Basis for a Swiss perspective on fall prevention in vulnerable older people1
DOI: https://doi.org/10.4414/smw.2011.13305
Y
Gschwind, I
Wolf, S
Bridenbaugh
Summary
During the 20th century Switzerland, like many other Western countries, experienced significant ageing of the population over the age of 65. As the lifespan of the Swiss population increases, so does the prevalence of falls. A multiplicity of fall prevention programmes are available, but extracting their most effective components remains a challenge. This article summarises the results of current studies on fall prevention, with a particular focus on methodological quality and successful reduction of fall incidence in vulnerable older people. Characteristics of effective fall prevention programmes in the fields of exercise, home modifications, appropriate footwear and walking aids are assessed. We then briefly discuss how these study results can be adapted to the Swiss context. This knowledge emphasises an interdisciplinary approach in the prevention of falls, the objective being to reinforce autonomy, promote health and enhance quality of life in vulnerable older people.
1 The work presented here is a summary of our work for the Swiss Best Practice Health Promotion [54]. We provided the current evidence for fall prevention, one of five subgroups of the Best Practice project ( http://www.gesundheitsfoerderung.ch/bpgfa ). These consolidated scientific findings are intended to provide a basis for new national recommendations for the implementation of fall intervention measures for vulnerable older people. Additionally, over the next two years, with the help of an expert working group, these findings are to be translated into hands-on practical tools, such as brochures, guidelines and training programmes.
Introduction
Switzerland, like most other Western countries, experienced rapid growth of the population over the age of 65 during the 20th century [1]. Currently, persons aged 65 years and over account for 16.6% of the permanent resident population. According to projections of the Swiss Federal Statistical Office [1], in about 40 years almost every third person will belong to this age group. This development is the result of a declining birth rate and a continuously increasing lifespan. As the lifespan of the Swiss population continues to rise, so does the prevalence of falls.
Approximately one third of individuals over the age of 65 fall at least once during a one-year period [2, 3]. This increases to nearly half in people over the age of 80 [3]. In addition to the heavy financial burden on the public health care system, falls and fall-related injuries affect the quality of life of older people due to restricted mobility and functional decline [4, 5]. Hip fractures in particular, with a one-year mortality of 22%, create a significant and increasing burden of illness for older persons in Switzerland [6]. In addition to physical injury, falls can have major psychological and social consequences, such as fear of falling [7, 8].
The majority of falls in older people are not usually the result of a single cause, but rather a combination of interacting factors [9, 10]. Numerous studies with either prospective or retrospective designs have identified a multitude of risk factors for falling [2, 11–14]. These factors have been broadly classified into intrinsic (e.g. poor balance, muscle weakness, impaired gait, low vision) or extrinsic factors (e.g. environmental hazards, inappropriate footwear). Understanding these risk factors is an important step in planning fall prevention strategies.
A variety of fall prevention programmes targeting older persons have been established in recent years. These prevention programmes have used either a single intervention strategy such as exercise, home hazard assessment with modifications, vision assessment with correction and medication management, or a combination of single interventions in a multifactorial approach. However, it is not yet clear which interventions are the most beneficial for vulnerable older people.
In this systematic literature review we summarise the results of current studies on fall prevention, with a particular focus on methodological quality and successful reduction of fall incidence in vulnerable older people. We focused on single intervention studies to be able to isolate possible effects of one component of these intervention programmes. We limited our review to fall prevention interventions specifically targeting vulnerable older people, since they are likely to benefit most. We then discuss how these study results can be interpreted in the Swiss context.
Search strategy
Studies were identified by conducting a computer-based literature search using PubMed, MEDLINE, CINAHL and EMBASE electronic databases. References from current fall prevention guidelines and books were also examined [12, 15–17]. Papers recommended by experts in the field of fall prevention and scientific colleagues were also considered. The search included papers and abstracts from January 1990 to August 2010. Inclusion criteria for this review were as follows: randomised controlled trials of single interventions and non-experimental studies published in English, German or French. We included multifactorial fall prevention programmes if either exercise, home modifications, appropriate footwear or walking aids were individually assessed in separate intervention arms. The targeted populations were vulnerable older people, described by terms often used to describe pre-frail older people, such as risk of falling, history of falls or transitioning to frailty. However, given the heterogeneity of the population enrolled in some of the studies reviewed, and inconsistent methodologies regarding the definition of pre-frail older people (e.g. the Fried [18] criteria), we refrained from describing the study populations as pre-frail and instead used the term vulnerable.
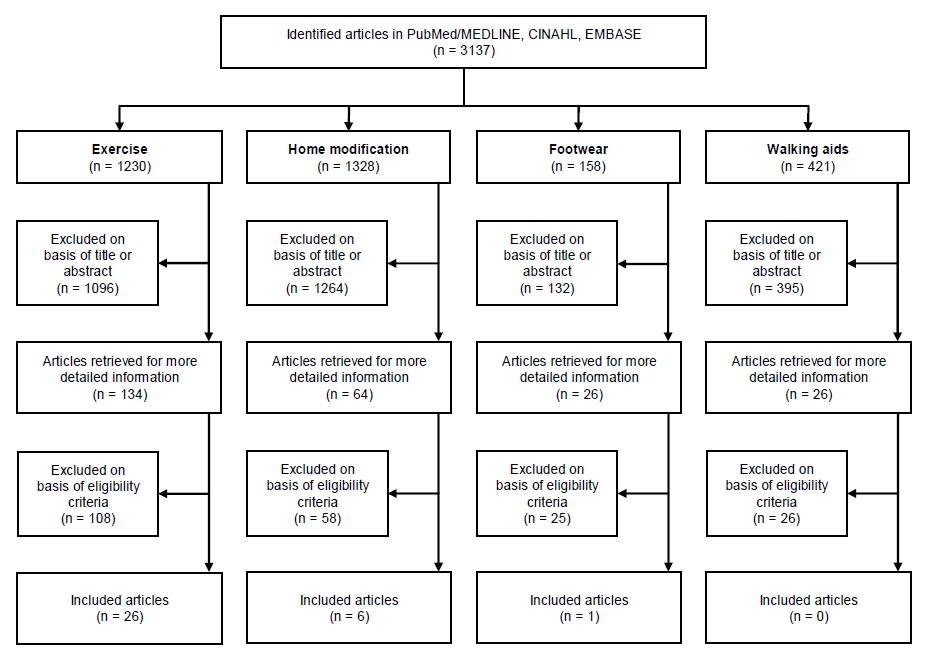
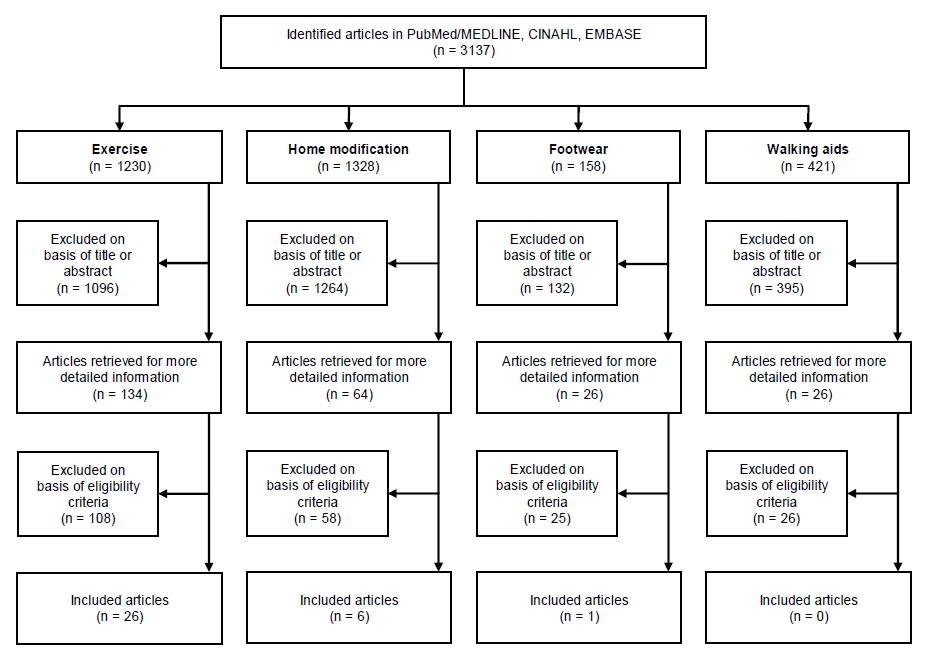
Figure 1
Flowchart for illustration of literature search and selection.
In this paper we will first present the information summary regarding intrinsic factors (exercise as a single intervention approach to reduce falls) followed by extrinisic factors (home assessment and modifications, footwear and walking aids, each as a single intervention approach to reduce falls).
Older people of both genders living alone were included. We also included one study [19] in which the participants were living in senior housing communities that included a continuum of care, because they displayed the physical capabilities (e.g. ADL and functional independence) of a vulnerable population. Participants in one study [20] lived in a residential care facility with no details provided on care status. In view of their ability to participate in a 12-week exercise programme, we considered this population appropriate for inclusion. Study participants were aged 65 or over. Only trials designed to assess fall prevention which documented the number of falls (i.e. by falls calendars) were examined.
Article selection
Two research authors screened title, key words and abstracts of identified studies for possible inclusion (YJG, IW). From the full text, those authors independently assessed potential eligibility for inclusion of papers concerning exercise, plus home modifications, appropriate footwear and walking aids. Any disagreement was resolved by discussion between the two authors or by a decision of a third author. Due to time, personnel and financial constraints, additional risk factors could not be included in the scope of this article.
The results were summarised qualitatively in a table and stratified according to type of intervention (exercise, home assessment and modifications, footwear and walking aids). We view this table of summarised studies as a valuable reference tool for those planning fall prevention programmes or studies (for further details see tables S1 - S3 published as separate PDF files: table S1 http://www.smw.ch/fileadmin/smw/pdf/Appendix/smw.2011.13305_appendix_table-S1.pdf - table S2 http://www.smw.ch/fileadmin/smw/pdf/Appendix/smw.2011.13305_appendix_table-S2.pdf - table S3 http://www.smw.ch/fileadmin/smw/pdf/Appendix/smw.2011.13305_appendix_table-S3.pdf ).
Quality assessment
Quality assessment of the articles included was based on the Physiotherapy Evidence Database (PEDro) methodological quality score (table 1) [21]. Randomised controlled trials indexed on PEDro are rated according to an 11-item scale [22]. Ten of the 11 scale items, excluding one item pertaining to external validity, contribute to the total PEDro score (range 0–10 points). The higher the score, the better the methodological quality [23].
A multidisciplinary group of health professionals met at a network congress of the Swiss Health Promotion institution (www.gesundheitsfoerderung.ch/bpgfa) to discuss the results of this systematic literature review. The feedback was included in the discussion section of this paper.
|
Table 1: Physiotherapy Evidence Database (PEDro) methodological quality scores of all included studies [21]. |
|
PEDro score1
|
Intervention studies
|
| 8 / 10 |
Barnett et al. [55], Campbell et al. [30], Campbell et al. [56], Logghe et al. [57], Robertson et al. [58] |
| 7 / 10 |
Buchner et al. [59], Lannin et al. [32], Rubenstein et al. [60], Voukelatos et al. [61], Wolf et al. [62], Yamada et al. [63] |
| 6 / 10 |
Cumming et al. [31], Day et al. [34], Faber et al. [26], Iwamoto et al. [64], Lord et al. [65], Luukinen et al. [66], Skelton et al. [67], Weerdesteyn et al. [68], Wolf et al. [69] |
| 5 / 10 |
Choi et al. [20], Li et al. [24], Lin et al. [33], McKiernan FE [45], Means et al. [70], Morgan et al. [71], Stevens et al. [35] |
| 4 / 10 |
Campbell et al. [72], Lin et al. [73], Lord et al. [74], Nowalk et al. [19] |
| N/A |
Inokuchi et al. [25] |
|
1 Scores range from zero to ten, higher score represents better methodological quality.
Ten of the 11 PEDro scale items of methodological quality are scored: randomisation, concealed allocation of subjects, baseline similarity of groups, blinding of participants, blinding of assessors, adequate follow-up (more than 85% of participants), intention to treat analysis, between-group statistical comparison, point measures and measures of variability; eligibility criteria specified is not scored. |
Interventions to prevent falls
Our initial literature search identified 3137 articles. Removal of duplicates and unsuitable papers based on information in the title or abstract resulted in 250 relevant articles. After thorough review of the full text of these articles, 33 of them fulfilled our eligibility criteria and were included in this review (fig. 1).
Exercise as a single intervention approach
This section summarises the characteristics of 26 exercise trials which were compared with each other to distinguish substantive characteristics for prospective exercise interventions in Swiss fall prevention. Overall the exercise trials showed a 14–47.5% reduction of fall rate for the intervention groups. The duration of the exercise trials ranged from five weeks to two years.
Population characteristics of the exercise trials identified
The 26 exercise trials were conducted in eight countries (n refers to the number of trials): Australia (n = 4), England (n = 1), Finland (n = 1), Japan (n = 3), Korea (n = 1), the Netherlands (n = 3), New Zealand (n = 4), Taiwan (n = 1) and the USA (n = 8). Most of these exercise trials were carried out in an urban setting (n = 20). In total, 7707 participants were recruited from emergency wards, fracture clinics, hospitals, physiotherapists’ practices, primary care providers, general practitioners, nurses, receptionists, researchers and others. Most of the exercise trials used patient files, plus population, resident and electoral registers for recruitment.
The study populations consisted of older community-dwellers living independently at home, in congregate housing, living facilities, self- and intermediate-care retirement villages, long-term care centres, senior housing communities and residential care facilities. Most of the exercise trials included more women than men (n = 20) with a range of 51.0% to 94.5% women. The mean age of study populations was between 69.0 ± 6.5 and 88.0 ± 3.0 years, and the size of the intervention groups ranged from 31 to 472 persons. The populations were heterogeneous in terms of physical health, for example, number of prescribed medications, cardiovascular complications and the presence of vision or hearing impairments.
Intervention characteristics of the exercise trials identified
Exercise frequency ranged from one to six sessions per week (n = 23 consisted of one to three sessions weekly) with a session duration of 30 to 120 min. The exercise sessions often consisted of a warm-up phase which lasted from five to 15 minutes (n = 8) and a cool-down phase which lasted five to ten minutes (n = 8). Common sites for the exercise sessions were ambulatory care centres, community or facility rooms, medical centres and at home. Exercise trials were with groups (n = 14), individuals (n = 3) or both individual and in groups (n = 5). The size of the exercising groups ranged from five to 20 participants.
Interventions took place in the following major categories: balance (e.g. one-leg stance), skeletal muscle strength (e.g. squats), gait (e.g. trail walking exercises), mobility (e.g. walking over doorsteps), coordination (e.g. dance steps), flexibility (e.g. stretching), endurance (e.g. on a treadmill) and functionality (e.g. sit to stand). A variety of exercise equipment was used such as strengthening machines, bicycle ergometers, balance boards, chairs, balls, elastic bands, as well as foot, hip and ankle weights. The trials analysed reported exercise supervision by qualified exercise instructors, licensed physiotherapists, nurses, occupational therapists, health therapists and tai chi masters.
The reported dropouts in the exercise trials were due to health problems (n = 15), death (n = 11), moving away (n = 7), institutionalisation in long-term care or hospitals (n = 7), conflicting schedules (n = 6), loss of interest (n = 4), transportation problems (n = 2), falls (n = 2), family commitments (n = 2), cognitive decline (n = 1), depression (n = 1), surgery (n = 1) and other reasons (n = 6). Only a few trials reported means of achieving long-term adherence by, for example, integrating musical (n = 4) or social components (n = 2). Music from the past of the participants was used to stimulate memories [19] and for accompaniment [24]. Social components consisted of recreational tea breaks [25] or sitting together over a drink [26].
Effective components of exercise interventions
Of the 26 total exercise intervention trials in this review, these six are focused on separately because of their high methodological quality (>5 of 10 points on the PEDro scale), large sample size (n >35 in the intervention group) and large fall prevention effect (>30% fewer falls during intervention period) (table 2). Compared to the other 20 exercise interventions, these six exercise interventions not only consisted of one to three supervised exercise sessions per week, but also at least two additional individual exercise sessions at home. On average, the weekly, usually supervised group exercise duration was higher at 60–180 minutes, whereas additional individual exercises at home were conducted for 15–35 minutes. Exercise interventions lasted from at least five weeks to one year and were held in smaller groups of nine to 12 participants. The exercise intensity was similar to the other 20 interventions and often stated to be moderate. Exercise of the six outstanding studies predominantly aimed to increase muscle strength in the lower extremities as well as to improve balance, gait, mobility and functionality.
|
Table 2: Characteristics of six particularly good exercise intervention trials.
|
|
Study
|
Participants
1
|
Intervention components
|
Adherence rate
|
Supervision
|
Main fall outcome
|
PEDro Score
|
| Barnett et al. (2003) [55] |
n = 163
age >70 years
at-risk for falls |
Class addressing physical fall risk factors designed by physiotherapist.
1x 60 min/wk for 1 year + home exercises.
5-10 min warm up: stretches, balance, coordination (modified Tai Chi, stepping, dance steps), aerobic capacity, muscle strength (body weight), functional exercise (sit to stand, weight transference, reaching). 10 min cool down. Music used. |
Median of attended exercise classes by exercise group was 23 out of 37. |
Three accredited and experienced exercise instructors. |
The rate of falls in the intervention group was 40% lower than that of the control group (IRR = 0.60, 95% CI 0.36-0.99). |
8 / 10 |
| Campbell et al. (1999) [56] |
n = 152
age >80 years
older women |
Individually tailored muscle strengthening and balance.
3x 30 min/wk and walking outdoors ≥3x/wk for 1 year.
Moderate strengthening with ankle cuff weights (0.5/1.0 kg): Walking on toes / heels, walking backwards / sideways / turning round, stepping over an object, bending and picking up an object, stair climbing at home, rising from sitting to standing. |
44% of the exercise group were exercised at least 3x/wk. |
Four home visits by a physiotherapist in the first two months of the study. |
The relative hazard for all falls for the exercise group was 0.69 (95% CI 0.49-0.97). |
8 / 10 |
| Robertson et al. (2001) [58] |
n = 240
age >80 years
older people |
Exercise programme run from a home health service based in a geriatric assessment and rehabilitation hospital.
3x approx. 30 min/wk and walking 2x/wk for 1 year.
Muscle strengthening (ankle cuff weights), balance retraining exercises and walking plan. |
43% performed the prescribed exercises ≥3x/wk, 72% at least 2x/wk. |
Trained district nurse without previous experience. |
A 46% reduction in the number of falls for exercise group (IRR = 0.54, 95% CI 0.32-0.90). |
8 / 10 |
| Skelton et al. (2005) [67] |
n = 81
age >70 years
frequent female fallers |
Individually tailored and targeted Falls Management Exercise (FaME) with Otago exercises core.
1x 60 min/wk for 36 wks and 2x 30 min/wk home exercises.
Reduction of asymmetry in strength of the lower limbs with Otago exercises core. The exercise classes were balance specific, individually tailored and targeted training for dynamic balance, strength, bone, endurance, flexibility, gait and functional skills. |
68% chose to continue exercising after the trial (implying high adherence to the original programme). |
Qualified exercise-for-the-older-person instructor with additional FaME training. |
A 31% reduction in the number of falls during the whole trial period for the exercise group (IRR = 0.69, 95% CI 0.50-0.96, p = 0.029). |
6 / 10 |
| Weerdesteyn et al. (2006) [68] |
n = 107
age >70 years
with a history of falls |
Low intensity Nijmegen Falls Prevention Programme
2x 90 min/wk for 5 wks.
Balance, gait (with additional motor and cognitive tasks) coordination in obstacle course with mimics of ADLs and potential fall risk (i.e. walking over doorsteps, stepping stones, uneven pavement, different ground surfaces). Practice of fall techniques. |
Attendance rate of 87%. |
N/A |
The number of falls in the exercise group decreased by 46% (IRR = 0.54, 95% CI 0.34-0.86). |
6 / 10 |
| Wolf et al. (2003/1996) [69] |
n = 200
age >75 years
older people |
Tai chi improving movement limitations of older people.
2x individual contact time of 45 min/wk and 2x 15 min/d at home for 15 wks.
Synthesis of 108 forms into 10, emphasising components of movement typically limited with ageing. |
Attendance in the Tai chi group was 76% (SD 19) (range: 6-100%). |
Tai Chi instructors. |
The rate of falls/risk of multiple falls was reduced by 47.5% (RR = 0.525, p = 0.01), adjusted. |
6 / 10 |
|
1 Age of participants only from intervention groups.
ADL: activities of daily living; CI: confidence intervals; IRR: incidence rate ratio; min: minutes; N/A: not applicable; RR: rate ratio; SD: standard deviation; wk(s): week(s). |
It was evident from all exercise interventions that monitoring exercise intensity is of the utmost importance to guarantee success. Progress, regular individual review (e.g. based on exercise protocols) and tailored adjustments form the basis of a successful and safe exercise intervention. Including social components in the interventions is important because it seems to improve adherence. A positive example of the integration of several of the above-mentioned components can be found in a recent Swiss study (published after completion of our systematic literature review) which reported a significant reduction in the fall rate of older people after their participation in a multi-tasking, rhythmic movement intervention to music [27].
High participation rates also depend on the dedication and motivation of the instructor, group composition and positive reinforcement by family members and general practitioners. Besides advertising or direct contact with older people, general practitioners may also have a pivotal role in recruitment of the targeted population. Additionally, exercise interventions must be feasible for vulnerable older people with respect to accessibility, financial means and personal schedules.
The success of any exercise intervention for fall prevention in vulnerable older people depends on the contents discussed above, but also duly bearing in mind distinct anthropometrical, socioeconomic, civil, ethnical, seasonal and educational data. The beneficial interaction between exercise, nutrition and supplementation (for example, proteins and vitamin D) has also to be considered in regard to functionality and quality of life in vulnerable older people [28, 29]. The latter information is missing throughout most of the trials investigated and highlights the complexity of designing a tailored and targeted exercise trial.
Home assessment and modifications as a single intervention approach
Six randomised controlled trials of home assessment and modifications were identified as a single intervention for evaluating environmental risk factors with the aim of reducing fall rates. These studies have reported inconsistent findings with only two showing a significant reduction in falls [30, 31]. Campbell et al. [30] found that there were 41% fewer falls in the intervention group compared with those who did not receive the home safety programme. The intervention in the study by Cumming et al. [31] reduced falls by 36% among participants with a history of falls.
The characteristics of the home modification studies included are presented in table 3. Countries of origin were (n refers to the number of trials): Australia (n = 4), New Zealand (n = 1) and Taiwan (n = 1). Participants in these six studies included community-dwelling individuals over the age of 65 [31-33], 70 [34, 35] or 75 [30]. Campbell et al. [30] targeted persons with severe vision impairment. Falls were monitored between a follow-up of three to 18 months.
|
Table 3: Characteristics of home assessment and modifications studies. |
|
Study
|
Participants
|
Intervention
|
Adherence to recommendations
|
Main fall outcomes
|
Comments
|
PEDro Score
|
| Campbell et al. (2005) [30] |
n = 391
age ≥75 years
poor vision |
Modified version of the Westmead Home Safety Assessment by OT, provision of equipment, payment and supervision (second visit, telephone call). |
90% adherence to one or more of the recommendations. |
Effective in reducing falls (IRR = 0.59, 95% CI 0.42-0.83). |
No significant difference in the reduction of falls at home compared with those away from the home environment. |
8 / 10 |
| Cumming et al. (1999) [31] |
n = 530
age ≥65 years
most were recruited while inpatient at hospital |
Westmead Home Safety Assessment by OT, facilitated any necessary home modification, supervision of home modifications (telephone call). |
Adherence at 12 months ranged from 19%-75%. |
Effective in previous fallers (RR = 0.64, 95% CI 0.50-0.83). Not effective in previous non-fallers (RR = 1.03, 95% CI 0.75-1.41). |
Home visit was effective in reducing risk of falling at home and away from home in previous fallers. |
6 / 10 |
| Day et al. (2002) [34] |
n = 1090
age ≥70 years
rated their health as good to excellent |
Home assessment by trained assessor, home hazards were removed or modified either by the participants themselves or via the City of Whitehorse's home maintenance programme (provision of materials and labour for providing modifications). |
N/A |
Not effective in reducing falls (RR = 0.92, 95% CI 0.78-1.08). |
Number of hazards was significantly reduced in the intervention group. Effective in combination with exercise (p = 0.02) and in combination with vision (p = 0.07). Strongest effect: all three interventions together (p = 0.004). |
6 / 10 |
| Lannin et al. (2007) [32] |
n = 10
age ≥65 years
recruited while inpatient at rehabilitation |
Westmead Home Safety Assessment by OT, advice for home modifications and equipment. Education: focussed on safe performance of activities in and around home. |
N/A |
One of the intervention participants fell within two weeks of discharge. Two of the control participants fell two weeks and one month post-discharge. |
None |
7 / 10 |
| Lin et al. (2007) [33] |
n = 150
age ≥65 years
fall history in the previous 4 weeks |
Safety assessment by public health workers, advice for home modifications. |
N/A |
Not effective in reducing the fall incidence rate per 1000 person years (1.1 in home safety group, 1.6 in exercise group, 2.4 in educational group). |
Quality of life (physical and environmental domain), functional reach, ADLs, functional balance and gait improved significantly. |
5 / 10 |
| Stevens et al. (2001) [35] |
n = 1737
age ≥70 years
healthy older people |
Home hazard assessment by trained nurse assessor, free installation of safety devices, education about home hazards. |
Maintained significant reduction in 4 out of 5 most prevalent home hazards. |
Not effective in reducing the rate of falls (falls on environmental hazards inside the home: IRR = 1.11, 95% CI 0.82-1.50). |
Covariates significantly associated with an increased rate of falls on environmental hazards were history of falling (RR 2.09) and use of a walking aid inside the home (RR 1.94). |
5 / 10 |
| ADL: activities of daily living; CI: confidence intervals; IRR: incidence rate ratio; N/A: not applicable; OT: occupational therapist; RR: rate ratio. |
Home assessment is an essential part of this single intervention approach. Four different assessment tools were used throughout the six trials of which two were specifically designed on the basis of published papers and existing checklists [33, 35]. The two successful fall prevention trials used the same validated and reliable home assessment form (table 3).
In four studies a single home visit took place to identify and modify potential fall risk factors [32–35]. These four studies showed no effect in reducing fall rate. The two studies that led to a reduction in fall rates included a follow-up contact to check whether suggested home modifications had been implemented. In one study, a second visit was conducted to check the equipment installed [30]. In the study by Cumming et al. [31] an occupational therapist called all participants two weeks after the assessment to check home modifications and to encourage adherence to recommendations. It thus seems reasonable to verify the recommended modifications after a certain time span. A telephone call may represent a cost-effective option for follow-up contact.
In the four ineffective trials, the intervention was conducted by trained nurses or public health workers. The two effective interventions were done by occupational therapists. The intervention in the study by Cumming et al. [31] was effective only among participants who reported having had at least one fall in the previous year. However, in this group falls outside the home were also significantly reduced. Similar results were presented by Campbell et al. [30] with no significant difference in the reduction of falls at home compared to those outside the home. This suggests that an effect may not be caused by the home modifications alone but also partly depends on professional advice by the occupational therapist.
Adherence is an important aspect of interventions. It was evaluated in three [30, 31, 35] of the six studies and varied between 13% and 90%. The most commonly recommended home modifications were: removal of obstacles, rugs and mats, installation of grab bars or rails, improvement of poor lighting, use of non-slip bathmat, repair of damaged flooring and fitting of contrast edging to steps. It is known from clinical practice that home assessments and modifications are poorly accepted by older people. Older people’s self perception of fall risk is often quite different from that of the health professional. Acceptance of suggested modifications can be facilitated by establishing a good relationship between the target person and the health professional. Help from a health professional or the relatives can also support adherence to home safety recommendations.
Effective components of home assessment and modifications
The outcomes of falls in the six studies showed inconsistent findings. The interventions which effectively reduced falls suggest that home assessment and modifications should be offered to people with a previous fall history, severe vision problems or after discharge from hospital. In view of the specific expertise needed in this area, occupational therapists should guide the intervention. Furthermore, the effectiveness of the intervention can be enhanced by follow-up contacts.
It is acknowledged that a home assessment and modifications should be part of a multifactorial approach [36], since the majority of the studies used a multifactorial approach and evidence in fall prevention is strong.
Footwear as a single intervention approach
The relationship between certain types or characteristics of footwear and the risk of falling is well established in the literature. Walking barefoot or wearing socks has been associated with a higher risk of falling [37–40] than when wearing shoes. Studies which examined footwear characteristics at the time of fall-related hip fractures showed that the most common type of footwear were slippers, walking barefoot or wearing socks [41, 42]. However, walking barefoot or wearing socks or slippers does not necessarily indicate that this type of footwear, or the absence of footwear, caused the fall. Shoes with low heels and a large contact area may help older people to reduce the risk of a fall [43]. Additionally, older people often choose their footwear for comfort and not safety reasons [42]. The difficulty in establishing a relationship between footwear and risk of falls is that the type of shoe worn may change according to the location and activity being undertaken. Furthermore, going shoeless indoors might be more common.
Most falls occur during the winter months [44]. A randomised controlled trial by McKiernan [45] was able to show that an anti-slip device attached to shoes significantly reduced outdoor falls in hazardous winter conditions in older people with a history of previous falls. However, not wearing a gait-stabilising device in hazardous winter conditions does not represent a risk factor for falling.
Effective components of footwear interventions
Anti-slip devices for shoes may be useful for older people in hazardous winter conditions (e.g. snow and ice). Based on lower quality studies, footwear should be worn indoors and outdoors, have a low heel height, high surface contact area and good fixation. Future research should be made to strengthen the evidence and make recommendations regarding the characteristics of safe shoes for older people.
Walking aids as a single intervention approach
The use of walking aids is considered a fall-associated risk factor [11, 12]. The study of Rubenstein and Josephson [11] showed that the use of a walking aid is related to a 2.6-fold (confidence interval: 1.2; 4.6) risk of falling. Some older people fall because of their walking aid, for example by improper use or tripping over the walking aid. A walking aid may also impede the compensatory stepping and grasping mechanism during balance recovery to avoid a fall [46, 47]. However, the increased fall risk associated with the use of a walking aid, as reported by Rubenstein and Josephson [11], probably reflects the functional status of the older people using the walking aids (those with gait disturbance, muscle weakness and increased fall risk are more likely to use a walking aid) rather than the aid itself. When walking aids are appropriately chosen for the clinical condition (for example, a four-points walker instead of a front-wheel walker for people with Parkinsonian gait disturbances), correctly sized (not too high or too low) and properly implemented, they can heighten walking safety by increasing the base of support, enhancing lateral stability and reducing lower-limb load [48], and thus perhaps reduce the risk of falling.
Important components of walking aid interventions
A suitable walking aid must be appropriate for the individual’s abilities and the environment, correctly sized and free of defects [49, 50], and should only be used if necessary. Also, prescription and training in the use of walking aids should be left to a health professional with expertise in the field [12, 51].
Fall prevention in the Swiss context
Fall prevention in Switzerland needs to overcome specific hurdles and framework conditions. There are many local, regional, cantonal and national peculiarities. It is comprehensible that settings of international studies are often not generally applicable to Swiss settings [52]. Specific geographical, infrastructure, socio-demographic and funding circumstances must be taken into consideration. Besides cultural differences, there are also language barriers to be overcome. In the best case, Swiss fall prevention endeavours are translated into all four of the country’s official languages (German, French, Italian and Romansh) to reach as many vulnerable older people as possible. The integration of international scientific findings also faces a unique regional, cantonal and federal legal and political system in Switzerland, which has administrative subdivisions into 26 cantons with considerable autonomy. These cantons are further subdivided into multiple small communities which are often equivalent to the remaining restricted living environment of older people. Gaining the support of local community authorities may be of crucial importance in reaching older people on the subject of fall prevention.
It is necessary to highlight the importance of cooperation and coordination between all health experts in the field of fall prevention. Interdisciplinary cooperation between exercise instructors, physiotherapists, occupational therapists, exercise and health scientists, as well as general practitioners, geriatricians and psychologists, form the foundation for successful fall prevention [53]. Besides professional supervision, different forms of social activity between or after intervention sessions may also improve adherence. In vulnerable older people a high level of motivation must be maintained to guarantee high adherence rates and thus prolong positive health effects of interventions.
|
Table 4: Important characteristics of successful interventions. |
|
Domain
|
Important components of interventions
|
| Exercise |
1–3 supervised group exercise sessions per week (60–180 minutes in total) and ≥2 additional individual exercise sessions at home (15–35 minutes per session).
Intervention duration of 5–52 weeks.
Moderate exercise intensity.
9–12 members per group.
Supervision by qualified and trained personnel.
Exercises for muscle strength of lower extremities, balance, gait, mobility and functionality. |
| Home assessment and modifications |
For older people with a previous fall history, severe vision problems, after discharge from hospital.
Guided by occupational therapists.
Implementation of follow-up contacts. |
| Footwear |
Use anti-slip devices in hazardous winter conditions.
Footwear should be worn indoors and outdoors, have a low heel height, high contact area and good fixation. |
| Walking aids |
Adapted to individual abilities and environment.
Correctly sized and free of defects.
Only used if necessary.
Training in the use of the walking aid.
Recommended by a health professional. |
Conclusion
This systematic literature review may serve as a basis for recommendations on the implementation of interventions in vulnerable older people in Switzerland. We identified important features of fall prevention interventions of high methodological quality which successfully showed a reduction in fall incidence rate. However, the rather heterogeneous intervention designs, the potential bias from low quality studies and the inclusion of non-experimental studies prevents us from performing a meta-analysis in the context of our systematic review. The optimal type, intensity, frequency and duration of fall prevention programmes required to significantly lower the rate of falls over the long term are still not known. This is partly due to the varying definitions of falls across studies and the inconsistency with which falls are monitored and reported. In this regard, older people who exercise may become more mobile and therefore more exposed to a greater risk of falling. Hence, apart from simply a change in the number of falls, further outcome measures such as the use of health care services, improvements in the overall level of disability or functionality, and psychosocial measures such as fear of falling and perceived quality of life must be taken into consideration when scrutinising the effectiveness of a fall prevention programme.
Exercise programmes for vulnerable older people should be adjusted to the individual health circumstances, to guarantee safe exercising and prevent health damage or injury. The exercise instructor and the social atmosphere may play a pivotal role in positively affecting adherence rates, sustainability of the programme and general enjoyment of the exercises. It is comprehensible that a multitude of exercise variables and heterogeneous conditions make it difficult to extract, compare and reproduce particular effective exercise components in a real-life setting. Consequently, general statements on exercise content for fall prevention in vulnerable older people in Switzerland remain challenging.
Environmental hazards, inadequate footwear and walking aids are implicated as a contributory factor in a large proportion of falls in older people. Considering the small number of published studies, the effectiveness of these fall prevention programmes as a single intervention should be examined in future research. To date, several studies have included environmental changes, inspection of footwear and walking aids as a component within a multifactorial approach. However, it is very difficult or wholly impossible to extract specific fall-related outcomes from these studies.
For a holistic fall prevention approach, further risk factors need to be included, such as visual problems, hearing impairment, syncope, incontinence, fall history, medication, inadequate clothing, cognitive decline, substance abuse and institutionalisation.
In summary, the challenges for a successful transfer of international fall prevention knowledge into the Swiss context are as follows: the efficiency of an intervention, acceptance and motivation of programme providers (e.g., instructors), the quality of the measures implemented and the programmes’ sustainability. Finally, it must be noted that not only the provision of fall prevention programmes, but also the demand of the target population itself – the vulnerable older people who are likely to derive the greatest benefit – is crucial for successful fall prevention. Prevention of falls is an active research area and for this reason it is recommended that these results be updated and revised in the near future.
Acknowledgements:Listed in alphabetical order
Christoph Bauer, MSc, Institute for Physiotherapy, Zurich University of Applied Sciences (ZHAW)
Andreas Biedermann, MD, Public Health Services GmbH, Herzogenbuchsee
Christophe Büla, MD, University Hospital Centre of Vaud (CHUV)
Esther Kaiser, Nurse, Home Medical Care (Spitex) Bäretswil
Silvia Knuchel, Physiotherapist, Citizens’ Hospital Solothurn
Eva Martin-Diener, MSc, Institute for Social and Preventive Medicine, University of Zurich
Frank Michel, PhD, Swiss Council for Accident Prevention (bfu)
Elsbeth Müller, MSc, Ergotherapy Einsiedeln
Jürg Naef, MD, Swiss Association of General Practitioners (SGAM)
Stefan Neuner-Jehle, MD, Institute of General Practice, University of Zurich
Barbara Pfenninger, Research Associate, Swiss Council for Accident Prevention (bfu)
Heidi Schmocker, Nurse, Pro Senectute Canton Bern
Laurence Seematter-Bagnoud, MD, Institute of Social and Preventive Medicine (IUMSP), University of Lausanne
Marielle Tschopp, Physiotherapist, Hospital Zofingen
Ruth Walter, Ergotherapy Swiss Red Cross, Canton Basel-Land
Lukas Zahner, PhD, Institute of Exercise and Health Sciences (ISSW), University of Basel
Literature search
1 Federal Statistical Office. Demographic portrait of Switzerland. 2009, Neuenburg.
2 Sattin RW. Falls among older persons: a public health perspective. Annu Rev Public Health. 1992;13:489–508.
3 Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319:1701–7.
4 Pijnappels M, van der Burg PJ, Reeves ND, van Dieen JH. Identification of elderly fallers by muscle strength measures. Eur J Appl Physiol. 2008;102:585–92.
5 Hausdorff JM, Rios DA, Edelberg HK. Gait variability and fall risk in community-living older adults: a 1-year prospective study. Arch Phys Med Rehabil. 2001;82:1050–6.
6 Pretto M, Spirig R, Kaelin R, Muri-John V, Kressig RW, Suhm N. Outcomes of elderly hip fracture patients in the Swiss healthcare system: a survey prior to the implementation of DRGs and prior to the implementation of a Geriatric Fracture Centre. Swiss Med Wkly. 2010;24:140:w13086. doi: 10.4414/smw.2010.13086.
7 Fletcher PC, Hirdes JP. Restriction in activity associated with fear of falling among community-based seniors using home care services. Age Ageing. 2004;33(3):273–9.
8 Tinetti ME, Mendes de Leon CF, Doucette JT, Baker DI. Fear of falling and fall-related efficacy in relationship to functioning among community-living elders. J Gerontol. 1994;49:M140–7.
9 Campbell AJ, Borrie MJ, Spears GF, Jackson SL, Brown JS, Fitzgerald JL. Circumstances and consequences of falls experienced by a community population 70 years and over during a prospective study. Age Ageing. 1990;19(2):136–41.
10 Rubenstein LZ: Falls in older people. epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35(Suppl 2):ii37–41.
11 Rubenstein LZ, Josephson KR. The epidemiology of falls and syncope. Clin Geriatr Med. 2002;18:141–58.
12 Lord SR, Sherrington C, Menz HB. Falls in older people: risk factors and strategies for prevention. 2007, Cambridge: Cambridge University Press.
13 Skelton DA, Todd C. What are the main risk factors for falls amongst older people and what are the most effective interventions to prevent these falls? How should interventions to prevent falls be implemented? 2004, Denmark: World Health Organisation Health Evidence Network, World Health Organisation.
14 Tinetti ME. Clinical practice. Preventing falls in elderly persons. N Engl J Med. 2003;348(1):42–9.
15 Australian Community Care. Guidebook for preventing falls and harm from falls in older people: best practice guidelines for Australian Community Care. 2009: Australian Commission on Safety and Quality in Health Care.
16 Gillespie LD, Robertson MC, Gillespie WJ, Lamb SE, Gates S, Cumming RG, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2009;(2):CD007146. DOI: 10.1002/14651858.
17 Stevens JA, Sogolow ED. Preventing falls: what works. A CDC compendium of effective community-based interventions from around the world. 2008, Atlanta: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control.
18 Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–M57.
19 Nowalk MP, Prendergast JM, Bayles CM, D'Amico FJ, Colvin GC. A randomized trial of exercise programs among older individuals living in two long-term care facilities: the fallsfree program. J Am Geriatr Soc. 2001;49:859–65.
20 Choi JH, Moon JS, Song R. Effects of sun-style tai chi exercise on physical fitness and fall prevention in fall-prone older adults. J Adv Nurs. 2005;51:150–7.
21 http://www.pedro.org.au . accessed in April 2011.
22 Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83(3):713–21.
23 Tooth L, Bennett S, McCluskey A, Hoffmann T, McKenna K, Lovarini M. Appraising the quality of randomized controlled trials: inter-rater reliability for the OTseeker evidence database. Eval Clin Pract. 2005;11(6):547–55.
24 Li F, Harmer P, Fisher JK, McAuley E, Chaumeton N, Eckstrom E, Wilson NL. Tai chi and fall reductions in older adults: a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2005;60(2):187–94.
25 Inokuchi S, Matsusaka N, Hayashi T, Shindo H. Feasibility and effectiveness of a nurse-led community exercise programme for prevention of falls among frail elderly people: a multi-center controlled trial. J Rehabil Med. 2007;39:479–85.
26 Faber MJ, Bosscher RJ, Chin A, Paw MJ, van Wieringen PC. Effects of exercise programs on falls and mobility in frail and pre-frail older adults: a multicenter randomized controlled trial. Arch Phys Med Rehabil. 2006;87:885–96.
27 Trombetti A, Hars M, Herrmann FR, Kressig RW, Ferrari S, Rizzoli R. Effect of music-based multitask training on gait, balance, and fall risk in elderly people: a randomized controlled trial. Arch Intern Med. 2011;171(6):525–33.
28 Bauer JM. Nutrition in older persons: basis for functionality and quality of life. Der Internist. 2011:1–8.
29 Annweiler C, Montero-Odasso M, Schott AM, Berrut G, Fantino B, Beauchet O. Fall prevention and vitamin D in the elderly: an overview of the key role of the non-bone effects. J Neuroeng Rehabil. 2010;7:50.
30 Campbell AJ, Robertson MC, La Grow SJ, Kerse NM, Sanderson GF, Jacobs RJ, et al. Randomised controlled trial of prevention of falls in people aged over or equal 75 with severe visual impairment: the VIP trial. BMJ. 2005;331(7520):817.
31 Cumming RG, Thomas M, Szonyi G, Salkeld G, O’Neill E, Westbury C, et al. Home visits by an occupational therapist for assessment and modification of environmental hazards: a randomized trial of falls prevention. J Am Geriatr Soc. 1999;47:1397–402.
32 Lannin NA, Clemson L, McCluskey A, Lin CW, Cameron ID, Barras S. Feasibility and results of a randomised pilot-study of pre-discharge occupational therapy home visits. BMC Health Serv Res. 2007;14(7):42.
33 Lin MR, Wolf SL, Hwang HF, Gong SY, Chen CY. A randomized, controlled trial of fall prevention programs and quality of life in older fallers. J Am Geriatr Soc. 2007;55:499–506.
34 Day L, Fildes B, Gordon I, Fitzharris M, Flamer H, Lord S. Randomised factorial trial of falls prevention among older people living in their own homes. BMJ. 2002;325:128.
35 Stevens M, Holman CD, Bennett N, de Klerk N. Preventing falls in older people: outcome evaluation of a randomized controlled trial. J Am Geriatr Soc. 2001;49:1448–55.
36 American Geriatrics Society, British Geriatrics Society, American Academy of Orthopedic Surgeons Panel on Falls Prevention. Summary of the updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc. 2011;59:148–57.
37 Kelsey JL, Berry SD, Procter-Gray E, Quach L, Nguyen US, Li W, et al. Indoor and outdoor falls in older adults are different: the maintenance of balance, independent living, intellect, and Zest in the Elderly of Boston Study. J Am Geriatr Soc. 2010;58(11):2135–41.
38 Menz HB, Morris ME, Lord SR. Footwear characteristics and risk of indoor and outdoor falls in older people. Gerontology. 2006;52(3):174–80.
39 Koepsell TD, Wolf ME, Buchner DM, Kukull WA, LaCroix AZ, Tencer AF, et al. Footwear style and risk of falls in older adults. J Am Geriatr Soc. 2004;52(9):1495–501.
40 Larsen ER, Mosekilde L, Foldspang A. Correlates of falling during 24 h among elderly Danish community residents. Prev Med. 2004;39(2):389–98.
41 Sherrington C, Menz HB. An evaluation of footwear worn at the time of fall-related hip fracture. Age Ageing. 2003;32(3):310–4.
42 Hourihan F, Cumming RG, Taverner-Smith KM, Davidson I. Footwear and hip fracture-related falls in older people. Australas J Ageing. 2000;19(2):91–3.
43 Tencer AF, Koepsell TD, Wolf ME, Frankenfeld CL, Buchner DM, Kukull WA, et al. Biomechanical properties of shoes and risk of falls in older adults. J Am Geriatr Soc. 2004;52(11):1840–6.
44 Berg K, Wood-Dauphinee S, Williams JI. Clinical and laboratory measures of postural balance in an elderly population. Physiotherapy Canada. 1989;41:304–11.
45 McKiernan FE. A simple gait-stabilizing device reduces outdoor falls and nonserious injurious falls in fall-prone older people during the winter. J Am Geriatr Soc. 2005;53(6):943–7.
46 Bateni H, Heung E, Zettel J, McLlroy WE, Maki BE. Can use of walkers or canes impede lateral compensatory stepping movements? Gait & Posture. 2004a;20(1):74–83.
47 Bateni H, Zecevic A, McIlroy WE, Maki BE. Resolving conflicts in task demands during balance recovery: does holding an object inhibit compensatory grasping? Exp Brain Res. 2004b;157(1):49–58.
48 Bateni H, Maki BE. Assistive devices for balance and mobility: benefits, demands, and adverse consequences. Arch Phys Med Rehabil. 2005;86(1):134–45.
49 Perell KL, Nelson A, Goldman RL, Luther SL, Prieto-Lewis N, Rubenstein LZ. Fall risk assessment measures: an analytic review. J Gerontol A Biol Sci Med Sci. 2001;56(12):M761–6.
50 Simpson C, Pirrie L. Walking aids: a survey of suitability and supply. Physiotherapy. 1991;77:231–4.
51 Kressig RW. Stürze. In: Stoppe G, Mann E. Geriatrics for general practitioners. 2009, Bern: Verlag Hans Huber.
52 Feder G, Cryer C, Donovan S, Carter Y. Guidelines for the prevention of falls in people over 65. BMJ. 2000;321(7267):1007–11.
53 Tinetti ME, Baker DI, King M, Gottschalk M, Murphy TE, Acampora D, et al. Effect of dissemination of evidence in reducing injuries from falls. N Engl J Med. 2008;359(3):252–61.
54 Gschwind YJ, Wolf I, Bridenbaugh SA, Kressig RW. Best practice health promotion for older people (BPGF): falls prevention. http://www.gesundheitsfoerderung.ch/pdf_doc_xls/d/gesundheitsfoerderung_und_praeventition/allgemeines/bpgfa/d/BPGFA-Sturzpraevention-Gesamtstudie-2011.pdf
55 Barnett A, Smith B, Lord SR, Williams M, Baumand A. Community-based group exercise improves balance and reduces falls in at-risk older people: a randomised controlled trial. Age Ageing. 2003;32:407–14.
56 Campbell A, Robertson M, Gardner M, Norton R, Buchner D. Falls prevention over 2 years: a randomized controlled trial in women 80 years and older. Age Ageing. 1999;28:513–8.
57 Logghe IH, Zeeuwe PE, Verhagen AP, Wijnen-Sponselee RM, Willemsen SP, Bierma-Zeinstra SM, et al. Lack of effect of tai chi chuan in preventing falls in elderly people living at home: a randomized clinical trial. J Am Geriatr Soc. 2009;57:70–5.
58 Robertson MC, Devlin N, Gardner MM, Campbell AJ. Effectiveness and economic evaluation of a nurse delivered home exercise programme to prevent falls. a randomised controlled trial. BMJ. 2001;322:1–6.
59 Buchner DM, Cress ME, de Lateur BJ, Esselman PC, Margherita AJ, Price R, Wagner EH. The effect of strength and endurance training on gait, balance, fall risk, and health services use in community-living older adults. J Gerontol A Biol Sci Med Sci. 1997;52A:M218–24.
60 Rubenstein LZ, Josephson KR, Trueblood PR, Loy S, Harker JO, Pietruszka FM, et al. Effects of a group exercise program on strength, mobility, and falls among fall-prone elderly men. J Gerontol A Biol Sci Med Sci. 2000;55:M317–21.
61 Voukelatos A, Cumming RG, Lord SR, Rissel C. A randomized, controlled trial of tai chi for the prevention of falls: the central Sydney tai chi trial. J Am Geriatr Soc. 2007;55:1185–91.
62 Wolf SL, Sattin RW, Kutner M, O'Grady M, Greenspan AI, Gregor RJ. Intense tai chi exercise training and fall occurrences in older, transitionally frail adults: a randomized, controlled trial. J Am Geriatr Soc. 2003;51:1693–701.
63 Yamada M, Tanaka B, Nagai K, Aoyama T, Ichihashi N. Trail-walking exercise and fall risk factors in community-dwelling older adults: preliminary results of a randomized controlled trial. J Am Geriatr Soc. 2010;58(10):1946–51.
64 Iwamoto J, Suzuki H, Tanaka K, Kumakubo T, Hirabayashi H, Miyazaki Y, et al. Preventative effect of exercise against falls in the elderly: a randomized controlled trial. Osteoporos Int. 2009;20:1233–40.
65 Lord SR, Castell S, Corcoran J, Dayhew J, Matters B, Shan A, Williams P. The effect of group exercise on physical functioning and falls in frail older people living in retirement villages: a randomized, controlled trial. J Am Geriatr Soc. 2003;51:1685–92.
66 Luukinen H, Lehtola S, Jokelainen J, Väänänen-Sainio R, Lotvonen S, Koistinen P. Pragmatic exercise-oriented prevention of falls among the elderly: a population-based, randomized, controlled trial. Prev Med. 2007;44:265–71.
67 Skelton D, Dinan S, Campbell M, Rutherford O. Tailored group exercise (Falls Management Exercise – FaME) reduces falls in community-dwelling older frequent fallers (an RCT). Age Ageing. 2005;34:636–9.
68 Weerdesteyn V, Rijken H, Geurts ACH, Smits-Engelsman BCM, Mulder T, Duysen J. A five-week exercise program can reduce falls and improve obstacle avoidance in the elderly. Gerontology. 2006;52:131–41.
69 Wolf SL, Huimnan XB, Nancy GK, Elizabeth M, Carol C, Tingsen X. Selected as the best paper in the 1990s: reducing frailty and falls in older persons: an investigation of tai chi and computerized balance training. J Am Geriatr Soc. 2003;51(12):1794–803.
70 Means KM, Rodell DE, O'Sullivan PS. Balance, mobility, and falls among community-dwelling elderly persons: effects of a rehabilitation exercise program. Am J Phys Med Rehabil. 2005;84:238–50.
71 Morgan RO, Virnig BA, Duque M, Abdel-Moty E, DeVito CA. Low-intensity exercise and reduction of the risk for falls among at-risk elders. J Gerontol A Biol Sci Med Sci. 2004;59:M1062-7.
72 Campbell AJ, Robertson MC, Gardner MM, Norton RN, Tilyard MW, Buchner DM. Randomised controlled trial of a general practice programme of home based exercise to prevent falls in elderly women. BMJ. 1997;315:1065-9.
73 Lin M-R, Hwang H-F, Wang Y-W, Chang S-H, Wolf SL. Community-based tai chi and its effect on injurious falls, balance, gait, and fear of falling in older people. Phys Ther. 2006;86:1189-201.
74 Lord SR, Ward JA, Williams P, Strudwick M. The effect of a 12-month exercise trial on balance, strength, and falls in older women: a randomized controlled trial. J Am Geriatr Soc. 1995;43:1198-1206.