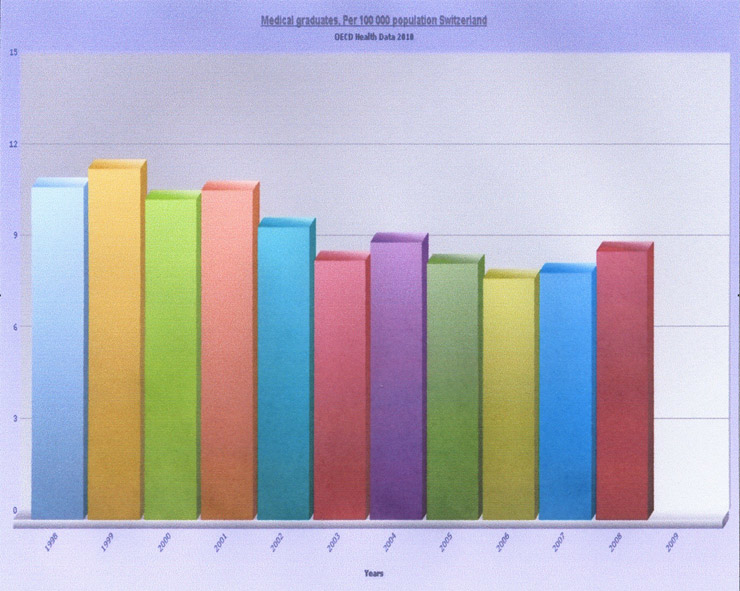
Figure 1
Evolution ofthe number of the new graduates/100 000 population in Switzerland between 1998-2008
DOI: https://doi.org/10.4414/smw.2011.13251
There is a progressive aging of the Swiss population with 16.8% of residents being over 64 years of age in 2009, compared to 9.6% in the early 1950s [1]. The projections for 2020 predict a proportion of 20–25% of residents to be older than 65 years [1]. As a consequence, needs for advanced treatments and particularly surgical care under anaesthesia are steadily increasing and will continue to increase. This is particularly the case for hip and knee replacements, cancer care and cataract surgery [2].In 2008, a total number of 1’166’631 anaesthetic procedures were performed in Switzerland, representing a 35% augmentation compared to 2002 [3].As a result, healthcare costs have increased greatly to reach 10.7% of the overall Gross Domestic Product (GDP) of Switzerland in 2008 [3].Annual costs related specifically to surgical care excess 11 billion francs [2].Consequently both cantons and the Swiss Confederation launched a series of initiatives aimed at controlling healthcare costs [4, 5].These include: a) a unified reimbursement scheme called TarMed introduced in 2004, b) a gradual reduction in acute care beds availability in hospitals, c) a progressive transfer of treatment costs directly to patients (30.8% of overall health expenditures, the highest rate in OCDE countries after Korea and Mexico), and d) a limitation in the number of physicians licensed and eligible for reimbursement under compulsory health insurance introduced in 2002 [6–9].In parallel, universities have limited the number of positions available for new students in medical schools by numerus clausus, which has been gradually introduced in Swiss universities since 1998 [10]. Consequently, the number of new graduates has dropped from 10.9/100’000 residents in 1998 to 8.8/100’000 residents in 2008 (fig. 1) [3].This is one of the lowest rates in Europe, as only Belgium, Poland and Slovenia have less medical graduates entering the healthcare workforce every year.
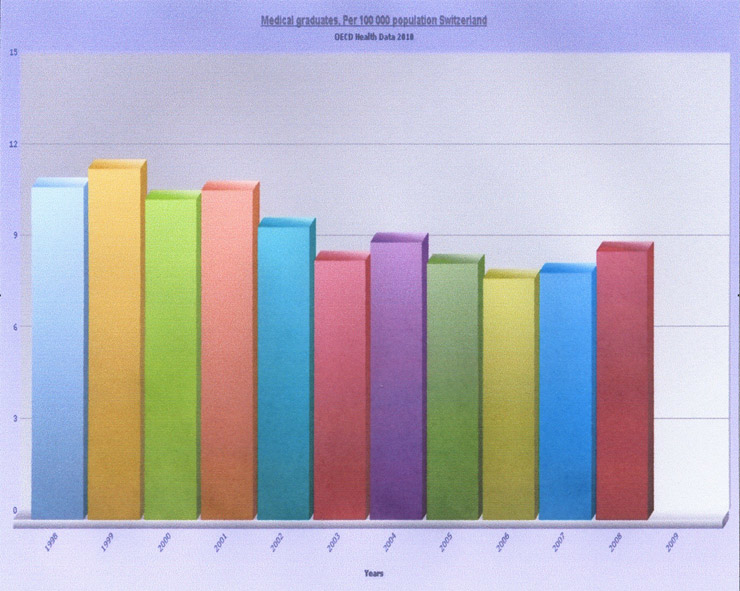
Figure 1
Evolution ofthe number of the new graduates/100 000 population in Switzerland between 1998-2008
If these different initiatives seek to stabilise health care costs, their potential side effects on professional practice, particularly in anaesthesia, cannot be minimised. This specialty is known to be very sensitive to cost containment strategies [11, 12].By limiting access to private professional practice while strictly controlling anaesthetic procedure fees, these initiatives can potentially harm the attractiveness of the specialty. In addition, the gradual decrease in the number of new doctors leaving medical schools and entering specialty training in anaesthesia and intensive care can also add to the drop of practicing anaesthetists. As a result, Switzerland may face a shortage of anaesthetists, particularly as the attractiveness of the profession is the main factor that determines the choice of the specialty (no preliminary examination or other type of selection process in place to enter the specialty). A study performed in 2002 in the French speaking part of Switzerland had shown a satisfying anaesthetic coverage of the population compared to other European countries, with an average density of 19.4 anaesthetists (including those certified and in training) per 100000 residents. In comparison, these figures are 19.9 per 100000 for Germany, 16.1 per 100000 in France and 15.5 per 100000 in Italy [13, 14].It is however currently unclear whether, seven years later, in the context of implicit rationing of healthcare provision, these cost containment strategies have had an effect on the number of anaesthetists in Switzerland and more particularly in the French and Italian speaking parts of the country, which contain four out of the seven medical schools. The impact of these cost containment initiatives on anaesthetists’ satisfaction is also unknown. It is crucial to answer this question in order to anticipate a possible demographic crisis in the anaesthesia workforce supply.
The purpose of this study was to assess current anaesthetists’ density, characteristics and satisfaction in the French and Italian speaking parts of Switzerland and to compare the results with data available and collected before the introduction of Cantonal and Federal cost containment initiatives in Switzerland.
We performed a cross-sectional study between March and June 2009 in the French and Italian speaking areas of Switzerland (7.5 cantons). We included all anaesthetists (in training or certified) practicing anaesthesia as a main activity, in public or private hospitals. We excluded participants if they were practising anaesthesia for one year or less as part of their training as emergency physicians or intensive care unit (ICU) specialists. We also excluded anaesthetists working full time in ICUs.
For each canton, two local study coordinators were recruited and asked to contact local professional organisations, private and public hospitals to list all anaesthetists working in their canton. This was done because the membership database of the Swiss physicians’ professional organisation (Federatio Medicorum Helveticorum - FMH) does not include physicians from foreign countries. The listing was used to identify study participants to be included in the survey. A questionnaire was handed or sent by local coordinators to each participant listed. Each participant, hospital and canton had a pre-defined ID number attributed by the study coordinators (CM, GH). Questionnaires were then sent to the study centre in Geneva. Anonymity was guaranteed by the fact that study coordinators only knew the ID numbers, and the list of names of practicing anaesthetists to which questionnaires were sent was only in possession of the local study coordinators. As a result, it was not possible to match ID numbers recorded on individual surveys and participants’ names. Reminders were systematically sent to all participants until the total numbers of questionnaires from the anaesthetists listed for each canton was reached, which required a maximum of 3 reminders. Written data collected through the survey were captured in an electronic format by a professional operator (Data Conversion, Geneva),before being sent to the study investigators by mail.
We used a 103 item questionnaire and included the same questions as those used in a previous 2002 survey on the anaesthetist workforce in Switzerland. The initial questionnaire was developed in French. It was designed by anaesthetists and epidemiologists at the Geneva University Hospital, and was reviewed and pre-tested by a Steering Committee of 15 professional anaesthetists for readability and acceptability. One independent bilingual physician translated all items into Italian and the final version was also pre-tested for readability and acceptability before being used.
The dimensions measured included personal information (i.e. gender, age, family status, professional training) and information on professional activity (i.e. type of institution, position, activity ratio, workload in March 2009, day and night calls, professional life plan). We also assessed participants’ satisfaction regarding different aspects of anaesthetic practice and life in general using specific validated items from the Johns Hopkins precursor study [15]. Three independent professional translators had previously translated these items from English into French [16]. To specifically measure the impact of the restriction on the number of physicians licensed for reimbursement under the compulsory health insurance scheme, an additional item specifically assessing this aspect was added to the questionnaire.
To assess density and other variables requiring population data, we used information recorded in the original listing from the local study coordinators, and population data available from the OCDE healthcare database and from the Swiss Federal Institute of Statistics in Neuchatel. University Hospitals Human Research and Ethics approval was not required for this study as no patient or sensitive information were collected.
Socio-demographic characteristics and professional activity related variables were described using frequency tables and proportions. Continuous variables such as age and working hours were transformed into separate and mutually exclusive categories. For other continuous variables (retirement age), we used means and standard deviations. Densities were calculated with proportions using data from local investigator registries and information (i.e. population by canton) from the databases of the Federal Office of Statistics. To assess the impact of cost containment policies on anaesthetists’ characteristics and working hours, we compared variables of the current study with data available from the previous study with the same questions and dimensions investigated in 2002. For job satisfaction, we used eight specific questions from the Johns Hopkins Precursor Study [15] related to work satisfaction, relationships with patients and colleagues as well as self-evaluated quality of care provided. These questions were limited to physicians practising for more than 10 years, as we asked them to compare the current situation to the situation ten years ago, before the introduction of federal restrictive measures to limit the number of physicians. We also assessed, by stratifying for anaesthesia practice category, the specific impact of the federal decree restricting physicians’ license for reimbursement under the compulsory health insurance. For all these analyses, the canton of Ticino and the Bernese Jura were excluded as no data had been collected for these two cantons in 2002. We used Chi-square, Fisher’s exact test, or binary logistic regression for categorical variables and derived odds ratio (OR) with 95% confidence interval (CI) to assess differences between groups. For continuous variables, including scores of satisfaction, we used student T test, Wilcoxon rank test and analysis of variance (ANOVA), depending on the number and distribution of variables. All statistical tests were two-tailed, with a level of significance set at p <0.05. Statistical analyses were performed with SPSS (Statistical Package for Social Sciences, version 17.0).
We identified a total of 506 practising anaesthetists (in training or certified), from the local coordinators lists, in the 7.5 cantons of the study (fig. 2). After the initial mailing and three reminders, 416 physicians (82%) participated in the survey. Participants were mainly men (58%) aged between 36 to 55, and of Swiss or European nationality (98%). The participation rate was the highest in the cantons of Fribourg (95%) and Valais (93%). The participant’s characteristics and level of participation are detailed in table 1.
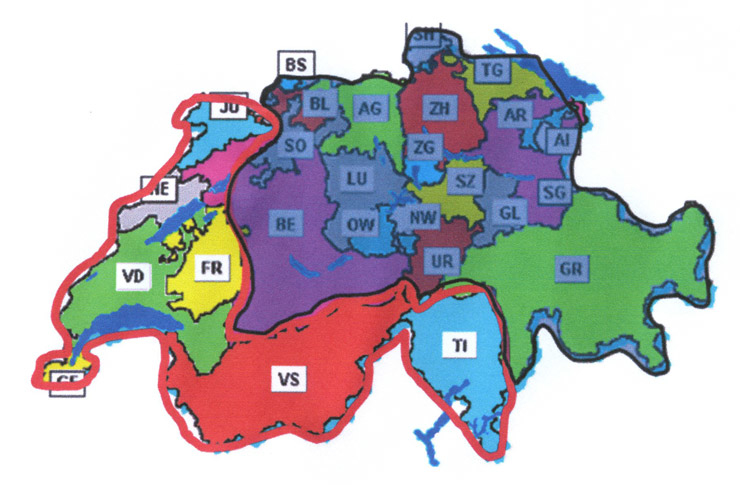
Figure 2
Study Sites
The overall density of anaesthetists for the French and Italian speaking parts of the country was 21.7/100’000 residents. The highest rate was found in the canton of Geneva and Vaud with one anaesthetist per 3’034 residents and 3866 residents respectively. Both cantons have medical schools and tertiary academic institutions. The lowest rate was in the Bernese Jura with one anaesthetist per 12’750 residents. Despite restriction policies, the overall number of anaesthetists has significantly increased since 2002, with 12% more practising anaesthetists in 2009, representing 1 anaesthetist for 4375 residents compared to 1 anaesthetist for 5136 residents in 2002. This increase is however smaller than the overall 35% augmentation in the number of surgical procedures (inpatient and outpatient) performed in Switzerland since 2002. Details are provided in table 2.
These characteristics are summarised in table 3. Compared to the period before the restriction policies implementation extracted from the 2002 survey data, an aging of practicing anaesthetists can be identified in 2009 with 14% versus 11% of anaesthetists being over 55 years of age. More women have joined the profession and their proportion has increased with 42% in 2009 compared to 35% in 2002 (p = 0.06). There are also more non-Swiss anaesthetists practicing in public or private since implementation of cost containment policies, with 19% compared to 11% in 2002 (p <0.05). The overall number of anaesthetists with a FMH title has also increased from 64% to 72% (p <0.05). The balance between the public and private sector remains constant with three quarters of anaesthetists still working in public hospitals in 2009 (p = 0.23).
The most important change between the two periods is a significant reduction in working hours in public hospitals. The average number of hours worked in public hospitals in 2002 was 59 hours/week on average. In 2009, this number dropped to 53 hours/week (p <0.001). In contrast, in private hospitals there was no difference before/after restriction policies and the average working time was around 50 hours a week (p = 0.43).
The majority of anaesthetists (60.8%) considered that their overall personal situation was better than in the previous 10 years (table 4). Increased satisfaction was higher in the area of the quality of care provided. In regards to relationships with patients, colleagues, workload or satisfaction at work, the views were mostly neutral showing no difference with the period before 2002, except in the area of respect shown to the doctor which was quoted by most participants as neutral to worse.
The successive federal decrees restricting the number of physicians licensed for reimbursement under the compulsory health insurance scheme had no impact on anaesthetists’ future projects, regardless of the type of hospital they were practicing in. The majority of anaesthetists surveyed (87.7%) answered that these measures had no influence on their future projects (table 5).
| Table 1: Demographic characteristics of participants. | |||
| Variables | n | % | |
| Gender | Males Females | 239 171 | 58 42 |
| Age | <35 years 36–55 years >55 years | 97 254 56 | 24 62 14 |
| Nationality | Switzerland European countries Other | 337 69 6 | 81 16 2 |
| Participants by Canton | Fribourg Geneva Jura Bernese Jura Neuchâtel Ticino Valais Vaud | 416 117 7 2 18 54 43 134 | 95* 80 88 50 78 95 93 82 |
| *% of all listed anaesthetists | |||
| Table 2: Density of anaesthetists for each canton in 2002 and 2009. | ||||
| Year 2002 | Year 2009 | |||
| Canton | 1 anaesth / n residents n total of residents = 1792513 | n anaesth / 100000 residents | 1 anaesth / n residents n total of residents = 1946875 | n anaesth / 100000 residents |
| Geneva | 1/3535 | 28/100000 | 1/3034 | 33/100000 |
| Vaud | 1/4646 | 21/100000 | 1/3866 | 25/100000 |
| Fribourg | 1/6676 | 15/100000 | 1/6244 | 16/100000 |
| Valais | 1/8188 | 12/100000 | 1/6591 | 15/100000 |
| Neuchâtel | 1/7915 | 12/100000 | 1/6561 | 13/100000 |
| Jura | 1/9847 | 10/100000 | 1/8727 | 11/100000 |
| Total | 1/5136 | 19.4/100000 | 1/4375 | 22.8/100000 |
| Table 3: Anaesthetists characteristics & working conditions in 2002 and 2009. | |||||
| Variables | Year 2002 n (%) | Year 2009 n (%) | OR 95% CI | p value | |
| Age | ≤35 y 36–55 y >55 y | 73 (23) 209 (66) 34 (11) | 97 (24) 254 (62) 56 (14) | 1.0 0.92 (0.65–1.32) 1.25 (0.74–2.11) | 0.43 |
| Gender | Female Male | 113 (35) 206 (65) | 171 (42) 239 (58) | 1.0 1.32 (0.98–1.79) | 0.06 |
| Nationality | Swiss European Others | 282 (89) 32 (10) 4 (1) | 338 (81) 69 (17) 6 (2) | 1.0 1.79 (1.11–2.81) 1.25 (0.35–4.74) | 0.03 |
| FMH* | No Yes | 115 (36) 202 (64) | 109 (28) 288 (72) | 1.0 1.50 (1.09–2.06) | 0.01 |
| Hospital type | Public Private Others | 236 (74) 68 (21) 15 (5) | 316 (77) 92 (22) 2(1) | 1.0 1.04 (0.73–1.49) 0.50 (0.22–1.14) | 0.23 |
| Activity | Specialist anaesthetist Sub-specialist anaesthetist | 283 (89) 35 (11) | 345 (83) 63 (17) | 1.0 0.67 (0.43–1.05) | 0.08 |
| Working hours/week | <50 H 51–69 H >69 H | 68 (25) 159 (57) 51 (18) | 187 (49) 161 (42) 41 (9) | 1.0 0.36 (0.25–0.52) 0.29 (0.17–0.48) | <0.001 |
| Working hours / hospital type, mean (SD) | Public Private | 59 (12) 49 (19) | 53 (11) 50 (16) | Not applicable | <0.001 0.46 |
| Age of retirement desired | Mean (SD) | 60 (2.9) | 61 (3.1) | Not applicable | 0.02 |
| *Federatio Medicorum Helveticum ‒ Swiss Medical Association | |||||
| Table 4: Job satisfaction evaluated in 2009, compared to 10 years ago. | ||||||
| Much worse | Much better | |||||
| n | n (%) | |||||
| 1. The quality of care you are currently able to provide compared to 10 years ago | 301 | 4 (1.3) | 37 (12.3) | 67 (22.3) | 131 (43.5) | 62 (20.6) |
| 2. Your relationship with your patients compared to 10 years ago | 299 | 1 (0.3) | 35 (11.7) | 145 (48.5) | 81 (27.1) | 37 (12.4) |
| 3. Your relationship with your colleagues (physicians/non physicians) compared to 10 years ago | 301 | 3 (1.0) | 32 (10.6) | 143 (47.5) | 89 (29.6) | 34 (11.3) |
| 4. Respect you receive as a physician Your relationship with your patients compared to 10 years ago | 301 | 15 (5.0) | 69 (22.9) | 135 (44.9) | 53 (17.6) | 29 (9.6) |
| 5. Your income compared to 10 years ago | 302 | 15 (5.0) | 77 (25.5) | 73 (24.2) | 89 (29.5) | 48 (15.8) |
| 6. Your workload compared to 10 years ago | 301 | 16 (5.3) | 82 (27.2) | 69 (22.9) | 106 (35.2) | 28 (9.4) |
| 7. Your satisfaction at work compared to 10 years ago | 302 | 3 (1.0) | 50 (16.6) | 114 (37.7) | 101 (33.4) | 34 (11.3) |
| 8. Your overall current situation compared to 10 years ago | 301 | 2 (0.7) | 41 (13.6) | 75 (24.9) | 142 (47.2) | 41 (13.6) |
| Table 5: Impact of licences restriction on physicians‘ future projects by type of hospital. | ||
| No impact on future projects n (%) | Impact on future projects n (%) | |
| University hospital n = 156 | 139 (89.1) | 17 (10.9) |
| Regional hospital n = 150 | 125 (83.3) | 25 (16.7) |
| Private hospital n = 91 | 84 (92.3) | 7 (7.7) |
| Independent n = 2 | 2 (100) | |
| p = 0.17 ‒ Chi square test for difference by type of hospital | ||
The different Swiss healthcare costs containment policies implemented since 2002 have had very little impact on anaesthetists’ density, working conditions and satisfaction in the French and Italian speaking parts of the country. Rather than a decrease in the number of practicing anaesthetists, an overall increase of 12% since 2002 could be observed. This increase was particularly important in cantons with teaching hospitals and University Hospitals such as Geneva and Vaud. Furthermore, these policies and more specifically the restriction on the number of physicians licensed for reimbursement under the compulsory health insurance had, for the moment, no impact on satisfaction either. The majority of anaesthetists surveyed (87.7%) answered that these new laws had no influence on their plans for the future. They were even, on average, more satisfied than 10 years ago.
These results are in line with findings from other studies assessing the current status and impact of quotas of medical students in universities, and regulation of physicians’ locations in OCDE countries [17, 18]. Nearly all these countries regulate the number of medical graduates and Germany, Austria, Denmark, Italy, Norway, Mexico, Turkey and Hungary restrict physicians in the location of their practice. In none of these countries, including Switzerland, does there seem to be a high correlation between these measures and a shortage of medical supply [17, 18]. This suggests that medical workforce supply and shortage do not exclusively rely on the number of medical graduates supply or the freedom of practice location for physicians. Many other factors seem to impact on medical workforce supply and shortage. One of them is migration. An increasing number of countries rely on foreign medical workforce and Switzerland is no exception. A recent report from the Swiss Science and Technology Council showed that 12% of physicians in Switzerland were of foreign origin in 2000 [19]. In 2007, they represented 29% of the medical workforce. More specifically in anaesthesia, the proportion of anaesthetists of foreign origin in Switzerland was 14% in 2004, with most coming from Germany or new member states of the European Union [13]. In the French and Italian speaking parts of the country, as demonstrated in the current study, this proportion increased from 11% in 2002 to 19% in 2009. This phenomenon has been enhanced by the pressing demand for care. In Switzerland, there has been an overall increase of 35% in the number of surgical procedures (inpatient and outpatient) per capita performed since 2002. This has happened despite a significant reduction in the number of beds available in Swiss hospitals. To fulfil demand, both public and private hospitals have increased turnover from 33.8 patients per bed/year to 42.1 patients per bed/year and have adjusted their workforce accordingly. There has been an increase of overall hospital workforce from 141474 workers in 2001 to 161160 in 2008, including operating theatre staff and anaesthesia staff [2, 3]. When Swiss trained physicians were not available, other countries have been able to provide staff for operating theatres and hospitals (nurses, physicians, technicians). Thus, to compensate for poor or mistaken medical workforce planning, many western European countries manage to adapt their workforce to the increasing demand for care by recruiting physicians trained in foreign countries. However, recruiting doctors from countries that have the greatest need of physicians and particularly anaesthesiologists is, in the long run, ethically difficult to justify [13]. Furthermore, relying on foreign medical workforce to offset the increasing demand for surgical and anaesthetic procedures is a dangerous game: many other European countries are also facing a medical workforce shortage, particularly in anaesthesia [12]. To keep their physicians practicing inside the country, a number of European states may increase salaries. As a result, Switzerland may become less attractive and a serious shortage of anaesthetists may become very likely. The second phenomenon explaining the apparent absence of impact of cost containment policies on the anaesthesia workforce in the French and Italian parts of Switzerland is the variability between cantons on how restrictions on workforce are put in place. For instance if Bern, Basel, Fribourg and Zurich apply a strict “numerus clausus” in their universities, Geneva, Lausanne and Neuchâtel remain more liberal. The same is true for the decrees limiting the number of physicians licensed for reimbursement under the compulsory health insurance scheme. Furthermore, this decree has been primarily designed to limit the number of physicians working in ambulatory care and the private sector. Since the majority of anaesthetists are employed in public hospitals, the impact of these decrees on the number of practicing anaesthetists is likely to be very weak. The third reason might be the delay between the introduction of numerous clauses at university entry and the potential impact on medical workforce density, after six to seven years of medical studies. Finally, a fourth phenomenon explaining our study findings is the introduction in 2004 of working hours regulation for physicians in training in Swiss hospitals. For trainees, the overall working hours is limited to 50 hours a week.
As physicians in training deliver care under supervision, they participate to the workforce and contribute to the provision of care to the population, including in anaesthesia. The reduction of working hours has resulted in an increased need of medical workforce to complete clinical tasks and duties in hospitals. This is likely to have counteracted initiatives to limit the number of practicing physicians in Switzerland.
Another interesting finding of the current study was that satisfaction has increased compared to the 10 previous years. Cost containment policies and workforce restrictions do not seem to have had any impact on the overall level of satisfaction of anaesthetists. These results are in contradiction with other studies on this topic and studies performed in other European countries, which show that dissatisfaction is increasing among physicians regardless of their specialty [20–22]. The main reasons for dissatisfaction seem to be diminished prestige, diminished autonomy of the medical profession imposed by health care systems and a low income in regards to the high level of workload associated with clinical work. Similarly in Switzerland, Buddeberg-Fischer et al. analysed a cohort of Swiss physicians over a follow up period of 8 years, and found a significant level of chronic stress among young physicians associated to an increased risk of life dissatisfaction and burnout [23, 24]. In our study, the level of satisfaction of anaesthetists was particularly high in the area of quality of care which they were able to provide (more than 60% rated it as rather better than in the previous 10 years). One explanation is the technical progress in anaesthesia medication and monitoring leading to better patient care. Another explanation is that anaesthetists, as opposed to others specialties, face an increased administrative workload to a lesser extent than physicians. When analysing questionnaire results on workload, the answers tend to be neutral. Although a quarter of participating anaesthetists are younger than 35 and belong to the “Y generation” known to consider family and leisure time as important, this does not seem to impact on study results [25]. This is probably because these physicians, born after 1980 and having a practice of less than 10 years, could not answer the questions about satisfaction.These results are particularly surprising as working hours in Switzerland are much higher than in other European countries. In the current study, the average working time was 53 hours/week. In comparison in Germany, the average working time is 48 hours/week and in Norway it is 38 hours/week, in agreement with the EU Working-Time Directive limiting clinical work to a maximum of 48 hours/week [26].One explanation is a memory bias, as participants were asked about their satisfaction from 10 years earlier. Study findings on this topic may lack some level of precision.
The main objective of cost containment policies is to control costs by regulating access to care and increasing healthcare system efficiency. However, if these policies are maintained for too long a period or become too restrictive, a significant reduction in the quality of care provided, associated with an increased workload for physician and dissatisfaction for patients can be expected. This does not yet seem to be the case for anaesthesia care in the Latin part of Switzerland. However, projections of the future needs of an ageing Swiss population and the increasing reliance on a foreign medical workforce strongly suggest that these policies will not be sustainable in the long run.
The current study has several limitations. Firstly, we performed a cross-sectional survey and despite comparisons with a previous similar survey, our results provide only time-limited results and possible causal relationships are only hypothesised from which we cannot draw definitive conclusions. Secondly, although the level of participation was high (82%), we did not get answers from all participants and the non-responders could possibly have influenced study results. Thirdly, for the assessment of satisfaction we used self-reported rating scales, which are possibly subject to measurement errors. Furthermore, participating anaesthetists, despite anonymisation of the questionnaire, may have given socially or professionally acceptable answers: the so-called “social desirability” bias. Finally, we did not include anaesthetists working in ICU care and lacked information on this category of professionals. Despite these limitations, the present study is the first study to investigate the impact of cost containment and workforce restrictions policies in a large sample of anaesthetists in the French and Italian speaking parts of Switzerland. Future studies should explore this problem in other specialties and in the German-speaking part of the country, and a national survey should be conducted to answer this question with certainty.
Due to the progressive aging of the Swiss population, there is an increasing demand for anaesthesia and surgical care. In parallel, a number of implicit rationing policies have been introduced by the Confederation and the cantons to limit healthcare costs. These policies seem to have had no impact on anaesthetists’ workforce density, working conditions and overall satisfaction in the French and Italian speaking parts of Switzerland. This is partly due to an increase in the number of non-Swiss anaesthetists, variability between cantons in the application of cost containment policies and the concomitant introduction of working hour regulations for trainees. This opens the question as to whether these policies should be maintained and will be sustainable in the long term.
1 Office Fédéral de la Statistique. Annuaire statistique de la Suisse 2004, Zürich: Neue Zürcher Verlag, 2004.
2 OFS, «Coûts du système de santé et démographie: Coûts détaillés par âge en 2002 et évolution sur la période 1985–2020», Rapport technique, Neuchâtel: Office fédéral de la statistique, 2005a.
3 Organisation for Economic Co-Operation and Development. OECD Health Data 2010. Available at http://www.oecd-ilibrary.org/. Accessed November 5 2010.
4 Santos-Eggimann B. Is there evidence of implicit rationing in the Swiss Healthcare system. Final report to the Swiss Federal Office of Public Health / OFAS Ko/02 VW 625.
5 Petit-Pierre M-C-. La question du rationnement des soins devient toujours plus pertinente. Le Temps 1998;17 dec:12.
6 Brunner HH. Structure tarifaire uniforme: Compte rendu sur le projet GRAT INFRA I. Bulletin des médecins suisses 1999;80(5):243–6.
7 OFS, «Statistique des hôpitaux 1997–2000»: Evolution du nombre de lits, du nombre de cas et de la durée moyenne de séjour sur la base de la statistique des hôpitaux de l’OFS. Rapport technique, Neuchâtel: Office fédéral de la statistique, 2003a.
8 OFS, «Coût de la santé en Suisse»: Evolution de 1960 à 2000. Rapport technique, Neuchâtel: Office fédéral de la statistique, 2003a.
9 Législation fédérale. Ordonnance RS 832.103 Ordonnance sur la limitation de l’admission des fournisseurs de prestations à pratiquer à la charge de l’assurance-maladie obligatoire. Available at http://www.admin.ch/ch/f/rs/832_103/index.html. Accessed 20 December 2010.
10 Hänsgen K-D, Spicher B. Numerus Clausus: le «test d’aptitudes pour les études de médecine» (AMS) permet-il de trouver les personnes les plus aptes? Bulletin des médecins suisses; 2002.
11 Dorsey ER, Jarjoura D, Rutecki GW. Influence of controllable lifestyle on recent trends in specialty choice by US medical students. JAMA. 2003;290(9):1173–8.
12 Gautier JF, N’Guyen JL, Soltner C, Beydon L. French residents in anaesthesia and critical care – a nationwide survey. Ann Fr Anesth Reanim. 2004;23(8):794–8.
13 Egger Halbeis CB, Cvachovec K, Scherpereel P, Mellin-Olsen J, Drobnik L, Sondore A. Anaesthesia workforce in Europe. Eur J Anaesthesiol. 2007;24:991–1007.
14 Mamie C, Meyer P-A, Crettenand B, Morabia A, Clergue F. Evolution prévisible des effectifs médico-infirmiers en anesthésie en Suisse romande. Revue Médicale Suisse. 2004;491:1–9.
15 Thomas CB. Observations on some possible precursors of essential hypertension and coronary artery disease. Bull Johns Hopkins Hosp. 1951;89:419–41.
16 Deom M, Agoritsas T, Bovier PA, Perneger TV. What doctors think about the impact of managed care tools on quality of care, costs, autonomy, and relations with patients. BMC Health Serv Res. 2010;7;10:331.
17 Simoens S, Hurst J. OECD Publishing Services .The Supply of Physician Services in OECD Countries. OECD Health Working Papers 2006: 21.
18 Paris V, Devaux M, Wei L. OECD Publishing Services. Health Systems Institutional Characteristics: A Survey of 29 OECD Countries. OECD Health Working Papers 2010: 50.
19 Conseil Suisse de la Science et de la Technologie. Démographie médicale et réforme de la formation professionnelle des médecins; 2007.
Funding / potential competing interests: Dr Guy Haller is a holder of a postgraduate research scholarship from the University of Geneva. No other potential conflict of interest relevant to this article was reported.