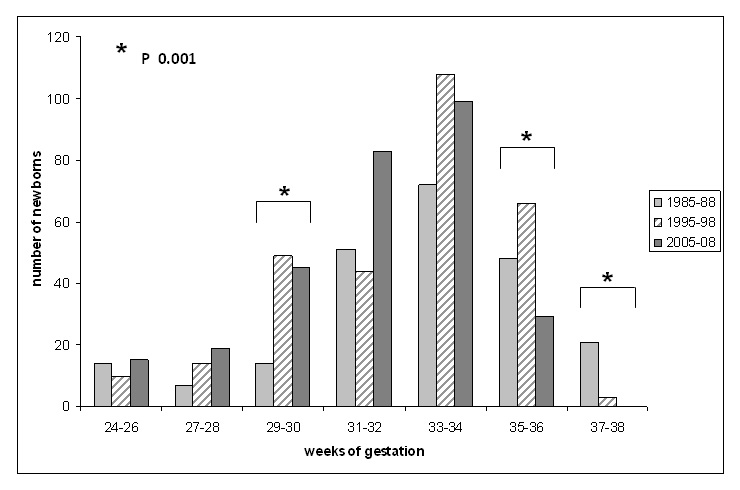
Figure 1
Distribution of live born triplets according to gestational age in the three Swiss surveys.
DOI: https://doi.org/10.4414/smw.2011.13308
The dramatic increase in the incidence of higher-order multiple births since the mid-seventies is well documented in medical literature [1–4] and is mainly related to assisted reproductive technology (ART). In addition to the economic and logistical problems associated with multiple births, these infants have a high mortality and morbidity rate compared with those of singletons [3–6]. Switzerland’s first national epidemiological survey was performed from 1985 to 1988 and published in 1992 [7]. Ten years later, a second national survey with the same study design analysed higher-order multiple births between 1995 and 1998 and was published in 2003 [8]. This second study also compared the mortality and morbidity of triplets to matched singletons. Ten years later, we decided to conduct a third national survey in Switzerland.
The objectives of the study are to determine the incidence of higher-order multiple births in Switzerland, to evaluate the neonatal morbidity and perinatal mortality, and to analyse the change observed within this population over the last two decades.
The present study is retrospective. All 136 Swiss obstetrics departments were contacted and invited to supply details on the number of higher-order multiple births in their hospitals between 1 January 2005 and 31 December 2008. Deliveries before 24 0/7 weeks of gestation were excluded, as these infants usually receive comfort care in accordance with the guidelines of the Swiss Society of Neonatology. All perinatal centres and hospitals (collectively “hospitals”) with integrated neonatal units answered, a few small hospitals with fewer than 500 deliveries per year did not. The probability that higher-order multiple births occur in these hospitals is very low. A comparison with data from the Swiss Federal Statistical Office revealed that 95% of all triplet deliveries and 100% of all quadruplet and quintuplet births were included in the present survey. One investigator (SE) visited the hospitals in order to collect data about the pregnancy, the birth and the neonatal outcome. A few hospitals sent their data to this investigator. All data were processed anonymously. The results were compared with data from the first (1985 to 1988) and second (1995 to 1998) Swiss national surveys. All three surveys were based on the same methodology. Data were collected retrospectively by a single investigator on the basis of the same protocol. The investigator in the first survey (RAM) visited all hospitals in order to analyse the medical records. By the time of the second and third surveys, the majority of hospitals had switched to electronic medical records, which they sent anonymously to the investigator.
For the purpose of this study, following definitions were used: growth retardation was defined as a birth weight below the third percentile according to Voigt et al. [9]; respiratory distress was defined according to the Swiss Society of Neonatology as the presence of at least two of the following clinical signs: cyanosis while breathing room air, grunting, tachypnoea >60/min, nasal flaring, and intercostal retractions. Bronchopulmonary dysplasia was defined according to Bancalari as the requirement for supplemental oxygen by the postmenstrual age of 36 weeks [10]. In regards to cerebral ultrasound, the definition of intracranial haemorrhage was that of Papile [11] and periventricular leukomalacia was defined according to de Vries [12].
Statistics: A chi-square test was used to analyse proportions and a t-test to compare groups with normally distributed variables, and a Mann Whitney U test was used for non-normal distribution. A value of p <0.05 was considered statistically significant.
From 1 January 2005 to 31 December 2008, a total of 108 higher-order multiple births (105 triplet births, two quadruplet births and one quintuplet birth) were recorded by the Swiss Federal Statistical Office. The incidence of higher multiple births during the study period is therefore 35.3/100,000 live births for triplets, 0.7/100,000 live births for quadruplets, and 0.3/100,000 live births for quintuplets. Considering an average number of live births in Switzerland of about 75,000 per year during the study period, this means that about 26 triplet deliveries are observed every year. Over the last twenty years, the incidence of quadruplet births in Switzerland has decreased, whereas that of triplet births is in constant progression (table 1).
No details were obtained for five of the triplet sets. We analysed data from the remaining 103 higher-order multiple births (100 triplet births, two quadruplet births and one quintuplet birth). Ten triplets but no quadruplet or quintuplet died in utero, making a total of 303 live-born higher-order multiples.
| Table 1: Incidence of higher-order multiple births in Switzerland over the last twenty years. | ||||
| Triplet births | Quadruplet births | Quintuplet births | Higher-order multiple births, total | |
| 1985–88 | 25.2 | 2.9 | 0.0 | 28.1 |
| 1995–98 | 30.8 | 1.2 | 0.0 | 32.0 |
| 2005–08 | 35.3 | 0.7 | 0.3 | 36.3 |
| Incidence = n per 100000 live births | ||||
In 9% of triplet pregnancies, the method of conception is not known. Out of the remaining 91 triplet pregnancies, 25 (27.4%) occurred spontaneously, 22 (24.2%) after ovulation induction (OI) and 44 (48.4%) after in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI). The quintuplet pregnancy and one of the quadruplet pregnancies occurred after OI and the second quadruplet pregnancy after IVF. Therefore, all quadruplet and quintuplet pregnancies were the result of ART.
The mothers were 33 years old on average, ranging from 22 to 47 years, with no significant difference between spontaneous conception and ART.
Pregnancies were complicated by premature contractions (79%), premature prolonged rupture of membranes (16%), preeclampsia (10%) or gestational diabetes (5%). 51% of women were given intravenous tocolysis and prenatal steroids were administered to 89% of mothers.
All higher-order multiple births were premature. The median gestational age (GA) was 32 1/7 weeks for triplets (range 24 5/7 to 35 6/7 weeks), 29 2/7 weeks for quadruplets (range 27 6/7 to 30 4/7 weeks) and 28 4/7 weeks for the only set of quintuplets.
All quadruplet and quintuplet deliveries and 94% of triplet deliveries occurred in a perinatal centre with an integrated neonatal intensive care unit (NICU). The remaining 6% of triplet births occurred in a hospital with an integrated level II neonatal unit. One of these 18 triplets had to be transferred to a NICU after birth, and five other multiples were subject to immediate postnatal transfer to another NICU because of capacity problems. Thus, 2% of infants were out-born.
All infants were delivered by caesarean section apart from one set of triplets because of poor prognosis due to severe hydrops at 24 weeks of gestation, and the first baby of a quadruplet pregnancy who was delivered spontaneously before an emergency caesarean section was performed in order to deliver the other three babies.
The median birth weight was 1614 g for triplets (range 540 to 2940 g), 1157 g for quadruplets (range 740 to 1405 g) and 1066 g for quintuplets (range 890 to 1380 g). Growth retardation was observed in 2% of triplets but not in any of the quadruplets or quintuplets.
The gender of 9 of the 10 triplets who died in utero is not known. For the remaining 291 triplets, the male to female ratio was 1 to 1.1. The small sample of quadruplets and quintuplets had a male to female ratio of 1 to 2.3.
The majority of higher-order multiples required cardiopulmonary resuscitation within the first few minutes of life. 66% of triplets and 100% of quadruplets and quintuplets were given supplemental oxygen. Bag and mask ventilation was required for 32% of triplets, 75% of quadruplets and 60% of quintuplets. 49% of triplets received nasal continuous positive airway pressure (CPAP) and a further 7% were intubated. 100% of quadruplets and quintuplets were given nasal CPAP in the delivery room; three quadruplets subsequently required endotracheal intubation in the delivery room.
No information was available on the determination of blood groups, examination of placenta membranes, or genetic analysis. It was therefore not possible to determine chorionicity or zygoty.
Table 2 lists neonatal morbidity and mortality for the triplets with a breakdown according to GA. 70% of triplets and 100% of quadruplets and quintuplets presented with respiratory distress. Surfactant deficiency was the main cause of respiratory distress, followed by transient tachypnoea. Surfactant deficiency was also the most frequent pathology associated with mechanical ventilation. 13% of triplets (38/287), 38% of quadruplets (3/8) and 100% of quintuplets (5/5) required mechanical ventilation over a period of time ranging from one to thirty days (median 6 days). Nasal CPAP was administrated to 51% of triplets (147/289) and 100% of quadruplets and quintuplets (15/15) over a median period of six days (range 1 to 59 days). 49% of triplets and 100% of quadruplets and quintuplets were given supplemental oxygen during a median period of 10 days (1-98) for triplets, 20 days (1-60) for quadruplets and 18 days (2-52) for the only set of quintuplets. Bronchopulmonary dysplasia was observed in 13 triplets (5%), all of which were born with a GA of less than 32 weeks.
Cerebral ultrasound was performed in 94% of triplets and 100% of quadruplets and quintuplets. A severe intracranial haemorrhage of grade III with or without venous infarction was observed in three triplets, two of whom died. Periventricular leukomalacia of grade I was observed in 13% of triplets (38/285), 50% of quadruplets (4/8) and 80% of quintuplets (4/5). Five triplets (2%) and one quintuplet (13%) subsequently developed bilateral cystic periventricular leukomalacia.
| Table 2: Neonatal morbidity in live born triplets related to their gestational age. | |||||
| Total | <26 weeks | 26–28 weeks | 29–31 weeks | 32–36 weeks | |
| Respiratory distress | 200/287 (69.7%) | 6/6 (100%) | 28/28 (100%) | 64/69 (92.8%) | 102/184 (55.4%) |
| Surfactant deficiency | 66/287 (23.0%) | 6/6 (100%) | 24/28 (85.8%) | 26/69 (37.7%) | 10/184 (5.4%) |
| BPD in survivors | 13/280 (4.6%) | 0/0 | 8/27 (29.6%) | 5/69 (7.2%) | 0/184 (0%) |
| Respiratory support (mechanical ventilation and/or CPAP) | 185/287 (64.4%) | 6/6 (100%) | 25/28 (89.3%) | 61/69 (88.4%) | 93/184 (50.5%) |
| Intracranial haemorrhage grade ≥III | 3/267 (1.1%) | 1/6 (20.0%) | 1/27 (3.7%) | 1/68 (1.5%) | 0/166 (0%) |
| Persistent ductus arteriosus, treated | 33/269 (12.3%) | 0/6 (0%) | 14/28 (50.0%) | 18/69 (26.1%) | 1/166 (0.6%) |
| Proven necrotising enterocolitis | 8/287 (2.8%) | 0/6 (0%) | 2/28 (7.1%) | 3/69 (4.3%) | 3/184 (1.6%) |
| ROP all grades in survivors | 6/125 (4.8%) | 0/0 | 4/23 (17.4%) | 2/49 (4.1%) | 0/53 (0%) |
| Neonatal mortality | 7/287 (2.4%) | 6/6 (100%) | 1/28 (3.6%) | 0/69 (0%) | 0/184 (0%) |
| BPD = bronchopulmonary dysplasia; CPAP = continuous positive airways pressure; ROP = retinopathy of prematurity. | |||||
Ten triplets died in utero, seven further triplets died during the first four days of life. All of these had a GA of less than 28 weeks and six out of seven of less than 26 weeks (table 2). Perinatal mortality was thus 6% for triplets. None of the quadruplets or quintuplets died. A comparison between spontaneous and assisted triplet pregnancies showed no significant differences regarding maternal age, GA, birth weight and perinatal mortality.
Nearly one third of all higher-order multiples were transferred at some stage to another hospital closer to the family’s domicile. For these infants, the period of time from birth to discharge home is not known. For the remaining infants, the median hospital stay was 33 days for triplets (range 1–117 days), 62 days for quadruplets (range 43–81 days) and 156 days for quintuplets (range 61–517 days).
Compared with the first two Swiss national surveys on higher-order multiple births [7–8], the incidence of quadruplet and quintuplet births has decreased over time, whereas the incidence of triplet births is in constant progression (table 1). The evolution of neonatal outcome of quadruplets and quintuplets is difficult to describe because of the small sample. Regarding triplet births, the maternal age increased from 29 to 33 years, the GA declined by one week and the birth weight diminished by about 10% as a result. Table 3 contains a comparison between the first and the third triplet populations.
| Table 3: Outcome of triplets in the three Swiss national surveys and comparison between the first and the third studies. | ||||
| Group 1 1985–88 N = 227 | Group 2 1995–98 N = 294 | Group 3 2005–08 N = 290 | Pv between groups 1 and 3 | |
| Maternal age (years) | 29 | NA | 33 | |
| Method of conception (%): | ||||
| – Spontaneous | 39 | 30 | 25 | <0.001 |
| – Ovulation induction | 50 | 29 | 22 | <0.001 |
| – IVF or ICSI | 11 | 32 | 44 | <0.001 |
| – Others or unknown | 9 | 9 | <0.001 | |
| Gestational age (weeks) | 33 + 0 | 32 + 5 | 32 + 1 | |
| Delivery in perinatal centre (%) | 56 | 73 | 94 | <0.001 |
| Caesarean section (%) | 90 | 97 | 99 | <0.001 |
| Birth weight (g) | 1787 | 1665 | 1614 | |
| Respiratory distress (%): | 66 | 52 | 70 | ns |
| – Surfactant deficiency | 18 | 22 | 23 | ns |
| – Transient tachypnoea | 44 | 16 | 13 | <0.001 |
| – Other | 4 | 14 | 34 | <0.001 |
| Respiratory support (%): | 19 | 39 | 64 | <0.001 |
| – Mechanical ventilation | 18 | 16 | 13 | <0.05 |
| – CPAP | 1 | 23 | 51 | <0.001 |
| BPD (%) | 5 | 1 | 5 | ns |
| Proven NEC (%) | 2 | NA | 3 | ns |
| Cerebral ultrasound performed (%) | 33 | 73 | 94 | <0.001 |
| – ICH, all grades (%) | 26 | 15 | 9 | <0.001 |
| – PVL >14 days or cystic PVL (%) | 3 | 3 | 13 | <0.001 |
| Perinatal mortality (%) | 13 | 6 | 6 | <0.001 |
| NA = not available; ns = not significant. | ||||
In this third population-based national survey, the incidence of higher-order multiple births was 35.3/100,000 live births for triplets, 0.7/100,000 live births for quadruplets and 0.3/100,000 live births for quintuplets. It is difficult to compare our findings on quadruplets and quintuplets with the literature because these births are very rare. Regarding triplet births, our incidence correlates with international data [13–16], ranging from 4/100,000 to 150/100,000 live births. However, comparison is not always reliable because the lowest limit of GA varies. The rarity of incidence of quintuplets prohibits any meaningful comparison with data from the first and the second Swiss surveys [7–8]. The incidence of quadruplets dropped to 25% of the level observed in the mid-eighties. This improvement may be attributed to the restrictive legislation introduced in Switzerland in 2001, which permitted a maximum of three embryos to be transferred and caused most fertility centres to limit the number of replaced embryos to two for the majority of patients (FIVNAT-CH) [17]. In contrast, the incidence of triplet births increased by 40% over the last twenty years (table 1). This increase is alarming and also difficult to explain. Average maternal age, known to be associated with multiple pregnancies, shifted from 29 to 33 years between the first and the third survey. However, the percentage of spontaneous triplet pregnancies decreased from 39% to 25% (p <0.001) and no significant difference in maternal age between spontaneous and assisted higher-order multiple pregnancies was observed. Multifetal pregnancy reduction of quadruplets or quintuplets to triplets may also play a minor role but this information is usually not available in the patients’ files. Thus, ART is probably the main reason for the high incidence of triplet births [1–4]. In Switzerland, pregnancies assisted by embryo transfer are subject to supervision by the local authorities which grant permission to perform ART only to gynaecologists with specific qualifications in this field. Some authors [4, 18–19] even recommend “single-embryo transfer” in order to eliminate twins or triplets in IVF. On the other hand, there is no law forbidding doctors from prescribing ovulation-stimulating drugs. Compared to embryo transfer, OI is easier to perform, cheaper, and the cost of the hormonal treatment is assumed by health insurance companies [20]. Twenty years ago, 50% of all triplet pregnancies were attributable to OI. Today, this percentage has fallen to 22% (table 3), which is still too high, considering that OI can lead to a pregnancy with an uncontrolled high number of embryos. While a constant two thirds of triplet pregnancies during the three surveys came about following ART, the remaining pregnancies were either documented as spontaneous, or not documented. Since the mode of conception is not always accurate because some parents prefer not to inform their doctor of it, the number of assisted conceptions could be even higher than assessed. A further problem is the place where ART is performed; this information was all but impossible to obtain from our present data. However, a survey performed in Zurich over seven years (data unpublished) revealed that, of the triplets not spontaneously conceived and born at Zurich University Hospital, only 23% were the result of treatment in Zurich. Another 43% were the result of treatment within Switzerland and 34% of treatment in a foreign country. This “infertility tourism” plays an important role in the incidence observed and is also very difficult to control.
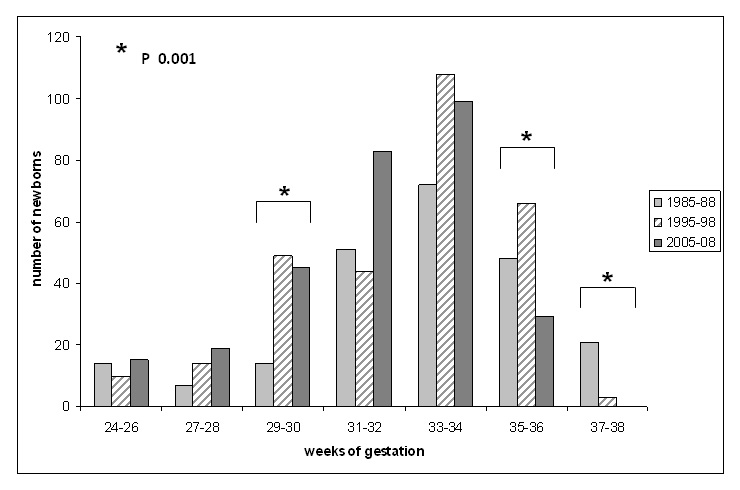
Figure 1
Distribution of live born triplets according to gestational age in the three Swiss surveys.
International literature [13–14, 16] demonstrated a dramatic rise of up to 400% in the incidence of higher-order multiple pregnancies from the mid-seventies till the mid-nineties but since then, several countries such as Norway, Finland, Sweden and England and Wales were able to demonstrate a regular decrease [13–16, 21], an achievement that is hardly detectable in the United States and still missing in Switzerland.
The mean GA of triplets is comparable with data in the literature [8, 16, 22–24] but fell from 33 to 32 weeks of gestation within twenty years. Not surprisingly, the mean birth weight of 1614 g is also about 10% lower compared with the first survey [7] but still corresponds to international data [16, 22–24], which gives a range of 1437 to 1736 g. The birth weight of quadruplets and quintuplets was comparable with the findings of Strauss et al. [24] but the small samples in both studies make a comparison difficult.
One of the most promising changes over the last two decades is the increasing centralisation, which improved from 56% twenty years ago to 94% at present. This is clearly in accordance with the guidelines of the Swiss Society of Neonatology [25]. Few infants required postnatal transfer, and all but one did so because of capacity problems in the primary NICU, an ongoing problem in Switzerland. This pinpoints the logistical problems encountered by the sudden arrival of three, four or five small premature infants. Figure 1 shows the breakdown of live born triplets according to their GA in the three surveys. Comparison between the first and the third studies demonstrates a shift towards more premature infants.
The neonatal morbidity of higher-order multiples is mainly marked by respiratory problems occurring in two-thirds of triplets and 100% of quadruplets and quintuplets. Whereas the incidence of respiratory distress, hyaline membrane and bronchopulmonary dysplasia disease unfortunately remains constant over the time, the respiratory treatment has changed considerably. The first Swiss survey twenty years ago mentioned that 19% of triplets were dependent on respiratory assistance (mechanical ventilation or nasal CPAP), while this was the case for 39% in the second survey and 64% (p <0.001) in the third. We observed a fall in mechanical ventilation and a massive increase in the use of nasal CPAP, which is employed more frequently nowadays. We think that many infants in the first survey would have benefited from CPAP support but the technology was not always available.
Neurological morbidity is much better documented nowadays than twenty years ago (table 3). While the incidence of intracranial haemorrhage has decreased, that of periventricular leukomalacia has increased over the time. A probable explanation is that current ultrasound machines are performing better and neonatologists are better aware of the need to test for white matter disease. Adverse neurodevelopmental outcome of triplets compared to singletons is well documented in the literature [3–4, 26–28] and the second Swiss survey also demonstrated a trend towards more intracranial haemorrhage and periventricular leukomalacia compared with singletons. Concerning this matter, it would be helpful to determine chorionicity in higher-order multiples, as dichorionic triplets have a significantly higher mortality and morbidity rate than trichorionic triplets [29–30]. Unfortunately, this issue was poorly documented in our study group.
The perinatal mortality of triplets dropped significantly from 13% to 6% between the first and the second survey [8] but has remained stable since. All but one infant who died had a GA of less than 26 weeks. Despite the small sample, it seems logical to attribute the mortality to the extreme prematurity and not to the higher-order multiple birth. However, there is a direct correlation between both, as higher-order multiple births result in premature infants.
The successful decrease in the incidence of quadruplet births in Switzerland is the consequence of the restrictive Swiss legislation introduced in 2001 and attests to the fact that health professionals are aware of the very high risk to which quadruplets are exposed. However, the incidence of triplet births shows an increase of 40% over the last two decades and morbidity has not improved. This demonstrates that ART in Switzerland is not yet under control and monitoring needs to be improved. Infertility treatment in Switzerland should be exclusively managed by specialists recognised by the Swiss Society of Reproductive Medicine, who will not only decide if a pregnancy is possible, but also choose the most appropriate treatment and inform the patients correctly about the risks and consequences thereof, particularly regarding the high neonatal morbidity rate presented by these infants.
Acknowledgement:The authors would like to thank all participating hospitals for their collaboration. Thank you also to Rachel Folkes for editorial assistance.
1 Nakhuda GS, Sauer MV. Addressing the growing problem of multiple gestations created by assisted reproductive therapies. Semin Perinatol. 2005;29:355–62.
2 Reddy UM, Wapner RJ, Rebar RW, Tasca RJ. Infertility, assisted reproductive technology, and adverse pregnancy outcomes: executive summary of a National Institute of Child Health and Human Development Workshop. Obstet Gynecol. 2007;109(4):967–77.
3 Shinwell ES, Haklai T, Eventov-Friedman S. Outcome of multiplets. Neonatology. 2009;95:6–14.
4 Wimalasundera RC, Trew G, Fisk NM. Reducing the incidence of twins and triplets. Best Pract Res Clin Obstet Gynaecol. 2003;17(2):309–29.
5 Imaizumi Y. Infant mortality rates in single, twin and triplet births, and influencing factors in Japan, 1995–98. Paediatr Perinat Epidemiol. 2001;15:346–51.
6 Shinwell ES, Blickstein I, Lusky A, Reichmann B. in collaboration with the Israel Neonatal Network. Excess risk of mortality in very low birthweight triplets: a national, population based study. Arch Dis Child Fetal Neonatal Ed. 2003;88:F36–F40.
7 Arlettaz R, Duc G. Triplés et quadruplés en Suisse, 1985–1988. Schweiz Med Wschr. 1992;122:511–6.
8 Arlettaz R, Paraskevopoulos E, Bucher HU. Triplets and quadruplets in Switzerland: comparison with singletons, and evolution over the last decade. J Perinat Med. 2003;31:242–50.
9 Voigt M, Fusch C, Olbertz D, Hartmann K, Rochow N, Renken C, et al. Analyse des Neugeborenenkollektivs der Bundesrepublik Deutschland: Vorstellung engmaschiger Perzentilwerte (-kurven) für die Körpermasse Neugeborener. Geburtsh Frauenheilk. 2006;66:956–70.
10 Bancalari E, Claure N. Definitions and diagnostic criteria for bronchopulmonary dysplasia. Semin Perinatol. 2006;30(4):164–70.
11 Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1500 gm. J Pediatr. 1978;92(4):529–34.
12 De Vries LS, Eken P, Dubowitz LMS. The spectrum of leukomalacia using cranial ultrasound. Behav Brain Res. 1992;49(1):1–6.
13 Black M, Bhattacharya S. Epidemiology of multiple pregnancy and the effect of assisted conception. Semin Fetal Neonatal Med. 2010;15:306–12.
14 Blickstein I, Keith LG. The decreased rates of triplet births: temporal trends and biologic speculations. Am J Obstet Gynecol. 2005;193:327–31.
15 Simmons R, Doyle P, Maconochie N. Dramatic reduction in triplet and higher order births in England and Wales. BJOG. 2004;111:856–8.
16 Tandberg A, Bjørge T, Nygård O, Børdahl PE, Skjaerven R. Trends in incidence and mortality for triplets in Norway 1967–2006: the influence of assisted reproductive technologies. BJOG. 2010;117:667–75.
17 Schweizerische Gesellschaft für Reproduktionsmedizin: Fortpflanzungsmedizinverordnung des Bundes (FMedV) 4.12.2000.
18 Barri PN, Coroleu B, Clua E, Tur R. Prevention of prematurity by single embryo transfer. J Perinat Med. 2011;39:237–40.
19 De Neubourg D, Gerris J. What about the remaining twins since single-embryo transfer? How far can (should) we go? Hum Reprod. 2006;21(4):843–6.
20 Lüthi T. Das Problem der Mehrlingsschwangerschaften. Schweiz Ärztezeitung. 2006;87(21):943–7.
21 Källén B, Finnström O, Lindam A, Nilsson E, Nygren KG, Otterblad Olausson P. Trends in delivery and neonatal outcome after in vitrofertilization in Sweden: data for 25 years. Hum Reprod. 2010;25(4):1026–34.
22 Battin M, Wise M, DeZoete A, Stone P. Infant and perinatal outcomes of triplet pregnancy in Auckland: better than expected? N Z Med J. 2009;122(1298):39–47.
23 Min SJ, Luke B, Min L, Misiunas R, Nugent C, Van de Ven C, et al. Birth weight references for triplets. Am J Obstet Gynecol. 2004;191:809–14.
24 Strauss A, Paek BW, Genzel-Boroviczény O, Schulze A, Janssen U, Hepp H. Multifetal gestation – maternal and perinatal outcome of 112 pregnancies. Fetal Diagn Ther. 2002;17:209–17.
25 Working group of the Swiss Society of Neonatology. Care and resuscitation of the newborn infant. Paediatrica. 2007;18(3):36–45.
26 Feldman R, Eidelman AI. Does a triplet birth pose a special risk for infant development? Assessing cognitive development in relation to intrauterine growth and mother-infant interaction across the first 2 years. Pediatrics. 2005;115(2):443–52.
27 Topp M, Huusom LD, Langhoff-Roos J, Delhumeau C, Hutton JL, Dolk H, on behalf of the SCPE collaborative group. Multiple birth and cerebral palsy in Europe: a multicenter study. Acta Obstet Gynecol Scand. 2004;83:548–53.
28 Wadhawan R, Oh W, Vohr BR, Wrage L, Das A, Bell EF. Neurodevelopmental outcomes of triplets or higher-order extremely low birth weight infants. Pediatrics. 2011;127:e654–60.
29 Adegbite AL, Ward SB, Bajoria R. Perinatal outcome of spontaneously conceived triplet pregnancies in relation to chorionicity. Am J Obstet Gynecol. 2005;193:1463–71.
30 Bajoria R, Ward SB, Adegbite AL. Comparative study of perinatal outcome of dichorionic and trichorionic iatrogenic triplets. Am J Obstet Gynecol. 2006;194:415–24.
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article was reported.