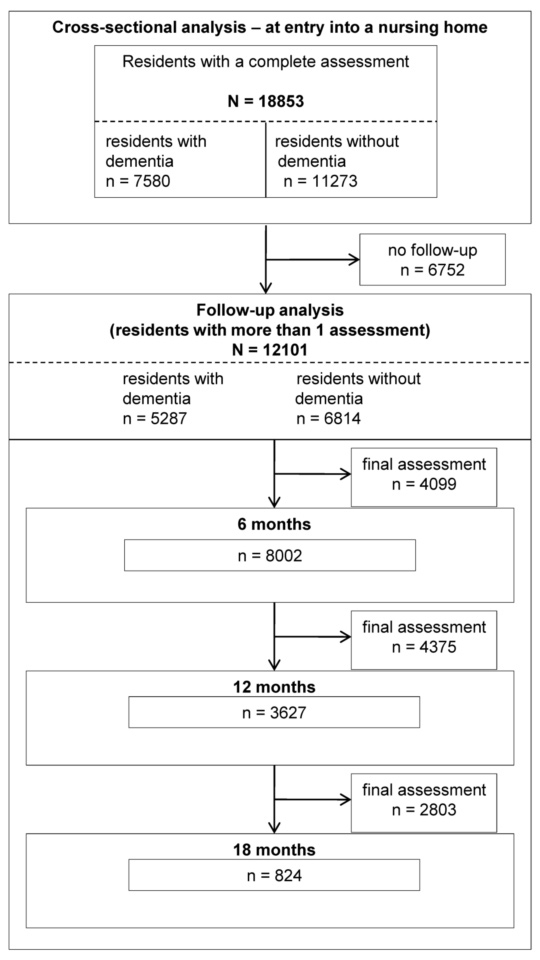
Figure 1 shows the flow chart with the number of residents assessed at entry and during follow-up.
DOI: https://doi.org/10.4414/smw.2011.13254
Mental illness is common in nursing homes. Studies have suggested that 50–70% of the residents suffer from dementia [1] and more than 40% suffer from depressive disorders, which often remain undiagnosed [2]. Common co-morbidities of dementia are behavioural and psychological symptoms (BPSD) which are observed in almost 90% of nursing home residents during the progression of disease [3, 4]. They include aggressive and inappropriate behaviours, wandering, agitation, anxiety, depressive mood, delusions and hallucinations [5]. They are difficult to treat and are a common reason for the high prescription rate of psychotropic medication in nursing home residents with dementia [6–8].
In studies across Europe, most residents (50–80%) of nursing and other care homes, particularly those with dementia, take at least one psychotropic medication, mainly antipsychotics [9–13]. A cross-national study found that antipsychotics were more commonly prescribed in Swiss nursing homes (35.9%) compared to Canadian nursing homes (32.9%) [8] and this trend has been confirmed in another study showing higher prescription rates in Switzerland than in Northern America or China [14]. The reasons for the differences are not entirely understood, but they may be in part related to different treatment standards or to different access to treatment. It has been suggested that the prescription of antipsychotics in nursing homes can be reduced by practice recommendations [15], by specialised pharmaceutical support [16] or with regular reviews or educational interventions [17].
There is converging evidence that antipsychotic use can be associated with serious risks in patients with dementia. Antipsychotics seem to contribute to a more rapid progression of dementia [18], to higher rates of cerebrovascular events [19, 20] and to increased mortality [21, 22]. Further side effects of antipsychotics include sedation and dizziness, which may lead to falls and fractures [23, 24]. Despite these risks, antipsychotics are sometimes unavoidable when non-pharmacological interventions have not been effective [25]. In such difficult clinical situations, potential side effects of antipsychotics need to be carefully weighed against potential benefits [26]. A systematic review suggested that there is no evidence for the long term use of antipsychotics in the management of BPSD [27] and recent clinical guidance suggests that antipsychotics should not be the first line treatment for BPSD and, if unavoidable, the duration of treatment should be kept to the lowest effective dose and for the shortest duration possible [15, 28].
Here, we studied psychotropic medication use in a large sample of Swiss nursing home residents at baseline and during follow-up. We compared the prescription of different psychotropic medication (antipsychotics, antidepressants, anxiolytics and hypnotics) in residents without and with dementia and hypothesised that psychotropic medication use is highest in residents with dementia, especially for those with BPSD. Furthermore, we anticipated that the prescription of antipsychotics is still rather continuous (i.e. longer than 6 months) despite other treatment recommendations.
The nursing homes in the Swiss cantons of Aargau, Basel-City and Solothurn (representing 13.5% of the Swiss population) use the Resident Assessment Instrument Minimum Data Set (RAI-MDS) for quality control and to assess functional status or care needs [29]. Assessments are done by trained nursing home staff. Residents are assessed at entry and regularly at least every six months during follow-up. Of 160 nursing homes invited to contribute their RAI-MDS data, 90 homes agreed to provide their data for our research, under the condition that the data was transferred anonymously and that no reference was made to a specific nursing home or resident. The majority of nursing homes contributing their data are run and owned by the community and are non-profit organisations. They offer care for approximately 50 to 80 residents. The company (Q-Sys AG: http://www.qsys.ch) pooling the RAI-MDS data in Switzerland offered to be the intermediary organisation between the nursing homes and the research team to guarantee anonymity. As the data were acquired for quality control and were anonymised, the ethical review board felt that no ethical permission was needed in order to analyse them. The original sample included 21821 residents who lived in nursing homes during the time period from 1997 to 2007. The analysis of another study focussing on delirium in nursing homes was also done within the sample [30]. For the current study, only residents with a complete baseline assessment during this ten year period were included for the cross-sectional analysis (n = 18853) and those with at least one follow-up assessment were included for the follow-up analysis (n = 12101). The flow chart of the study is summarised in figure 1.
The data of the Swiss version of RAI-MDS, Version 2.0 1996 [29, 31] was prospectively collected by Q-Sys AG and was provided to us for retrospective analysis. RAI-MDS was developed by the US Institute of Medicine in 1986 for quality control. It has become the most widely used instrument to assess the functional status and care needs in nursing homes in Europe and Northern America. It includes more than 300 individual items and 18 major problem areas associated with nursing home residents, such as medication group, delirium, communication, falls, psychosocial well-being and cognitive loss. Information is collected by observations of nursing home staff and interviews with residents, relatives or doctors in charge of the residents. The RAI-MDS is also regularly used for research studies [32].
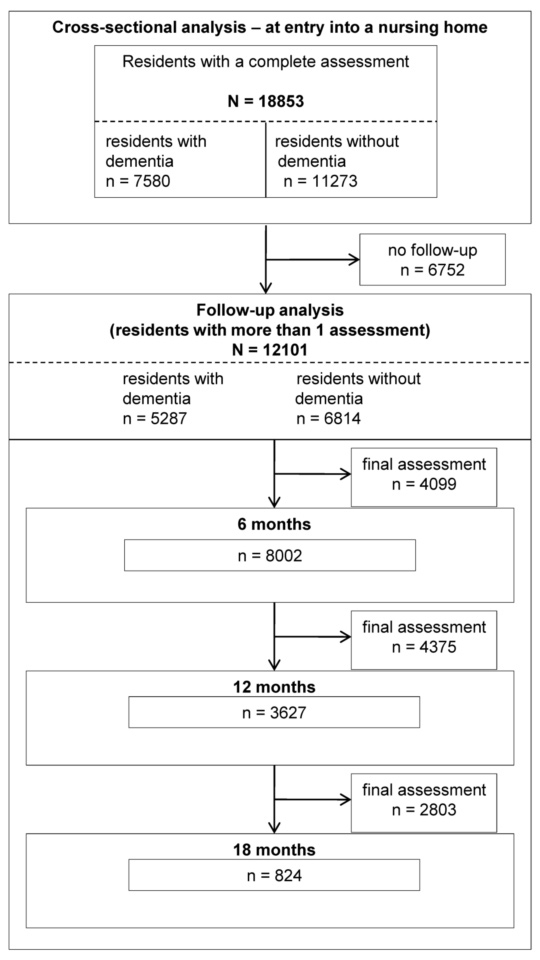
Figure 1 shows the flow chart with the number of residents assessed at entry and during follow-up.
For this study the following variables were included: gender (male, female), age (years), living alone pre-admission (no, yes). Dementia was recorded as present or absent in the medical diagnosis section of RAI-MDS with no further aetiological differentiation. All medical diagnoses were made by the physicians in charge of the resident following the usual International Classification of Diseases (ICD-10) diagnostic criteria (http://www.who.int/whosis/icd10). The item “affective disorders” included anxiety, depression and bipolar disorders. Diagnosis was based on ICD-10 and was recorded as either present or absent. Affective disorders were considered to be present if at least one affective disorder was present. The item “behavioural disturbances” was assessed according to the observations of the trained nurses in charge of the resident and included the frequency of wandering, verbal and physical aggression, socially disruptive behaviours and resistance to care. Behavioural disturbances were considered to be either present or absent, if at least one of the five items was present.
The use of antipsychotics, antidepressants, anxiolytics and hypnotics were recorded as psychotropic medication in the medication section of RAI-MDS. All medication groups were categorised as present or absent but no recording was made about the name or dosage of a specific medication. Continuous users were residents who had taken antipsychotics or antidepressants at entry and throughout all follow-up assessments. Intermittent users had the psychotropic medication at entry with interruptions during follow-up.
Data were analysed with the Statistical Package for Social Sciences (Version 17.0). Categorical data were analysed with Pearson chi-square tests and independent sample t-tests were used for numerical variables. All p-values were two tailed and the minimal significance level was set at p ≤0.001 to account for the large sample size and for multiple testing. A log-linear analysis was used to assess predictions of categorical variables (e.g. whether dementia and antipsychotic use at entry predict the use of antipsychotics at follow-up). It is an extension of the chi-square test and allows analysis of complex contingency tables with more than two categorical variables of interest.
Demographic and clinical characteristics of the nursing home residents at entry are summarised in table 1. Most residents were females. Residents with dementia (40.2%) were older and were less often living independently prior to the nursing home admission. Behavioural disturbances were more common in residents with dementia, unlike affective disorders which were more commonly reported in residents without dementia.
| Table 1:Residents’ characteristics. | ||||
| Residents with dementia | Residents without dementia | Odds Ratio (95% CI) | p-value | |
| Number | 7580 | 11273 | – | – |
| Females | 5134 (67.7) | 7662 (68.0) | 1.01 (0.98–1.05) | = 0.733 |
| Age [mean; ± SD] | 84.0 ± 7.8 | 82.9 ± 9.2 | – | <0.001* |
| Living alone before admission | 2870 (37.9) | 5122 (45.4) | 1.20 (1.15–1.24) | <0.001 |
| Behavioural disturbances (only) | 2874 (37.9) | 1443 (12.8) | 5.14 (4.76–5.54) | <0.001 |
| Affective disorders (only) | 923 (12.2) | 1804 (16.0) | 1.32 (1.20–1.44) | <0.001 |
| Depression | 854 (11.3) | 1693 (15.0) | 1.29 (1.18–1.41) | <0.001 |
| Anxiety disorders | 124 (1.6) | 221 (2.0) | 1.11 (1.02–1.20) | = 0.006 |
| Behavioural disturbances and affective disorders | 844 (11.1) | 478 (4.2) | 3.45 (3.01–3.95) | <0.001 |
| Numbers expressed as n (%) unless otherwise indicated * t (18851) = 7.79 | ||||
Most residents (61.3%) received psychotropic medication, and 28.4% of all residents received antipsychotics. Psychotropic medication use was highest in residents with dementia compared to residents without dementia (table 2). More than 70% of the residents with dementia took at least one psychotropic medication when entering the nursing home. A total of 49% of the residents with dementia (3718 out of 7580) had behavioural disturbances and most of them (77.7%) were on psychotropic medication. The most commonly prescribed medication in residents with dementia and behavioural disturbances were antipsychotics (57.0%) followed by antidepressants (28.5%) which were taken either solely or in combination with other psychotropic medication.
The majority of residents without dementia (55.0%) were on psychotropic medication as well, however the most commonly prescribed medications were antidepressants and not antipsychotics. This is well in line with the observation that affective disorders are also more common in residents without dementia (see for comparison table 1).
| Table 2: Psychotropic medication use at the entry assessment. | ||||
| Residents with dementia | Residents without dementia | Odds Ratio (95% CI) | p-value | |
| Number | 7580 | 11273 | – | – |
| Any psychotropic medication | 5365 (70.8) | 6203 (55.0) | 1.98 (1.86–2.11) | <0.001 |
| Any antipsychotics | 3397 (44.8) | 1958 (17.4) | 3.86 (3.62–4.13) | <0.001 |
| Any antidepressants | 2243 (29.6) | 3005 (26.7) | 1.16 (1.08–1.23) | <0.001 |
| Use of psychotropic medication | ||||
| Antipsychotics only | 1639 (21.6) | 803 (7.1) | 3.60 (3.29–3.94) | <0.001 |
| Antidepressants only | 799 (10.5) | 1245 (11.0) | 0.95 (0.86–1.04) | = 0.276 |
| Hypnotics only | 523 (6.9) | 1482 (13.1) | 1.91 (1.73–2.09) | <0.001 |
| Anxiolytics only | 174 (2.3) | 350 (3.1) | 1.14 (0.94–1.37) | = 0.001 |
| Antipsychotics and antidepressants | 653 (8.6) | 389 (3.5) | 2.64 (2.32–3.00) | <0.001 |
| Antipsychotics and hypnotics | 482 (6.4) | 296 (2.6) | 2.52 (2.17–2.92) | <0.001 |
| Antipsychotics and anxiolytics | 190 (2.5) | 126 (1.1) | 2.28 (1.81–2.85) | <0.001 |
| Antipsychotics and 2 others | 381 (5.0) | 277 (2.5) | 3.97 (2.61–6.03) | <0.001 |
| All 4 classes | 52 (0.7) | 67 (0.6) | 1.16 (0.80–1.66) | = 0.436 |
| Numbers expressed as n (%) unless otherwise indicated | ||||
There were 12’101 residents eligible for the follow-up analysis (5287 with dementia and 6814 without dementia). They had 3.1 (SD 0.9) follow-up assessments on average and the average follow-up period was 12 months. In the follow-up sample, there was no difference found with regards to age (p = 0.092), gender (p = 0.772) and other socio-demographic variables (p = 0.035) when residents with dementia were compared with those without dementia. The number of residents decreased during follow-up: 8002 residents had an assessment 6 months after entry; 3627 were assessed 12 months after entry and 824 had an assessment 18 months after entering a nursing home. During the follow-up period, 5.1% (967) of the residents were newly diagnosed with dementia.
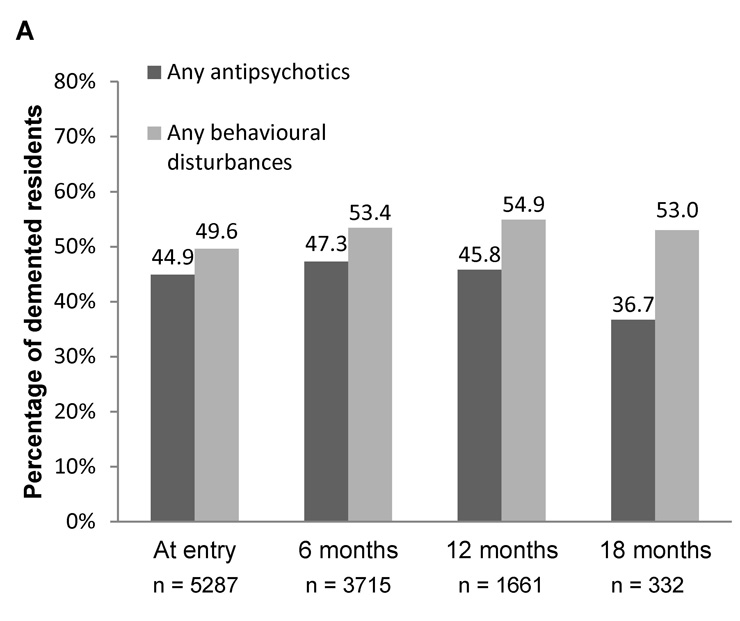
Figure 2A shows the relative number of residents with dementia on antipsychotics and with behavioural disturbances at entry and during follow-up.
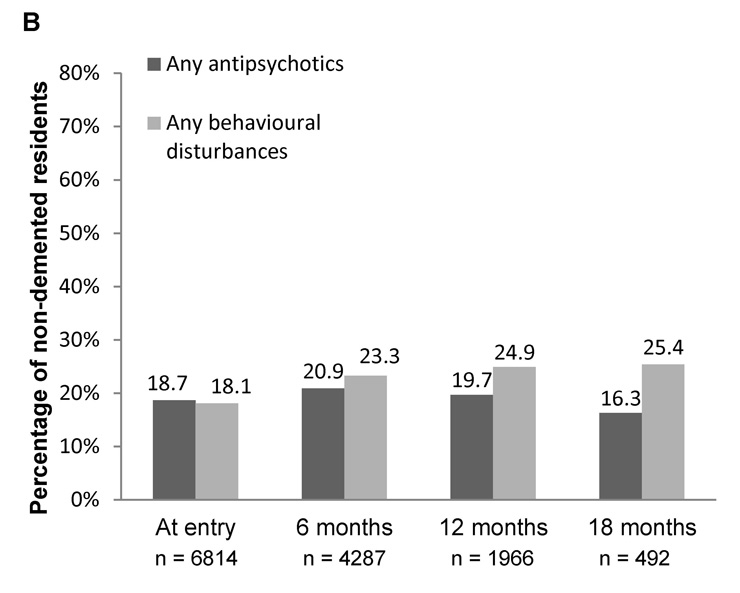
Figure 2B shows the relative number of residents without dementia on antipsychotics and with behavioural disturbances at entry and during follow-up.
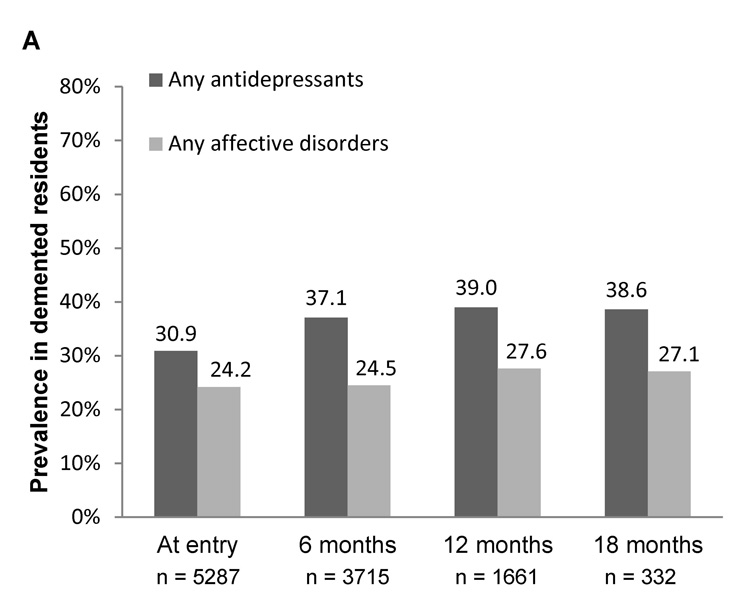
Figure 3A shows the relative number of residents with dementia on antidepressants and with affective disorders at entry and during follow-up.
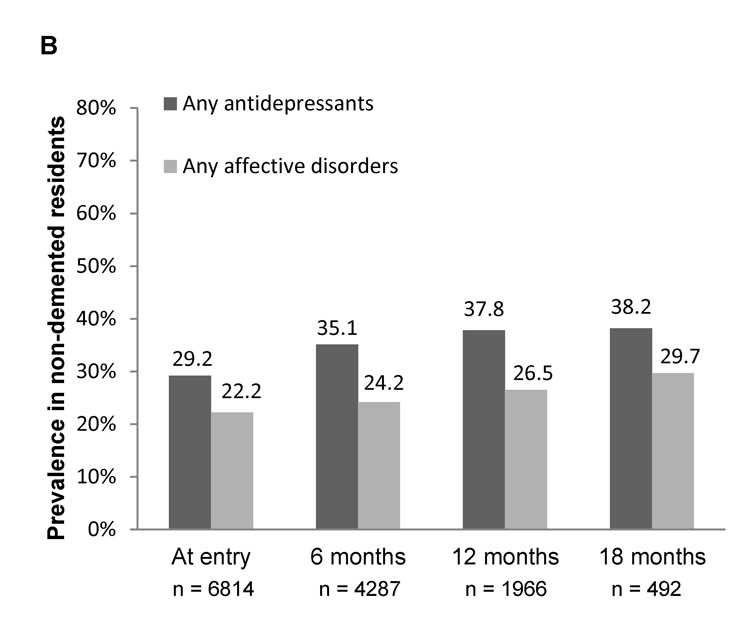
Figure 3B shows the relative number of residents without dementia on antidepressants and with affective disorders at entry and during follow-up.
Nearly half (49.6%) of the residents with dementia eligible for follow-up had behavioural disturbances and 44.9% of them received treatment with an antipsychotic at their entry assessment. The prescription of antipsychotics during follow-up was continuous in the majority (69.5%) of residents with dementia. Furthermore, results of the log-linear analysis showed that prescription of antipsychotics at entry predicted (p <0.001) the prescription of antipsychotics at the final assessment (95% CI: 2.65–3.03). A similar prediction was found for behavioural disturbances at entry. They also predicted (p <0.001) the prescription of antipsychotics after 6 months (95% CI: 2.02–2.52), after 12 months (95% CI: 2.16–2.81) and in the final assessment (95% CI: 1.89–2.37).
During the follow-up period, several residents with dementia started treatment with antipsychotics (fig. 2A): 10.7% started treatment within the first follow-up period (0 to 6 months); 6.1% started treatment in the second follow-up interval (6 to 12 months) and 5.7% started treatment in the third follow-up interval (12 to 18 months). In residents with dementia, the prevalence of behavioural disturbances increased during the first 12 months follow-up. However, the percentage of residents with dementia taking antipsychotics decreased after 12 months.
Antipsychotics were less commonly prescribed to residents without dementia (18.7% of the 6814 eligible for follow-up), and behavioural disturbances were also less common (18.1%) than in residents with dementia (see fig. 2A and 2B). The majority of the residents without dementia (60%) used antipsychotics continuously from the first to the final assessment. However, the continuous prescription rate was lower compared to the rate of residents with dementia (95% CI: 1.32–1.75, p <0.001).
Of the residents with dementia eligible for follow-up, 24.2% had affective disorders and 30.9% received antidepressants at their entry assessment. Antidepressant use at entry was also common in residents without dementia (29.2%). They were prescribed continuously for residents with dementia (66.1%) and for residents without dementia (67.8%) with no significant group differences (95% CI: 0.98–1.07; p = 0.302). The two groups were also not different with regards to the prevalence of affective disorders or the prescription of antidepressants during follow-up (see fig. 3A and 3B). In both groups, the percentages of antidepressant users increased during follow-up and the percentages of residents with affective disorders remained lower than the percentages of antidepressant users.
The current findings confirm that psychotropic medication is commonly used in Swiss nursing homes, in the cantons of Aargau, Basel-City and Solothurn. More than two thirds of the residents with dementia were on psychotropic medication, mainly antipsychotics, which were predominantly prescribed for residents with behavioural disturbances. The prescription of antipsychotics was rather continuous and their use at entry predicted their use during follow-up. This is in contrast with recent treatment recommendations suggesting that the use of antipsychotics should be restricted to clear target symptoms (i.e. severe aggression or psychosis) and prescribed for shortest duration possible [15, 28].
As in previous studies, most residents received psychotropic medication [33, 34]. Overall the use of psychotropic medication is comparable with the rates found in other European studies (50% to 80%) [9–12]. The rate in the current study was slightly lower than in a previous study in four French-speaking Swiss cantons, where 78% of the residents were taking psychotropic medication [8]. The residents in this previous study were, however, slightly older and the prevalence of dementia tended to be higher and this may explain part of the differences. The most commonly used drugs in the French-speaking cantons were hypnotics and anxiolytics, whereas in our study the most commonly used drugs were antipsychotics. These differences may be related to different approaches in the diagnosis and management of nursing home residents.
A total of 28% of all nursing home residents in the current study were taking antipsychotics and this compares well with the rates found in previous studies (22 to 34%) [14, 33, 35]. Behavioural symptoms and dementia were the main predictors of antipsychotic prescription in nursing home residents in previous research [36–38] and this was likely the case in our sample too. The rather continuous prescription of antipsychotics found here and in other studies [39] is not in agreement with treatment recommendations, which suggest that BPSD are rather transient phenomena and that the need for continuing treatment needs to be reviewed regularly every 3–6 months [28, 40–42].
This study included the RAI data from 1997 to 2007 and it is therefore likely that the warnings about the potential side effects of antipsychotics in patients with dementia, which started in 2004, has not yet affected prescription habits. Several studies have suggested that the use of antipsychotics in patients with dementia can be associated with a more rapid progression of dementia [18, 43], more cerebrovascular events [19, 20] and higher mortality [21]. Furthermore, neuroleptic sensitivity is common in dementia with Lewy bodies or Parkinson’s disease dementia [44, 45]. Risks can therefore outweigh potential benefits [46, 47] and antipsychotics should therefore not be used in general as the first line treatment for BPSD. Common reasons for prescribing them despite the risks mentioned are the lack of trained nurses to apply non-pharmacological interventions. Such interventions include cognitive stimulation, music therapy, snoezelen and other sensory stimulation for example. They can be applied either in groups or on a one-to-one basis [48]. Non-pharmacological interventions and pharmacological alternatives to antipsychotics (e.g. antidepressants, cholinesterase inhibitors, memantine and antiepileptics) should be considered for residents with dementia, before prescribing antipsychotics [49].
The number of residents treated with antidepressants was higher than the prevalence of affective disorders. This indicates possible under-diagnosis of affective disorders or that depressive symptoms in the early phase of dementia were treated but not explicitly diagnosed. Other studies have found that under-diagnosis of depression in nursing homes is common, especially in residents with dementia [50, 51]. Although depressive features were not more common in residents with dementia compared to those without, there were more demented residents treated with antidepressants during follow-up. This suggests that some residents with BPSD were treated with antidepressants, for the management of aggression, depressive features or the treatment of insomnia for example [52–54]. Switzerland currently has no national guidelines to define standards of care for people with dementia. There are however local initiatives, in the canton of Fribourg for example, which have shown that medication use in nursing homes can be reduced by practice recommendations [15] or by specialised pharmaceutical support [16].
In parallel to the strengths of the study, such as the sample size or the use of an internationally used RAI-MDS methodology, there are several limitations which need to be considered when interpreting the findings. Firstly, RAI-MDS was primarily developed for quality control. It is a nurse led instrument and the medical information (e.g. about medication) included in RAI-MDS is less detailed than one would wish for research purposes. Details about substance and dosage of medication are not recorded and this limits the interpretation of our findings to substance classes. The number of RAI-MDS assessments during follow-up was variable and no clear final assessment was done, when patients died for example. It was therefore not possible to consider death as an outcome variable. Anonymity was an important condition for the nursing homes providing their data to our research. This condition possibly increased the number of nursing homes willing to contribute their data for research, however it restricted the possibility to analyse differences between the nursing homes, which has been done in previous research [8]. As in all epidemiological studies, the method used here is less detailed than in interventional studies. However, these limitations were considered when drawing conclusions.
Psychotropic medication is commonly prescribed in Swiss nursing homes and the most commonly prescribed medications to residents with dementia were antipsychotics and antidepressants. Furthermore, the prescription of antipsychotics at entry predicted their use in the final assessment in most residents. Continuous prescription of antipsychotics for more than 6 months in residents with dementia needs to be carefully reconsidered in view of potential risks, which include neuroleptic sensitivity, death, cardiovascular events or more rapid disease progression. Recent treatment recommendations suggest that non-pharmacological interventions should be considered first for the treatment of BPSD before antipsychotics are used. If antipsychotics are prescribed for residents with dementia, their use should be restricted to treat psychosis or severe aggression and treatment should be given in the lowest effective dose for the shortest duration possible. Finally it is recommended to review the need for continued treatment regularly, every 3 to 6 months. Future research is needed to determine whether regular medication reviews and staff training are effective strategies to reduce psychotropic medication use.
Acknowledgements:The authors would like to thank the nursing home staff who administered the RAI-MDS to all the patients and the nursing homes who offered their permission to use RAI-MDS data for analyses.
1 Matthews FE, Dening T. Prevalence of dementia in institutional care. Lancet. 2002;360(9328):225–6.
2 Kramer D, Allgaier AK, Fejtkova S, Mergl R, Hegerl U. Depression in nursing homes: prevalence, recognition, and treatment. Int J Psychiatry Med. 2009;39(4):345–58.
3 Testad I, Aasland AM, Aarsland D. Prevalence and correlates of disruptive behavior in patients in Norwegian nursing homes. Int J Geriatr Psychiatry. 2007;22(9):916–21.
4 Seitz D, Purandare N, Conn D. Prevalence of psychiatric disorders among older adults in long-term care homes: a systematic review. Int Psychogeriatr. 2010;22(7):1025–39.
5 Finkel SI, Costa e Silva J, Cohen G, Miller S, Sartorius N. Behavioral and psychological signs and symptoms of dementia: a consensus statement on current knowledge and implications for research and treatment. Int Psychogeriatr. 1996;8(Suppl 3):497–500.
6 Alanen HM, Finne-Soveri H, Noro A, Leinonen E. Use of antipsychotics among nonagenarian residents in long-term institutional care in Finland. Age Ageing. 2006;35(5):508–13.
7 Snowdon J, Day S, Baker W. Current use of psychotropic medication in nursing homes. Int Psychogeriatr. 2006;18(2):241–50.
8 Gobert M, D’Hoore W. Prevalence of psychotropic drug use in nursing homes for the aged in Quebec and in the French-speaking area of Switzerland. Int J Geriatr Psychiatry. 2005;20(8):712–21.
9 Selbaek G, Kirkevold O, Engedal K. The prevalence of psychiatric symptoms and behavioural disturbances and the use of psychotropic drugs in Norwegian nursing homes. Int J Geriatr Psychiatry. 2007;22(9):843–9.
10 Hosia-Randell H, Pitkala K. Use of psychotropic drugs in elderly nursing home residents with and without dementia in Helsinki, Finland. Drugs Aging. 2005;22(9):793–800.
11 Pitkala KH, Laurila JV, Strandberg TE, Tilvis RS. Behavioral symptoms and the administration of psychotropic drugs to aged patients with dementia in nursing homes and in acute geriatric wards. Int Psychogeriatr. 2004;16(1):61–74.
12 Mann E, Kopke S, Haastert B, Pitkala K, Meyer G. Psychotropic medication use among nursing home residents in Austria: a cross-sectional study. BMC Geriatr. 2009;9:18.
13 Nijk RM, Zuidema SU, Koopmans RT. Prevalence and correlates of psychotropic drug use in Dutch nursing-home patients with dementia. Int Psychogeriatr. 2009;21(3):485–93.
14 Feng Z, Hirdes JP, Smith TF, Finne-Soveri H, Chi I, Du Pasquier JN, et al. Use of physical restraints and antipsychotic medications in nursing homes: a cross-national study. Int J Geriatr Psychiatry. 2009;24(10):1110–8.
15 Locca JF, Bula CJ, Zumbach S, Bugnon O. Pharmacological treatment of behavioral and psychological symptoms of dementia (BPSD) in nursing homes: development of practice recommendations in a Swiss canton. J Am Med Dir Assoc. 2008;9(6):439–48.
16 Locca JF, Ruggli M, Buchmann M, Huguenin J, Bugnon O. Development of pharmaceutical care services in nursing homes: practice and research in a Swiss canton. Pharm World Sci. 2009;31(2):165–73.
17 Nishtala PS, McLachlan AJ, Bell JS, Chen TF. Psychotropic prescribing in long-term care facilities: impact of medication reviews and educational interventions. Am J Geriatr Psychiatry. 2008;16(8):621–32.
18 Eggermont LH, de Vries K, Scherder EJ. Psychotropic medication use and cognition in institutionalized older adults with mild to moderate dementia. Int Psychogeriatr. 2009;21(2):286–94.
19 Douglas IJ, Smeeth L. Exposure to antipsychotics and risk of stroke: self controlled case series study. BMJ. 2008;337:a1227.
20 Rochon PA, Normand SL, Gomes T, Gill SS, Anderson GM, Melo M, et al. Antipsychotic therapy and short-term serious events in older adults with dementia. Arch Intern Med. 2008;168(10):1090–6.
21 Schneider LS, Dagerman KS, Insel P. Risk of death with atypical antipsychotic drug treatment for dementia: meta-analysis of randomized placebo-controlled trials. JAMA. 2005;294(15):1934–43.
22 Liperoti R, Onder G, Landi F, Lapane KL, Mor V, Bernabei R, et al. All-cause mortality associated with atypical and conventional antipsychotics among nursing home residents with dementia: a retrospective cohort study. J Clin Psychiatry. 2009;70(10):1340–7.
23 Hartikainen S, Lonnroos E, Louhivuori K. Medication as a risk factor for falls: critical systematic review. J Gerontol A Biol Sci Med Sci. 2007;62(10):1172–81.
24 Jalbert JJ, Eaton CB, Miller SC, Lapane KL. Antipsychotic use and the risk of hip fracture among older adults afflicted with dementia. J Am Med Dir Assoc. 2010;11(2):120–7.
25 Kong EH, Evans LK, Guevara JP. Nonpharmacological intervention for agitation in dementia: a systematic review and meta-analysis. Aging Ment Health. 2009;13(4):512–20.
26 Kozman MN, Wattis J, Curran S. Pharmacological management of behavioural and psychological disturbance in dementia. Hum Psychopharmacol. 2006;21(1):1–12.
27 Sink KM, Holden KF, Yaffe K. Pharmacological treatment of neuropsychiatric symptoms of dementia: a review of the evidence. JAMA. 2005;293(5):596–608.
28 Jeste DV, Blazer D, Casey D, Meeks T, Salzman C, Schneider L, et al. ACNP White Paper: update on use of antipsychotic drugs in elderly persons with dementia. Neuropsychopharmacology. 2008;33(5):957–70.
29 Anliker M, Bartelt G, Garms-Homolova V, Gilgen R, Staudenmeier B, Weiss U. RAI-Handbuch. Gesamtausgabe Version 2.0. St. Gallen: Q-Sys AG; 2000.
30 von Gunten A, Mosimann UP. Delirium upon admission to Swiss nursing homes: a cross-sectional study. Swiss Med Wkly. 2010;140(25-26):376–81.
31 Morris JN, Fries BE, Bernabei R, Steek K, Ikegami N, Carpenter I, et al. Long term care resident assessment instrument. User's manual version 2.0. InterRai; 1996.
32 Anliker M. Erfahrungen mit RAI in den Alters- und Pflegeheimen der Schweiz. Printernet. 2007;9(5):332–5.
33 Azermai M, Elseviers M, Petrovic M, Van Bortel L, Stichele RV. Geriatric drug utilisation of psychotropics in Belgian nursing homes. Hum Psychopharmacol. 2011.
34 Molinari V, Chiriboga D, Branch LG, Cho S, Turner K, Guo J, et al. Provision of psychopharmacological services in nursing homes. J Gerontol B Psychol Sci Soc Sci. 2010;65B(1):57–60.
35 Shah SM, Carey IM, Harris T, Dewilde S, Cook DG. Antipsychotic prescribing to older people living in care homes and the community in England and Wales. Int J Geriatr Psychiatry. 2011;26(4):423–34.
36 Nishtala PS, McLachlan AJ, Bell JS, Chen TF. Determinants of antipsychotic medication use among older people living in aged care homes in Australia. Int J Geriatr Psychiatry. 2010;25(5):449–57.
37 Alanen HM, Finne-Soveri H, Noro A, Leinonen E. Use of antipsychotic medications among elderly residents in long-term institutional care: a three-year follow-up. Int J Geriatr Psychiatry. 2006;21(3):288–95.
38 Macdonald AJ, Carpenter GI, Box O, Roberts A, Sahu S. Dementia and use of psychotropic medication in non-“Elderly Mentally Infirm” nursing homes in South East England. Age Ageing. 2002;31(1):58–64.
39 Nobili A, Pasina L, Trevisan S, Riva E, Lucca U, Tettamanti M, et al. Use and misuse of antipsychotic drugs in patients with dementia in Alzheimer special care units. International Clinical Psychopharmacology. 2009;24(2):97–104.
40 Alexopoulos GS, Streim J, Carpenter D, Docherty JP. Using antipsychotic agents in older patients. J Clin Psychiatry. 2004;65(Suppl 2):5–99; discussion 100–102; quiz 103–4.
41 Ballard C, Creese B, Corbett A, Aarsland D. Atypical antipsychotics for the treatment of behavioral and psychological symptoms in dementia, with a particular focus on longer term outcomes and mortality. Expert Opin Drug Saf. 2010.
42 Ballard C, Howard R. Neuroleptic drugs in dementia: benefits and harm. Nat Rev Neurosci. 2006;7(6):492–500.
43 Schaufele M, Bickel H, Weyerer S. Which factors influence cognitive decline in older adults suffering from dementing disorders? Int J Geriatr Psychiatry. 2002;17(11):1055–63.
44 Aarsland D, Perry R, Larsen JP, McKeith IG, O'Brien JT, Perry EK, et al. Neuroleptic sensitivity in Parkinson’s disease and parkinsonian dementias. J Clin Psychiatry. 2005;66(5):633–7.
45 Ballard C, Grace J, McKeith I, Holmes C. Neuroleptic sensitivity in dementia with Lewy bodies and Alzheimer's disease. Lancet. 1998;351(9108):1032–3.
46 Lawlor BA. Behavioral and psychological symptoms in dementia: the role of atypical antipsychotics. J Clin Psychiatry. 2004;65(Suppl 11):5–10.
47 Frank L, Kleinman L, Ciesla G, Rupnow MF, Brodaty H. The effect of risperidone on nursing burden associated with caring for patients with dementia. J Am Geriatr Soc. 2004;52(9):1449–55.
48 Livingston G, Johnston K, Katona C, Paton J, Lyketsos CG. Systematic review of psychological approaches to the management of neuropsychiatric symptoms of dementia. Am J Psychiatry. 2005;162(11):1996–2021.
49 Aupperle P. Management of aggression, agitation, and psychosis in dementia: focus on atypical antipsychotics. Am J Alzheimers Dis Other Demen. 2006;21(2):101–8.
50 Gruber-Baldini AL, Zimmerman S, Boustani M, Watson LC, Williams CS, Reed PS. Characteristics associated with depression in long-term care residents with dementia. Gerontologist. 2005;45 Spec No 1(1):50–5.
51 Cohen CI, Hyland K, Kimhy D. The utility of mandatory depression screening of dementia patients in nursing homes. Am J Psychiatry. 2003;160(11):2012–7.
52 Pollock BG, Mulsant BH, Rosen J, Mazumdar S, Blakesley RE, Houck PR, et al. A double-blind comparison of citalopram and risperidone for the treatment of behavioral and psychotic symptoms associated with dementia. Am J Geriatr Psychiatry. 2007;15(11):942–52.
53 Ballard CG, Gauthier S, Cummings JL, Brodaty H, Grossberg GT, Robert P, et al. Management of agitation and aggression associated with Alzheimer disease. Nat Rev Neurol. 2009;5(5):245–55.
54 Henry G, Williamson D, Tampi RR. Efficacy and tolerability of antidepressants in the treatment of behavioral and psychological symptoms of dementia, a literature review of evidence. Am J Alzheimers Dis Other Demen. 2011;26(3):169–83.
Funding / potential competing interests: The work was supported by the Swiss Alzheimer Association and the Swiss Society for Old Age Psychiatry. There are no conflicts of interest related to this work, be they financial or non-financial.