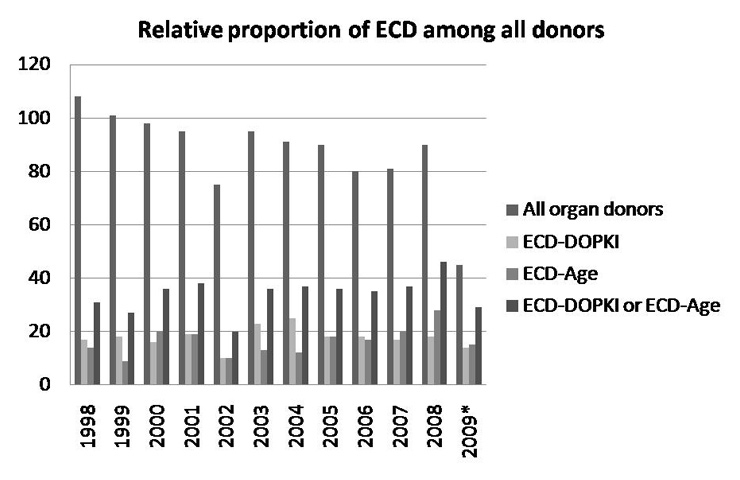
Figure 1
Relative proportion of ECD among all organ donors. Number of ECD (ECD-DOPKI, ECD-Age and ECD-DOPKI or ECD-Age) and number of all donors in Switzerland from 1998-2009. The 2009 data were available until July only.
DOI: https://doi.org/10.4414/smw.2011.13230
In Switzerland, a total of 86 brain-dead people on average have donated one or more organs for transplantation per year for the last ten years. On the other hand, more than 900 people were on the waiting list to receive an organ at the end of the year 2008. Consequently, marginal organ donors, so-called extended criteria donors (ECD), are increasingly considered to regularly expand the pool of potential donors.
We are facing a problem, in that to date there are no uniform and generally utilised criteria for the definition of ECD, and data of ECD transplantation in Switzerland are sparse. In the present study, we applied a combination of the criteria of the European consortium “Improving the Knowledge and Practices in Organ Donation” (DOPKI) [1] and advanced donor age. The DOPKI consortium was funded by the European Commission and consisted of 13 organisations representing 16 European countries, including Switzerland. They focused on improving knowledge of extended criteria organ donation, and developing a unified method for organ donation and outcome measurement, particularly with respect to safety and quality of marginal organ donation. Advanced donor age as a risk factor for transplant function has been defined by several studies [2, 3], and we added donor age ≥60 years as an additional criterion but with separate analysisfor the definition of ECD in the present study.
To increase knowledge of ECD transplantation in Switzerland, we created a database of extended criteria donation in heart, lung, liver and kidney transplantation from 1.1.1998 until 30.6.2009. Extended criteria donor transplantations were identified using DOPKI and/or advanced age ≥60 as criteria and further characterised by donor and recipient data, such as age, gender, cause of death, transplantation centre and cold ischaemia time. Once the database was created we further investigated whether transplantation using ECD affected primary organ function (PF) within the first seven days after transplantation.
This is a retrospective cohort study of brain-dead organ donors in Switzerland between 1998 and 2009 gathering epidemiological data based on chart review.
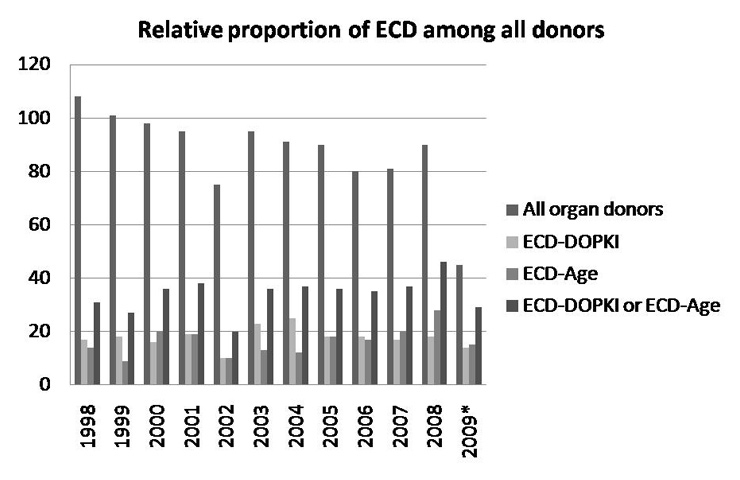
Figure 1
Relative proportion of ECD among all organ donors. Number of ECD (ECD-DOPKI, ECD-Age and ECD-DOPKI or ECD-Age) and number of all donors in Switzerland from 1998-2009. The 2009 data were available until July only.
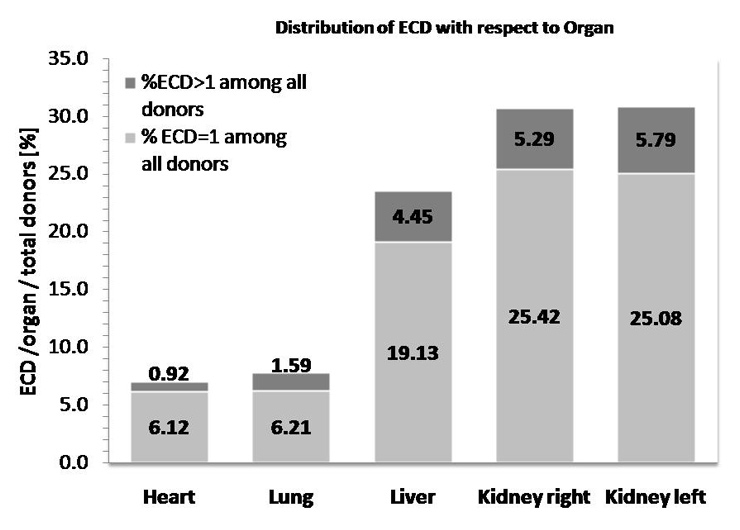
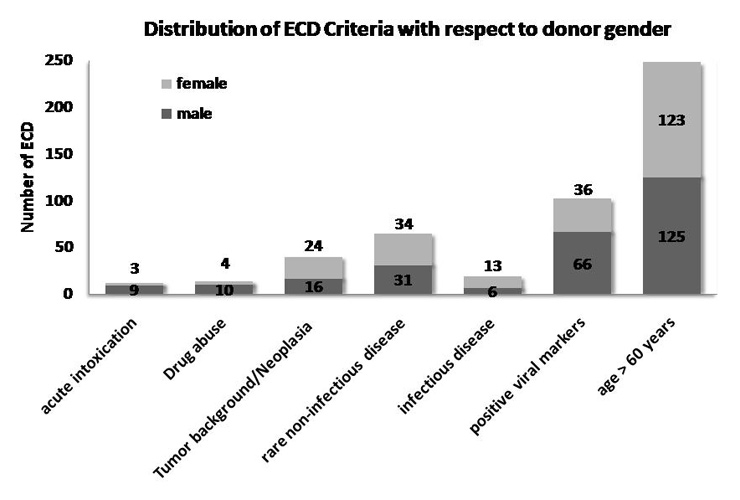
Figure 2
Relative distribution of organs from ECD with 1 and >1 fulfilled criterion in all donated hearts, lungs, livers and kidneys. Percent of ECD among all transplanted organs is shown with respect to the proportion of donors fulfilling 1 or >1 criteria (seven criteria: six DOPKI and advanced age).
Documents of all brain dead organ donors between 1.1.1998 and 30.6.2009 were analysed at “Swisstransplant”, the national donor organ allocation organisation in Switzerland. For the time period January 1998 until June 2007 respective patient data were taken from the individual patient and allocation charts. Thereafter a computerised Swiss Organ Allocation System (SOAS) was introduced, and data on transplantations from July 2007–2009 were extracted from there.
ECD represent all extended criteria donors taken together, including extended criteria donors defined by the presence of at least one of the six DOPKI criteria irrespective of age (ECD-DOPKI) or only by advanced age of ≥60 years (ECD-Age).
To be considered as ECD or ECD-DOPKI for this study, donors had to fulfil at least one of the following DOKPI criteria irrespective of age: 1. acute intoxication, 2. current neoplasia and/or positive tumour background (no current tumour or in full remission for at least 5 years), 3. rare diseases, including those of congenital or genetic origin, 4. viral markers (hepatitis B antigen [HBs Ag], anti-HBc antibodies [HBc Ab], hepatitis C antibodies [HCV Ab], lues), 5. rare infectious disease and/or 6. drug abuse [4]. DOPKI criteria conceal a strict and precise definition of the terms “rare disease” and “rare infectious disease”. In this respect, the respective diseases are not pre-defined by the DOPKI commission and their definition depends upon the judgment of the physician(s) responsible for the classification of a given organ donor.
Advanced age has been shown as a risk factor for deteriorating transplant outcome and was added as an inclusion criterion [2, 5]. We defined advanced age as donor age ≥60 years. ECD-Age represents ECD defined by advanced age without DOPKI criterion.
Amongst the ECD, inclusion criteria, age, gender, cause of death and organs donated (heart, lung, liver, kidney) were recorded. Also, cold ischaemia time and primary organ function during the first seven days after transplantation were assessed.
Partially excluded from the study were organs that were allocated to recipients living abroad due to incomplete data with respect to CIT and PF. These organs were only included for total organ counts.
Primary organ function was considered to bepresent if the transplanted organ sustained the life of the recipient or led to absence of dialysis requirement in the case of kidney transplantations. Absence of primary function (primary non-function, no-PF) included explantation, return to dialysis and recipient death.
CIT data for our reference group “all organ donors” (non-ECD + ECD) were extracted from Swisstransplant for transplantations between 2006 and 2008, as previously published [6].
Data were analysed using Excel (Microsoft Office 2007, Microsoft Inc., CA, USA). For analysis we assessed distribution and frequency of ECD criteria with respect to age and gender, and evaluated the influence of each ECD and of CIT on primary outcome. Donors donating multiple organs were analysed individually for each organ, including right and left kidney.
Descriptive statistics including frequency and distribution of DOPKI criteria, age and gender among all included donors were evaluated using GraphPad Prism. Significance of differences was analysed by ANOVA and a p-value <0.05 was considered significant.
Using SAS in a logistic regression analysis, we tested the following variables for their effect on PF or number of DOPKI criteria: donor age, recipient age, donor gender, CIT, number of DOPKI and type of DOPKI criteria; the latter two were tested with respect to PF only; PF was further tested for its effect on the number of DOPKI criteria. In a first step we analysed each variable for each organ individually. In cases with too small numbers we used the entire data-set, and subsequent stratification for organs to assess if effects were more prominent in a specific organ only. Chi-squared test with a p-value of <0.05 was used to determine whether the variable affected the outcome significantly.
During the observation period from January 1998 to July 2009, a total of 1049 organ donors were screened in Switzerland.
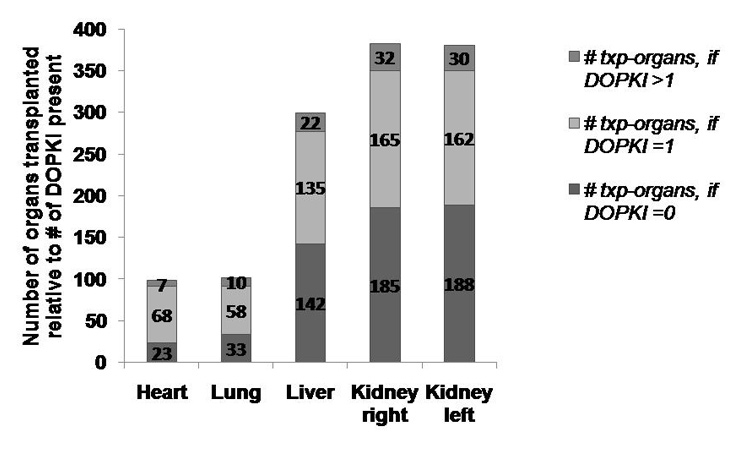
Figure 3a
Distribution of DOPKI criteria among ECD-DOPKI.
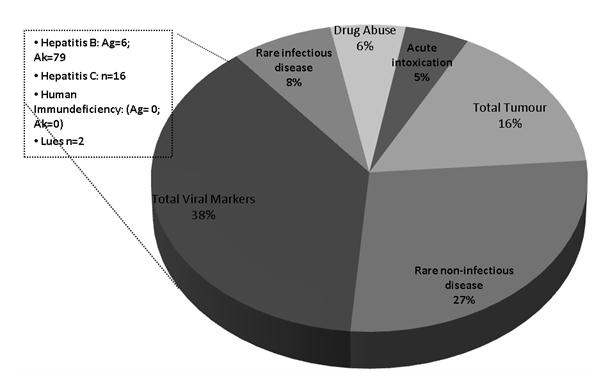
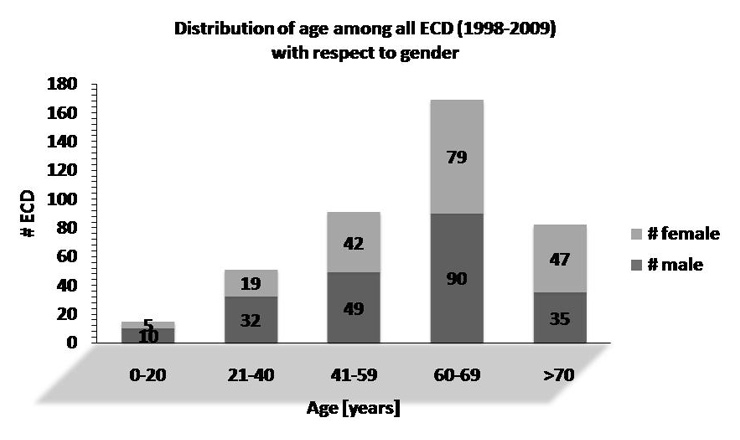
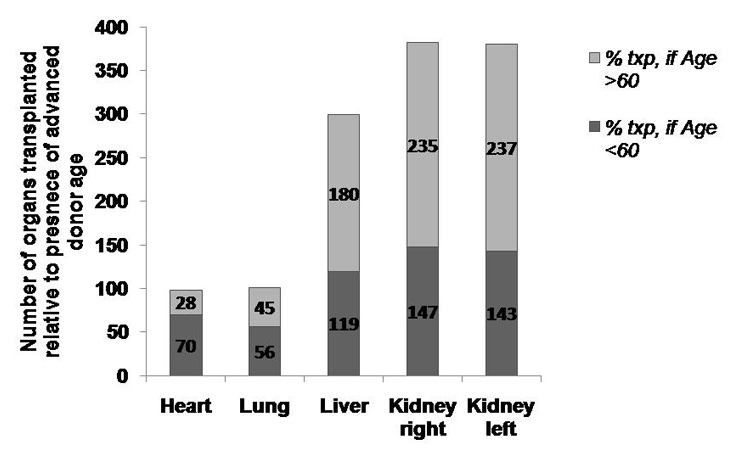
Figure 3b
Organs transplanted from ECD aged <60 y (ECD-DOPKI <60 y) and ≥60 y (ECD-DOPKI >60 years and ECD-Age). All ECD included in the study were considered, also ECD with organs transplanted abroad.
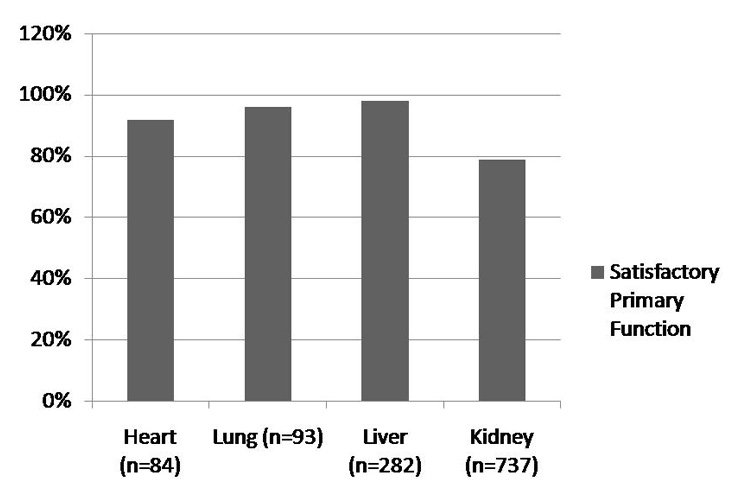
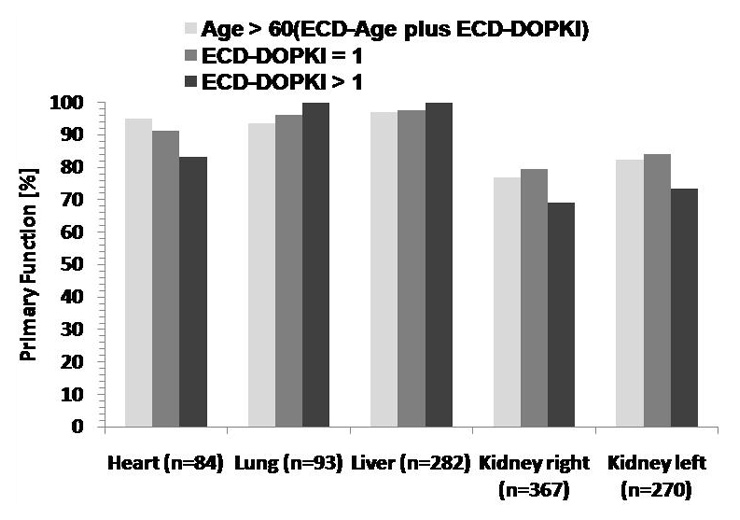
Figure 4
Primary organ function. Percentage of primary organ function in ECD with ECD ≥60 years, ECD ≥65 years and ECD ≥70 years (derived from ECD-Age and ECD-DOPKI), ECD-DOPKI=1 and ECD-DOPKI>1, separate for every organ.
A subgroup of 408 patients (39%) was classified as ECD based on DOPKI criteria and/or advanced age (≥60 years), as follows: A total of 213 donors were defined as ECD-DOPKI, including 160 donors defined according to DOPKI alone (age <60 yr) and 53 donors according to DOPKI with advanced age of ≥60 yr. In addition, a total of 195 organ donors were defined by advanced age alone (ECD-Age).
A total of 1257 organs were transplanted from these 408 ECD. Among those, 61 organs (5.2%) were transplanted into recipients living in foreign countries and were excluded from further analysiswith respect to CIT and PF. Consequently, 1196 organs remained for detailed evaluation(table 1). The relative proportion of ECD among all organ donors continuously increased during the evaluated years from 28.7% in 1998 to 64.4% in 2009 (fig. 1). Interestingly, the overall number of donors per year more or less decreased continuously from 108 in 1998 to 90 in 2008.
To assess the frequency and distribution of the sevencriteria for ECD definition, consisting of six DOPKI criteria in ECD-DOPKI and advanced age (≥60 yr) in ECD-Age, we evaluated a total of 408 donors with respect to type of organ transplanted and donor gender. The majority of donors fulfilled one ECD criterion (n = 329), followed by donors with two ECD criteria (n = 64), donors with three criteria (n = 12), and donors with four criteria (n = 3). None of the ECD presented more than four criteria. Kidney transplantations were by far the most frequent, followed by liver, lung and heart (fig. 2).
Among all ECD, advanced age was by far the most frequent criterion, followed by viral infection. ECD were almost equally distributed among male and female donors.
Considering all 408 ECD, a total of 195 donors were screened negative for DOPKI criteria and were only aged ≥60 years, forming the group of ECD-Age. The remaining total of 176 ECD-DOPKI presented 1 of the six DOPKI conditions (ECD-DOPKI = 1), and a total of 37 ECD-DOPKI showed >1 condition (ECD-DOPKI >1). We note that due to the small numbers of ECD-DOPKI with 2, 3 and 4 DOPKI criteria, we placed these in the ECD-DOPKI>1 group for further analyses.
Overall, a total of 588 organs were transplanted from ECD-DOPKI=1, and a total of 182 organs from ECD-DOPKI>1. The percentage of organs were transplanted from ECD-DOPKI>1, ranging from 7–9%. Interestingly, the relative proportion of organs transplanted from ECD-DOPKI with >1 criteria was almost equal for all organs (table 1).
Looking at each of the six DOPKI criteria in particular, the following relative frequency among ECD-DOPKI was noted: Positive viral markers (38%), rare diseases (27%), positive history of malignancy (10%; first diagnosis >5 years ago), rare infectious diseases (8%), current neoplasia (6%), oral substance abuse (6%; oral and intravenously), and acute intoxication (5%) (fig. 3a).
A total of 102 organ donors presented at least one positive viral marker, and a total of 256 organs were transplanted from this group. The following viral markers were included: hepatitis B antigen (n = 6), anti-HBc antibodies (n = 78), hepatitis C antibodies (n = 16), positive lues serology (n = 2), as well as HIV Ag and Ab (each n = 0). It is worth mentioning that in the six positive HBs Ag cases organ recipients were in all cases positive for HBs Ag too. A total of 15 ECD-DOPKI presented neoplasia at the time of inclusion (malignant and benign) and 48 organs had been transplanted from them. The two most frequent tumours of this group were astrocytoma WHO Grade I-IV (n = 6) and meningioma (n = 3). ECD-DOPKI with positive tumour background (malignant and benign; n = 25) donated 80 organs. Here the two most frequent neoplasias were breast cancer (n = 5) and skin cancer (n = 3). ECD-DOPKI with rare diseases (congenital and acquired; n = 67) donated 207 organs. Epilepsy was the most frequent rare disease (n = 21), followed by chronic inflammatory diseases and psychiatric disorders. The condition rare infectious disease was present in 20 ECD-DOPKI who donated 59 organs. Infection of the central nervous system was present in 11 cases, in 4 cases infection of the respiratory tract and in 3 cases infection with resistant bacteria (methicillin-resistant Staphylococcus aureus [MRSA] and extended spectrum beta lactamase [ESBL]). Substance abuse occurred in 14 organ donors, and a total of 44 organs were transplanted from this population. Twelve ECD-DOPKI were consuming drugs at the time of transplantation (1 intravenously) and two had a positive history of intravenous drug abuse but were off drugs for at least two years before transplantation. The following drugs were used: amphetamine, benzodiazepine, cannabis, heroin, cocaine, methadone and opiates; but in many cases more than one drug had been used at the same time. The DOPKI criterion “acute intoxication” occurred in 12 cases, including CO-intoxication (n = 4), medical-drug intoxications (opiates, benzodiazepines, paracetamol, antidepressants, antipsychotics and combinations; n = 5), substance abuse (cocaine, ecstasy; n = 1), methanol (n = 1) and sulfuric acid (n = 1). A total of 42 organs were transplanted from this group.
Overall, primary function (PF) was high in all ECD organs (ECD-DOPKI plus ECD-Age), ranging from 73% in current neoplasia to 100% in substance abuse; in between were rare infectious disease (79%), acute intoxication, positive tumour background and rare disease (88%), as well as positive viral markers (92%).
The age of all 408 ECD ranged from 1–85 years with an average of 57 years (SD ± 16). Almost two thirds of ECD were ≥60 years, and only 15 donors belonged to the group paediatric/adolescent. Among the group aged over 60 years, 67% were aged between 60–69 years (n = 169), and 33% between 70 and 85 years (n = 82).In all age groups more male donors were present, with the exception of age >70 in which there were more female donors.
Organs transplanted from donors of age ≥70 numbered 488 within the observation period. The most frequent cause of death in this group was cerebral haemorrhage, in a proportion of 38%, followed by traumatic brain injury (23%) and anoxia (11%).
From the subgroup of donors aged 60–69 years, 489 organs were transplanted. Here the most common cause of death was again cerebral haemorrhage, with 66%, followed by traumatic brain injury (14%) and cerebrovascular insult (8%). The average age was 64 years (SD ± 3).
A total of 160 ECD belonging to the group ECD-DOPKIwere aged 0–59 years with a mean of 41 years (SD ± 14). In this subgroup, 496 organs were transplanted. The most common cause of death was cerebral hemorrhage too, followed by traumatic brain injury and anoxia.
With respect to type and number of organs transplanted from donors aged 60 and over, more kidneys and more livers were transplanted from advanced age donors than from younger donors. In contrast, hearts and lungs were more often transplanted when donors were younger than 60. From a total of 98 hearts transplanted, only 28 donors were over 60. With regard to kidneys, 472 organs were transplanted from donors aged over 60 years, compared to 290 organs from donors below 60 (fig. 3c).
Among the 1260 organs transplanted from 408 extended criteria donors between 1998 and mid-2009, kidneys were transplanted most frequently, followed by livers, lungs and hearts.
A total of 64 organs were exported and transplanted in foreign institutions. Hence these organs had to be excluded from follow-up analyses with respect to CIT and PF due to lack of follow-up data (kidney n = 25, liver n = 17, lung n = 8, heart n = 14).
The average age of organ donors was between 47 years (heart) and 57 years (kidney and liver). In organ recipients the average age ranged between 49 years (lung) and 57 years (heart). In all organs the majority of donors and recipients were male.
A comparison between CIT of ECD and all brain-dead organ donors (ECD and non-ECD) is shown in table 2. There is no obvious difference between the two groups; it should be noted that we only have data from all brain-dead organ donors grouped together, not from non-ECD alone.
This outcome supports the assumption that an initial difference in organ function (within the first seven days) between ECD and all organ donors, overwhelmingly non-ECD, may be caused by the additional risk factors in ECD and not by the length of CIT.
| Table 1: Characteristics of ECD in Switzerland (1998–2009). | ||||
| Heart | Lung | Liver | Kidney | |
| ECD Tx 1998–2009 [#] | 84 | 93 | 282 | 737 |
| Mean donor age [years](ECD ± age >60 years) | 46.8 | 51.6 | 56.8 | 57.3 |
| Donor gender [%male] | 60.7 | 52.7 | 53.6 | 52.0 |
| Cause of death Cerebral haemorrhage Traumatic brain injury Suicide Anoxia Cerebrovascular insult Tumour Other | 27 27 10 7 4 3 6 | 47 18 8 2 7 4 7 | 167 43 23 15 16 6 12 | 407 127 51 55 41 14 42 |
| ECD organs per ECD category ECD-Age (age ≥60 y) ECD-DOPKI, with 1 criterion ECD-DOPKI, with >1 criterion | 20 58 6 | 32 52 9 | 134 128 22 | 368 313 56 |
| Age of ECD organs Age <60 (ECD-DOPKI) Age ≥60 (ECD-Age and ECD-DOPKI) | 59 25 | 50 43 | 111 171 | 276 461 |
| Recipient age [years] | 51.3 | 49.2 | 51.8 | 53.4 |
| Recipient gender [%male] | 75 | 55.9 | 85.2 | 62.6 |
| Gender mismatch [%] | 36 | 27 | 40 | 49 |
| Δ Age(donor vs recipient) [years] | -4.56 | 2.4 | 4.95 | 3.83 |
| Mean CIT [min] | 144.7 | 267.6 | 440.9 | 735.4 |
| Txp follow-up [%PF] | 91.7 | 95.6 | 97.9 | 80.7 |
| Table 2: Comparison between mean CIT of ECD and of all organ donors (ECD and non-ECD). | ||||
| Heart | Lung | Liver | Kidney | |
| ECD | 145 min. (45–304) | 267 min. (111–462) | 441 min. (115–848) | 735 min. (159–2040) |
| All organ donors | 171 min. (57–399) | 287 min. (84–659) | 441 min. (168–1050) | 714 min. (267–1658) |
Figure 4 shows all organs in relation to their primary function according to the criteria Age ≥60 y, Age ≥65 y and Age ≥70 y. With the exception of the heart in organ donors aged over 70, where all three recipients died, satisfying primary function was present in at least 72%. Surprisingly, a 100% satisfactory outcome was attained twice and both times the donors were aged over 70 years (lung n = 10 and liver n = 57).
The categories ECD-DOPKI>1 and ECD-DOPKI=1 showed a satisfactory primary function from 71.4% in kidney if ECD-DOPKI>1 to 100% in lung and liver in ECD-DOPKI>1. The number of achieved criteria (ECD = 1 versus ECD >1) did not influence the transplantation outcome.
A total of 77 hearts (92%) showed PF within the first seven days after transplantation; only 7 recipients (8%) died from haemorrhagic shock (n = 1), cerebrovascular bleeding (n = 1), and in five cases the cause of death was not documented. The most often present ECD criterion in the event of primary non-function was a positive history of malignancy (n = 3) and rare diseases (n = 3).
In the case of lung transplantation, 89 organs (96%) showed PF within the first seven days. Only 4 lung recipients (4%) died from haemorrhagic shock (n = 1), cardiopulmonary cause of death (n = 1) and unknown cause of death (n = 2). The present criteria in these four cases were rare disease (n = 2), age >60 yr (n = 1) and CO-intoxication (n = 1).
Satisfactory PF was present in 276 livers (98%); 6 recipients (2%) either died (septicaemia, cerebrovascular insult, liver necrosis: n = 1 each) or survived short-term with primary non-function (n = 3). In these six patients the fulfilled ECD-criteria were donor age >60 years (n = 4), positive HBc Ab (n = 1) and current neoplasia (n = 1).
Within the first seven days after kidney transplantation, 596 recipients (79%) showed primary function (PF) and 141 transplanted organs (21%) showed primary non-function with return to dialysis (n = 140, including allograft explantation in 7 cases) or recipient death (n = 1). The three most frequently fulfilled criteria in cases of pNF were: donor age >60 years (n = 46), positive viral markers with respect to HBV (HBc Ab; n = 8) and HCV (HCV Ab; n = 3), and rare disease (n = 8).
Looking at each organ independently, a comparison between the length of CIT in ECD represented by ECD-DOPKI>1, ECD-Age and ECD>1 did not show a wide difference between primary function and no-primary function within 7 days after transplantation, irrespective of the ECD type (fig. 5).
In the case of the heart (fig. 5a), 73 organs were available for calculation of CIT with a mean overall CIT of 145 min. Comparison of CIT of hearts with PF and those without PF, the average overall CIT in the second group was 22 min longer. In the group of DOPKI>1 and ECD>1, CIT was in the primary non-function category longer than in cases with primary function.
CIT of the lungs (fig. 5b) was calculated with 86 organs. In these organs, overall CIT showed a difference of 31 minutes to the disadvantage of the primary non-function group. Here it is the same situation as in the case of the hearts: CIT in the primary non-function group was longer in the categories DOPKI>1 and ECD>1.
258 livers (fig. 5c) were available for calculation of CIT; overall CIT with PF (441 min) did not greatly differ from CIT in livers without PF (434 min). In the category DOPKI>1 no organ presented primary non-function. In the remaining categories (Age >60 and ECD>1), CIT in organs with primary function was slightly longer.
A total of 432 kidneys (fig. 5d and e) were available for calculation of overall CIT. Although kidneys had the longest cold ischaemia time compared to the other organs (mean CIT = 741min.), there was no gross difference between overall CIT of kidneys with or without PF. There was little difference with respect to CIT in the three different groups.
Organ shortage remains the biggest problem in transplant medicine today. Thus, every effort should be undertaken to increase organ donation. Overall the number of cadaver organ donors per year in Switzerland has remained stable over the last eleven years with a maximum of 108 donors in 1998 and a minimum of 75 donors in 2002 (mean of 86 donors per year). However, short-term analysis since the introduction of the national transplantation law in 2007 may indicate that organ donation could be on the increase in recent years. Interestingly, the percentage of ECD among all donors has continuously increased during our observation period, but epidemiological and clinical data of these donors have never been analysed.
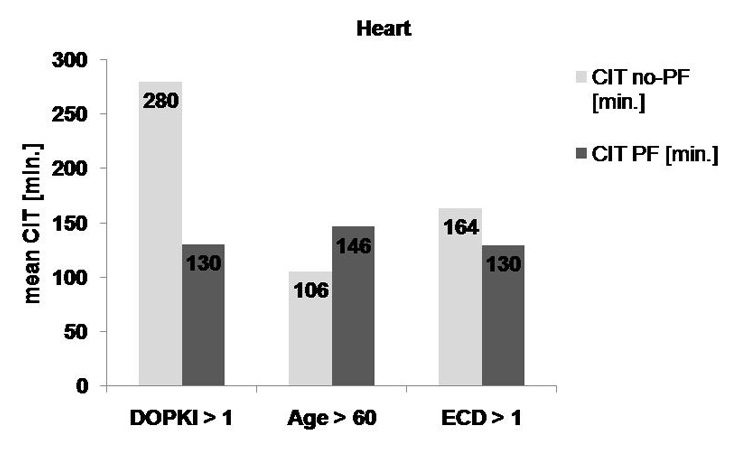
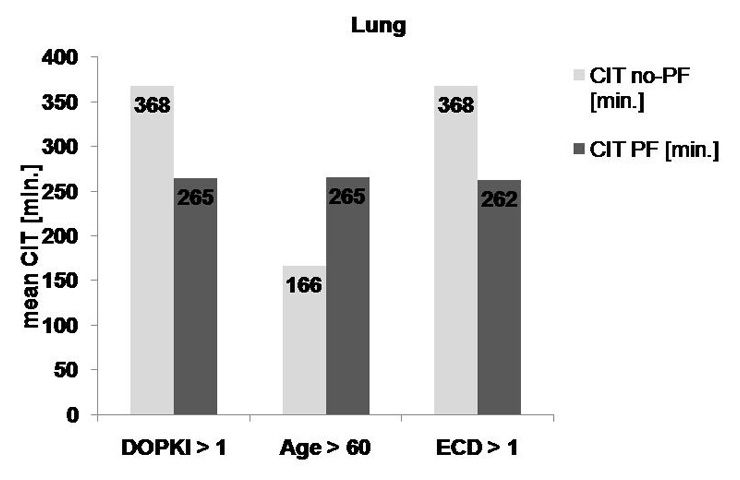
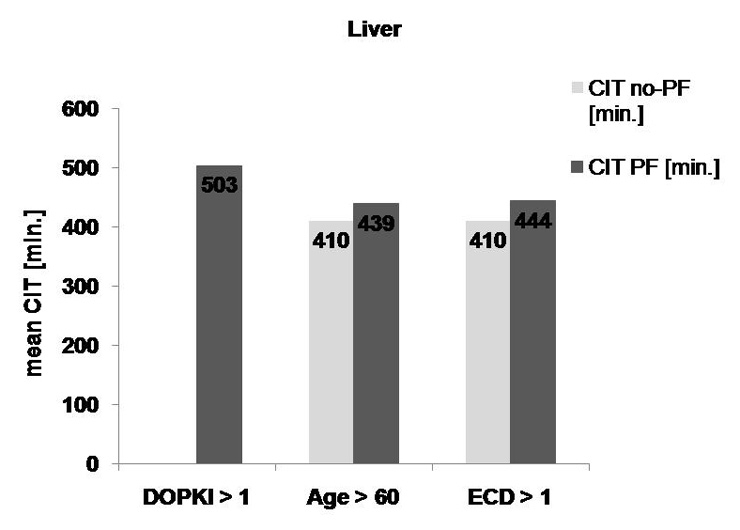
Figure 5a, 5b, 5c
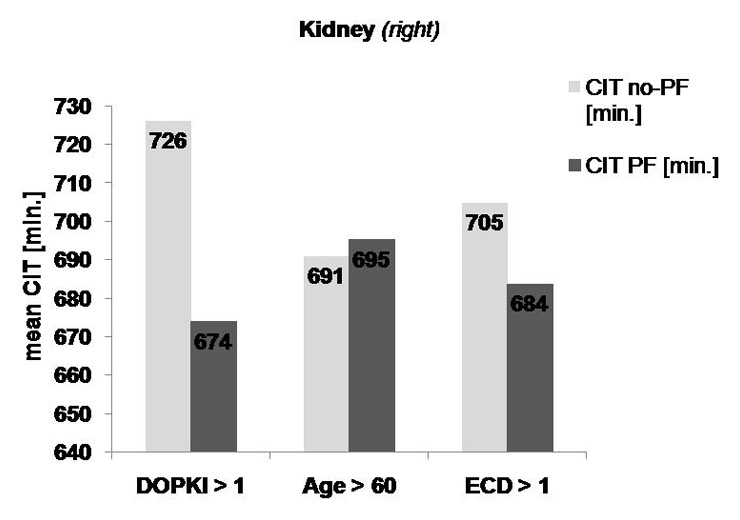
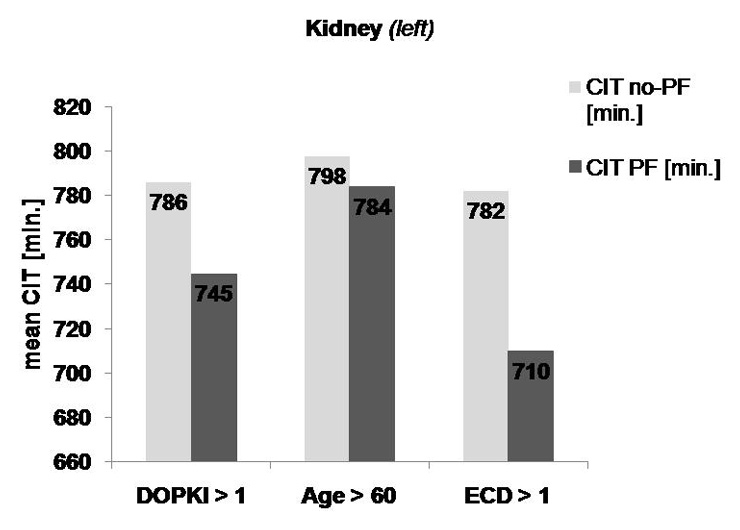
Figure 5d, 5e
Comparison of CIT in primary function and non-primary function of organs from ECD-DOPKI >1, Age ≥60 (ECD-Age) and ECD>1 (ECD-Age plus ECD-DOPKI) Heart, (b) Lung, (c) Liver, (d) Kidney right and left
In the literature different definitions of ECD exist, depending upon the type of organs transplanted. Prominent examples of organ-specific definitions of ECD are the following: Heart: Inotropic support and history of smoking [7], as well as increased donor age [4]; lungs: PaO2/FiO2 ratio less than 300 mm Hg just before procurement, pulmonary infiltrate on chest radiography or infection documented in sputum, age >55 yr, donor smoking history >20 py, or evidence of significant chest trauma [8]. Liver: Ideal donor: age <40 yr, no steatosis or other underlying chronic liver lesion andno transmissible disease [9]. Kidney: Donor age >55 yr, non-heart beating donor, cold ischaemia time >36 h, donor hypertension or diabetes mellitus >10 yr duration [1], or advanced donor age of ≥60 yr or else 50–59 yr with at least two of the following risk factors: hypertension, cerebrovascular injury, serum creatinine >1.5 mg/dL (UNOS criteria) [10].
The prime aim of our study was a survey to collect epidemiological data of ECD in Switzerland. As a member of the DOPKI-Consortium which is now included in EFRETOS (European Framework for the Evaluation of Organ Transplants; http://www.eurotransplant.org/?id=efretos ), we utilised the DOPKI definition of ECD in our survey, plus advanced donor age. Besides including various pathologies, the DOPKI criteria have the advantage of being applicable with respect to all solid organs transplanted. Advanced age was included as an additional criterion and added due to the final DOPKI report [1, 2].
To be diagnosed as an ECD, the donor needs to present one of the following six features: acute intoxication, current neoplasia or positive tumour background, rare diseases including those of congenital or genetic origin, positive viral markers (HBs Ag, HBc Ab, HCV Ab, Lues, HIV Ab and Ag), rare infectious diseases and drug abuse. Thus, we have detected a very wide spectrum of accepted ECD.
Independently of the evaluated diagnostic DOPKI criterion, the number of recipients with satisfactory primary organ function was always much larger than the group with a bad primary outcome. However, the evaluation of primary organ function within the first seven days after transplantation leads only to limited conclusions with respect to ECD because of the very limited data set in our investigation.
Furthermore, it must be borne in mind that with respect to positive viral markers and advanced donor age, only a limited number of recipients can be considered for transplantation. In particular, organs from HBs Ag-positive donors are transplanted only to HBs Ag-positive recipients and organs of donors of advanced age are generally not considered for children or very young adults. In cases of substance abuse, either at the time of study inclusion or in the past, the positive short term outcome during the first week after transplantation was 100%. However, the recipient number was relatively small and thus a definite conclusion is not possible. In the case of acute intoxication, positive tumour background (first diagnosis >5 years ago) and rare diseases, the primary outcome was satisfactory in 88% of cases. Sufficient organ function within the first seven days after transplantation was achieved in positive viral markers in 92%, by rare infectious diseases in 79% and in the case of current neoplasia in 73% of cases. In this respect, it is always important to consider the number of transplanted organs in every single risk group: substance abuse 44 organs, acute intoxication 42 organs, positive tumour background 80 organs, rare diseases 207 organs, positive viral markers 256 organs, rare infectious diseases 59 organs and current neoplasia 48 organs. Primary organ non-function in recipients of organs from donors with current neoplasia or positive tumour background was never caused by a tumour.
However, the need for dialysis will certainly diminish for many cases during a longer follow-up. Therefore, a more extensive recipient observation period is necessary to draw final conclusions with respect to the suitability of ECD kidneys.
To be able to draw significant conclusions in order to qualify ECD, a longer interval between transplantation and evaluation would be necessary. In addition, other important factors such as recipient co-morbidity, sensitisation (e.g. presence of donor-specific antibodies), immunosuppression and re-transplantation would need to be considered.
With the exception of the liver, mean cold ischaemia time (CIT) in organs with insufficient primary function was longer than in the group with satisfactory primary function. The negative effect of prolonged CIT is already known [1, 11, 12]. Whether the partial negative outcome in primary organ function is the result of longer CIT or the additional risk factors is difficult to say. However, it was apparent from our data that a larger number of achieved ECD criteria does not automatically imply a higher degree of primary organ failure. Equally, the number of ECD criteria fulfilled does not automatically imply retardation in organ allocation and transplantation. Table 2 shows the comparison of CIT of ECD and all organ donors (ECD and non-ECD). It is apparent that using the organs of ECD does not automatically imply a longer CIT.
There are several limitations to our study. First, donor documents are notoriously incomplete. For instance, it is not always stated whether tumours were malignant or benign, and there is certainly substantial underreporting, for example with respect to a history of substance abuse. Second, the DOPKI definitions of rare diseases and rare infections are somewhat arbitrary and are not clearly defined. Thus, we have included occasional ECD based on several benign lesions such as meningeoma. Hence the short term outcome in our ECD population is biased towards overly positive results. Evaluation of such criteria would exceed the scope of this study but could be evaluated in a further project.
Among all seven ECD criteria analysed, possibly only donor age and acute intoxication did influence short term survival.
In Switzerland a broad range of ECD derived organs have been transplanted in the past. Organs from such ECD may be used safely in the majority of situations with good short term outcome. However, to definitively judge outcome requires much longer recipient follow-up and many other factors need to be included into the assessment. In addition, a modified definition of ECD is needed for outcome analyses.
1 DOPKI Improving the knowledge and practices in organ donation. Final Report of Work packages; http://www.dopki.eu
2 Ojo AO, Hanson JA, Meier-Kriesche HU, Okechukwu CN, Wolfe RA, Leichtman AB, et al. Survival in Recipients of Marginal Cadaveric Donor Kidneys Compared with Other Recipients and Wait-Listed Transplant Candidates. J Am Soc Nephrol. 2001;12:589–97.
3 Blanche C, Kamlot A, Blanche DA, Kearney B, Magliato KE, Czer LSC, et al. Heart transplantation with donors fifty years of age and older. J Thorac Cardiovasc Surg. 2002;123:810–5.
4 DOPKI Improving the knowledge and practices in organ donation. Final Report of Work packages; http://www.dopki.eu
5 Topkara VK, Cheema FH, Kesavaramanujam S, Mercando ML, Forster CS, Argenziano M, et al. Effect of Donor Age on Long-Term Survival Following Cardiac Transplantation. J Card Surg. 2006;21:125–9.
6 Beyeler et al. Organs, Tissues, Cells, 2009.
7 Tsao CI, Chen RJ, Chou NK, Ko WJ, Chi NH, Yu HY, et al. The Influence of Donor Characteristics on Survival After Heart Transplantation. Transplantation Proceedings, Volume 40, Issue 8, Pages 2636–7.
8 Kawut SM, Reyentovich A, Wilt JS, Anzeck R, Lederer DJ, O’Shea MK, et al. Outcomes of extended donor lung recipients after lung transplantation. Transplantation. 2005;79(3):310–6.
9 Durand F, Renz JF, AlkoferB,Burra P, Clavien PA,Porte RJ, et al. Report of the Paris consensus meeting on expanded criteria donors in liver transplantation. Liver Transpl. 2008;14:1694–707.
10 http://www.unos.org/docs/Kidney_Brochure.pdf
11 Nickkholgh A, Weitz J, Encke J, Sauer P, Mehrabi A, Bückler MW, et al. Utilization of extended donor criteria in liver transplantation: a comprehensive review of the literature. Nephrol Dial Transplant. 2007;22(Suppl 8):viii29–viii36.
12 Orens JB, Boehler A, de Perrot M, Estenne M, Glanville AR, Keshavjee S, et al. A review of lung transplant donor acceptability criteria. J Heart Lung Transplant. 2003;22(11):1183–200.
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article was reported.