Figure 1
Number of deceased donors in Switzerland, per year.
DOI: https://doi.org/10.4414/smw.2011.13265
Solid organ transplantation nowadays is confronted with two major issues: first, organ shortage, and second, the increasing age of deceased donors. Switzerland has one of the lowest organ donation rates in Europe (15.4 per million of population [pmp] in 1998, 11.8 pmp in 2008). Since 2003, the gap between donated organs and patients on the waiting list has widened dramatically. By the end of 2008, 942 patients were listed for a transplantation (+47% compared with 2003), while the quota of organ donors and the total number of transplanted organs declined by 5.3% and 3%, respectively [1]. As a consequence, the waiting list mortality has risen by 12.7% between 2003 and 2008[1, 2].
Various reasons can be cited for the mounting average age of the donors. Generally, the demographic trend in “first world” countries shows an increase in life expectancy, so it should come as no surprise that the donors are getting older as well. A more specific reason might be found in the fact that in Switzerland, during the study period, several measures and campaigns to improve the security for leisure activities and road safety were implemented, most prominently the reduction of the legal blood-alcohol limit for driving to 0.5‰ on 1 January 2005.
Up to now, the transplantation of organs from the so-called marginal or extended criteria donors (ECDs) has been associated with inferior outcomes. There is no generally recognised definition of the criteria which have to be fulfilled by a donor to be considered an ECD, but the following parameters are usually taken account of: donor age above 50–65 years (depending on the organ), prolonged cold and/or warm ischaemia time, and prolonged donor ICU stay. Given that ECDs will possibly become more prevalent (due to organ shortage and the growing average age of the donors), a careful donor and recipient profiling and selection may gain relevance in the not so distant future – but for now, let the results of our analysis of the deceased organ donors’ patient characteristics speak for themselves.
Data were obtained from Swisstransplant, Switzerland’s national organ procurement organisation. In a retrospective study, patient records of all deceased (brain-dead) organ donors in Switzerland between 1 January 1998 and 31 December 2008 were reviewed. There were 1004 brain-dead donors in total (59.4% male, 40.6% female) aged on average 46.1 ± 17.6 years. Data were collected and analysed for heart, lung, liver, kidney, and pancreas retrieval.
Frequency and distribution of donor criteria, overall and number of organs procured per donor were evaluated using Excel 2007 (Microsoft Inc., CA, USA) and GraphPad Prism 5.00 for Windows (San Diego, CA, USA). Significance of differences was analysed in Excel using a two sided Student t-test and a p-value <0.05 was considered significant.
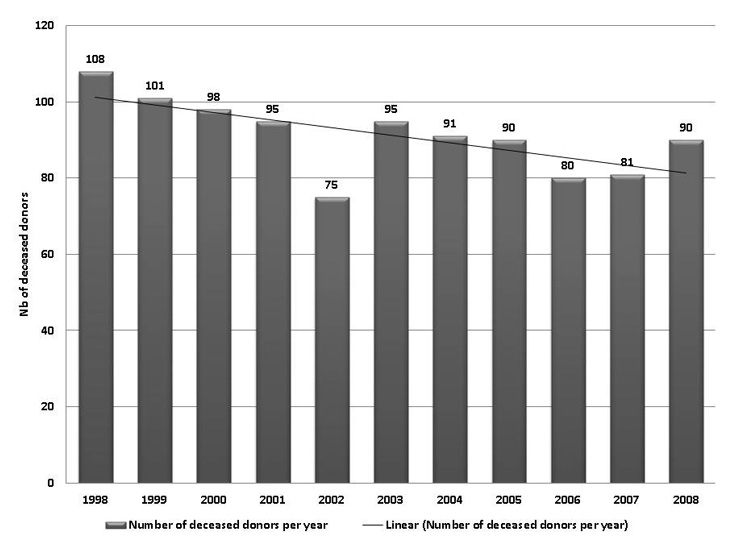
Figure 1 shows the number of deceased organ donors per year in Switzerland from 1998 to 2008. In 1998, the total of donors was the highest (108) in the whole study period. It then declined gradually to 95 donors in 2001. In the year 2002, there was a 21% collapse of the donor quota, which then bottomed at 75. From 2003 (95 donors) to 2006 (80 donors), the rates still showed a negative trend, whereas the number of donors is increasing again since 2007 (+11.1% in 2008). Statistical analysis revealed, due to the small number of donors per year, no significant decrease of organ donors in the time period between 1998 and 2008. However the linear trend (y = 1.9818x+103.16), displayed in figure 1, showed a tendency towards a decrease of organ donors in the observed time period.
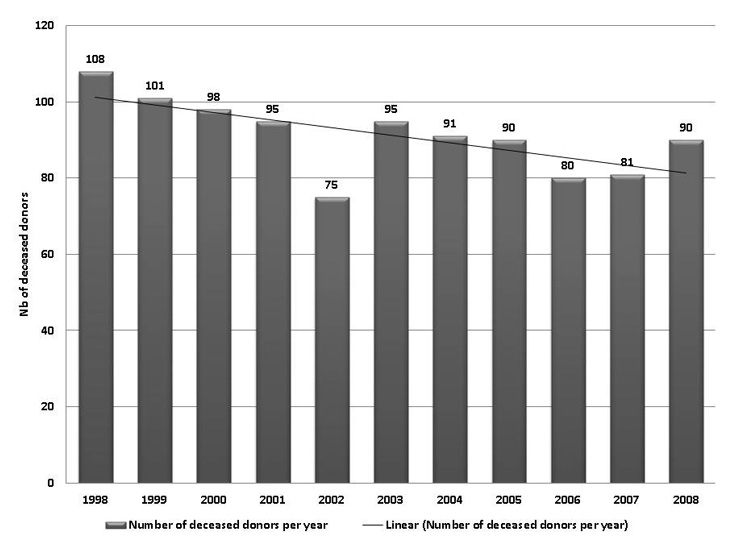
Figure 1
Number of deceased donors in Switzerland, per year.
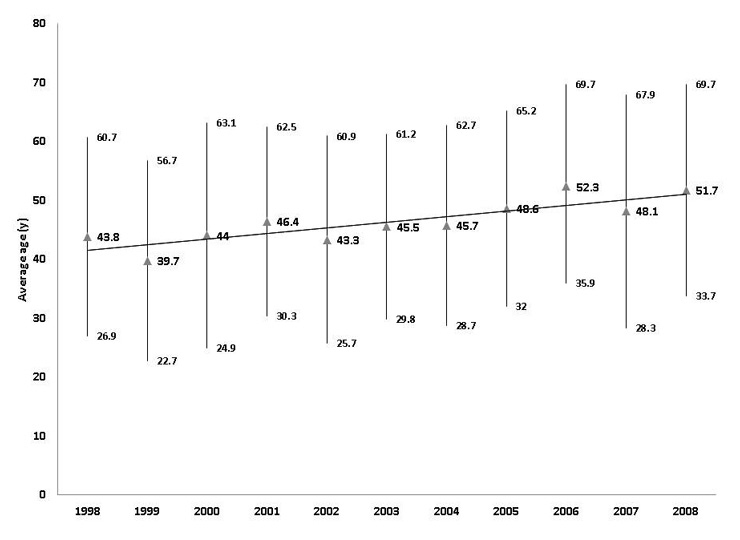
Figure 2
Average age (in years) of the deceased donors per year, displaying ±1.SD (standard deviation) and linear trend.
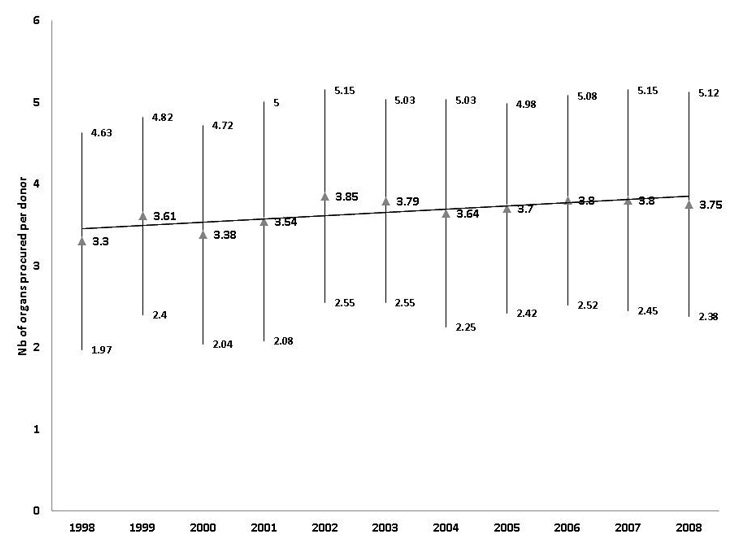
Figure 3
Average number of organs procured per donor, displaying ±1.SD (standard deviation) and linear trend.
The mean age of the donors is displayed in figure 2. Even though there are minor variations from one year to another, it shows a clear upward trend from an average of 43.8 ± 16.9 years in 1998 to 51.7 ± 18.0 years in 2008 (+27.6%; p <0.05). This can be confirmed by the linear trend (y = 0.9527x+40.565), which clearly shows an increase in the average age of organ donors within the time period of 1998 to 2008.
The mean number of organs procured per donor increased during the study period, even though it varied quite substantially between the years, with a minimum of 3.30 ± 1.33 organs per donor in 1998, and two peaks with 3.85 ± 1.3 organs per donor in 2002 and 3.80 ± 1.28 in 2006, respectively 3.80 ± 1.35 in 2007 (fig. 3). There is a statistical significant increase in the number of procured organs per donor comparing the first time period between 01/1998 to 06/2003 and the second time period 07/1998 to 12/2008 (p <0.05).
The distribution of the causes of death is displayed in figure 4. When comparing the 2008 data with those of 1998, it is striking to note that cerebral haemorrhage (CHE) accounts for more than half of the causes in 2008 (52.8%, +16.7 percentage points). Conversely, the share of cranio-cerebral trauma (CTR) decreased by 22 percentage points to 16.9% of the donors’ deaths. The proportion of donors who died of suicide (SUI) was relatively stable over the years (median 5.6%), except for two peaks in 1999 and 2002 (12.9% and 13.3%, respectively). In 2008, donors who suffered anoxia (ANOX) became the third largest group (13.5%, +8.9 percentage points). A quite stable share of less than 10% during the whole study period was found for cerebrovascular insults (CVI, 0–6.1%), tumours (TUMOR, 0–3.7%), others (OTH, 0–7.8%), and no available data (N/A, 0–1.2%).
Figure 5 gives an overview of the development of the donors’ age distribution. When comparing the percentage shares in 1998 with those in 2008, the ≥65 years group (usually considered ECDs) had the most remarkable growth rate (+216.2%), and reaches a 26.6% share of all deceased donors in 2008. The largest group remains the 16–55 year-olds with a share of 50% of all donors in 2008 (–23.6% compared with 1998). In 2008, the joint share of the 56–64 year-olds group and the ≥65 years group is 46.8%, and it thus almost equals the 16–55 year-olds group. The 0–15 years group is the smallest with less than 10 donors per year.
Figure 6 shows the evolution of transplanted heart, lung, liver, kidney, and pancreas grafts per year. The average number of transplantations per year was 331.9 (±23.4), with a minimum of 289 transplantations in 2002 and a maximum of 364 in 1999.
During the comprehensive study period, a total of 3651 heart, lung, liver, kidney, and pancreas grafts were transplanted. Kidneys accounted for 52% of the transplantations, livers for 21.1%, hearts for 11%, lungs for 9.9%, and pancreas for 5.9%. Table 1 summarises the number of organs, the quota of transplantation (which designates the respective percentage of grafts that were actually transplanted) and the average age of the donors, calculated by organ.
The quota of transplantations was 94.7% for kidneys, but only 21.6% for pancreas. As for the average age of the donors, it was highest in the liver grafts group (49.4 ± 13.7 years) and lowest in the lung grafts group (43.7 ± 15.7 years), without reaching statistical significance (p = ns).
| Table 1: Summary of the transplanted grafts 1998–2008 per organ (heart, lung, kidney, liver and pancreas (whole pancreas and islets); quota of transplantations = percentage of procured organs in relation to the total number of donors in this study (n = 1004)); average age of donor, displayed by procured organ. Results displayed as mean value ± 1. SD (standard deviation). | ||||||||||
| Heart | Lung | Kidney | Liver | Pancreas | ||||||
| Number | 402 | 362 | 1900 | 770 | 217 | |||||
| Quota of transplantations | 40.0% | 36.1% | 94.7% | 76.7% | 21.6% | |||||
| Donors’ age (years, mean ±1 SD) | 46.4 | ±16.7 | 43.7 | ±15.7 | 48.65 | ±13.85 | 49.4 | ±13.7 | 45.6 | ±9.3 |
As mentioned before, transplantation in Switzerland is confronted not only with a low donation rate, but it is also faced with organ donors whose mean age increased by 7.9 years between 1998 and 2008 (p <0.05). When looking at the average number of organs procured per donor (fig. 3), it seems that the discrepancy between a rising number of transplant candidates and a restricted donor pool has lead to the transplantation of organs previously not allocated for various reasons. The noteworthy quota of organs procured per donor in Switzerland is similar to the one in the UK, which has a comparable donation rate [3], and it is considerably higher than in countries with elevated donation rates [4, 5]. Unsurprisingly, the peaks in the number of organs procured per donor occurred in the same years (2002, 2006) when the number of donors was lowest (fig. 1), resulting in a relatively stable proportion of transplanted organs over the years (fig. 6). The high quota of organs procured per donor, ranging from 3.30 ± 1.33 to 3.85 ± 1.30 during the study, is even more remarkable, given the development of the age distribution of the donors, with the ≥56 years old group having a share of over 40% since 2006 (fig. 5). These findings are astonishing considering that a large recently published analysis of the United Network for Organ Sharing (UNOS) deceased donor registry data revealed that both, increasing age, and anoxia as cause of death significantly influence organ yield [6]. In this study, the average number of organs procured per donor was 3.13 ± 1.77 (compared with 3.65 ± 0.18 in our study), and the mean age of the donors was 40.1 ± 19 years while in our study population, it was 46.1 ± 17.6 years.
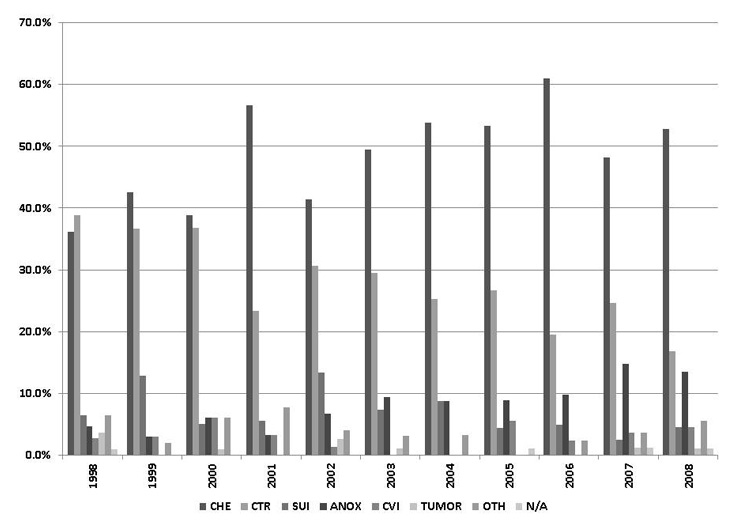
Figure 4
Causes of death (percentage) of the donors per year.
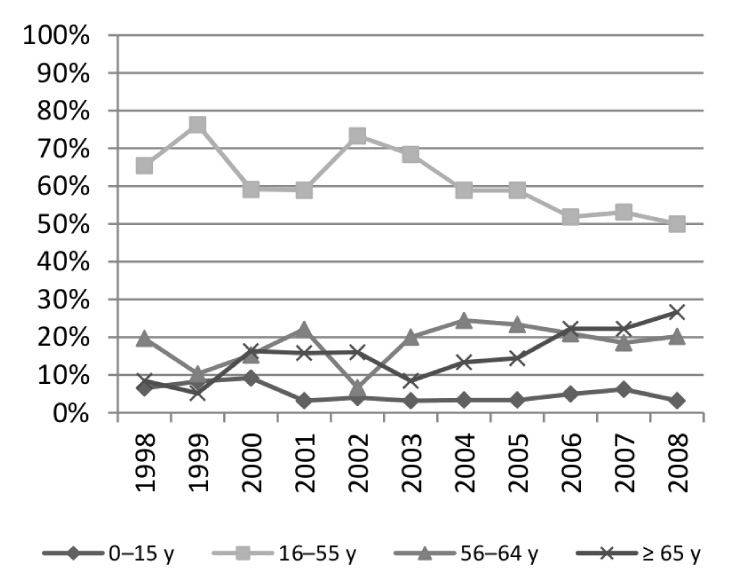
Figure 5
Age distribution of the donors per year, displaying the percentage of donors within the age range of 0 to 15 years, 16 to 55 years, 56 to 64 years and 65 years and above.
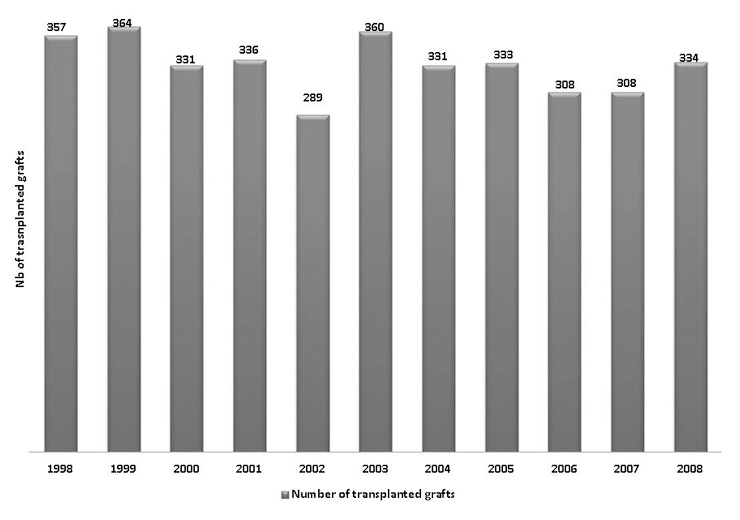
Figure 6
Number of transplanted solid organs in Switzerland. Results displayed for organs procured from deceased donors. Living is not included in this figure.
The distribution of the causes of death of the donors (fig. 4) shows growing shares for cerebral haemorrhage as well as for anoxia, while cranio-cerebral trauma, the largest group in 1998, lost more than half of its size during the study. These data are in line with a recently published overview on the causes of death in Switzerland by the Federal Statistical Office [7]. Table 2 below shows a selection of these data with the absolute numbers and the incidence per 100’000 population. When contrasting 2008 with 1998, road accidents (supposedly causing cranio-cerebral trauma) decreased 33.8% by number and 40.3% by incidence per 100’000 population.
A similar downward trend in the share of accidents was also observed in the Eurotransplant area, where in 1998, 32% of the deceased donors belonged to this category, while in 2008, the rate had dropped to 22.9% (–28.4%) [8, 9]. As pointed out in the Introduction section, data on the incidence of road accidents in Switzerland suggest that the reduction of the legal blood-alcohol limit for driving to 0.5‰ on 1 January 2005 may have resulted in a substantial reduction of lethal road accidents, which in total decreased by 19.8% and 9.5% in the years 2005 and 2006, compared with the respective preceding year [10].
Considering the question whether the more frequent transplantation of grafts from ECDs might have a negative impact on the outcomes, recent studies in the use of ECD heart [11, 12], lung [13–16], liver [17–19], kidney [20–22], and pancreas grafts [23] show somewhat promising results. In summary, most studies emphasise the potential of ECD grafts to reduce waiting list mortality [24–26], as well as the significance of an appropriate donor and recipient profiling and selection, e.g., age matching and risk assessment [17, 21, 23, 24, 27, 28]. However, and despite this encouraging upshot, it should be kept in mind that the data presented in our study show that in Switzerland – as opposed to other countries, where ECDs are supposed to expand the donor pool, grafts from ECDs are not supplementing the availability of organs but replacing grafts no longer available from “standard” donors. This fact must be taken into account when comparing outcome data from different countries.
Limitations of the study: The authors are aware that this study gives only an overview of deceased Swiss donor characteristics in the defined study period between 1998 and 2008. However for the first time these data have been analysed in the context of a long time-period, showing significant increases in the average age of donors and in the number of organs procured per donor. The results clearly underline the importance of taking into account donor characteristics in a small country like Switzerland with a very low number of donors per million habitants, compared to the countries surrounding us, when analysing and comparing outcome data with other countries.
In conclusion, the present study shows that in Switzerland, like in other European countries, organ shortage leads to a higher number of organs procured per donor. Furthermore, a shift in the causes of death markedly increased the average age of donors, and transplantation medicine is confronted with a growing number of ECDs. The good news is that despite these adversities, outcomes do not worsen, and that nowadays, amongst others due to refined immunosuppressive regimens [29–31], the 10-year survival of transplant recipients is better than ever before.
| Table 2: Comparison of causes of death 1998 vs. 2008, by the Federal Statistical Office [7]. | ||||||||||
| 1998 | 2008 | |||||||||
| Number | Percentage | Incidence per 100'000 pop. | Number (compared with 1998) | Percentage | Incidence p. 100'000 pop. (compared with 1998) | |||||
| Total number of deaths in Switzerland | 62567 | 100% | 601 | 61233 | (–2.1%) | 100% | 478 | (–20.5%) | ||
| Cerebrovascular diseases | 4854 | 8% | 41 | 4077 | (–16.0%) | 7% | 27.4 | (–33.2%) | ||
| Cardiac diseases (total) | 18852 | 30% | 166 | 16956 | (–10.1%) | 28% | 118 | (–28.9%) | ||
| Ischaemic cardiac diseases | 11257 | 18% | 101 | 8861 | (–21.3%) | 14% | 63 | (–37.6%) | ||
| Circulation system | 25443 | 41% | 222 | 22321 | (–12.3%) | 36% | 155 | (–30.2%) | ||
| Pulmonary embolism | 333 | 1% | 3.1 | 300 | (–9.9%) | 0% | 2.2 | (–29.0%) | ||
| Accidents and violence | 3561 | 6% | 41.6 | 3742 | (+5.1%) | 6% | 36.3 | (–12.7%) | ||
| Accidents (total) | 2036 | 3% | 22.2 | 2274 | (+11.7%) | 4% | 20.1 | (–9.5%) | ||
| Road accidents | 547 | 1% | 7.2 | 362 | (–33.8%) | 1% | 4.3 | (–40.3%) | ||
| Suicide | 1371 | 2% | 17.5 | 1313 | (–4.2%) | 2% | 14.4 | (–17.7%) | ||
| Source: Federal Statistical Office, http://www.bfs.admin.ch | ||||||||||
1 Swisstransplant. Jahresbericht 2008. Bern: Swisstransplant, Schweizerische Nationale Stiftung für Organspende und Transplantation; 2009. Available from: http://www.swisstransplant.org.
2 Swisstransplant. Jahresbericht 2007. Bern: Swisstransplant, Schweizerische Nationale Stiftung für Organspende und Transplantation; 2008. Available from: http://www.swisstransplant.org.
3 Summers DM, Counter C, Johnson RJ, Murphy PG, Neuberger JM, Bradley JA. Is the Increase in DCD Organ Donors in the United Kingdom Contributing to a Decline in DBD Donors? Transplantation. 2010;Nov 12 [Epub ahead of print].
4 Klein AS, Messersmith EE, Ratner LE, Kochik R, Baliga PK, Ojo AO. Organ donation and utilization in the United States, 1999-2008. Am J Transplant. 2010;10(4, Pt 2):973–86.
5 Matesanz R, Coll E, Garrido G. Realities in organ donation. Am J Transplant. 2007;7(11):2641–2; author reply 2643–4.
6 Selck FW, Deb P, Grossman EB. Deceased organ donor characteristics and clinical interventions associated with organ yield. Am J Transplant. 2008;8(5):965–74.
7 Bundesamt für Statistik BFS. Medienmitteilung: Todesursachen des Jahres 2008. Eidgenössisches Departement des Innern EDI, Bundesamt für Statistik BFS; 2010. Available from: http://www.bfs.admin.ch/bfs/portal/de/index/news/medienmitteilungen.Document.135839.pdf.
8 Cohen B, Persijn G, De Meester J (eds.). Eurotransplant Annual Report 1998. Leiden: Eurotransplant International Foundation; 1998. Available from: http://www.eurotransplant.org/?id=annual_report.
9 Oosterlee A, Rahmel A (eds.). Eurotransplant Annual Report 2008. Leiden: Eurotransplant International Foundation; 2008. Available from: http://www.eurotransplant.org/?id=annual_report.
10 bfu – Beratungsstelle für Unfallverhütung. Unfallgeschehen im Strassenverkehr, 1965–2009 (Fig. USV.T.02). In: STATUS 2010: Statistik der Nichtberufsunfälle und des Sicherheitsniveaus in der Schweiz, Strassenverkehr, Sport, Haus und Freizeit. Bern: bfu; 2010. Available from: http://www.bfu.ch/PDFLib/1415_75.pdf.
11 Forni A, Luciani GB, Chiominto B, Pilati M, Mazzucco A, Faggian G. Impact of donor quality on outcome of heart transplantation. Eur J Cardiothorac Surg. 2010;38:788–94.
12 Forni A, Faggian G, Chiominto B, Iafrancesco M, Patelli F, Innocente F, et al. Heart transplantation in older candidates. Transplant Proc. 2007;39(6):1963–6.
13 Mordant P, Bonnette P, Puyo P, Sage E, Grenet D, Stern M, et al. Advances in lung transplantation for cystic fibrosis that may improve outcome. Eur J Cardiothorac Surg. 2010;38(5):637–43.
14 Meers C, Van Raemdonck D, Verleden GM, Coosemans W, Decaluwe H, De Leyn P, et al. The number of lung transplants can be safely doubled using extended criteria donors; a single-center review. Transpl Int. 2010;23(6):628–35.
15 Dezza MC, Parigi PC, Corno V, Lucianetti A, Pinelli D, Zambelli M, et al. Lung transplantation with grafts from elderly donors: a single-center experience. Transplant Proc. 2010;42(4):1262–4.
16 Aigner C, Winkler G, Jaksch P, Seebacher G, Lang G, Taghavi S, et al. Extended donor criteria for lung transplantation – a clinical reality. Eur J Cardiothorac Surg. 2005;27(5):757–61.
17 Segev DL, Maley WR, Simpkins CE, Locke JE, Nguyen GC, Montgomery RA, et al. Minimizing risk associated with elderly liver donors by matching to preferred recipients. Hepatology. 2007;46(6):1907–18.
18 Schemmer P, Nickkholgh A, Hinz U, Gerling T, Mehrabi A, Sauer P, et al. Extended donor criteria have no negative impact on early outcome after liver transplantation: a single-center multivariate analysis. Transplant Proc. 2007;39(2):529–34.
19 Zapletal C, Faust D, Wullstein C, Woeste G, Caspary WF, Golling M, et al. Does the liver ever age? Results of liver transplantation with donors above 80 years of age. Transplant Proc. 2005;37(2):1182–5.
20 De Serres SA, Caumartin Y, Noël R, Lachance JG, Côté I, Naud A, et al. Dual-Kidney Transplants as an Alternative for Very Marginal Donors: Long-Term Follow-Up in 63 Patients. Transplantation. 2010;90(10):1125–30.
21 Saxena R, Yu X, Giraldo M, Arenas J, Vazquez M, Lu CY, et al. Renal transplantation in the elderly. Int Urol Nephrol. 2009;41(1):195–210.
22 Remuzzi G, Cravedi P, Perna A, Dimitrov BD, Turturro M, Locatelli G, et al. Long-term outcome of renal transplantation from older donors. N Engl J Med. 2006;354(4):343–52.
23 Neidlinger NA, Odorico JS, Sollinger HW, Fernandez LA. Can ’extreme’ pancreas donors expand the donor pool? Curr Opin Organ Transplant. 2008;13(1):67–71.
24 Cameron AM, Ghobrial RM, Yersiz H, Farmer DG, Lipshutz GS, Gordon SA, et al. Optimal utilization of donor grafts with extended criteria: a single-center experience in over 1000 liver transplants. Ann Surg. 2006;243(6):748–53; discussion 753–5.
25 Barshes NR, Horwitz IB, Franzini L, Vierling JM, Goss JA. Waitlist mortality decreases with increased use of extended criteria donor liver grafts at adult liver transplant centers. Am J Transplant. 2007;7(5):1265–70.
26 Merion RM, Ashby VB, Wolfe RA, Distant DA, Hulbert-Shearon TE, Metzger RA, et al. Deceased-donor characteristics and the survival benefit of kidney transplantation. JAMA. 2005;294(21):2726–33.
27 Pascual J, Zamora J, Pirsch JD. A systematic review of kidney transplantation from expanded criteria donors. Am J Kidney Dis. 2008;52(3):553–86.
28 López-Navidad A, Caballero F. Extended criteria for organ acceptance. Strategies for achieving organ safety and for increasing organ pool. Clin Transplant. 2003;17(4):308–24.
29 Cai J, Terasaki PI. Induction Immunosuppression Improves Long-Term Graft and Patient Outcome in Organ Transplantation: An Analysis of United Network for Organ Sharing Registry Data. Transplantation. 2010;Nov 4 [Epub ahead of print].
30 Dandel M, Lehmkuhl HB, Knosalla C, Hetzer R. Impact of different long-term maintenance immunosuppressive therapy strategies on patients’ outcome after heart transplantation. Transpl Immunol. 2010;23(3):93–103.
31 Agüero J, Almenar L, Martínez-Dolz L, Chamorro C, Moro J, Rueda J, et al. Influence of immunosuppression regimen on heart transplantation survival. Transplant Proc. 2006;38(8):2550–2.
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article was reported.