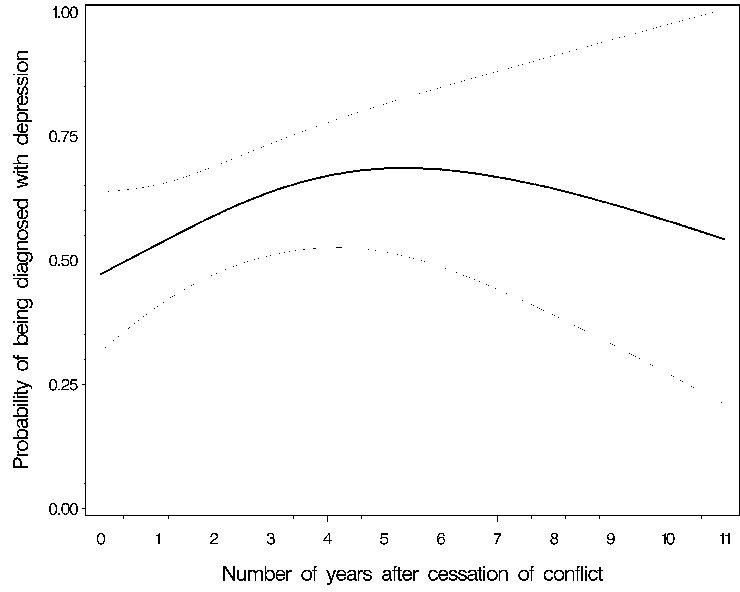
Figure 1
Probability of being diagnosed with depression in relation to the number of years after cessation of conflict (with 95% confidence interval).
DOI: https://doi.org/10.4414/smw.2011.13252
During the past 60 years, there have been more than 200 wars worldwide [1], which have had, and still have, a profound impact on the health of people that is over and above the impact of the injuries that are directly attributable to the conflict. Worldwide there are approximately 13 million refugees fleeing from violent conflicts, famine or human rights violations [2–4]. Although most refugees remain near their home countries in Asia or Africa, some manage to travel to Europe and seek asylum there [5]. Asylum seekers are persons whose application for asylum or refugee status is pending in the administrative or legal system of a sanctuary state [6, 7]. According to the United Nations Refugee Agency, 134,900 individuals applied for asylum in Europe during the first half of 2006 [8].
Even in extensive calculations of the costs of war, the expenses that asylum seekers or refugees generate in the receiving countries are not fully taken into account [9]. These costs, though, are important in the context of increasing global interconnectedness and mobility, having both political and health policy implications [10–12]. A major political issue is the burden of asylum seekers on the health care systems of the countries to which they apply for sanctuary [5, 13–16]. As many of these asylum seekers come from countries where there is violent conflict, their disease profile may be different from that of the native population of the sanctuary country. The reason for this difference is not only the direct effects of the violence itself, but it may also be as a result of the absence of a well-functioning (health care) infrastructure in the country of origin.
There have been increasing numbers of epidemiological studies of war-affected populations, mostly among veterans [1], but also among refugee populations such as the Kosovars [17], Bosnians [18], Tamils [19], Rwandans [20] and Senegalese [21], to mention but a few. Several studies have identified severe consequences of living in war-torn countries, mainly in the form of mental health problems, such as depression or post-traumatic stress disorder (PTSD) [2, 22]. Increases of injuries and infectious diseases have also been reported [22–24]. Less is known, however, about the consequences of violent conflicts on general health care costs in the receiving countries and on the prevalence of other diseases that are not mental disorders. Therefore, the goal of this study was to compare disease profiles and resulting health care costs of asylum seekers from countries where there is violent conflict to asylum seekers from countries where there is no violent conflict, and to examine whether disease profiles are related to costs.
This cross-sectional study collected data from one Swiss canton that organised asylum seekers' health care using a Health maintenance organisation (HMO) model. People seeking protection in Switzerland can file an asylum application at a border-crossing reception centre of the Federal Office for Migration. There they undergo a first brief round of questioning about their reasons for seeking asylum and have a health check. This comprises of immunisations and screening for infectious diseases including hepatitis B and tuberculosis. The Swiss border-crossing health check is comparable to the screening checks provided for asylum seekers in most other European countries [5]. Asylum seekers are then allocated to one canton. Primary health care for asylum seekers is provided by the public health system in each canton.
This study used a representative sample of people applying for asylum in Switzerland. The sample is representative of asylum seekers in Switzerland because of the country’s policy of mandatory health care insurance for all persons living on Swiss territory [25]. After refugees arrive in Switzerland, they must apply for asylum at one of five reception centres, from which they are randomly assigned to one of the 26 Swiss cantons according to a pre-established distribution quota. Asylum seekers are provided with health care insurance by the Federal Office of Migration for as long as they have asylum seeker status [26]. The insurance includes free access to health care and coverage of all health care costs (If the person is accepted as a refugee, he or she is moved to another insurance programme.)
The canton that provided the data, Basel, was an urban canton required by the preset federal quota system to absorb 2.3% of Swiss asylum seekers. The canton assigned its asylum seekers alternately to two participating Health Maintenance Organisations (HMOs) [27], one of which was founded explicitly to provide health care for this population and was integrated within the Department of Ambulatory Internal Medicine of the University Hospital. This HMO was known as the A-Care (“A” = “asylum”) HMO and was the source of the patients included in this study (i.e., patients newly enrolled during the study period).
After receiving clearance from the ethical committee EKBB (Ethik-Kommission beider Basel), data for this study were routinely collected by the hospital administration and merged with additional demographic data obtained from the Federal Office for Migration. Data on costs were collected by the accounting office of the hospital administration and reflected consultations, diagnostic exams (lab, x-ray, electrocardiograms, magnetic resonance imaging, etc.), medical interventions, patient stays at the clinic, and medication. The data collection period was from the beginning of January 2000 through to the end of December 2003, after which the A-Care programme was terminated.
The “costs” variable reflected the total health care costs that were generated during the period in which the patient was covered by insurance. Cost data were expressed as Swiss Francs and then converted to Euros (EUR) by using the exchange rate in effect on 31 December 2003 (1 Swiss Franc = 0.6415 Euro [28]). Other variables for this study included gender, age, the length of time during which the asylum seeker was insured, the number of visits to the HMO, the medical diagnoses, and the status of the patient’s asylum application (“asylum decision” or asylum status). Decisions regarding asylum status are assigned to one of three categories by the Federal Office of Migration: (1) “positive” (a person is accepted and obtains refugee status), (2) “pending,” or (3) “negative” (the asylum application is rejected).
Diagnoses: The physicians involved in the A-Care recorded the respective patient diagnoses using the International Classification of Disease, 10th revision (ICD). Although there was no obligation to provide a diagnosis, they documented up to ten main diagnoses and entered them in the hospital’s electronic diagnosis database. Medical diagnosis categories included the eight most frequent diagnostic groups (“blocks”) of the ICD system: diseases of the musculoskeletal system, diseases of the respiratory system, mental disorders, skin diseases, injuries, infectious and parasitic diseases, pregnancy-childbirth-puerperium, and cardiovascular diseases [29].
Patients were divided into two groups: those from countries with violent conflict at the time they were included in the A-Care programme, and those from countries without violent conflict. We based our assignments of the countries to either violent conflict or no violent conflict based on the Uppsala Conflict Data Programme (by the Department of Peace and Conflict research, Uppsala University [30]).
The countries of origin where there was a violent conflict during the timeframe of the study were Afghanistan, Burundi, the Democratic Republic of Congo, Ivory Coast, Liberia, Niger, Somalia, Sri Lanka, Ethiopia (from June 2000 on), Iraq (from March 2003 on), Sudan, Angola (until March 2003), Sierra Leone (until 2002) and Algeria (until 2002). For countries of origin in which violent conflicts had ended prior to the beginning of the study, we recorded the year that conflict ended (dating back to 1990): Azerbaijan (1994), Ecuador (1995), Guinea-Bissau (1999), Mauritania (1991), Bosnia-Herzegovina (1995), and Serbia/Montenegro/Kosovo (1999).
Data analysis included calculating frequencies for categorical variables and medians/interquartile ranges for continuous variables. In order to use the highly skewed “costs” variable, which was not transformable to normal because of a subsample of 185 patients (19%) who did not generate any costs, as an outcome in a multiple regression analysis, we categorised this variable into pentiles to fit a proportional odds model. A proportional odds model is a logistic regression analysis that estimates an odds ratio across the possible cut-offs of an ordinal outcome [31]. We also used a binary logistic regression analysis and a non-linear regression technique called generalised additive modelling for post-hoc analyses in which we regressed the amount number of years previously which a conflicthad ended onto the probability of depression and post-traumatic stress disorder, respectively [32]. All analyses were performed by using SAS® version 9.1.
Table 1 shows the characteristics of the two groups of asylum seekers – those from countries with areas of violent conflict and those from countries with no violent conflict. The groups had comparable age (median 22 years) and gender (≈60% male) distributions. Simple comparisons showed that health care use was higher for patients from countries with violent conflict. The medians of their total health care costs (974 vs. 449; p = 0.0002), their number of visits to the health care system (7 vs. 3; p <0.0001), and the length of time during which they were insured (395 vs. 212; p = 0.0003) were all about twice as high as compared to patients from countries with no conflicts. Also, patients from countries with violent conflict showed different disease patterns, with higher frequencies of respiratory diseases (23% vs. 13%; p = 0.001), skin diseases (13% vs. 8%; p = 0.02) and injuries (13% vs. 8%; p = 0.02). Also, women from these countries had more pregnancies (9% vs. 4%; p = 0.01). As for co-morbidities, there were higher frequencies of blood diseases (5% vs. 2%, p = 0.009) and of endocrine diseases (11% vs. 7%; p = 0.002). However, and contrary to our expectations, the prevalence of mental disorders, whether depression or PTSD, was not found to be higher in this group.
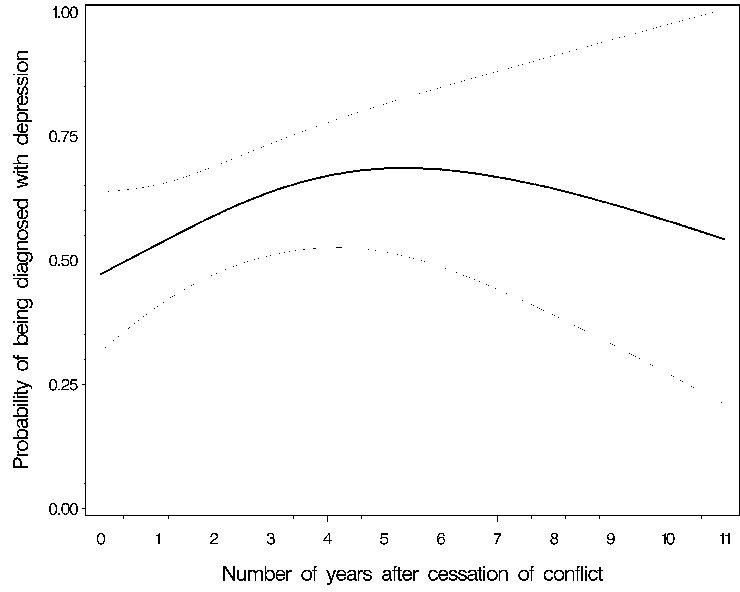
Figure 1
Probability of being diagnosed with depression in relation to the number of years after cessation of conflict (with 95% confidence interval).
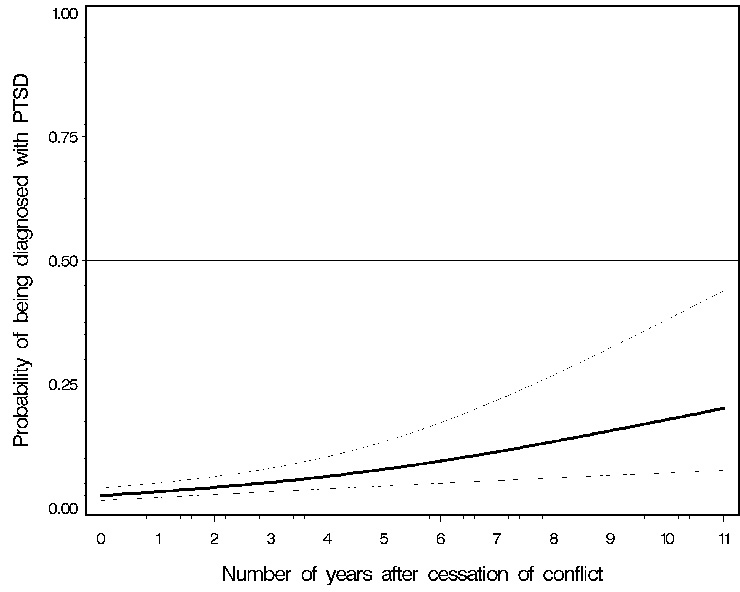
Figure 2
Probability of being diagnosed with post-traumatic stress disorder (PTSD) in relation to the number of years after cessation of conflict (with 95% confidence interval).
Table 2 presents the median health care costs for asylum seekers by gender and ICD diagnosis. It consistently shows that the costs for patients from countries with conflicts were higher when there was no diagnosis of an ICD disorder. When an ICD disorder was diagnosed, there was no difference in health care costs for patients from countries with conflict and patients from countries with no conflict. This pattern was not the result of other diagnoses. It can therefore be hypothesised that even though patients from countries with violent conflicts generate more costs than patients from other countries, these costs must be explained by factors other than a higher prevalence of a given diagnosis.
We tested this hypothesis by conducting a three-step proportional odds model (table 3). Model 1 is the base model and only controls for age and gender. It showed that a person from a country with a violent conflict had 94% higher odds for generating more costs (OR = 1.94; 95% CI: 1.40–2.69). This finding remained relatively unaltered in model 2, which comprised of model 1 variables plus the ICD diagnoses (OR 1.64; 95% CI: 1.16–2.31).
However, model 3, which comprised of model 2 variables plus three more variables from table 1, fully explained the cost differences between the two sub-samples (OR = 0.97; 95% CI: 0.64–1.46). The variables chosen for the models were selected on the basis of their obvious relationship to costs (”number of visits,“ ”time spent in A-Care HMO”) or on the basis of an expected relationship that was due to the nature of this specific HMO (”time spent in A-Care HMO”, “asylum decision”). The variables were interrelated: patients who eventually received refugee status (either due to humanitarian reasons or due to health reasons, such as a need for chronic dialysis) spent a longer period of time in the A-Care HMO, which in turn partly explained their higher number of visits to the HMO.
Of the three extra variables in model 3, each separately had the power to explain the fact that costs seemed to differ between asylum seekers from countries with conflict and those from countries with no conflict. However, the variable “asylum decision” was the highest predictor of costs among them. Individuals from conflict countries were less likely to be rejected by the Federal Office of Migration and were therefore more likely to obtain refugee status and to leave the A-care programme.
In model three, mental disorders were the strongest predictor of costs among the different diseases (OR 1.69, CI 1.06–2.68, cf. table 3). Why then are the mental disorders so important in increasing costs and at the same time why aren’t they more prevalent among people from countries with conflict (table 1)? To follow up on these findings, we carried out a post-hoc analysis. One possible reason why mental disorders were not highly prevalent in patients from countries in conflict may be that these disorders show up only some time after a person has experienced a traumatic event. Therefore, we looked at the group of people who did not come from countries classified as countries with violent conflict to see whether they had experienced violent conflict earlier in the past . If a country had experienced such conflict, we calculated the number of years that had elapsed since that conflict had ended. We then checked whether there was any evidence of a relationship between this variable and the frequency of the two most common mental disorder diagnoses (i.e. depression and post-traumatic stress disorder (PTSD)). This analysis was done on a subsample of patients where there was a violent conflict in the previous decade (n = 647).
While we found no evidence for a relationship between a diagnosis of depression and time since the end of the conflict (see fig. 1, and table 4), we did indeed detect an increase in PTSD diagnoses the longer ago that a violent conflict had ended (see fig. 2, and table 5). We concluded: the higher the number of years after the conflict, the higher the probability of being diagnosed with PTSD (p = 0.003).
| Table 1: Study sample characteristics (n = 969). | ||||
| Category | Variable | No violent conflict (n = 835) | Violent conflict (n = 134) | p-value (*) |
| Demographics | Mean age (SD) | 22 (14) | 22 (15) | 0.72 |
| Number of men | n = 518 (62%) | n = 79 (60%) | 0.50 | |
| Costs | Median cost in Euros (IQR) | 449 (53–1970) | 974 (301–3437) | 0.0002 |
| HMO use | Median duration of A-Care insurance in days (IQR) | 212 (120–515) | 395 (167–853) | 0.0003 |
| Median number of visits (IQR) | 3 (0–12) | 7 (2–21) | <.0001 | |
| Median number of visits per year (IQR) | 4.7 (0–17.6) | 8.2 (1.8–17.9) | 0.02 | |
| Asylum status | Status: Accepted as a refugee Decision pending Rejected | n = 84 (10%) n = 286 (34%) n = 465 (56%) | n = 37 (27%) n = 80 (60%) n = 19 (14%) | <.0001 (°) |
| Origin | Europe (sub-)Saharan African Far east Middle east and Maghreb Other | 587 (100%) 50 (45%) 47 (43%) 134 (92%) 17 (100%) | 0 (0%) 61 (55%) 62 (57%) 11 (7.6%) 0 (0%) | <.0001 |
| Main diagnoses | Prevalence of diseases of the musculoskeletal system (M block) | n = 114 (14%) | n = 27 (20%) | 0.06 |
| Prevalence of diseases of the respiratory system (J block) | n = 105 (13%) | n = 32 (24%) | 0.001 | |
| Prevalence of mental disorders (F block): | n = 118 (14%) | n = 15 (11%) | 0.41 | |
| Prevalence of depression | n = 59 (7%) | n = 5 (4%) | 0.19 | |
| Prevalence of post-traumatic stress disorder | n = 32 (4%) | n = 4 (3%) | 0.80 | |
| Prevalence of skin diseases (L block) | n = 66 (8%) | n = 19 (14%) | 0.02 | |
| Prevalence of injuries (S/T block) | n = 64 (8%) | n = 19 (14%) | 0.02 | |
| Prevalence of infectious and parasitic diseases (A-B block) | n = 49 (6%) | n = 13 (10%) | 0.12 | |
| Prevalence of cardio-vascular diagnoses (I block) | n = 34 (4%) | n = 9 (7%) | 0.17 | |
| Prevalence of diagnoses related to pregnancy, childbirth, puerperium (O block) | n = 33 (4%) | n = 12 (9%) | 0.01 | |
| Co-morbidities | Malignant neoplasms (C-block) | n = 8 (1%) | n = 1 (1%) | 0.81 |
| Diseases of blood, blood-forming organs, immune mechanism (D50-D89) | n = 14 (2%) | n = 7 (5%) | 0.009 | |
| Endocrine, nutritional, and metabolic disease (E-block) | n = 39 (7%) | n = 15 (11%) | 0.002 | |
| Diseases of the nervous system (G-block) | n = 26 (3%) | n = 1 (1%) | 0.12 | |
| Diseases of the eye and ear (H-block) | n = 45 (5%) | n = 11 (8%) | 0.19 | |
| Diseases of the digestive system (K-block) | n = 94 (11%) | n = 16 (12%) | 0.82 | |
| Diseases of the genitourinary system (N-block) | n = 35 (4%) | n = 10 (7%) | 0.09 | |
| Symptoms, signs, and abnormal clinical and laboratory findings, not classified elsewhere (R-block) | n = 78 (9%) | n = 16 (12%) | 0.35 | |
| External causes of morbidity and mortality (V-Y-block) | n = 3 (<1%) | n = 0 (0%) | 0.49 | |
| Factors influencing health status and contact with health services (Z-block) | n = 109 (13%) | n = 23 (17%) | 0.20 | |
| IQR = Interquartile range (*) Chi²/ Fisher's exact test for nominal variables, Mann-Whitney U for continuous variables. (°) The group of people whose requests for asylum were denied contained the lowest proportion of applicants from countries where there were areas of violent conflict (rank-ordered ANOVA with Tukey test p <0.0001). | ||||
| Table 2: Details of costs (in Euros) per gender and ICD diagnosis. | ||||||
| Variable | Value | No violent conflict | Violent conflict | p-value | ||
| n | Median costs (IQR) | n | Median costs (IQR) | (*) | ||
| Gender | Male | 518 | 313 (0–1227) | 79 | 812 (240–2173) | <.0001 |
| Female | 317 | 959 (139–3415) | 55 | 1620 (399–4019) | 0.21 | |
| Diseases of the musculoskeletal system | No diagnosis | 721 | 351 (22–1516) | 107 | 791 (205–2188) | 0.0005 |
| Diagnosis | 114 | 2641 (778–6331) | 27 | 3437 (1251–4721) | 0.54 | |
| Diseases of the respiratory system | No diagnosis | 730 | 356 (22–1686) | 102 | 893 (223–3914) | 0.0002 |
| Diagnosis | 105 | 1732 (533–5835) | 32 | 1337 (689–3114) | 0.36 | |
| Mental disorders | No diagnosis | 717 | 351 (15–1479) | 119 | 902 (254–3202) | <.0001 |
| Diagnosis | 118 | 3287 (627–6769) | 15 | 2188 (683–11143) | 0.84 | |
| Skin diseases | No diagnosis | 769 | 411 (39–1788) | 115 | 921 (263–3420) | <.0001 |
| Diagnosis | 66 | 1960 (644–6612) | 19 | 1306 (427–3914) | 0.45 | |
| Injuries | No diagnosis | 771 | 385 (38–1716) | 115 | 892 (240–3147) | 0.0001 |
| Diagnosis | 64 | 2502 (1160–6473) | 19 | 1358 (716–9539) | 0.61 | |
| Infectious and parasitic diseases | No diagnosis | 786 | 412 (43–1878) | 121 | 892 (263–3147) | 0.0002 |
| Diagnosis | 49 | 1438 (609–4050) | 13 | 3116 (1307–4721) | 0.35 | |
| Diagnoses related to pregnancy, birth, puerperium | No diagnosis | 803 | 413 (43–1765) | 122 | 863 (254–2209) | 0.0002 |
| Diagnosis | 32 | 5516 (3961–7452) | 12 | 4866 (3114–6359) | 0.33 | |
| Cardio-vascular disease | No diagnosis | 801 | 419 (43–1799) | 125 | 892 (263–2945) | 0.0004 |
| Diagnosis | 34 | 4590 (1627–12791) | 9 | 9539 (4094–11502) | 0.37 | |
| (*) Mann-Whitney U test ICD = International Classification of Diseases IQR = Interquartile range | ||||||
| Table 3: Results of proportional odds model for testing the effect of coming from a country where there was violent conflict on health care costs, controlling for demographic and disease profile variables (N = 969). | |||
| Model | Variable | Odds Ratio (95% Confidence Interval) | p-value |
| Model 1 (R² = 9%) | Violent conflict | 1.94 (1.40–2.69) | <.0001 |
| Gender (1 = male; 2 = female) | 2.32 (1.83–2.93) | <.0001 | |
| Age | 1.02 (1.01–1.03) | <.0001 | |
| Model 2 R² = 29%; p <.0001* | Violent conflict | 1.64 (1.16–2.31) | 0.004 |
| Gender (1 = male; 2 = female) | 2.66 (2.09–3.39) | <.0001 | |
| Age | 0.99 (0.98–1.00) | 0.05 | |
| Diseases of the musculoskeletal system | 2.74 (1.84–4.09) | <.0001 | |
| Diseases of the respiratory system | 1.74 (1.19–2.55) | 0.004 | |
| Mental disorders | 3.20 (2.17–4.72) | <.0001 | |
| Skin diseases | 1.38 (0.88–2.16) | 0.16 | |
| Injuries | 2.62 (1.63–4.22) | <.0001 | |
| Infectious and parasitic diseases | 2.82 (1.69–4.71) | <.0001 | |
| Cardio-vascular diagnoses | 4.28 (2.09–8.80) | <.0001 | |
| Model 3 R² = 69%; p <.0001* | Violent conflict | 0.97 (0.64–1.46) | 0.88 |
| Gender (1 = male; 2 = female) | 1.70 (1.28–2.26) | 0.0002 | |
| Age | 0.96 (0.95–0.97) | <.0001 | |
| Diseases of the musculoskeletal system | 1.06 (0.66–1.70) | 0.82 | |
| Diseases of the respiratory system | 0.81 (0.52–1.25) | 0.34 | |
| Mental disorders | 1.69 (1.06–2.68) | 0.03 | |
| Skin diseases | 0.60 (0.36–1.00) | 0.05 | |
| Injuries | 0.64 (0.36–1.14) | 0.13 | |
| Infectious and parasitic diseases | 1.53 (0.85–2.74) | 0.15 | |
| Cardio-vascular diagnoses | 1.39 (0.52–3.69) | 0.50 | |
| Number of visits | 1.25 (1.22–1.29) | <.0001 | |
| Duration of the A-Care insurance (months) | 1.01 (1.00–1.03) | 0.11 | |
| Decision: rejected vs. pending decision | 0.36 (0.26–0.50) | <.0001 | |
| Decision: rejected vs. accepted | 0.67 (0.43–1.04) | 0.07 | |
| Decision: pending decision vs. accepted | 0.53 (0.34–0.83) | 0.006 | |
| *R² = Nagelkerke R². The corresponding p-value represents the difference with the previous model, calculated by comparing the log likelihood parameters. | |||
| Table 4: Results of the additive modelling analysis, testing the relationship between depression and the number of years after cessation of conflict. | |||||
| Model | Parameter | DF | Sums of Squares | Chi-square | p-value |
| Depression | Spline (number of years after cessation of conflict) | 2 | 2.67 | 2.67 | 0.26 |
| Table 5: Results of the logistic regression analysis testing the relationship between post-traumatic stress disorder (PTSD) and the number of years after cessation of conflict. | |||||
| Parameter | DF | Estimate | Standard Error | Chi-square | p-value |
| Intercept | 1 | –3.5974 | 0.2733 | 173.25 | <.0001 |
| Number of years after cessation of conflict | 1 | 0.2173 | 0.0741 | 8.59 | 0.0034 |
In this epidemiological study, we investigated the effects of immigration from war zones on the cost of health care in receiving countries. We found that health care costs were twice as high for patients from countries with violent conflict than for patients from countries where there was no conflict.Our data suggest that the main driver behind the higher costs of asylum seekers from countries with violent conflicts is due less to their demographic or clinical profile than to the fact that applications for asylum by individuals from countries with violent conflicts are less often or less quickly rejected. A longer stay in the health care system leads to more health care usage and, consequently, higher cost generation during the time that the patients have asylum seeker status.
It is possible, however, that a patient’s clinical profile plays a larger role in cost generation than is suggested by our data. For instance, language barriers and a lack of routinely available interpreter services in the A-Care HMO have resulted in poor communication, which in turn may have led to a lower number of diagnoses for specific conditions (mental disorders, in particular), thereby downplaying the actual contribution of diagnoses to costs. In fact, we found in another study, that was based on the same patient population, that the presence of an interpreter made it possible to reach an effective solution after fewer visits, and, conversely the absence of interpreters made the number of visits increase [33].
In spite of the fact that, in contrast to many studies, mental problems were diagnosed only infrequently in this patient population and that this could be considered as evidence for the existence of language barriers, there are some other possible explanations for the low numbers of these diagnoses. One alternative explanation is that mental complaints were expressed with somatic symptoms rather than psychological ones [2, 34, 35]. Another possible explanation is that mental disorders take a longer time to develop [36, 37] and are possibly triggered by what Keilson has termed sequential-traumatisation (implying a sequence of traumatising events, and not just one event [38]) or by post-migration stress [39–41]. Our post-hoc analysis provided some evidence for the latter alternative. However, we are aware that this apparent connection may also be a result of other processes, such as how the former level of violence in the country of origin relates to the manifestation of symptoms in the patient.
A similar side-finding, for which we do not have enough qualitative information to allow interpretation of the observation, is that women from countries with violent conflicts had significantly more pregnancies than those from countries with no conflicts. This observation is in line with previous findings of an increased risk of rape and unwanted pregnancies in women fleeing from war-torn countries [42, 43].
Whether the results of this study can be generalised depends on the legal system of a country or region in terms of dealing with asylum seekers and the organisation of the health care system. The health care system in Switzerland is fragmented across the various cantons and, so does not allow pooling of data across different cantons. However, because asylum seekers are randomly allocated to cantons, extrapolation to the entire population of asylum seekers in Switzerland can be surmised. Refugees staying in the country illegally are, of course, not part of the generalisable population.
Our study has a number of limitations including the lack of socio-cultural information about the study participants, the necessarily ambiguous distinction between conflict and non-conflict countries, and the fragmented landscape of the Swiss health care system leading to small samples. Finally, the fact that the primary care physicians recorded the diagnoses without standardisation, may have introduced heterogeneity and possibly bias.
Notwithstanding its limitations, the merit of this study is, to our knowledge, that it is one of the first that has addressed health care costs with respect to the existence of violent conflict in the countries of origin of asylum seekers. The data contributes, firstly, to the body of research that considers such conflicts as a “major health determinant” [44] and a public health issue [45], and, secondly, to the development of ways in which asylum seekers are screened, integrated in local health systems, and cared for by migration offices [13, 46, 47], which creates opportunities for offering more appropriate health care and lowering health care costs associated with this patient population.
Although it is clear that a large part of the cost difference measured in this study was a result of higher numbers of asylum seekers from countries with violent conflicts being accepted as refugees, more information about the cost-determining factors may be gathered by a more precise measurement of diseases in this group. This may be achieved by making interpreter services routinely available (e.g., through leverage of migration offices, asylum seeker and refugee departments, or ministries of health), which could result in better diagnosis and treatment. In any case, the higher burden of disease found among patients from war-torn countries calls for more comprehensive screening strategies of asylum seekers [5, 48] in the receiving countries.
What is already known on this topic:
– During the past 60 years, there have been more than 200 wars worldwide, which have had, and still have, a profound impact on the health of people that is over and above the impact of the injuries that are directly attributable to the conflict.
– Asylum seekers fleeing from war-torn countries suffer disproportionately from ill health, mainly in the form of mental health problems (e.g., depression, post-traumatic stress disorder).
– What the consequences of violent conflicts on general health care costs in the receiving countries are is not known.
What this study adds:
– Healthcare costs of asylum seekers from countries experiencing violent conflict were found to be higher than those of asylum seekers from countries where there is no conflict.
– Despite a higher prevalence of illness in patients from countries with violent conflict, the length of time spent in administrative asylum seeker status seemed to be the main driver of health care costs.
– Language barriers and the lack of comprehensive early screening of asylum seekers are likely reasons of driving costs upward.
1 Kienzler H. Debating war-trauma and post-traumatic stress disorder (PTSD) in an interdisciplinary arena. Soc Sci Med. 2008;67(2):218–27.
2 Adams KM, Gardiner LD, Assefi N. Healthcare challenges from the developing world: post-immigration refugee medicine. Bmj. 2004;328(7455):1548–52.
3 People’s Health Movement, Global Health Watch 2 – an alternative World Health Report2008, London: Zed Books.
4 Hearn-Walker J. Migrants’ access to health care needs to be improved, conference is told. Bmj. 2009;338: p. b1244.
5 Norredam M, Mygind A, Krasnik A. Access to health care for asylum seekers in the European Union – a comparative study of country policies. Eur J Public Health. 2006;16(3):286–90.
6 Correa-Velez I, Gifford SM, Bice SJ. Australian health policy on access to medical care for refugees and asylum seekers. Aust New Zealand Health Policy. 2005;2:23.
7 Harris M, Zwar N. Refugee health. Aust Fam Physician. 2005;34(10):825–9.
8 UN Refugee Agency, Asylum Levels and Trends in Industrialized Countries: Second Quarter, 2006, 2006: Geneva.
9 Stiglitz J, Bilmes L. The three trillion dollar war2008, New York: W.W. Norton & Company, Inc.
10 Macpherson DW, Gushulak BD, Macdonald L. Health and foreign policy: influences of migration and population mobility. Bull World Health Organ. 2007;85(3):200–6.
11 Beaglehole R, Yach D. Globalisation and the prevention and control of non-communicable disease: the neglected chronic diseases of adults. Lancet. 2003;362(9387):903–8.
12 Gushulak BD, Macpherson DW. The basic principles of migration health: Population mobility and gaps in disease prevalence. Emerg Themes Epidemiol. 2006;3:3.
13 Feldman R. Primary health care for refugees and asylum seekers: A review of the literature and a framework for services. Public Health. 2006;120(9):809–16.
14 Thomas SL, Thomas SD. Displacement and health. Br Med Bull. 2004;69:115–27.
15 Hull SA, Boomla K. Primary care for refugees and asylum seekers. Bmj. 2006;332(7533):62–3.
16 Bischoff A, et al. Health and ill health of asylum seekers in Switzerland: an epidemiological study. Eur J Public Health. 2009;19(1):59–64.
17 Cardozo BL, et al. Mental Health, Social Functioning, and Attitudes of Kosovar Albanians Following the War in Kosovo. JAMA. 2000;284(5):569–77.
18 Momartin S, et al. Dimensions of trauma associated with posttraumatic stress disorder (PTSD) caseness, severity and functional impairment: a study of Bosnian refugees resettled in Australia. Soc Sci Med. 2003;57(5):775–81.
19 Silove D. The psychosocial effects of torture, mass human rights violations, and refugee trauma: toward an integrated conceptual framework. J Nerv Ment Dis. 1999;187(4):200–7.
20 Schaal S, Elbert T. Ten years after the genocide: trauma confrontation and posttraumatic stress in Rwandan adolescents. J Trauma Stress. 2006;19(1):95–105.
21 Tang SS, Fox SH. Traumatic experiences and the mental health of Senegalese refugees. J Nerv Ment Dis. 2001;189(8):507–12.
22 McColl H, Johnson S. Characteristics and needs of asylum seekers and refugees in contact with London community mental health teams: a descriptive investigation. Soc Psychiatry Psychiatr Epidemiol. 2006;41(10):789–95.
23 Barr RG, Menzies R. The effect of war on tuberculosis. Results of a tuberculin survey among displaced persons in El Salvador and a review of the literature. Tuber Lung Dis. 1994;75(4):251–9.
24 Hondius AJ, et al. Health problems among Latin-American and middle-eastern refugees in The Netherlands: relations with violence exposure and ongoing sociopsychological strain. J Trauma Stress. 2000;13(4):619–34.
25 OECD, OECD Reviews of Health Systems Switzerland, ed. OECD2006, Paris: WHO & OECD.
26 Wieland T. Gesundheitsversorgung von Asylsuchenden: Grenzen unseres Gesundheitssystems. Schweizerische Aerztezeitung. 2000;81:2673–6.
27 Reinhardt UE. The Swiss health system: regulated competition without managed care. JAMA. 2004;292(10):1227–31.
28 OANDA. The currency converter. 2009 2/5/2009]; Available from: http://www.oanda.com/.
29 DIMDI, ICD-10. Internationale statistische Klassifikation der Krankheiten und verwandter Gesundheitsprobleme. Band 12001, Bern: Hans Huber.
30 Department of Peace and Conflict Research (Uppsala University). Uppsala Conflict Data Program. 2011 [cited 2011 2011/04/09]; Available from: http://www.pcr.uu.se/research/ucdp/.
31 O’Connell AA. Logistic regression models for ordinal response variable2006, London: Sage publications.
32 Hastie T, Tibshirani RJ. Generalized Additive Models1990, London: Chapman & Hall.
33 Bischoff A, Denhaerynck K. What do language barriers cost? An exploratory study among asylum seekers in Switzerland. BMC Health Services Research. 2010;10(1):248.
34 Westermeyer J, et al. Somatization among refugees: an epidemiologic study. Psychosomatics. 1989;30(1):34–43.
35 Junod Perron N, Hudelson P. Somatisation: illness perspectives of asylum seeker and refugee patients from the former country of Yugoslavia. BMC Fam Pract. 2006;7:10.
36 Marshall GN, et al. Mental health of Cambodian refugees 2 decades after resettlement in the United States. JAMA. 2005;294(5):571–9.
37 Mollica RF, et al. Longitudinal study of psychiatric symptoms, disability, mortality, and emigration among Bosnian refugees. JAMA. 2001;286(5):546–54.
38 Moser C. Zwischen Normalität und Ueber-Leben: Bosnische Flüchtlinge in der Schweiz, in Migration – eine Herausforderung für Gesundheit und Gesundheitswesen, SRK, Editor 2004, Seismo Verlag, Sozialwissenschaften und Gesellschaftsfragen: Zürich. p. 139–149.
39 Silove D, Steel Z, Watters C. Policies of deterrence and the mental health of asylum seekers. JAMA. 2000;284(5):604–11.
40 Hallas P, et al. Length of stay in asylum centres and mental health in asylum seekers: a retrospective study from Denmark. BMC Public Health. 2007;7(1):288.
41 Heptinstall E, Sethna V, Taylor E. PTSD and depression in refugee children: associations with pre-migration trauma and post-migration stress. Eur Child Adolesc Psychiatry. 2004;6:373–80.
42 Bartlett LA, Purdin S, McGinn T. Forced migrants – turning rights into reproductive health. Lancet. 2004;363(9402):76–7.
43 Otsea K. Prioritizing reproductive health for refugees. Initiat Reprod Health Policy. 1999;3(1):1–3.
44 Morabia A. War, a major health determinant. Soz Praventivmed. 2001;46(3):145.
45 Obermeyer Z, Murray CJ, Gakidou E. Fifty years of violent war deaths from Vietnam to Bosnia: analysis of data from the world health survey programme. BMJ. 2008;336(7659):1482–6.
46 Loutan L, et al. Impact of trauma and torture on asylum seekers. European Journal of Public Health. 1999;9:93–6.
47 Wieland T. Gesundheitsversorgung von Asylsuchenden. Schweizerische Aerztezeitung. 2000;81(47):2673–6.
48 Francois G, et al. Inspecting asylum seekers upon entry – a medico-ethical complex. Eur J Public Health. 2008;18(6):552–3.
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article were reported.