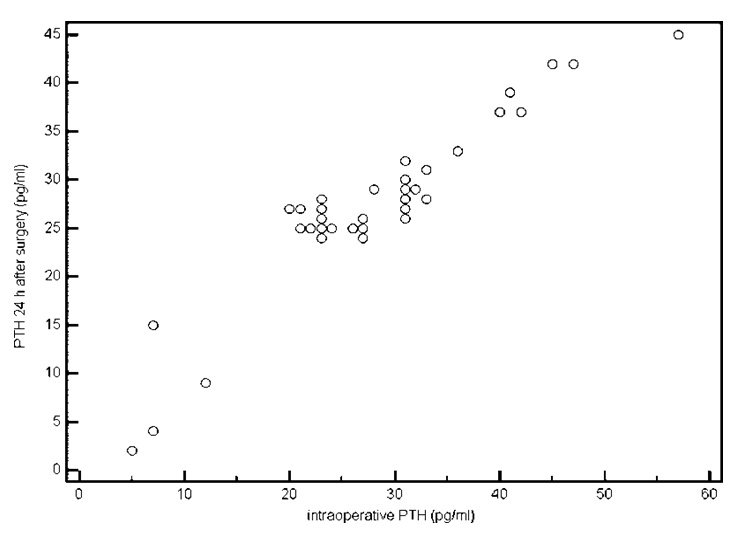
Figure 1
Scatter plot for correlation between intraoperative rapid PTH assay and standard PTH assay taken 24 hours after surgery. Correlation coefficient = 0.95 (P < 0.001).
DOI: https://doi.org/10.4414/smw.2011.13299
In non-neoplastic thyroid diseases, total thyroidectomy is sometimes indicated for cases such as multinodular goiter, obstructive symptoms; retrosternal goiter, even in the absence of obstruction; primary hyperthyroidism or Grave’s disease (that is unresponsive to medical management); recurrent or secondary hyperthyroidism, etc. [1].
Permanent hypoparathyroidism and recurrent laryngeal nerve damage are two major morbidities of thyroid surgery, accounting for most medical litigation [2]. The nerve stimulator is increasingly used to prevent nerve injury during thyroidectomy [3]. Careful dissection and aid of the operating microscope should preserve the important structures in close vicinity to the thyroid gland, namely, the parathyroid glands and the laryngeal nerves. Despite these applications, occasionally postoperative hypoparathyroidism and subsequent hypocalcaemia ensue; causes of such a drop of parathyroid levels may be due to several reasons, such as inadvertent excision of a parathyroid gland(s), which according to Lin et al. (2002)’s study occurred in 9% of patients undergoing thyroidectomy [4], as the majority of patients (95%) had two or less parathyroid glands in their excised specimens, in addition to induced capsular bleeding due to inadvertent incision which commonly occurred [5–7], or indirect injury to the glands by a very meticulous homeostasis technique, with subsequent avascular necrosis. In addition, determination of parathyroid viability based on their color changes may not be reliable [6].
The occurrence of postoperative hypocalcaemia remains the single most important factor predicting the occurrence of permanent hypoparathyroidism [8, 9]. Close postoperative monitoring of serum calcium levels is a standard of care, and concerns about postoperative hypocalcaemia contribute to delays in discharge [10, 11], also measuring plasma calcium levels, the evening after thyroidectomy are of little value in predicting the onset of subsequent hypocalcaemia or symptoms because of its relative slow decline [12], in addition, the relatively infrequent requirement for calcium supplementation suggests that routine treatment is probably not cost-effective and complicates the detection of true hypocalcaemia [10].
But since the half life of the parathyroid hormone in serum is a matter of minutes, (less than 5 min) [13], the determination of intraoperative parathyroid hormone (PTH) levels has been used for insurance of complete surgical ablation of the parathyroid glands in cases of hyperparathyroidism, and has had success rates reaching 96% [14, 15]. In addition, the sensitivity of this test in predicting postoperative calcium levels has been found to be 89% to 97% [16, 17].
By facilitating early hospital discharge and reducing the need for additional serum calcium testing, the rapid PTH assay may avoid the additional costs involved in serum calcium monitoring [18]. One potential additional application of this tool is to select patients for parathyroid autotransplantation during thyroidectomy [19].
The present study aimed to test the sensitivity and specificity of intraoperative rapid PTH assay test for prediction of early and permanent postoperative hypoparathyroidism after total thyroidectomy in patients with multinodular goiter, whether toxic or non-toxic, or diffuse toxic goiter (Graves disease), and the applicability to guide the search for inadvertently removed parathyroid glands for possible auto transplantation.
The study was designed as a prospective study, and was conducted over a one year period from November 2009 to October 2010 at Ain-Shams University Hospitals in one sub-unit from the otolaryngology head and neck surgery department, and one from the general surgery department.
Approval of the ethical and moral committee of the University for the design and protocol of the study was obtained, and an informed consent was obtained from the patients before enrollment.
Patient selection was based upon the fulfillment of the following requirements, age from 20–60 years, no history of previous neck surgery, malignancy, radiotherapy or chemotherapy, having indication for total thyroidectomy (being multinodular goiter, whether toxic or non-toxic, or diffuse toxic goiter (Graves’ disease), not responding or poorly tolerant to medical treatment).
Patients underwent the routine preoperative thyroid gland assessment by the internist, in the form of assessing the levels of T3, FT3, TSH, and having a neck ultrasonography. Additionally, TC99 scan, and FNAC (fine-needle-aspiration-cytology) were done, all aiming to diagnose the thyroid condition. Then the indicated patients were referred to the otolaryngology and surgery departments for surgical interference.
All cases with toxic symptoms had control of manifestations of toxicity by the internist, using propranolol (Inderal®, Zeneca), in various doses, ±Neo-Mercazole® (Roche), ±Aqueous Iodine oral solution.
Additionally, after deciding on surgery, the patients had their serum PTH levels measured one day preoperatively, intraoperatively, and 24 hours postoperatively.
For intraoperative rapid PTH assay, blood samples were taken from the patients ten minutes after complete resection of the thyroid gland and assessed for intact PTH using microparticle electrochemiluminescence immunoassay of the plasma (Roche Diagnostics, Germany) on Cobas e 411 analyser that employs a sandwich test principle in which a biotinylated monoclonal antibody reacts with the N- terminal fragment (1-37) and a monoclonal antibody labeled with a ruthenium complex reacts with the C-terminal fragment (38-84). The total duration of the assay was approximately 18 min (15 to 20 minutes). Using 50 µl of the sample, and the measuring range is 1.20–5000 pg/ml, with normal range referred to be 25–60 pg/ml. The clinical pathologist (laboratory department) that performed the tests was the same in all patients (co-author), taking into consideration to blind her from the surgical details of number of glands observed and identified, or reimplantation performed.
The thyroid tissue that was preserved in NaCl 0.9% (saline) solution till the result of the test was obtained. If the intraoperative PTH assay level was less than 25 pg/ml (minimum normal value), and/or if less than 3 parathyroid glands could be identified and secured intraoperatively, the specimen was examined under the microscope for possible inadvertent excised parathyroid gland tissue, and if it was found, was prepared and reimplanted in a sternomastoid muscle pocket, after tagging by a small silk suture knot.
Patients with intraoperative PTH assays <25 pg/ml were labeled as at-risk for early or permanent hypoparathyroidism. Ca level detection was done for them 24 hours after the operation to know the Ca state and compare them to PTH level.
Patients were regarded as having early hypoparathyroidism if standard PTH assay taken 24 hours after surgery was <25 pg/ml, and as having permanent hypoparathyroidism if serial PTH assays (usually bi-weekly assessed) were constantly <25 pg/ml till the end of the follow up period (12 weeks after surgery).
As a control group, all other cases undergoing thyroidectomy with the same inclusion criteria, but not done by the authors' subunits were reviewed through their files for permanent hypoparathyroidism for the same 3 month postoperative interval.
Data collected was tabulated and statistical analysis was done on a personal computer using MedCalc© version 11 (MedCalc Software bvba, Mariakerke, Belgium).
Normally distributed numerical data were presented as mean (SD), and nominal data as ratio or as number [%]. Correlation between normally distributed numerical data was tested using Pearson’s product-moment correlation.
Receiver-operator characteristic (ROC) curves were plotted to test the value of intraoperative rapid PTH assay to predict early or permanent hypoparathyroidism, and to test the value of standard PTH assay taken 24 hours after surgery for prediction of permanent hypoparathyroidism.
Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), positive likelihood ratio (LR+), and negative likelihood ratio (LR-) were calculated for both intraoperative fast PTH assay and standard PTH assay taken 24 hours after surgery as predictors for hypoparathyroidism.
The study included 52 patients recruited consecutively from the designated author’s sub-units at Ain Shams University Hospitals, all had total thyroidectomy; 32 cases were nontoxic multinodular goiter, 14 cases controlled toxic multinodular goiter, and 6 cases Graves’ disease with failed medical treatment.
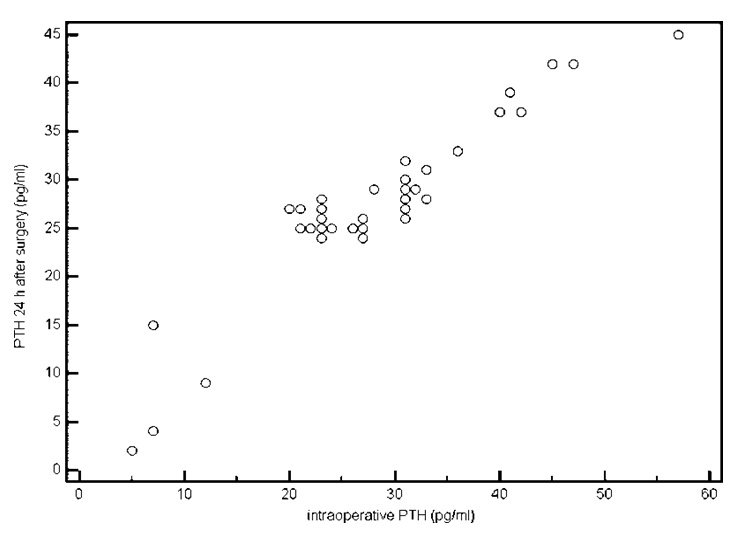
Figure 1
Scatter plot for correlation between intraoperative rapid PTH assay and standard PTH assay taken 24 hours after surgery. Correlation coefficient = 0.95 (P < 0.001).
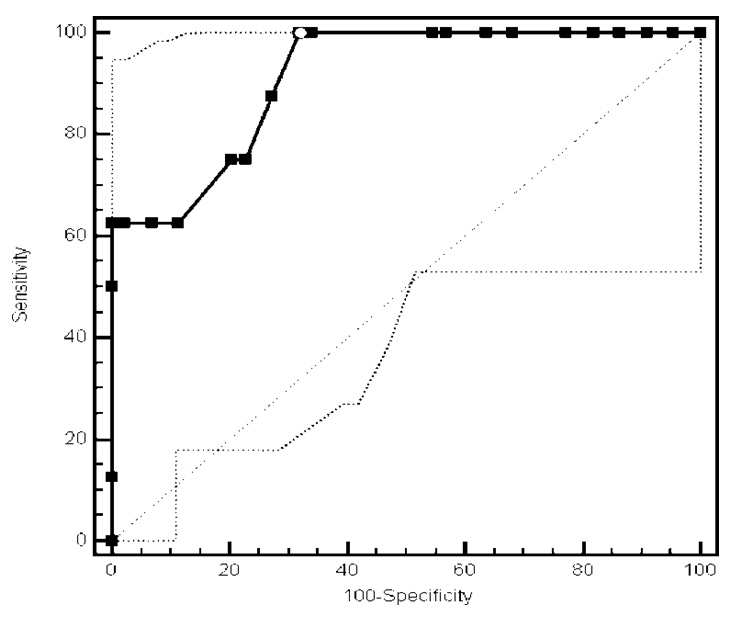
Figure 2
Receiver operating characteristic (ROC) curve for prediction of early hypoparathyroidism using intraoperative rapid PTH assay. Area under the curve (AUC) = 0.912 (SE = 0.05, 95% CI = 0.8 – 0.973, P < 0.0001). White dot along the curve represents optimal cutoff value (PTH < 27 pg/ml). This had sensitivity of 100% (95% CI = 63.1% – 100%), specificity of 68.2% (95% CI = 52.4% – 81.4%, LR+ of 3.1 (95% CI = 2.6 – 3.8), LR– of 0, PPV of 36.4% (95% CI = 17.2% – 59.3%), and NPV of 100.0% (95% CI = 88.1% – 100%).
All the patients included in the study performed total thyroidectomy, the recurrent laryngeal nerves were identified and preserved in all patients, and the superior laryngeal nerve was identified and preserved when apparent (41 patients). Fifty of the 52 patients had no form of vocal fold mobility affection postoperatively, and two patients had paresis of one of their vocal folds, which subsided completely after 3 weeks. Demographic, operative, and postoperative data are displayed in (table 1).
When handling the parathyroid glands, the 4 parathyroid glands could be identified in only 24 of the 52 patients, 3 parathyroid glands were identified in 8 patients, 2 parathyroid glands were identified in 18 patients, and in two patients no definite parathyroid glands could be identified (table 1). The vascular supply of identified glands was preserved as much as the approach allows.
Of the preoperative PTH estimates, all patients had a normal range of PTH, i.e., 25–60 pg/ml, with a mean of 45.6 pg/ml (SD ± 12.9). The intraoperative PTH levels and the 24h postoperative levels were monitored and revealed that all (100%) patients had variable degrees of reduction of their PTH levels when compared to their own preoperative levels. Value of intraoperative rapid PTH assay and standard PTH assay taken 24 hours after surgery for prediction of early and permanent hypoparathyroidism is shown in table 2.
Sixteen of the 52 patients (30.7%) had reduction of their intraoperative PTH levels below 25 pg/ml; 11 patients had ranges of PTH between 15–25 pg/ml, and 5 had levels below 15 pg/ml. There was a strong correlation between intraoperative rapid PTH assays and standard PTH assays taken 24 hours after surgery (correlation coefficient = 0.95, P <0.001) (fig. 1).
Of the 11 patients with levels of PTH between 15–25 pg/ml, 6 of them had 3 parathyroid glands identified, and 5 had all 4 parathyroid glands identified. Re-examination of the excised thyroid gland did not reveal any detectable parathyroid tissue. Of the 5 patients whose intraoperative PTH levels were below 15 pg/ml, two were the patients where no parathyroid glands could be identified, in the other 3 patients, only 2 glands were identified. In 4 out of these 5 patients when the excised thyroid gland was examined, some parathyroid tissue could be identified, and was reimplanted in a sternomastoid muscle pocket after preparation and tagging by a silk suture knot.
Further assessment of PTH levels was done in the 16 patients with intraoperative and 24h-postoperative PTH levels below 25 pg/ml, the 11 patients who had values between 15–24 pg/ml recovered to normal PTH levels within 4 weeks. The 5 patients with intraoperative PTH levels below 15 pg/ml failed to regain normal PTH levels up to 12 weeks postoperative, even in those patients where parathyroid tissue was reimplanted, although the 4 patients who had parathyroid tissue reimplanted intraoperatively restored some of their parathyroid function as indicated by relative rise of their PTH levels, but did not reach even the low normal levels, while the single patient whom had no glands identified at all and no tissue could be identified for reimplantation had almost no rise in his postoperative PTH levels.
Statistical analysis by the receiver operating characteristic (ROC curve) for prediction of early hypoparathyroidism using intraoperative rapid PTH assay is shown in figure 2. The curve had an area under the curve (AUC) of 0.912 (SE = 0.05, 95% CI = 0.8–0.973, P <0.0001). The optimal cutoff value was a PTH level <27 pg/ml. This had sensitivity of 100% (95% CI = 63.1–100%), specificity of 68.2% (95% CI = 52.4–81.4%, LR+ of 3.1 (95% CI = 2.6–3.8), LR– of 0, PPV of 36.4% (95% CI = 17.2–59.3%), and NPV of 100.0% (95% CI = 88.1–100%).
By using the receiver operating characteristic (ROC) curves for prediction of permanent hypoparathyroidism via comparing the intraoperative rapid PTH assay with the standard PTH assay taken 24 hours after surgery, we found that both curves had an AUC of 1.0 (SE = 0, 95% CI = 0.932 – 1.0, P <0.001). The two curves were identical (P = 1.0). The optimal cutoff value was a PTH level <12 pg/ml on the intraoperative PTH curve, or <15 pg/ml on the postoperative PTH curve. Both cutoff values had a sensitivity of 100% (95% CI = 47.8–100%), a specificity of 100% (95% CI = 92.5–100%), LR– of 0, PPV of 100% (95% CI = 47.8–100%), and NPV of 100% (95% CI = 92.5–100%), whether or not parathyroid tissue was reimplanted (fig. 3).
None of our patients complained of symptoms or presented clinical signs of hypocalcaemia, as we depended on the Intra and 24 hour postoperative PTH level, and we prescribed calcium carbonate 2–3 g daily) and vitamin D analogue (Rocaltrol 0.25–0.5 μg daily) (Roche Laboratories, Nutley, NJ) for 6 out of the 11 patients (who had PTH level between 15–25 pg/ml) for preventing hypocalcaemia, and discontinued it when the level of PTH rose to reach 27 pg/ml ( within 2–4 weeks). All 5 patients with intraoperative PTH level below 15 pg/ml had to maintain the treatment as a regular supplement therapy.
| Table 1: Demographic, operative, and postoperative data. | |
| Total number of patients | 52 patients |
| Age (yr) | 35.8 (9.0) |
| Gender (female/male) | 45/7 |
| Indication for surgery | |
| Simple multinodular goiter | 32 [61.5%] |
| Toxic multinodular goiter | 14 [26.9%] |
| Graves disease | 6 [11.5%] |
| Operative time (min) | 87.5 (32.3) |
| Number of parathyroid glands identified during dissection | |
| 4 | 24 [46.2%] |
| 3 | 8 [15.4%] |
| 2 | 18 [34.6%] |
| 1 | |
| 0 | 2 [3.8%] |
| Intraoperative PTH level by fast assay (pg/ml) | 30.3 (11.6) |
| PTH level 24 hours after surgery by standard assay (pg/ml) | 28.9 (9.5) |
| Number of patients labeled as at-risk of hypoparathyroidism (intraoperative fast PTH assay <25 pg/ml) | 15 [28.8%] |
| Number of patients labeled as having early hypoparathyroidism (standard PTH assay <25 pg/ml at 24 hours after surgery) | 8 [15.4%] |
| Number of patients labeled as having permanent hypoparathyroidism (standard PTH assays constantly <25 pg/ml) | 5 [9.6%] |
| Data are mean (SD), ratio, or number [%]. | |
| Table 2: Value of intraoperative rapid PTH assay and standard PTH assay taken 24 hours after surgery, for prediction of early and permanent hypoparathyroidism. | |||
| Intraoperative fast PTH assay | Standard PTH assay taken 24 hr after surgery | ||
| Early hypo-parathyroidism | Permanent hypo-parathyroidism | Permanent hypo-parathyroidism | |
| Sensitivity | 100.0% (95% CI = 63.1% – 100%) | 100.0% (95% CI = 47.8% – 100.0%) | 100.0% (95% CI = 47.8% – 100.0%) |
| Specificity | 84.1% (95% CI = 70.0% – 93.4%) | 78.7% (95% CI = 64.3% – 89.3%) | 93.6% (95% CI = 82.5% to 98.7%) |
| LR+ | 6.3 (95% CI = 3.2 – 12.4) | 4.7 (95% CI = 2.7 – 8.2) | 15.7 (95% CI = 5.2 – 46.8) |
| LR– | 0.00 | 0.00 | 0.00 |
| Disease prevalence | 15.4% (95% CI = 6.9% – 28.1%) | 9.6% (95% CI = 3.2% – 21.0%) | 9.6% (95% CI = 3.2% – 21.0%) |
| PPV | 53.3% (95% CI = 26.6% – 78.7%) | 33.3% (95% CI = 11.8% – 61.6%) | 62.5% (95% CI = 24.5% –91.5%) |
| NPV | 100.00% (95% CI = 90.1% – 100.0%) | 100.0% (95% CI = 90.5% – 100.0%) | 100.0% (95% CI = 92.0% – 100.0%) |
| 95% CI = 95% confidence interval, LR– = negative likelihood ratio, LR+ = positive likelihood ratio, NPV = negative predictive value, PPV = positive predictive value. | |||
Preservation of the parathyroid gland during thyroidectomy for non-neoplastic thyroid disease is one of the indicators of successful surgery. Introduction of preservation-assisting techniques, as the use of microscopic identification and dissection, and the use of the harmonic scalpel if available, with good surgical expertise, has resulted in a high preservation rate for the parathyroid glands and other vital structures as the laryngeal nerves. Despite this advancement in thyroid and parathyroid surgery, still postoperative hypocalcaemia as a result of hypoparathyroidism, is a recorded complication in thyroid surgery, reaching 10% of all cases undergoing thyroid surgery [4]. However, the phenomenon of calcium decline within 24 hours is not a response specific to thyroid surgery. Postoperative evolution of calcium and other electrolytes after operations of the same magnitude and duration performed outside the cervical area, such as herniorrhaphy, strictly parallels that of thyroidectomised patients [6]. In contrast, the PTH level did not fall after such unrelated operations [20].
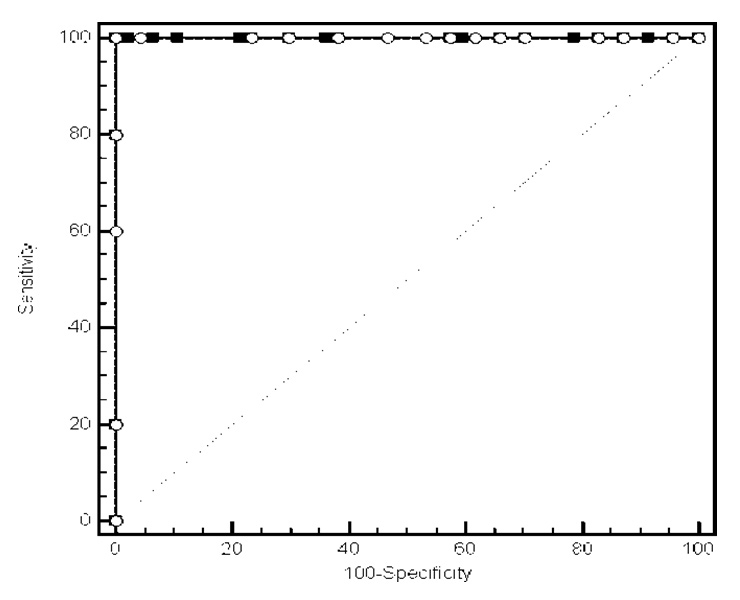
Figure 3
Receiver operating characteristic (ROC) curves for prediction of permanent hypoparathyroidism using intraoperative rapid PTH assay or standard PTH assay taken 24 hours after surgery. Both curves had an area under the curve (AUC) of 1.0 (SE = 0, 95% CI = 0.932 – 1.0, P < 0.001). The two curves were identical (P = 1.0). The optimal cutoff value was a PTH level < 12 pg/ml on the intraoperative PTH curve or < 15 pg/ml on the postoperative PTH curve. Both cutoff values had a sensitivity of 100% (95% CI = 47.8% – 100%), a specificity of 100% (95% CI = 92.5% – 100%), LR– of 0, PPV of 100% (95% CI = 47.8% – 100%), and NPV of 100% (95% CI = 92.5% – 100%).
Because the half-life of PTH in blood is only minutes [13], intraoperative PTH assay was used in various cases of hyperparathyroidism to prove complete surgical ablation of the parathyroid glands [14, 15]. Later the same test was used to predict postoperative hypocalcaemia in thyroid and parathyroid surgery [21–23]. Other studies demonstrated that below normal intraoperative PTH levels would predict hypoparathyroidism with resultant hypocalcaemia [18, 22, 24].
Our results showed that in all the cases performing total thyroidectomy, a certain degree of reduction in PTH levels occurs, which confirmed with 24h postoperative PTH assessment revealing similar and even further reduction in their PTH levels, as there was strong correlation between intraoperative rapid PTH assays and standard PTH assays taken 24 hours after surgery (correlation coefficient = 0.95, P <0.001), agreeing with the findings of Lemaire et al. [25]. It is suggested that this reduction in the hormonal levels occurs due to manipulation of the gland, with resultant variable degrees of vascular insult to the parathyroid glands, or at least the superior pair. This reduction may be even to levels below the normal acceptable range, but not enough to produce hypocalcaemia, as we found this in 5 patients with minimal reduction below 25 pg/ml, but without symptoms, signs or laboratory hypocalcaemia, agreeing with the findings of Higgins et al. [22].
Also, we found that (ROC) curve for prediction of early hypoparathyroidism using intraoperative rapid PTH assay was statistically highly significant (P <0.0001), and the optimal cutoff value for predicting early hypoparathyroidism was a PTH level <27 pg/ml, this had sensitivity of 100% and specificity of 68.2%. But (ROC) curves for prediction of permanent hypoparathyroidism using intraoperative rapid PTH assay or standard PTH assay taken 24 hours after surgery {as both curves were identical, with no statistical significant difference (P = 1.0)} were statistically significant (P <0.001), and the optimal cutoff value was a PTH level <12 pg/ml on the intraoperative PTH curve or <15 pg/ml on the postoperative PTH curve. Both cutoff values had a sensitivity of 100% and a specificity of 100%
Patients with levels below the minimum normal levels but not down to 15 pg/ml usually recover completely, as occurred in 11 patients in our study within 4 weeks postoperatively spontaneously in 5 patients, and aided with Ca carbonate replacement therapy for 4 weeks in 6 patients, and we successfully discontinued Ca supplement once the level rose to 25 pg/ml, without further management, also agreeing with the findings of Richards et al. [21], Higgins et al. [22], and Lo et al. [18]. As in our study, the rapid PTH assay during thyroidectomy could identify patients at risk of developing clinically significant hypoparathyroidism and we depended on the intra and postoperative PTH level, when it was less than 15 pg/ml, we suspected hypocalcaemia and so we prescribed immediately postoperative calcium carbonate 2–3 g daily and vitamin D analogue (in 9.6% of our patients), hence not one of our patients had symptoms or presented clinical signs of hypocalcaemia.
We also demonstrated that intraoperative PTH levels may predict direct injury to the parathyroid glands, when reaching levels below 60% of the lowest normal value, this agrees with the results of Warren et al. [26], who found that intraoperative PTH levels below 15 pg/ml are associated with such findings. It also agrees with the results of Lam and Kerr [24], but with lower estimates, stating that the cut-off level was 8 pg/ml, and those of Richards et al. [21], with cut-off levels of 10 pg/ml.
Intraoperative PTH assay was used also to lead to safe and early postoperative hospital discharge [27]. As both the rapid PTH assay and consecutive early calcium measurements are accurate in predicting postoperative normocalcemia. However, the rapid PTH assay gives reliable results within about 15–20 minutes after sampling, but serum calcium monitoring requires at least 24 hours, as well as an additional 4-hour turnover time, before the results are available. As in our study, 36 patients (70%) were discharged early without the need for serum calcium monitoring when the intra operative and postoperative values were above the normal values, and another 5 (10% of our patients) delay till ensuring the normocalcemic state, then they are discharged the next day, only 11 patients needed reassessment (20%)
Although auto transplantation of parathyroid tissue that was inadvertently removed restored some parathyroid function, but in our results, although the number of patients with such condition in our series is small, it was not enough to regain normal levels of PTH, at least up to 12 weeks postoperative, raising the question; is it worthwhile in terms of time and fear of possible future parathyroid problems to actually attempt such auto transimplantation, so long as the patient will be on supplementation therapy any way.
We also found that there is no significant extension of the operation time more than expected for total thyroidectomy, as the rapid PTH assay is available within about 15 minutes, also this procedure is cost effective as we saved the routine postoperative serum Ca level assessment, routine Ca supplement for all patients postoperatively (even if for few days), and discharge 80% of our patients early without fear of hypocalcaemia, in addition predicting which patients might develop permanent hypocalcaemia and treat them early.
But there were some limitations in our studying to be reconsidered in further studies, among them were the small sample size, inability for randomisation of our study design, and the variable values reported for the cut off value of PTH causing hypocalcaemia symptoms and need intervention. Another relative limitation is the short follow up period (3 months) in assessing the long term predictability of the test, although we have followed up patients for up to 18 months without apparent change in the 3 months postoperative results, but this was not in the original design and was not done regularly nor systematically for all patients, thus results are not documented in a standard mode.
Intraoperative PTH assay can allow intraoperative monitoring of parathyroid function and predict the postoperative outcome during operation, also identify patients at risk of developing postoperative hypoparathyroidism, and guide the surgeon to re-exam the removed specimen of inadvertently removed parathyroid tissue with possible auto transplantation, or more practically lead to early replacement therapy to prevent hypocalcaemia, and lead to the safe and early hospital discharge, some relative limitations in our study to be reconsidered in further studies, are small sample size, inability for randomisation, and the variable values reported for the cut off value of PTH that cause hypocalcaemia symptoms and need intervention. Extension of the follow up period for determination for predictability of the results of the test should also be considered in further studies.
1 Farling PA. Thyroid disease. Br J Anaesth. 2000;85:15–28.
2 Ready AR, Barnes AD. Complications of thyroidectomy. Br J Surg. 1994;81:1555–6. [PubMed]
3 Brennan J, Moore EJ, Shuler KJ. Prospective analysis of the efficacy of continuous intraoperative nerve monitoring during thyroidectomy, parathyroidectomy, and parotidectomy. Otolaryngol Head Neck Surg. 2001;124:537–43. [PubMed]
4 Lin DT, Patel SG, Shaha AR, Singh B, Shah JP. Incidence of inadvertent parathyroid removal during thyroidectomy Incidence of inadvertent parathyroid removal during thyroidectomy. Laryngoscope. 2002;112(4):608–11.
5 Zedenius J, Wadstrom C, Delbridge L. Routine autotransplantation of at least one parathyroid gland during total thyroidectomy may reduce permanent hypoparathyroidism to zero. Aust NZ J Surg. 1999;69:794–9.
6 Kuhel WI, Carew JF. Parathyroid biopsy to facilitate the preservation of functional parathyroid tissue during thyroidectomy. Head Neck. 1999;21:442–6. [PubMed]
7 Katz AD. Parathyroid autotransplantation in patients with parathyroid disease and total thyroidectomy. Am J Surg. 1981;142:490–3. [PubMed]
8 McHenry CR, Speroff T, Wentworth D, et al. Risk factors for postthyroidectomy hypocalcemia. Surgery. 1994;116:641–8. [PubMed]
9 Pattou F, Combemale F, Fabre S, et al. Hypocalcemia following thyroid surgery: Incidence and prediction of outcome. World J Surg. 1998;22:718–24. [PubMed]
10 Marohn MR, LaCivita KA. Evaluation of total/near-total thyroidectomy in a short stay hospitalisation: safe and cost-effective. Surgery. 1995;118:943–7. [PubMed]
11 Adams J, Andersen P, Everts E, et al. Early postoperative calcium levels as predictor of hypocalcemia. Laryngoscope. 1998;108:1829–31. [PubMed]
12 McHenry CR, Pollard A, Walfish PG, et al. Intraoperative parathormone level measurement in the management of hyperparathyroidism. Surgery. 1990;108:801–8. [PubMed]
13 Wallach J (ed). Serum parathyroid hormone. In “Interpretation of diagnostic tests”, 8th ed. 2007. Lippincott Williams & Wilkins, Philadelphia, PA Chapter 13, Endocrine diseases, pp. 684–6.
14 Stratmann SL, Kuhn JA, Bell MS, et al. Comparison of quick parathyroid assay for uniglandular and multiglandular parathyroid disease. Am J Surg. 2002;184(6).
15 Mandell DL, Genden EM, Mechanick JI, et al. The influence of intraoperative parathyroid hormone monitoring on the surgical management of hyperparathyroidism. Arch Otolaryngol Head Neck Surg. 2001;127(7):821–7.
16 Irvin GL III, Derio GT III. A new, practical intraoperative hormone assay. Am J Surg. 1994;168:466–8. [PubMed]
17 Gardner SC, Leight GS Jr. Initial experience with intraoperative PTH determinations in the surgical management of 100 consecutive cases of primary hyperparathyroidism. Surgery. 1999;126:1132–8. [PubMed]
18 Lo CY, Luk JM, Tam SC. Applicability of intraoperative parathyroid hormone assay during thyroidectomy. Ann Surg. 2002;236(5):564–9.
19 Lo CY, Lam KY. Routine parathyroid autotransplantation during thyroidectomy. Surgery. 2001;129:318–23. [PubMed]
20 Demeester-Mirkine N, Hooghe L, Van Geertruyden J, et al. Hypocalcemia after thyroidectomy. Arch Surg. 1992;127:854–8. [PubMed].
21 Richards ML, Bingener-Casey J, Pierce D, et al. Intraoperative parathyroid hormone assay: an accurate predictor of symptomatic hypocalcemia following thyroidectomy. Arch Surg. 2003;138(6):632–5.
22 Higgins KM, Mandell DL, Govindaraj S, et al. The role of intraoperative rapid parathyroid hormone monitoring for predicting thyroidectomy-related hypocalcemia. Arch Otolaryngol Head Neck Surg. 2004;130(1):63–7.
23 Díez Alonso M, Sánchez López JD, Sánchez-Seco Peña MI, Ratia Jiménez T, Arribas Gómez I, Rodríguez Pascual A, et al. Serum PTH levels as a predictive factor of hypocalcaemia after total thyroidectomy. Cir Esp. 2009;85(2):96–102.
24 Lam A, Kerr PD. Parathyroid hormone: an early predictor of postthyroidectomy hypocalcemia. Laryngoscope. 2003;113(12):2196–200.
25 Lemaire FX, Debruyne F, Delaere P, Vander Poorten V. Parathyroid function in the early postoperative period after thyroidectomy. Acta Otorhinolaryngol Belg. 2001;55(2):187–98.
26 Warren FM, Andersen PE, Wax MK, Cohen JI. Intraoperative parathyroid hormone levels in thyroid and parathyroid surgery. Laryngoscope. 2002;112(10):1866–70.
27 Houlton JJ, Pechter W, Steward DL. PACU PTH facilitates safe outpatient total thyroidectomy. Otolaryngol Head Neck Surg. 2011;144(1):43–7.
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article was reported.