | 95.7 | 75.8 | 88.2 | 90.4 |
| Note: Se: specificity; Sp: specificity; PPV: positive predictive values; NPV: negative predictive values. | |||||||||
| Table 3: Results of univariate analysis by chi square analysis. | ||||
| Index items | Odds Ratio Value | 95% Confidence Interval | Asymp. Sig. (2-sided) (p <0.05) | |
| Lower | Upper | |||
| Pain | 0.708 | 0.306 | 1.634 | 0.416 |
| Swelling | 0.547 | 0.317 | 0.945 | 0.029 |
| Limited motion | 0.639 | 0.370 | 1.102 | 0.106 |
| Giving way | 5.586 | 2.536 | 12.303 | 0.000 |
| Locking | 3.739 | 2.043 | 6.843 | 0.000 |
| Clicking | 2.608 | 0.748 | 9.094 | 0.120 |
| Quadriceps atrophy | 2.426 | 1.373 | 4.287 | 0.002 |
| Joint line tenderness test | 3.393 | 1.919 | 6.001 | 0.000 |
| Induration around knee joint | 0.366 | 0.114 | 1.175 | 0.155 |
| Varus or valgus deformity | 1.957 | 0.225 | 17.038 | 0.536 |
| Lack of flexion or extension | 0.315 | 0.128 | 0.777 | 0.009 |
| Floating patella test | 1.792 | 0.706 | 4.552 | 0.215 |
| Soto-holl test | 0.761 | 0.439 | 1.321 | 0.332 |
| Apley’s test | 11.652 | 4.820 | 28.171 | 0.000 |
| McMurray’s test | 13.897 | 6.656 | 29.014 | 0.000 |
| Kellogg-Speed test | 0.356 | 0.135 | 0.935 | 0.030 |
| Pain on hyperextension | 4.786 | 1.418 | 16.157 | 0.006 |
| Pain on hyperflexion | 0.072 | 0.008 | 0.630 | 0.009 |
| Table 4: Results of multivariate logistic regression analysis of the significant clinical variables. | ||
| Variables | B | Sig. |
| Giving way | 1.003 | 0.030 |
| Locking | 0.769 | 0.037 |
| McMurray’s test | 2.407 | 0.000 |
| Swelling | 0.098 | 0.755 |
| Quadriceps atrophy | 1.421 | 0.233 |
| Joint line tenderness test | 0.751 | 0.386 |
| Lack of flexion or extension | 0.851 | 0.356 |
| Apley’s test | 1.250 | 0.264 |
| Kellogg-Speed test | 1.348 | 0.246 |
| Pain on hyperextension | 0.023 | 0.879 |
| Pain on hyperflexion | 1.965 | 0.161 |
| Table 5: Results of multivariate logistic regression analysis of the significant clinical variables and MRI. | ||
| Variables | B | Sig. |
| Locking | 3.009 | 0.005 |
| McMurray’s test | 1.531 | 0.009 |
| MRI | 2.262 | 0.001 |
| Swelling | 0.304 | 0.581 |
| Giving way | 0.112 | 0.738 |
| Quadriceps atrophy | 0.003 | 0.960 |
| Joint line tenderness test | 1.289 | 0.256 |
| Lack of flexion or extension | 2.618 | 0.106 |
| Apley’s test | 0.182 | 0.669 |
| Kellogg-Speed test | 1.741 | 0.187 |
| Pain on hyperextension | 0.197 | 0.657 |
| Pain on hyperflexion | 0.186 | 0.667 |
| Table 6: Reliability of giving way, locking, McMurray’s test, and combining MRI, for diagnosis of meniscal tears (179 knees). | ||||||||||||
| Variable | True positive | True negative | False positive | False negative | Accuracy (%) | Se (%) | Sp (%) | PPV (%) | NPV (%) | Percentage missed (%) | Probability missed diagnosis | Probability false diagnosis |
| Giving way | 67 | 21 | 4 | 87 | 49.2 | 43.5 | 84 | 94.4 | 19.4 | 56.5 | 0.56 | 0.16 |
| Locking | 85 | 24 | 1 | 69 | 60.9 | 55.2 | 96 | 98.8 | 25.8 | 44.8 | 0.45 | 0.04 |
| McMurray’s test | 116 | 20 | 6 | 37 | 76 | 75.8 | 76.9 | 95.1 | 35.1 | 24.2 | 0.24 | 0.23 |
| Giving way, MRI | 112 | 46 | 16 | 5 | 88.3 | 95.7 | 74.2 | 87.5 | 90.2 | 4.3 | 0.04 | 0.26 |
| Locking, MRI | 114 | 47 | 15 | 3 | 89.9 | 97.4 | 75.8 | 88.4 | 94 | 2.6 | 0.03 | 0.24 |
| McMurray’s test, MRI | 114 | 46 | 16 | 3 | 89.4 | 97.4 | 74.2 | 87.7 | 93.9 | 2.6 | 0.03 | 0.26 |
| Giving way+ and locking+ | 51 | 24 | 1 | 103 | 41.9 | 33.1 | 96 | 98.1 | 18.9 | 66.9 | 0.67 | 0.04 |
| Locking+ and McMurray’s test+ | 67 | 24 | 1 | 87 | 50.8 | 43.5 | 96 | 98.5 | 21.6 | 56.5 | 0.56 | 0.04 |
| Giving way+ and McMurray’s test+ | 54 | 23 | 2 | 100 | 43.0 | 35.1 | 92 | 96.4 | 18.7 | 64.9 | 0.65 | 0.08 |
| Giving way+ and locking+ and McMurray’s test+ | 41 | 24 | 1 | 113 | 36.3 | 26.6 | 96 | 97.6 | 17.5 | 73.4 | 0.73 | 0.04 |
| Note: Se: specificity; Sp: specificity; PPV: positive predictive values; NPV: negative predictive values.+: positive. | ||||||||||||
The frequent association of meniscal tears with other intra-articular lesions has been observed. Meniscal tears and other intra-articular lesions also have common symptoms [20–23]. We used 262 samples from 250 individuals with or without meniscal lesions to gain a better estimation of history and physical examination’s specificity, and to thus more accurately identify optimal clinical tests to predict the presence of a meniscal tear found in arthroscopy.
As it has been found that McMurray’s, joint line tenderness and Apley’s [24] tests are not diagnostically accurate when used alone, for example, joint line tenderness was sensitive (75%) but not specific (27%), while the McMurray’s test was specific (97%) but not sensitive (52%) [11], the diagnostic value of a history plus a physical examination is limited. In unclear situations, the clinician requests an MRI for additional information to aid planning the operation and to predict the prognosis. However, many studies have shown no significant differences in the clinical and MRI diagnosis of meniscal tears [16, 25–30]. For example, the sensitivity of MRI for detecting tears of the posterior horn of the lateral meniscus is lower than for tears at other meniscal locations [31]. One study even showed that, when the MRI was normal, high clinical suspicion and a skilled clinical examination were more reliable [24]; another study showed that 37% of the operations supported by a significant disorder on MRI were unjustified [32]. Several investigators combined these tests with other components of the physical examination such as patient history and imaging [24, 26, 33]. Unfortunately, no conclusions can be drawn when examining these studies, due to their vast differences.
In this study, univariate analysis by the chi-square test revealed that history and physical findings such as swelling, giving way, locking, quadriceps atrophy, joint line tenderness test, lack of flexion or extension, Apley’s test, McMurray’s test, Kellogg-Speed test, pain on hyperextension, and pain on hyperflexion were diagnostic factors for a meniscal tear. By logistic regression analysis of the significant clinical variables, giving way, locking and McMurray’s test were independent diagnostic factors with a predicted correct percentage of 80.0% (p<0.05) for exhibiting a meniscal tear confirmed by arthroscopy. For the time being, history taking and physical examination, albeit of limited use, should be considered with individual patient demands to provide the basis for further evaluation; synthesis of a group of examination manoeuvres and historical items may be required for adequate diagnosis [34].
Abdon et al. [35] reported that clinical accuracy in diagnosing meniscal tears was 61%, but a combination of patient reported symptoms increased the predictive value of identifying a meniscal lesion to 70–80%. Researchers in that study had been able to determine variables of significant importance by discriminate analysis.
However, patient history and physical examination alone did not provide clinicians with levels of certainty in the 90th percentile that a patient had a meniscal tear. As clinical diagnosis was difficult, all possible steps should be taken to avoid errors [35].
The MRI accuracy for meniscal tears achieved in our study corresponds to that found by others [28, 36–38]. In this study, if an MRI was included in the model, the results of logistic regression analysis were that locking, McMurray’s test and MRI were statistically higher risk factors in knee arthroscopy individuals with meniscal tears and that the presence of these increasedthepredicted correct percentage for the diagnosis of meniscal tears found during arthroscopy to 91.6% (p<0.05).
Though MRI was more sensitive for meniscal tears, Ben-Galim et al. [26] demonstrated that MRI had a false positive rate of 65% for identifying medial meniscal tears and 43% for lateral meniscus tears compared with surgical findings. MRI, in addition to clinical evaluation, is recommended because of its high accuracy and negative predictive value [38].
In our study, giving way, locking, and McMurray’s test, respectively, had higher specificity (84, 96, 76.9) and PPV (94.4, 98.8, 95.1) compared with MRI (Ac, 88.8; Se, 95.7; Sp, 75.8; PPV, 88.2; and NPV, 90.4.), but lower accuracy (49.2, 60.9, 76), sensitivity (43.5, 55.2, 75.8) and NPV (19.4, 25.8, 35.1), for the diagnosis of meniscal tears. Combining MRI, accuracy, sensitivity, NPV of giving way, locking, and McMurray’s test for the diagnosis of meniscal tears found during arthroscopy were obviously higher than not combining MRI, and the probability of missed diagnosis obviously decreased from 56.5, 44.8, 24.2 to 4.3, 2.6, 2.6, respectively. When considering a positive clinical history and/or physical examination (i.e., patients who are symptomatic), the combined diagnostic accuracy (Ac, 50.8; Se, 43.5; Sp, 96; PPV, 98.5; and NPV, 21.6.) of positive locking and positive McMurray’s test was the highest, and the combined diagnostic accuracy (Ac, 36.3; Se, 26.6; Sp, 96; PPV, 97.6; and NPV, 17.5.) of positive giving way, positive locking and positive McMurray’s test was the lowest, so patients with coincidental positive locking and positive McMurray’s test were slightly more.
In conclusion, giving way, locking and McMurray’s test are independent clinical diagnostic factors for the diagnosis of meniscal tears found during arthroscopy. MRI has higher accuracy, sensitivity and NPV for the diagnosis of meniscal tears than giving way, locking and McMurray’s test. The combination of giving way, locking, McMurray’s test and MRI for confirmation is typical for a meniscal lesion diagnosis. Based on these findings, MRI should be used in a standard manner to detect meniscal tears found during arthroscopy.
Our study had several limitations: one major limitation was the retrospective design of the study. It also included a wide range of patient ages. This study only included patients admitted for arthroscopy and therefore the selected patient population is likely to have a high rate of meniscal tears. A total of 5 cases waited 6 weeks between the MRI and the arthroscopy, and this time could have permitted meniscus lesions to heal, thus producing false positive MRI.
1 Terry GC, Tagert BE, Young MJ. Reliability of the clinical assessment in predicting the cause of internal derangements of the knee. Arthroscopy. 1995;11(5):568–76.
2 Englund M, Guermazi A, Gale D, Hunter DJ, Aliabadi P, Clancy M, et al. Incidental meniscal findings on knee MRI in middle-aged and elderly persons. N Engl J Med. 2008;359(11):1108–15.
3 Kirkley A, Birmingham TB, Litchfield RB, Giffin JR, Willits KR, Wong CJ, et al. A randomized trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2008;359(11):1097–107.
4 Mohan BR, Gosal HS. Reliability of clinical diagnosis in meniscal tears.Int Orthop. 2007;31(1):57–60.
5 Wagemakers HP, Heintjes EM, Boks SS, Berger MY, Verhaar JA, Koes BW, et al. Diagnostic value of history-taking and physical examination for assessing meniscal tears of the knee in general practice. Clin J Sport Med. 2008;18(1):24–30.
6 Nickinson R, Darrah C, Donell S. Accuracy of clinical diagnosis in patients undergoing knee arthroscopy. Int Orthop. 2010;34(1):39–44.
7 Crawford R, Walley G, Bridgman S, Maffulli N. Magnetic resonance imaging versus arthroscopy in the diagnosis of knee pathology, concentrating on meniscal lesions and ACL tears: a systematic review. Br Med Bull. 2007;84(1):5–23.
8 Crues JV 3rd, Mink J, Levy TL, Lotysch M, Stoller DW. Meniscal tears of the knee: accuracy of MR imaging. Radiology. 1987;164(2):445–8.
9 Rubin DA, Paletta GA Jr. Current concepts and controversies in meniscal imaging. Magn Reson Imaging Clin N Am. 2000;8(2):243–70.
10 Esmaili Jah AA, Keyhani S, Zarei R, Moghaddam AK. Accuracy of MRI in comparison with clinical and arthroscopic findings in ligamentous and meniscal tears of the knee.Acta Orthop Belg. 2005;71(2):189–96.
11 Jeffrey LJ, Patrick GO, Kurt K. Evaluation of Acute Knee Pain in Primary Care. Ann Intern Med. 2003;139(7):575–88.
12 Meserve BB, Cleland JA, Boucher TR. A meta-analysis examining clinical test utilities for assessing meniscal tear.Clin Rehabil. 2008;22(2):143–61.
13 Malanga G, Andrus S, Nadler S, McLean J. Physical examination of the knee: a review of the original test description and scientific validity of common orthopedic tests. Arch Phys Med Rehabil. 2003;84(4):592–603.
14 Rose R. The accuracy of joint line tenderness in the diagnosis of meniscal tears. West Indian Med J. 2006;55(5):323–6.
15 Scholten RJ, Devillé WL, Opstelten W, Bijl D, van der Plas CG, Bouter LM. The accuracy of physical diagnostic tests for assessing meniscal lesions of the knee: a meta-analysis. J Fam Pract. 2001;50(11):938–44.
16 Miller GK. A prospective study comparing the accuracy of the clinical diagnosis of meniscus tear with magnetic resonance imaging and its effect on clinical outcome. Arthroscopy. 1996;12(4):406–13.
17 Canale ST, Beatty JH, editors. Phillips BB. Arthroscopy of the lower extremity. 11th ed. Philadelphia: Mosby Elsevier; 2007.
18 Gillquist J, Hagberg G. A new modification of the technique of arthroscopy of the knee joint. Acta Chir Scand. 1976;142(2):123–30.
19 Hamberg P. Treatment of meniscus lesions of the knee: a selective approach. Linkoping University Medical Dissertations;156. Linkoping, Sweden; 1983.
20 Englund M, Niu J, Guermazi A, Roemer FW, Hunter DJ, Lynch JA, et al. Effect of meniscal damage on the development of frequent knee pain, aching, or stiffness. Arthritis Rheum. 2007;56(12):4048–54.
21 Kornaat PR, Bloem JL, Ceulemans RY, Riyazi N, Rosendaal FR, Nelissen RG, et al. Osteoarthritis of the knee: association between clinical features and MR imaging findings. Radiology. 2006;239(3):811–7.
22 Bhattacharyya T, Gale D, Dewire P, Totterman S, Gale ME, McLaughlin S, et al. The clinical importance of meniscal tears demonstrated by magnetic resonance imaging in osteoarthritis of the knee. J Bone Joint Surg Am. 2003;85-A(1):4–9.
23 Link TM, Steinbach LS, Ghosh S, Ries M, Lu Y, Lane N, et al. Osteoarthritis: MR imaging findings in different stages of disease and correlation with clinical findings. Radiology. 2003;226(2):373–81.
24 Hegedus EJ, Cook C, Hasselblad V, Goode A, McCrory DC. Physical examination tests for assessing a torn meniscus in the knee: a systematic review with meta-analysis. J Orthop Sports Phys Ther. 2005;37(9):541–50.
25 Rose NE, Gold SM. A comparison of accuracy between clinical examination and magnetic resonance imaging in the diagnosis of meniscal and anterior cruciate ligament tears. Arthroscopy. 1996;12(4):398–405.
26 Ben-Galim P, Steinberg EL, Amir H, Ash N, Dekel S, Arbel R. Accuracy of magnetic resonance imaging of the knee and unjustified surgery. Clin Orthop Relat Res. 2006;447:100-4.
27 Jerosch J, Riemer S. How good are clinical investigative procedures for diagnosing meniscus lesions? Sportverletz Sportschaden. 2004;18(2):59–67.
28 Madhusudhan TR, Kumar TM, Bastawrous SS, Sinha A. Clinical examination, MRI and arthroscopy in meniscal and ligamentous knee Tears – a prospective study. J Orthop Surg Res. 2008;3:19–25.
29 Ryzewicz M, Peterson B, Siparsky PN, Bartz RL. The diagnosis of meniscus tears: the role of MRI and clinical examination. Clin Orthop Relat Res. 2007;455:123–33.
30 Muellner T, Weinstabl R, Schabus R, Vécsei V, Kainberger F. The diagnosis of meniscal tears in athletes. A comparison of clinical and magnetic resonance imaging investigations. Am J Sports Med. 1997;25(1):7–12.
31 Laundre BJ, Collins MS, Bond JR, Dahm DL, Stuart MJ, Mandrekar JN. MRI accuracy for tears of the posterior horn of the lateral meniscus in patients with acute anterior cruciate ligament tear and the clinical relevance of missed tears. Am J Roentgenol. 2009;193(2):515–23.
32 Kocabey Y, Tetik O, Isbell W, Atay O, Johnson D. The value of clinical examination versus magnetic resonance imaging in the diagnosis of meniscal tears and anterior cruciate ligament rupture. Arthroscopy. 2004;20(7):696–700.
33 Dervin GF, Stiell IG, Wells GA, Rody K, Grabowski J. Physicians’ accuracy and interrator reliability for the diagnosis of unstable meniscal tears in patients having osteoarthritis of the knee. Can J Surg.2001;44(4):267–74.
34 Solomon DH, Simel DL, Bates DW, Katz JN, Schaffer JL. The rational clinical examination. Does this patient have a torn meniscus or ligament of the knee? Value of the physical examination. JAMA. 2001;286(13):1610–20.
35 Abdon P, Lindstrand A, Thorngren KG. Statistical evaluation of the diagnostic criteria for meniscal tears. Int Orthop. 1990;14(4):341–5.
36 Ruth C, Gayle W, Stephen B, Nicola M. Magnetic resonance imaging versus arthroscopy in the diagnosis of knee pathology, concentrating on meniscal lesions and ACL tears: a systematic review. Br Med Bull. 2007;84(1):5–23.
37 Rayan F,Bhonsle S,Shukla DD. Clinical, MRI, and arthroscopic correlation in meniscal and anterior cruciate ligament tears. Int Orthop. 2009;33(1):129–32.
38 Muellner T, Nikolic A, Vécsei V. Recommendations for the diagnosis of traumatic meniscal tears in athletes. Sports Med. 1999;27(5):337–45.
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article were reported.