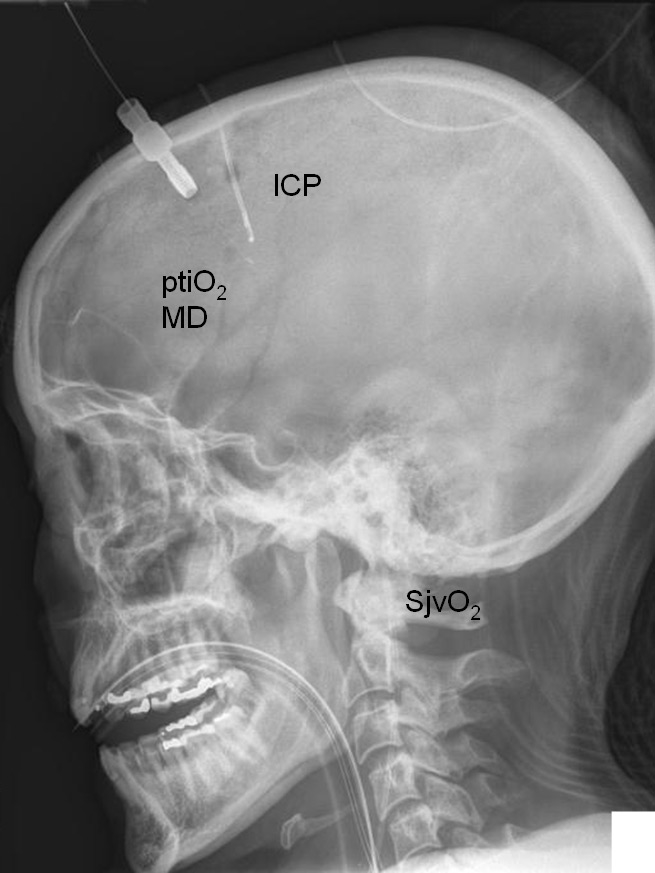
Figure 1
Illustrative lateral X- ray view showing positioning of ICP, ptiO2, microdialysis (MD), and jugular venous catheter allowing measurement of SjvO2. This allows to combine local (ptiO2, microdialysis) with global neuromonitoring (SjvO2).
DOI: https://doi.org/10.4414/smw.2011.13245
Severe traumatic brain injury (TBI) is associated with dramatic consequences for the individual patient and society, especially if persisting deficits preclude successful reintegration [1, 2]. This, in turn, leads to a tremendous socio- economic burden especially if young patients remain impaired, thereby being unable to contribute to the pension programme.
Based on the predominant vulnerability of the injured brain during the early posttraumatic phase and the fact that additional injuries during the acute and subacute phase strongly determine quality of survival, prevention of secondary insults is of utmost importance. Typical secondary insults due to hypoxia, hypotension, uncontrolled hyperventilation, hypoglycaemia as well as hypoventilation, hypertension, and hyperglycaemia must be actively looked for at all time points. Contrary to the puristic approach, the extent of additional injury cannot be assessed by relying on intracranial pressure (ICP) and cerebral perfusion pressure (CPP) alone. Extended neuromonitoring is important and may even become indispensable in contemporary intensive care treatment. Only with the help of extended neuromonitoring are we able to unmask otherwise occult signs of cerebral impairment, and most importantly, even at a normal ICP. In addition, extended neuromonitoring will allow us to fine tune quality and extent of our therapeutic interventions. Contemporary continuous basic bedside neuromonitoring consists of ICP and CPP. Extended bedside neuromonitoring comprises transcranial Doppler sonography (TCD), jugular venous oxygen saturation (SjvO2), partial tissue oxygen pressure (ptiO2), cerebral microdialysis to assess changes in cerebral metabolism (glucose, lactate, pyruvate, glutamate, glycerol), perfusion measurement, and electrophysiological studies including electrocorticography to unmask cortical spreading depression (CSD).
This review article will provide a detailed insight into neuromonitoring-guided treatment options aimed at preventing and reducing brain damage following severe TBI, focusing on the questions:
– How can we unmask cerebral impairment during pharmacological coma?
– What is the impact of extended neuromonitoring in routine intensive care?
– What is the level of evidence and what is to be expected for the future?
In clinical routine, different non-invasive and invasive monitoring methods are indispensable to unmask otherwise occult changes. Only then can we guide the type, extent and duration of specific therapeutic interventions (table 1). Based on the fact that traumatic lesions such as haemorrhages, contusions and oedema already exhibit a stereotypic growth pattern during the first hours after injury, specific neuromonitoring must be used early after TBI. It is also important to install extended neuromonitoring during phases with normal ICP <15 mm Hg during pharmacological coma allowing to unmask pathological processes and aimed at reducing progression of secondary brain damage.
The different techniques are associated with certain disadvantages summarised in table 2. Given the regional heterogeneity found under normal anatomical and physiological as well as pathological conditions a combination of parameters assessing global as well as local changes appears useful. In this context, SjvO2 reflects global changes while ptiO2 unmasks local alterations. To date, the location of the different probes is still discussed controversially. The ideal target area must be considered individually, knowing that monitoring of a normal area could result in missing episodes requiring therapeutic interventions while monitoring within a pathologic area could lead to excessive treatment possibly being less beneficial for the adjoining tissue. Furthermore, insertion of more probes which would allow assessment of dynamic changes in different regions is associated with an increased risk of additional injury, a substantial cost factor, and a certain risk of confusing the samples and values.
| Table 1:Neuromonitoring: areas of interest, implications and guidance of treatment options. | |||
| Monitoring | Area of interest | Implications | Guidance of treatment options |
| intracranial pressure (ICP) | focal/global | increase in intracranial volume and pressure | hyperventilation, blood pressure support, analgesia/sedation, body positioning, temperature |
| cerebral perfusion pressure (CPP) | global | Indirect assessment of cerebral perfusion | blood pressure support |
| SjvO2 | global | global cerebral perfusion and oxygenation | ventilation, oxygenation, CPP, analgesia/sedation, temperature, transfusion |
| ptiO2 | focal | local cerebral perfusion and oxygenation | ventilation, oxygenation, CPP, analgesia/sedation, temperature, transfusion |
| microdialysis | focal | local cerebral metabolism, perfusion, oxygenation, glucose supply, mitochondrial function glucose: glucose supply lactate: anaerobic metabolism lactate to pyruvate ratio: mitochondrial dysfunction, severe metabolic impairment glutamate: excitation glycerol: cell membrane damage | ventilation, oxygenation, CPP, analgesia/sedation, temperature, transfusion, nutritional support |
| TCD | focal | cerebral perfusion: low flow, hyperaemia, vasospasm | ventilation, CPP, analgesia/ sedation, transfusion |
| Electrocorticography | focal | local cortical spreading depression | sedation, CPP, nutrition (glucose) |
| Table 2:Advantages and disadvantages of the different neuromonitoring tools used to guide type, extent, and duration of treatment options. | ||
| Monitoring | Advantages | Disadvantages |
| Intracranial pressure (ICP) | • continuous assessment of intracranial pathology | • local measurement • regional heterogeneity • only supratentorial compartment • surgical intervention with potential for additional brain damage (haemorrhage, injury of deep structures, infections) • incorrect values following craniectomy, subdural air entrapment and absent wave curve |
| Cerebral perfusion pressure (CPP) | • continuous assessment of cerebral perfusion equivalent | • calculated value • estimated global perfusion • no assessment of regional perfusion • impossible without ICP |
| SjvO2 | • (continuous) assessment of cerebral oxygenation/ perfusion | • discontinuous assessment • requires blood sampling • limited stability of sensors for continuous assessment of oxygen saturation • requires cannulation with associated risks (bleeding, thrombosis, bacteraemia, infections) • impaired venous outflow with increased ICP |
| ptiO2 | • continuous assessment of cerebral oxygenation/ perfusion | • local measurement • regional heterogeneity • surgical intervention requiring trephination with potential for additional brain damage (haemorrhage, injury of deep structures, infections) • expensive |
| Microdialysis | • discontinuous assessment of cerebral metabolism/ indirect assessment of cerebral perfusion and oxygenation | • local measurement • regional heterogeneity • surgical intervention requiring trephination with potential for additional brain damage (haemorrhage, injury of deep structures, infections) • expensive |
| TCD | • indirect assessment of cerebral perfusion • indirect assessment of ICP via calculated pulsatility index | • discontinuous • requires expertise • requires additional investigations to differentiate vasospasm from hyperaemia (e.g., angiography, MRI, ptiO2, SjvO2, microdialysis) |
| Electrocorticography | • continuous assessment of electrical discharges | • local measurement • regional heterogeneity • surgical intervention requiring trephination and opening of the dura with potential for additional brain damage (haemorrhage, cortical injury, infections) • expensive • not widely performed |
The primary parameter used to judge cerebral deterioration is ICP. Elevated ICP due to increased intracranial volume induces new and progressing secondary damage which, in turn, can induce and maintain a vicious circle [3]. The oversimplified understanding that increased ICP >20 mm Hg is pathologic lead to the current misconception that normal ICP guarantees absence of pathologic processes. Extended neuromonitoring, however, shows that this is incorrect. New data show that metabolic and functional alterations even precede increases in ICP following TBI [4]. It is important to remember that this threshold of 20 mm Hg stems from a time of insufficient neuromonitoring as extended neuromonitoring (e.g., SjvO2, ptiO2, microdialysis, and TCD) had not been integrated in daily routine. A very simple measure to indirectly estimate global cerebral perfusion is to calculate cerebral perfusion pressure (CPP): CPP = MABP- ICP. A “normal” CPP, however, does not guarantee sufficient cerebral perfusion and oxygenation. To define an optimal CPP, other parameters as e.g., ptiO2, SjvO2, metabolism, and flow velocity are helpful. ICP measurement requires a surgical intervention which is associated with certain risks as e.g., bleeding, additional brain damage, infections. Furthermore, regional heterogeneity, influence of extent of midline shift, and the routine measurement confined to the supratentorial compartment are certain limitations [5]. As shown by Rosner et al. [6] ICP- dependent changes in CPP are dynamic, therefore requiring therapeutic flexibility, a fact which is regularly overlooked.
Cannulation of the internal jugular vein allows analysis of SjvO2, calculation of various metabolic indices (e.g. oxygen- glucose index: OGI, lactate- oxygen index: LOI, lactate- glucose index: LGI) [7, 8], determination of the oxygen extraction ratio (OER) and assessment of, for example, arterio- jugular venous lactate difference. These different parameters enable detailed assessment of cerebral energetic disturbances [8]. SjvO2 reflects changes in cerebral oxygen supply, cerebral perfusion and cerebral oxygen consumption as SjvO2 correlates directly with perfusion and correlates inversely with cerebral oxygen consumption. Thus, an increase in MABP with subsequent amelioration of CPP as well as reduced hyperventilation will improve cerebral oxygen supply due to pressure-dependent and vasodilation- mediated increased perfusion. Reducing cerebral oxygen consumption due to pharmacological inhibition of neuronal activity during pharmacological coma or by reducing brain temperature will also elevate SjvO2.
Global cerebral changes as reflected by SjvO2 correlate well with local measurements using ptiO2 [9]. SjvO2 ≤50% reflect cerebral ischaemia and should be avoided. Immediate correction is important [10] since hypoxic/ ischaemic SjvO2 values are associated with metabolic perturbation reflected by increased lactate and glutamate levels [11] as well as sustained mortality and morbidity [12].
SjvO2 values >80% reflect underlying hyperaemia or luxury perfusion which permits a reduction in CPP and a decrease in cerebral vasodilation by controlled hyperventilation.
The impact of calculating arterio- jugular venous lactate difference is less clear and convincing [13, 14], possibly due to the fact that the brain is capable of consuming lactate to produce energy under pathological conditions [15].
Cannulation of the jugular vein is associated with certain risks such as, for example, haemorrhage and puncture of the carotid artery if not controlled by sonography, thrombosis formation and catheter-related infections possibly progressing to sepsis. In addition, the side of insertion relative to the traumatic lesions has been discussed controversially.
Assessing ptiO2 unmasks both local changes and the cerebral consequences of systemic influences, thereby allowing guidance of the type and extent of therapeutic interventions [9, 16]. Similar to changes in SjvO2, ptiO2 values indirectly reflect cerebral perfusion and oxygenation [17]. Low SjvO2 and ptiO2 values unmask reduced cerebral perfusion due to, for example, systemic hypotension or local cerebral vasoconstriction caused by hyperventilation or vasospasm. Further reasons such as sustained oxygen consumption due to increased neuronal activity resulting from insufficient analgesia/ sedation, epileptic discharges, insufficient oxygen supply due to anaemia, impaired cardiac output, and insufficient oxygenation must be searched for and corrected. Thus, assessing global as well as local changes reflected by SjvO2 and ptiO2permits detailed and controlled therapeutic corrections. In this context, we can decide whether, for example, ventilation, haemodynamic support or haematocrit must be corrected.
Validation studies have shown that ptiO2 values <10 mm Hg (Licox®) reflecting tissue hypoxia are associated with increased extracellular glutamate if not corrected within 30 minutes [18, 19]. In addition, these ischaemic values correlate with neuropsychological deficits in survivors [20]. As summarised by Maloney- Wilensky and colleagues ptiO2 <10 mm Hg longer than 15 minutes is associated with worse outcome and increased mortality [21]. Taken together, these findings suggest that integrating continuous assessment of ptiO2 in daily routine could be valuable in the prevention of overlooking situations with impaired cerebral perfusion and oxygenation. To date, we still lack a clear consensus on how to correct decreased ptiO2 values and which sequence is the most appropriate as several approaches can be used, including increases in FiO2, CPP, paCO2, sedation and haemoglobin. In addition, it is unclear which target level should be used and if excessive or inadequate correction is harmful.
Abnormally elevated ptiO2values >30 mm Hg (corresponding to SjvO2 ≥80%) strongly suggest uncoupling of cerebral metabolism from cerebral perfusion. In this context, reduced cerebral oxygen consumption, for example, due to deep sedation is associated with strong vasodilation leading to hyperaemia and global luxury perfusion. Hyperaemia, in turn, elevates ICP caused by an increase in intracranial blood volume [22].
Cerebral microdialysis allows detailed insight into otherwise hidden metabolic alterations by measuring changes in glucose, lactate, pyruvate, glycerol, glutamate, and calculating lactate to pyruvate ratio [23, 24]. Due to the dialysis duration which is commonly 60 minutes, clinical decisions are based on metabolic changes which have already occurred previously. Consequently, the metabolic alterations unmasked by microdialysis should always be judged together with other parameters which are assessed continuously such as ptiO2, SjvO2, CPP, ICP. Continuous glucose analysis using microdialysis is currently being investigated.
To avoid injuries within the pre- and postcentral cortex, microdialysis (as well as ptiO2 and ICP) are inserted in the frontal lobe. Similar to the regional heterogeneity of interhemispheric pressure gradients we also find regionally different metabolic changes [25]. Nonetheless, signs of impaired cerebral metabolism are found even in regions without obvious signs of structural damage. This functional impairment can result from increased ICP due to local changes and can be induced by systemic influences due to, for example, hypotension, hyperaemia, vasospasm, hyperventilation, fever, epileptic discharges, hypoglycaemia or anaemia. In addition, improvement of signs of metabolic deterioration can be used to reflect positive therapeutic effects [26]. Integration of microdialysis allows reduction of CPP in a controlled manner to 50 mm Hg as practiced within the “LUND- concept” [27]. In addition to absolute values and relative changes of the different metabolic parameters over time, calculating lactate to pyruvate ratio reflects the severity of underlying metabolic impairment [28]. Pathologically increased lactate to pyruvate ratios are associated with subsequent chronic frontal lobe atrophy [28].
Elevated extracellular glutamate reflects excessive neuronal excitation or signs of severe cell damage resulting in release of intracellularly stored glutamate. Increased lactate levels exhibit an energetic deficit while decreasing glucose levels can result from increased cellular uptake and metabolism and/or insufficient supply due to systemic hypoglycaemia, impaired perfusion, or insufficient expression of glucose transporters. Elevated glycerol values reflect membrane damage.
Overall, microdialysis can be used to unmask pathological changes, characterise pathological relevance of certain alterations, and guide therapeutic interventions (e.g. hyperventilation, oxygenation, sedation, CPP level). As recently shown by Timofeev and colleagues low glucose and elevated lactate to pyruvate ratios are significant independent predictors of mortality [29]. Metabolic changes determined by microdialysis can even be used as an early warning system to unmask pathological alterations which precede increases in ICP by 12 hours [4, 19].
Taken together, these findings suggest that integrating monitoring of cerebral metabolism in daily routine could be valuable in the detetion of functional deterioration with subsequent oedema formation and increase in ICP. To date, we still lack a clear consensus on the threshold values required to prompt corrective measures, including increases in FiO2, CPP, paCO2, sedation, haemoglobin and glucose. In addition, it is unclear which target level should be used and if excessive or inadequate correction is harmful.
Since its introduction in clinical routine, transcranial Doppler sonography (TCD) has proven helpful in unmasking conditions of low flow [30], vasospasm and hyperaemia all of which require differential therapeutic interventions. TCD- determined cerebral blood flow velocity within the large basal cerebral arteries reflects regional cerebral perfusion, cerebral autoregulation, CO2- reactivity under normal and pathological conditions [31]. In addition to absolute flow velocities calculated values, such as the pulsatility index (PI) and resistance index (RI) allow non-invasive estimation of ICP and CPP [32, 33], providing individual anatomy allows sufficient insonation depth. This approach is helpful if an ICP probe cannot be inserted due to a coagulation disorder or if an ICP probe is damaged, thereby bridging the time until a new probe is inserted. However, this non- invasive assessment of ICP is not a substitute for continuously measured ICP.
Functional changes in neuronal activity and transmission of axonal information can be assessed by EEG, sensory evoked potentials (SEP) or acoustic evoked potential (AEP). These investigations require specialised and well-trained personnel. Changes within the different EEG frequency spectra and amplitudes are also influenced by the lesions themselves, concomitant analgesia/ sedation, hypothermia and hyperventilation. Whilst pathological changes in evoked potentials reliably predict mortality and morbidity [34] this is not the case for EEG analysis as the underlying pharmacological coma influences the different frequency bands. Apart from diagnosing epileptic discharges, EEG is commonly used to adapt the dose of barbiturates aimed at maintaining a burst suppression pattern during barbiturate coma. More detailed analysis of the shifts within the frequency bands has shown that post traumatically reduced variability of the alpha frequency is gaining increasing prognostic importance as this is associated with significantly reduced regeneration [35. 36]. Simplified EEG analysis (BIS® EEG, Narcotrend®) can be used to continuously assess and control sedation. The application of these techniques in the clinical intensive care routine still awaits indepth analysis.
CSD resulting from neuronal and glial depolarisation is a progressive functional disturbance associated with energy consuming processes [37], thereby contributing to the secondary growth of a pre-existing lesion that is of clinical relevance [38, 39]. CSD is caused by elevated extracellular potassium concentrations, decreased cerebral NO levels and reduced blood and brain glucose concentrations [40, 41]. Measurement of CSD requires subdural introduction of a special sensor directly placed on the cortical surface. CSD is associated with decreased cerebral glucose, increased lactate to pyruvate ratio and elevated lactate [42, 43]. Further investigations are required to determine if a decrease in glucose with an increase in lactate to pyruvate ratio is specific for CSD. This would allow identification of CSD based on metabolic changes using microdialysis. Assessment of CSD requires surgical insertion and subdural placement of specialized sensors which is currently only performed in specialised centers. This surgical intervention is also associated with certain risks such as subdural haematoma and infections.
Specialized probes positioned within the brain tissue allow determination of local cerebral blood flow (CBF) based on the difference in temperature between the neutral plate and the heated element. Changes in CBF can be used to diagnose impaired perfusion and disturbed autoregulation, thereby allowing guidance of treatment options such as hyperventilation and blood pressure variation [44, 45]. As with the other probes, interpretation of CBF values is confined to a small region of interest. In case of fever, accuracy of the temperature- dependent readings is questioned. In addition, surgery- associated complications must also be considered (additional tissue damage, bleeding, infection).
Basic treatment aims in patients suffering from severe TBI are to optimise cerebral perfusion, improve oxygenation and stabilise metabolism in order to prevent secondary progression of underlying brain damage. For this, integration of extended neuromonitoring in our daily clinical routine appears helpful. Extended neuromonitoring may provide more detailed insight into otherwise occult changes. For this, SjvO2, ptiO2, microdialysis, TCD and electroencephalographic studies provide important data enabling characterisation of functional influences defining threshold values and the adaption of therapeutic interventions in type, extent and duration (fig. 1). These monitoring modalities aid in preventing excessive therapeutic corrections which by themselves can induce additional damage. In this context, aggressive volume administration to increase CPP has been associated with a sustained risk of ARDS [46] and abdominal compartment syndrome [47], excessive ventilatory support to increase paO2 is feared to induce additional pulmonary damage [48], aggressive lowering of arterial blood glucose to prevent hyperglycaemia- induced cell damage increases frequency and extent of hypoglycaemic episodes [49], and a categorical transfusion regimen to improve cerebral oxygenation is offset by transfusion- related complications [50].
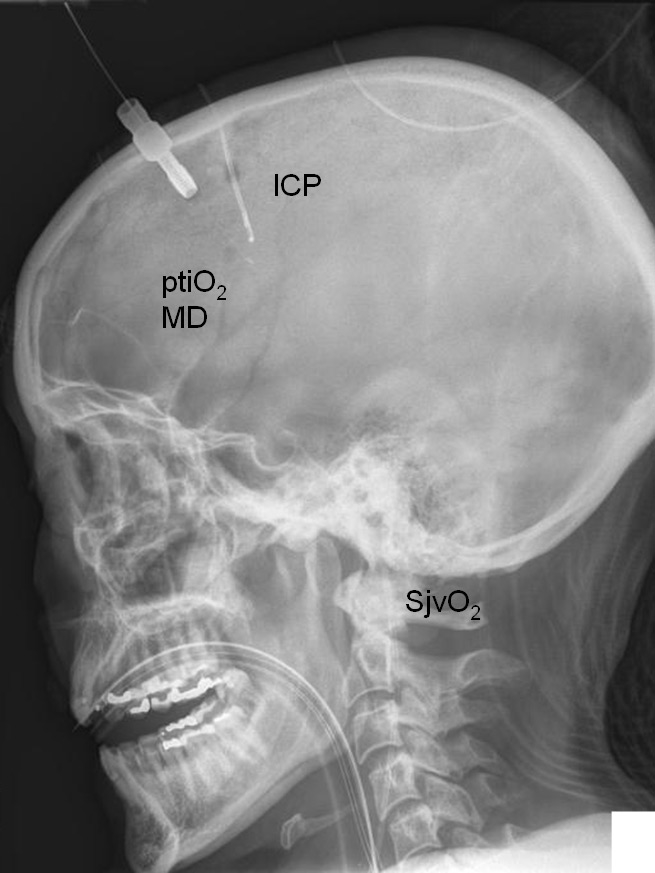
Figure 1
Illustrative lateral X- ray view showing positioning of ICP, ptiO2, microdialysis (MD), and jugular venous catheter allowing measurement of SjvO2. This allows to combine local (ptiO2, microdialysis) with global neuromonitoring (SjvO2).
Basic neuromonitoring limited to ICP and CPP cannot assess changes in cerebral perfusion, oxygenation, metabolism and electrophysiological function. Consequently, we are bound to not only miss important signs of deterioration but we will also fail to adapt and reduce therapeutic interventions once previous impairment has been corrected. There is increasing evidence that extended neuromonitoring can be used to:
– identify optimal CPP
– guide ventilatory support: oxygenation and ventilation
– define adequate haemoglobin level and guide transfusion practice
– determine optimal blood and brain glucose
– guide decompressive craniectomy
As already shown by Rosner and colleagues, the optimal CPP defined by the lowest ICP must be identified within each patient [51] and is subject to a strong intra- and interpatient variability even within a single day. According to the original description, optimal CPP was 90 mm Hg. Whether this also resulted in a CPP- dependent improvement of cerebral perfusion, oxygenation and metabolism cannot be determined as extended neuromonitoring had not been integrated in this study. As shown by Reinert and colleagues, ptiO2 is strongly influenced by CPP [26]. This was also corroborated by Marin-Caballos and colleagues nicely demonstrating that ptiO2 values can be used to determine the lower most acceptable CPP threshold [52]. The authors convincingly concluded that the generally recommended CPP threshold of 60 mm Hg is insufficient. This is in line with other reports showing that low and even “normal” CPP values cannot protect from cerebral hypoxia reflected by ptiO2 measurements and signs of impaired metabolism [24]. This underscores the necessity of continuously assessing ptiO2 and cerebral metabolism. In this context, a normal CPP of approximately 70 mm Hg has been shown to be insufficient for the perifocal tissue compared to normal appearing tissue in which ptiO2 was significantly higher [53]. CPP exceeding 75 mm Hg is required to induce highest ptiO2 values [26]. Integrating ptiO2 in clinical routine using a ptiO2- guided treatment protocol in addition to ICP and CPP significantly improved ptiO2 levels, kept ICP <20 mm Hg, maintained CPP at stable values (mean 76 mm Hg), improved outcome reflected by the Glasgow Outcome Scale and reduced mortality rate compared to the standard ICP/ CPP- directed therapy [54]. Similar findings were also reported by Spiotta and colleagues [55]. Mortality was linked to longer durations of compromised brain oxygen (ptiO2 <20 mm Hg), brain hypoxia (ptiO2 <15 mm Hg), more episodes and longer cumulative duration of compromised ptiO2 values and less successful treatment of compromised ptiO2 [55].
As shown by Nordström and colleagues it is of the utmost importance to focus not only on an individual parameter but to also consider concomitant therapy. Bearing this in mind reduction for example, of the CPP to 50 mm Hg is possible but cannot and should not be extended to all patients, especially if the appropriate neuromonitoring, e.g. cerebral microdialysis is not used [27]. In this context, lactate and the calculated lactate to pyruvate ratio reliably reflect insufficient cerebral perfusion and oxygen delivery responsible for energetic and metabolic impairment [27, 56]. Improvement in cerebral perfusion and correction of anaemia successfully normalised brain lactate to pyruvate ratio, glycero, and glutamate concentrations [56].
As in all critically ill patients lung protective ventilation is recommended to avoid lung injury and haemodynamic instability. Ventilatory settings are adjusted according to pre-defined paO2 and paCO2 targets. The paO2 and paCO2 targets, in turn, can be set by ptiO2 and SjvO2. This prevents excessive increase in FiO2, PEEP and ventilation frequency.
Oxygenation. Even during deep sedation and hypothermia, the metabolically active brain requires sufficient amounts of oxygen to fuel energy-consuming processes. For this, we require sufficient cardiac output, optimal local perfusion, adequate haemoglobin concentration and sufficient pulmonary function to enable ideal oxygen transport and cerebral oxygen supply. Under conditions of controlled hypothermia and pharmacological coma cerebral oxygen consumption is decreased. Thus, a categorical paO2 level dictating the ventilatory support might be inadequate as it promotes aggressive ventilatory settings. Cerebral oxygenation using ptiO2 and SjvO2 are very helpful in guiding ventilatory support.
As shown under clinical conditions, an increase in FiO2 significantly increased ptiO2 [26, 57] and reduced cerebral lactate [26]. Interestingly, a too aggressive increase in ptiO2 using normobaric hyperoxia (FiO2 1.0) was associated with decreased cerebral blood flow despite improved brain metabolism and coincided with worse outcome three months after TBI. As shown under experimental conditions, increasing oxygen supply alone is insufficient to improve cerebral oxygenation if impaired cerebral perfusion is not corrected [58].
Positive end expiratory pressure (PEEP). Elevated PEEP can induce pulmonary and circulatory impairment, especially during hypovolaemia by impairing venous backflow to the heart, thereby resulting in secondary reduced pulmonary perfusion with worse blood oxygenation. In addition, increased PEEP can contribute to elevated ICP due to impaired cerebral venous outflow and can also reduce mean arterial and cerebral perfusion pressure, thereby impairing cerebral perfusion and oxygenation [52, 59].
Hyperventilation. Uncontrolled and prophylactic hyperventilation during the first days following TBI induces additional secondary ischaemic brain damage [60] and must be avoided meticulously. Hypocapnia-induced vasoconstriction mediates impaired perfusion, metabolic and neurochemical alterations as reflected by reduced ptiO2 and SjvO2 and elevated extracellular glutamate and lactate [61]. Interestingly, even small changes in paCO2 from 38 to 34 mm Hg within normal limits are detrimental [62]. Consequently, extended neuromonitoring should also be performed in patients during anticipated normoventilation. Hyperventilation is an easy and helpful therapeutic intervention to decrease elevated ICP [63]. However, we should control hyperventilation by using appropriate neuromonitoring techniques to unmask signs of cerebral ischaemia due to hyperventilation-induced vasoconstriction because normal ICP levels achieved by hyperventilation will cause us to miss relevant pathological processes within the brain. This can only be prevented by integrating appropriate neuromonitoring. Reduced SjvO2, ptiO2 and signs of metabolic impairment (lactate, glutamate, lactate-to-pyruvate ratio) [64, 65] aid in assessing the lowest possible paCO2 level [66–69] and avoid active induction of secondary brain damage.
To prevent insufficient cerebral oxygenation adequate oxygen supply must be maintained. For this, an appropriate number of oxygen carriers, i.e. red blood cells and haemoglobin must be present. At present, it still remains unclear which haemoglobin count is optimal in patients with severe TBI. From a physiological point of view the haematocrit is optimal whenever the tissue is sufficiently supplied with oxygen without reducing perfusion due to increased viscosity. Inducing acute haemodilution with a haematocrit <21% under experimental conditions was detrimental [70]. In patients with pre-existing vasospasm following ruptured aneurysmal bleeding, active reduction in haematocrit from 36 to 28% resulted in significantly reduced cerebral oxygen supply [71]. Thus, any form of severe haemodilution should be avoided. Whether a gradual and slow decrease in haematocrit developing over days as observed under clinical conditions following severe TBI will also impair cerebral oxygenation and metabolism remains unclear. Concomitant therapy due to hypothermia and deep sedation could increase the hypoxic threshold, thereby allowing a lower haematocrit level and thus decreasing transfusion requirement. Under controlled critical care conditions with stable CPP and stable oxygenation and ventilation, ptiO2 can be used to define the transfusion threshold [72, 73]. Patients with a ptiO2 >15 mm Hg do not profit from red blood cell transfusion [73]. Only in patients with a haematocrit <30% did a transfusion of red blood cells persistently increase ptiO2 >15 mm Hg, providing ptiO2 was below 15 mm Hg [73]. Concomitantly, CPP must be maintained above 60 mm Hg to prevent cerebral hypoxia determined by ptiO2 due to low haemoglobin levels [74]. These data show that ptiO2 and brain metabolic parameters can be used to continuously assess critical transfusion threshold. Adapting the transfusion threshold based on a neuromonitoring-guided approach is expected to enable us to determine the correct time point and amount of transfusion of red blood cells, thereby avoiding categorical and even inadequate transfusion practice. The impact of neuromonitoring-guided transfusion practice on morbidity and mortality is currently being investigated in more detail.
Elevated blood glucose >9.4 mmol/l (>169 mg/dl) is associated with increased mortality and morbidity [75, 76]. Hyperglycaemia induces mitochondrial damage, aggravates oxidative stress, impairs neutrophil function, reduces phagocytosis, and diminishes intracellular destruction of ingested bacteria. These destructive cascades can be prevented by fast normalisation of elevated blood glucose levels. Maintaining blood glucose levels within tight limits between 4.4 and 6.1 mM (80 to 110 mg/dl) [77], however, is off-set by the risk of hypoglycaemia and strong variation in blood glucose levels [78]. The increased frequency of hypoglycaemia during the first days following injury was associated with sustained mortality [79–81]. As shown by Vespa and co-workers reducing blood glucose levels to 4.4–6.1 mmol/l significantly increased extracellular glutamate levels and augmented lactate to pyruvate ratio, reflecting excessive neuronal excitation and metabolic perturbation [82]. In addition, mortality was increased in patients with decreased blood glucose and low cerebral extracellular glucose levels [83]. Under experimental and clinical conditions blood glucose levels <5 mmol/l can induce CSD [84–88]. Thus, any correction to low normal blood glucose values should be tightly controlled by extended neuromonitoring. In this context, jugular venous parameters reflected increased cerebral oxygen consumption, lactate and CO2 production and decreased glucose uptake at low blood glucose levels with signs of improvement at arterial blood glucose levels between 6 and 9 mmol/l [6]. With the help of cerebral microdialysis the influence of insulin administration on brain metabolism can be characterised. In this context, insulin should not be given at arterial blood glucose levels <5 mmol/l as this significantly increased extracellular glutamate and lactate to pyruvate ratio while insulin administration is encouraged at arterial blood glucose levels >9 mmol/l to increase cerebral glucose levels and reduce lactate to pyruvate ratio [86, 87]. Optimal and safe blood glucose levels appear between 6 and 9 mmol/l. Cerebral microdialysis also helps in assessing optimal brain glucose levels. Brain glucose should remain above 1 mmol/l as brain glucose levels <1 mmol/l are associated with signs of metabolic impairment as reflected by increased lactate to pyruvate ratio [86–88]. Persistently low brain glucose levels were associated with electrographic seizures, non-ischaemic reductions in cerebral perfusion pressure, decreased jugular venous oxygen saturation, increased glutamate levels, and poor outcome [88]. Integrating brain glucose measurements in clinical routine has allowed us to optimise nutritional support to correct cerebral hypoglycaemia by increasing arterial blood glucose levels. This can be achieved by optimising enteral or parenteral nutrition (fig. 2). If this will also translate to an improved outcome remains to be shown.
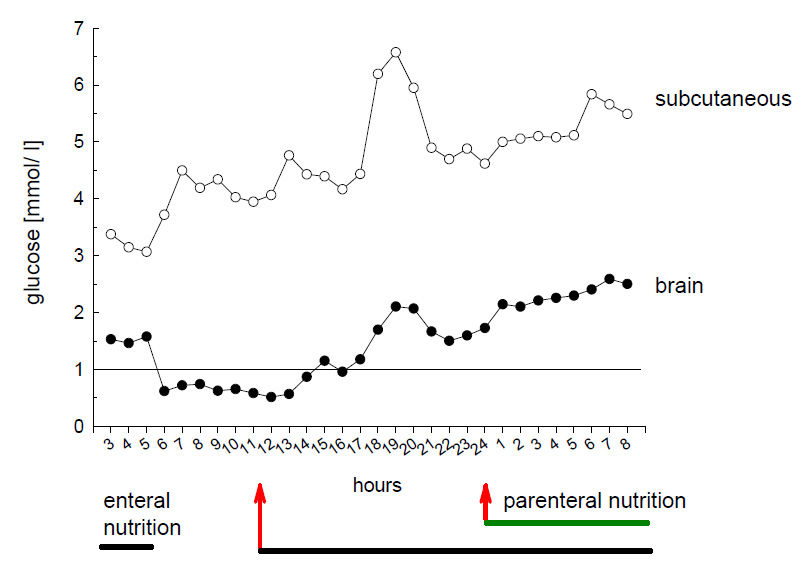
Figure 2
Illustrative case showing that brain and subcutaneous glucose are influenced by enteral and parenteral nutrition. Following cessation of enteral nutrition, brain glucose dropped below 1 mmol/ l. Restarting enteral nutrition corrected cerebral hypoglycaemia. Developing constipation prohibited increase in enteral nutrition. Parenteral nutrition was begun to prevent caloric deficiency and to prevent cerebral hypoglycaemia. Overall, changes in brain glucose are also reflected by subcutaneous glucose which reflects changes in arterial blood glucose (not shown). However, subcutaneous glucose did not unmask cerebral hypoglycaemia after stopping enteral nutrition. These changes occurred at ICP values <15 mm Hg which were maintained due to aggressive treatment consisting of deep sedation, controlled mild hypothermia (35°C), and controlled ventilation.
Intracranial hypertension impairs cerebral perfusion, oxygenation and metabolism. Decompressive craniectomy, in turn, will improve cerebral perfusion, oxygenation and metabolism which is most effective with dura enlargement [89–94]. The presence of pathological neuromonitoring before clinical deterioration [92] underscores the importance of integrating extended neuromonitoring in clinical routine. Consequently, extended neuromonitoring can aid in deciding when to perform a decompressive craniectomy [93]. It remains to be shown if extended neuromonitoring may be helpful in identifying the appropriate patients, thereby avoiding an increase in unfavourable outcome despite successfully treating intracranial hypertension as recently shown by Cooper et al. [94].
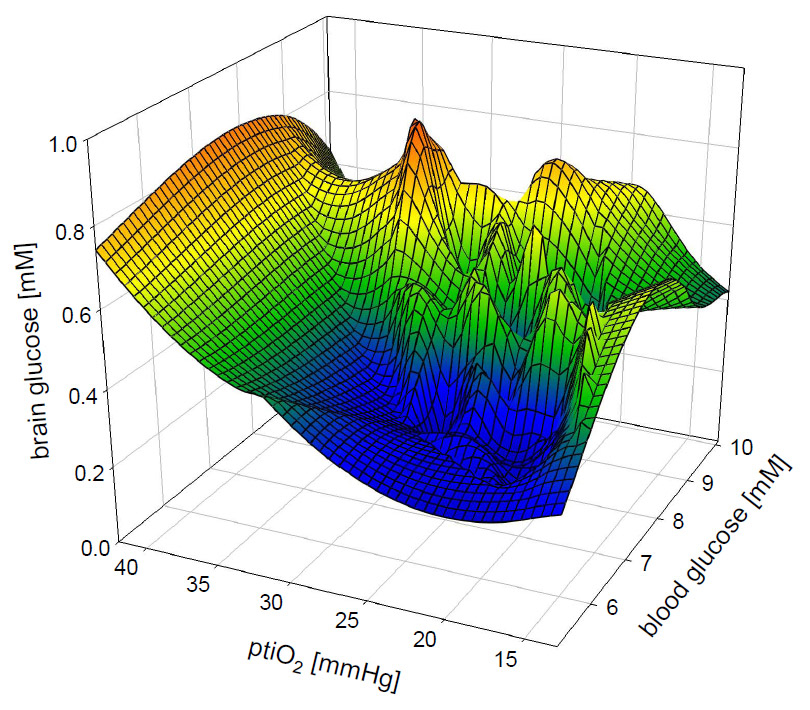
Figure 3
Three- dimensional graph showing functional impact of blood glucose and cerebral perfusion (indirectly assessed by ptiO2) on brain glucose. While low blood glucose can be compensated by a higher level of cerebral perfusion (higher ptiO2 values) to increase brain glucose levels, elevated blood glucose can compensate for lower level of cerebral perfusion (lower ptiO2 values). Optimal conditions unmasked by highest brain glucose levels appear to be at arterial blood glucose values between 8 and 9 mmol/l and ptiO2 values around 30 mm Hg.
The best of knowledge expressed in the maxim of evidence-based medicine requires clinically convincing and statistically sound data. In this context double blind, placebo-controlled, multicentre, international clinical trials are far superior to meta-analyses, systematic reviews, retrospective analyses, and expert opinions or individual experience. None of the techniques, including the non-invasive and continuous measurement of peripheral oxygen saturation (SpO2) as commonly used in daily clinical routine, have ever been investigated in a double blind, placebo-controlled, multicentre, international clinical trial with the aim of proving their importance in reducing mortality and improving outcome. Given ethical considerations it will not be possible to conduct a double blind, placebo-controlled clinical trial in which patients will be deprived of a certain neuromonitoring technique, as positive findings have been observed in individual patients and retrospective analyses. For a reliable interpretation and conduction of clinical trials evaluating the level of evidence for any technique requires an adequate level of experience. To gain this adequate level of experience, in turn, sufficient time and number of patients are required. Objectively seen, we are still midst in a learning phase and cannot assume that the current knowledge is set in stone as reflected by the steadily growing number of publications investigating the usefulness of extended neuromonitoring in clinical diagnostics and therapy. In addition, in depth knowledge is required. We must realize that the underlying pathophysiological interactions and circuits are multi- dimensional and that focusing on only one parameter is wrong. In this context, brain glucose, for example, is strongly influenced by blood glucose and perfusion (indirectly reflected by ptiO2) (fig. 3). Blood glucose as well as perfusion are influenced by other interventions which must also be considered. At the same time, oversimplification of very complex problems for facilitated integration in clinical routine must be avoided. This can only be provided by specialists. To make interpretation of the obtained data even more complicated we pretend to already have found the optimal treatment form when only focusing on one parameter. In reality, however, the conflicting impact, i.e. both, positive and negative, of our contemporary routine treatment is unclear. Although we are lacking a scientifically sound basis, we are convinced that we treat our patients to their benefit based on our current knowledge and experience. From a scientific point of view and in face of our duty to improve current intensive care medicine, it is unfair and not justified to downgrade the different techniques of extended neuromonitoring. Ongoing as well as future investigations will improve our understanding and subsequently the fine-tuning of our treatment options. At present, the level of evidence is convincing for the experienced specialists and doubtful for the sceptics and those who are not familiar with these techniques. The future will show us which of the techniques are “nice to have” and which must be considered essential. Based on my personal experience it has become very difficult for me to adequately treat patients without parameters reflecting cerebral oxygenation/ perfusion and brain metabolism. In clinical routine I do not base my decisions solely on changes in ICP and CPP. Downstream parameters are always used to define the optimal ICP and CPP level on an individual basis. With the integration of extended neuromonitoring we were able to significantly reduce the amount of transfused red blood cells and diminish the rate of acute lung injury due to excessive volume administration.
1 Maegele M, Engel D, Bouillon B, Lefering R, Fach H, et al. Incidence and outcome of traumatic brain injury in an urban area in Western Europe over 10 years. Eur Surg Res. 2007;39(6):372–9.
2 von Elm E, Osterwalder JJ, Graber C, Schoettker P, Stocker R, Zangger P, et al. Severe traumatic brain injury in Switzerland – feasibility and first results of a cohort study. Swiss Med Wkly. 2008;138(23-24):327–34.
3 Smith M. Monitoring intracranial pressure in traumatic brain injury. Anesth Analg. 2008;106(1):240–8.
4 Belli A, Sen J, Petzold A, Russo S, Kitchen N, Smith M. Metabolic failure precedes intracranial pressure rises in traumatic brain injury: a microdialysis study. Acta Neurochir (Wien). 2008;150(5):461–9.
5 Sahuquillo J, Poca MA, Arribas M, Garnacho A, Rubio E. Interhemispheric supratentorial intracranial pressure gradients in head-injured patients: are they clinically important? J Neurosurg. 1999;90(1):16–26.
6 Rosner MJ, Rosner SD, Johnson AH. Cerebral perfusion pressure: management protocol and clinical results. J Neurosurg. 1995;83(6):949–62.
7 Møller K, Paulson OB, Hornbein TF, Colier WN, Paulson AS, Roach RC, et al. Unchanged cerebral blood flow and oxidative metabolism after acclimatization to high altitude. J Cereb Blood Flow Metab. 2002;22(1):118–26.
8 Holbein M, Béchir M, Ludwig S, Sommerfeld J, Cottini SR, Keel M, et al. Differential influence of arterial blood glucose on cerebral metabolism following severe traumatic brain injury. Crit Care. 2009;13(1):R13.
9 Kiening KL, Unterberg AW, Bardt TF, Schneider GH, Lanksch WR. Monitoring of cerebral oxygenation in patients with severe head injuries: brain tissue PO2 versus jugular vein oxygen saturation. J Neurosurg. 1996;85(5):751–7.
10 Vigué B, Ract C, Benayed M, Zlotine N, Leblanc PE, et al. Early SjvO2 monitoring in patients with severe brain trauma. Intensive Care Med. 1999;25(5):445–51.
11 Chan MT, Ng SC, Lam JM, Poon WS, Gin T. Re-defining the ischemic threshold for jugular venous oxygen saturation – a microdialysis study in patients with severe head injury. Acta Neurochir Suppl. 2005;95:63–6.
12 Gopinath SP, Robertson CS, Contant CF, Hayes C, Feldman Z, Narayan RK, et al. Jugular venous desaturation and outcome after head injury. J Neurol Neurosurg Psychiatry. 1994;57(6):717–23.
13 Poca MA, Sahuquillo J, Vilalta A, Garnacho A. Lack of utility of arteriojugular venous differences of lactate as a reliable indicator of increased brain anaerobic metabolism in traumatic brain injury. J Neurosurg. 2007;106(4):530–7.
14 Pérez A, Minces PG, Schnitzler EJ, Agosta GE, Medina SA, Ciraolo CA. Jugular venous oxygen saturation or arteriovenous difference of lactate content and outcome in children with severe traumatic brain injury. Pediatr Crit Care Med. 2003;4(1):33–8.
15 Glenn TC, Kelly DF, Boscardin WJ, McArthur DL, Vespa P, Oertel M, et al. Energy dysfunction as a predictor of outcome after moderate or severe head injury: indices of oxygen, glucose, and lactate metabolism. J Cereb Blood Flow Metab. 2003;23(10):1239–50.
16 Rosenthal G, Hemphill JC 3rd, Sorani M, Martin C, Morabito D, Obrist WD, et al. Brain tissue oxygen tension is more indicative of oxygen diffusion than oxygen delivery and metabolism in patients with traumatic brain injury. Crit Care Med. 2008;36(6):1917–24.
17 Jaeger M, Soehle M, Schuhmann MU, Winkler D, Meixensberger J. Correlation of continuously monitored regional cerebral blood flow and brain tissue oxygen. Acta Neurochir (Wien). 2005;147(1):51–6.
18 Sarrafzadeh AS, Sakowitz OW, Callsen TA, Lanksch WR, Unterberg AW. Bedside microdialysis for early detection of cerebral hypoxia in traumatic brain injury. Neurosurg Focus. 2000;9(5):e2.
19 Meixensberger J, Kunze E, Barcsay E, Vaeth A, Roosen K. Clinical cerebral microdialysis: brain metabolism and brain tissue oxygenation after acute brain injury. Neurol Res. 2001;23(8):801–6.
20 Meixensberger J, Renner C, Simanowski R, Schmidtke A, Dings J, Roosen K. Influence of cerebral oxygenation following severe head injury on neuropsychological testing. Neurol Res. 2004;26(4):414–7.
21 Maloney-Wilensky E, Gracias V, Itkin A, Hoffman K, Bloom S, Yang W, et al. Brain tissue oxygen and outcome after severe traumatic brain injury: a systematic review. Crit Care Med. 2009;37(6):2057–63.
22 Jaeger M, Schuhmann MU, Soehle M, Meixensberger J. Continuous assessment of cerebrovascular autoregulation after traumatic brain injury using brain tissue oxygen pressure reactivity. Crit Care Med. 2006;34(6):1783–8.
23 Tisdall MM, Smith M. Cerebral microdialysis: research technique or clinical tool. Br J Anaesth. 2006;97(1):18–25.
24 Vespa P, Bergsneider M, Hattori N, Wu HM, Huang SC, Martin NA, et al. Metabolic crisis without brain ischemia is common after traumatic brain injury: a combined microdialysis and positron emission tomography study. J Cereb Blood Flow Metab. 2005;25(6):763–74.
25 Engström M, Polito A, Reinstrup P, Romner B, Ryding E, Ungerstedt U, et al. Intracerebral microdialysis in severe brain trauma: the importance of catheter location.J Neurosurg. 2005;102(3):460–9.
26 Reinert M, Barth A, Rothen HU, Schaller B, Takala J, Seiler RW. Effects of cerebral perfusion pressure and increased fraction of inspired oxygen on brain tissue oxygen, lactate and glucose in patients with severe head injury. Acta Neurochir (Wien). 2003;145(5):341–9.
27 Nordström CH, Reinstrup P, Xu W, Gärdenfors A, Ungerstedt U. Assessment of the lower limit for cerebral perfusion pressure in severe head injuries by bedside monitoring of regional energy metabolism. Anesthesiology. 2003;98(4):809–14.
28 Marcoux J, McArthur DA, Miller C, Glenn TC, Villablanca P, Martin NA, et al. Persistent metabolic crisis as measured by elevated cerebral microdialysis lactate-pyruvate ratio predicts chronic frontal lobe brain atrophy after traumatic brain injury. Crit Care Med. 2008;36(10):2871–7.
29 Timofeev I, Carpenter KL, Nortje J, Al-Rawi PG, O’Connell MT, Czosnyka M, et al. Cerebral extracellular chemistry and outcome following traumatic brain injury: a microdialysis study of 223 patients. Brain. 2011;134(Pt 2):484–94.
30 van Santbrink H, Schouten JW, Steyerberg EW, Avezaat CJ, Maas AI. Serial transcranial Doppler measurements in traumatic brain injury with special focus on the early posttraumatic period. Acta Neurochir (Wien). 2002;144(11):1141–9.
31 Rasulo FA, De Peri E, Lavinio A. Transcranial Doppler ultrasonography in intensive care. Eur J Anaesthesiol Suppl. 2008;42:167–73.
32 Moppett IK, Mahajan RP. Transcranial Doppler ultrasonography in anaesthesia and intensive care. Br J Anaesth. 2004;93(5):710–24.
33 Brandi G, Béchir M, Sailer S, Haberthür C, Stocker R, Stover JF. Transcranial color-coded duplex sonography allows to assess cerebral perfusion pressure noninvasively following severe traumatic brain injury. Acta Neurochir (Wien). 2010;152(6):965–72.
34 Carter BG, Butt W (2005) Are somatosensory evoked potentials the best predictor of outcome after severe brain injury? A systematic review. Intensive Care Med 31(6):765–75.
35 Roche RA, Dockree PM, Garavan H, Foxe JJ, Robertson IH, O’Mara SM. EEG alpha power changes reflect response inhibition deficits after traumatic brain injury (TBI) in humans. Neurosci Lett 2004;362(1):1–5.
36 Hebb MO, McArthur DL, Alger J, Etchepare M, Glenn TC, Bergsneider M, et al. Impaired percent alpha variability on continuous electroencephalography is associated with thalamic injury and predicts poor long-term outcome after human traumatic brain injury. J Neurotrauma. 2007;24(4):579–90.
37 Leao AAP. Spreading depression of activity in cerebral cortex. J Neurophysiol. 1944;7:359–90.
38 Dreier JP, Woitzik J, Fabricius M, Bhatia R, Major S, Drenckhahn C, et al. Delayed ischaemic neurological deficits after subarachnoid haemorrhage are associated with clusters of spreading depolarizations. Brain. 2006;129(Pt 12):3224–37.
39 Fabricius M, Fuhr S, Bhatia R, Boutelle M, Hashemi P, Strong AJ, Lauritzen M. Cortical spreading depression and peri-infarct depolarization in acutely injured human cerebral cortex. Brain. 2006;129(Pt 3):778–90.
40 Strong AJ, Hartings JA, Dreier JP. Cortical spreading depression: an adverse but treatable factor in intensive care? Curr Opin Crit Care. 2007;13(2):126–33.
41 Parkin M, Hopwood S, Jones DA, Hashemi P, Landolt H, Fabricius M, et al. Dynamic changes in brain glucose and lactate in pericontusional areas of the human cerebral cortex, monitored with rapid sampling on-line microdialysis: relationship with depolarisation-like events. J Cereb Blood Flow Metab. 2005;25(3):402–13.
42 Krajewski KL, Orakcioglu B, Haux D, Hertle DN, Santos E, Kiening KL, et al. Cerebral microdialysis in acutely brain-injured patients with spreading depolarizations. Acta Neurochir Suppl. 2011;110(Pt 1):125–30.
43 Feuerstein D, Manning A, Hashemi P, Bhatia R, Fabricius M, Tolias C, et al. Dynamic metabolic response to multiple spreading depolarizations in patients with acute brain injury: an online microdialysis study. J Cereb Blood Flow Metab. 2010;30(7):1343–55.
44 Jaeger M, Soehle M, Schuhmann MU, Winkler D, Meixensberger J. Correlation of continuously monitored regional cerebral blood flow and brain tissue oxygen. Acta Neurochir (Wien). 2005;147(1):51–6.
45 Rosenthal G, Sanchez-Mejia RO, Phan N, Hemphill JC 3rd, Martin C, Manley GT. Incorporating a parenchymal thermal diffusion cerebral blood flow probe in bedside assessment of cerebral autoregulation and vasoreactivity in patients with severe traumatic brain injury. J Neurosurg. 2011;114(1):62–70.
46 Robertson CS, Valadka AB, Hannay HJ, Contant CF, Gopinath SP, Cormio M, et al. Prevention of secondary ischemic insults after severe head injury. Crit Care Med. 1999;27(10):2086–95.
47 An G, West MA. Abdominal compartment syndrome: a concise clinical review. Crit Care Med. 2008;36(4):1304–10.
48 Pinheiro de Oliveira R, Hetzel MP, dos Anjos Silva M, Dallegrave D, Friedman G. Mechanical ventilation with high tidal volume induces inflammation in patients without lung disease. Crit Care. 2010;14(2):R39.
49 Meier R, Béchir M, Ludwig S, Sommerfeld J, Keel M, Steiger P, et al. Differential temporal profile of lowered blood glucose levels (3.5 to 6.5 mmol/l versus 5 to 8 mmol/l) in patients with severe traumatic brain injury. Crit Care. 2008;12(4):R98.
50 Cannon-Diehl MR. Transfusion in the critically ill: does it affect outcome? Crit Care Nurs Q. 2010;33(4):324–38.
51 Rosner MJ, Rosner SD, Johnson AH. Cerebral perfusion pressure: management protocol and clinical results. J Neurosurg. 1995;83(6):949–62.
52 Marín-Caballos AJ, Murillo-Cabezas F, Cayuela-Domínguez A, Domínguez-Roldán JM, Rincón-Ferrari MD, Valencia-Anguita J, et al. Cerebral perfusion pressure and risk of brain hypoxia in severe head injury: a prospective observational study. Crit Care. 2005;9(6):R670–6.
53 Longhi L, Pagan F, Valeriani V, Magnoni S, Zanier ER, Conte V, et al. Monitoring brain tissue oxygen tension in brain-injured patients reveals hypoxic episodes in normal-appearing and in perifocal tissue. Intensive Care Med. 2007;33(12):2136–42.
54 Narotam PK, Morrison JF, Nathoo N. Brain tissue oxygen monitoring in traumatic brain injury and major trauma: outcome analysis of a brain tissue oxygen-directed therapy. J Neurosurg. 2009;111(4):672–82.
55 Spiotta AM, Stiefel MF, Gracias VH, Garuffe AM, Kofke WA, Maloney-Wilensky E, et al. Brain tissue oxygen-directed management and outcome in patients with severe traumatic brain injury. J Neurosurg. 2010;113(3):571–80.
56 Ståhl N, Schalén W, Ungerstedt U, Nordström CH. Bedside biochemical monitoring of the penumbra zone surrounding an evacuated acute subdural haematoma. Acta Neurol Scand. 2003;108(3):211–5.
57 Menzel M, Doppenberg EM, Zauner A, Soukup J, Reinert MM, Clausen T, et al. Cerebral oxygenation in patients after severe head injury: monitoring and effects of arterial hyperoxia on cerebral blood flow, metabolism and intracranial pressure. J Neurosurg Anesthesiol. 1999;11(4):240–51.
58 Rossi S, Stocchetti N, Longhi L, Balestreri M, Spagnoli D, Zanier ER, Bellinzona G. Brain oxygen tension, oxygen supply, and oxygen consumption during arterial hyperoxia in a model of progressive cerebral ischemia. J Neurotrauma. 2001;18(2):163–74.
59 Caricato A, Conti G, Della Corte F, Mancino A, Santilli F, Sandroni C, et al. Effects of PEEP on the intracranial system of patients with head injury and subarachnoid haemorrhage: the role of respiratory system compliance. J Trauma. 2005;58(3):571–6.
60 Muizelaar JP, Marmarou A, Ward JD, Kontos HA, Choi SC, Becker DP, et al. Adverse effects of prolonged hyperventilation in patients with severe head injury: a randomized clinical trial. J Neurosurg. 1991;75(5):731–9.
61 Davis DP. Early ventilation in traumatic brain injury. Resuscitation. 2008;76(3):333–40.
62 Hutchinson PJ, Gupta AK, Fryer TF, Al-Rawi PG, Chatfield DA, Coles JP, et al. Correlation between cerebral blood flow, substrate delivery, and metabolism in head injury: a combined microdialysis and triple oxygen positron emission tomography study. J Cereb Blood Flow Metab. 2002;22(6):735–45.
63 Stocchetti N, Maas AI, Chieregato A, van der Plas AA. Hyperventilation in head injury: a review. Chest. 2005; 127(5):1812–27.
64 Sarrafzadeh AS, Kiening KL, Callsen TA, Unterberg AW. Metabolic changes during impending and manifest cerebral hypoxia in traumatic brain injury. Br J Neurosurg. 2003;17(4):340–6.
65 Marion DW, Puccio A, Wisniewski SR, Kochanek P, Dixon CE, Bullian L, et al. Effect of hyperventilation on extracellular concentrations of glutamate, lactate, pyruvate, and local cerebral blood flow in patients with severe traumatic brain injury. Crit Care Med. 2002;30(12):2619–25.
66 Unterberg AW, Kiening KL, Härtl R, Bardt T, Sarrafzadeh AS, Lanksch WR. Multimodal monitoring in patients with head injury: evaluation of the effects of treatment on cerebral oxygenation. J Trauma. 1997;42(5 Suppl):S32–7.
67 Soukup J, Bramsiepe I, Brucke M, Sanchin L, Menzel M. Evaluation of a bedside monitor of regional CBF as a measure of CO2 reactivity in neurosurgical intensive care patients. J Neurosurg Anesthesiol. 2008;20(4):249–55.
68 Soustiel JF, Mahamid E, Chistyakov A, Shik V, Benenson R, Zaaroor M. Comparison of moderate hyperventilation and mannitol for control of intracranial pressure control in patients with severe traumatic brain injury – a study of cerebral blood flow and metabolism. Acta Neurochir (Wien). 2006;148(8):845–51.
69 Carmona Suazo JA, Maas AI, van den Brink WA, van Santbrink H, Steyerberg EW, Avezaat CJ. CO2 reactivity and brain oxygen pressure monitoring in severe head injury. Crit Care Med. 2000;28(9):3268–74.
70 Hare GM, Mazer CD, Hutchison JS, McLaren AT, Liu E, Rassouli A, et al. Severe hemodilutional anemia increases cerebral tissue injury following acute neurotrauma. J Appl Physiol. 2007;103(3):1021–9.
71 Ekelund A, Reinstrup P, Ryding E, Andersson AM, Molund T, Kristiansson KA, et al. Effects of iso- and hypervolemic haemodilution on regional cerebral blood flow and oxygen delivery for patients with vasospasm after aneurysmal subarachnoid haemorrhage. Acta Neurochir (Wien). 2002;144(7):703–12.
72 Smith MJ, Stiefel MF, Magge S, Frangos S, Bloom S, Gracias V, Le Roux PD. Packed red blood cell transfusion increases local cerebral oxygenation. Crit Care Med. 2005;33(5):1104–8.
73 Leal-Noval SR, Rincón-Ferrari MD, Marin-Niebla A, Cayuela A, Arellano-Orden V, Marín-Caballos A, et al. Transfusion of erythrocyte concentrates produces a variable increment on cerebral oxygenation in patients with severe traumatic brain injury: a preliminary study. Intensive Care Med. 2006;32(11):1733–40.
74 Chang JJ, Youn TS, Benson D, Mattick H, Andrade N, Harper CR, et al. Physiologic and functional outcome correlates of brain tissue hypoxia in traumatic brain injury. Crit Care Med. 2009;37(1):283–90.
75 Van Beek JG, Mushkudiani NA, Steyerberg EW, Butcher I, McHugh GS, Lu J, et al. Prognostic value of admission laboratory parameters in traumatic brain injury: results from the IMPACT study. J Neurotrauma 2007;24:315–28.
76 Jeremitsky E, Omert LA, Dunham CM, Wilberger J, Rodriguez A. The impact of hyperglycaemia on patients with severe brain injury. J Trauma. 2005;58:47–50.
77 van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, et al. Intensive insulin therapy in the critically ill patients. N Engl J Med. 2001;345:1359–67.
78 Bilotta F, Caramia R, Cernak I, Paoloni FP, Doronzio A, Cuzzone V, et al. Intensive Insulin Therapy After Severe Traumatic Brain Injury: A Randomized Clinical Trial. Neurocrit Care. 2008;9(2):159–66.
79 Van den Berghe G, Wilmer A, Hermans G, Meersseman W, Wouters PJ, Milants I, et al. Intensive insulin therapy in the medical ICU. N Engl J Med. 2006;354:449–61.
80 Van den Berghe G, Schoonheydt K, Becx P, Bruyninckx F, Wouters PJ. Insulin therapy protects the central and peripheral nervous system of intensive care patients. Neurology. 2005;64:1348–53.
81 Vespa P, Boonyaputthikul R, McArthur DL, Miller C, Etchepare M, Bergsneider Met al. Intensive insulin therapy reduces microdialysis glucose values without altering glucose utilization or improving the lactate/pyruvate ratio after traumatic brain injury. Crit Care Med. 2006;34:850–6.
82 Oddo M, Schmidt JM, Carrera E, Badjatia N, Connolly ES, Presciutti M, et al. Impact of tight glycemic control on cerebral glucose metabolism after severe brain injury: a microdialysis study. Crit Care Med. 2008;36(12):3233–8.
83 Strong AJ, Smith SE, Whittington DJ, Meldrum BS, Parsons AA, Krupinski J, et al. Factors influencing the frequency of fluorescence transients as markers of peri-infarct depolarizations in focal cerebral ischemia. Stroke. 2000;31:214–22.
84 Hopwood SE, Parkin MC, Bezzina EL, Boutelle MG, Strong AJ. Transient changes in cortical glucose and lactate levels associated with peri-infarct depolarisations, studied with rapid-sampling microdialysis. J Cereb Blood Flow Metab. 2005;25:391–401.
85 Strong AJ, Hartings JA, Dreier JP. Cortical spreading depression: an adverse but treatable factor in intensive care? Curr Opin Crit Care. 2007;13:126–33.
86 Meierhans R, Béchir M, Ludwig S, Sommerfeld J, Brandi G, Haberthür C, et al. Brain metabolism is significantly impaired at blood glucose below 6 mM and brain glucose below 1 mM in patients with severe traumatic brain injury. Crit Care. 2010;14(1):R13.
87 Béchir M, Meierhans R, Brandi G, Sommerfeld J, Fasshauer M, Cottini SR, et al. Insulin differentially influences brain glucose and lactate in traumatic brain injured patients. Minerva Anestesiol. 2010;76(11):896–904.
88 Vespa PM, McArthur D, O’Phelan K, Glenn T, Etchepare M, Kelly D, et al. Persistently low extracellular glucose correlates with poor outcome 6 months after human traumatic brain injury despite a lack of increased lactate: a microdialysis study. J Cereb Blood Flow Metab. 2003;23(7):865–77.
89 Jaeger M, Soehle M, Meixensberger J. Effects of decompressive craniectomy on brain tissue oxygen in patients with intracranial hypertension. J Neurol Neurosurg Psychiatry. 2003;74(4):513–5.
90 Strege RJ, Lang EW, Stark AM, Scheffner H, Fritsch MJ, Barth H, Mehdorn HM. Cerebral oedema leading to decompressive craniectomy: an assessment of the preceding clinical and neuromonitoring trends. Neurol Res. 2003;25(5):510–5.
91 Jaeger M, Soehle M, Meixensberger J. Improvement of brain tissue oxygen and intracranial pressure during and after surgical decompression for diffuse brain oedema and space occupying infarction. Acta Neurochir Suppl. 2005;95:117–8.
92 Reithmeier T, Löhr M, Pakos P, Ketter G, Ernestus RI. Relevance of ICP and ptiO2 for indication and timing of decompressive craniectomy in patients with malignant brain oedema. Acta Neurochir (Wien). 2005;147(9):947–51.
93 Boret H, Fesselet J, Meaudre E, Gaillard PE, Cantais E. Cerebral microdialysis and P(ti)O2 for neuro-monitoring before decompressive craniectomy. Acta Anaesthesiol Scand. 2006;50(2):252–4.
94 Cooper DJ, Rosenfeld JV, Murray L, Arabi YM, Davies AR, D’Urso P, et al.; DECRA Trial Investigators; Australian and New Zealand Intensive Care Society Clinical Trials Group. Decompressive craniectomy in diffuse traumatic brain injury. N Engl J Med. 2011;364(16):1493–502.
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article was reported.