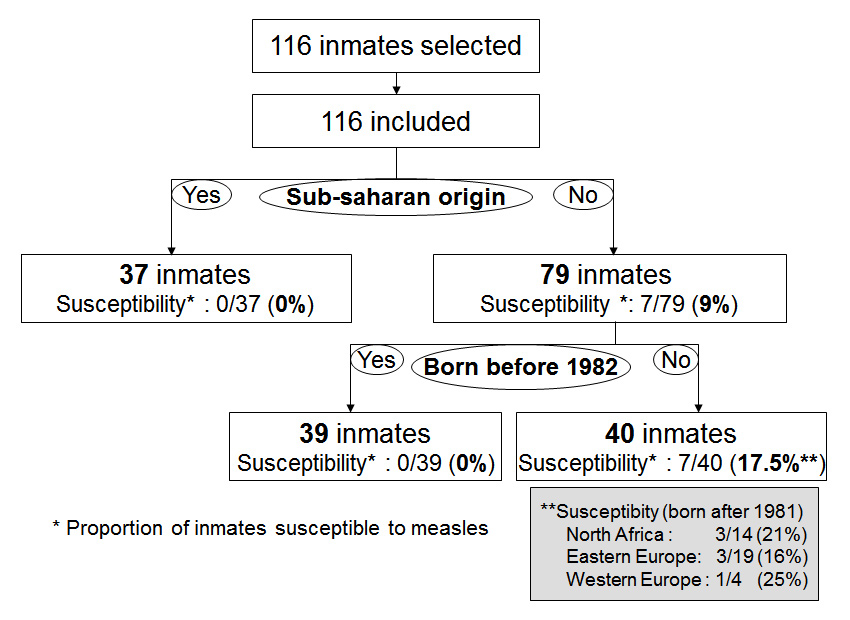
Figure 1
Flowchart: measles susceptibility according to origin and age in a pre-trial prison, 2009, Geneva, Switzerland.
DOI: https://doi.org/10.4414/smw.2011.13215
Measles is a highly contagious viral disease and the attack rate in susceptible exposed individuals is 75% [1]. Complications are more frequent if infection occurs during adulthood, leading to serious debilitation and even death [2–5].
In 1998, the World Health Organisation’s (WHO) member states adopted the goal of eradicating measles in Europe by 2010. However measles still persists on this continent despite the intensification of general vaccination campaigns. Switzerland has one of the poorest levels of immunisation coverage and one of the highest annual incidence rates of measles in Europe [6]. The current measles epidemic shows no sign of decline [7]. According to the WHO, target levels of susceptibility have been set for measles elimination in Europe with age group stratification. The target susceptibility for adults is set at 5% [8–10].
In Western Europe, before the beginning of mass vaccination programmes in the late 1960s, large and frequent outbreaks induced a high morbidity during childhood but led to excellent acquired immunity in adult populations. Mass vaccination reduced the amplitude of epidemics, but resulted in non-negligible susceptibility in adulthood since vaccination coverage is incomplete and unvaccinated people mostly remain non-immune. Unvaccinated people also often remain susceptible due to lowered virus circulation after a large-scale vaccination has been introduced [11]. Thus, it is well known that, in Western Europe, people born before 1963 have a high probability of being immune to measles contrary to younger people [7]. According to Coetze and De Jani, a similar trend exists in developing countries [12, 13]. However, we made the hypothesis that the cut-off date for increased susceptibility to measles is likely to be later than 1963 in developing countries since the implementation of vaccination campaigns started later and was less effective than in Western Europe.
The environmental and demographic characteristics in confined institutions, particularly in prisons, explain the high risk of measles epidemics. Large proportions of inmates are migrants who come from countries where vaccination coverage is low and whose susceptibility rates are unknown. Moreover, the potential for dissemination is high in overcrowded conditions [1, 14] and outbreaks of measles have been documented in various prisons in Western countries [15, 16]. It is important to identify specific groups at risk for measles and to tailor health information and preventative measures specifically for these groups. Catch-up vaccination campaigns among identified groups who are not immunised can dramatically close immunity gaps [17].
We aimed to estimate the susceptibility to measles and its risk factors among inmates in the largest Swiss pre-trial prison in order to estimate the risk of measles outbreaks and develop policies and guidelines for health services in prisons.
This cross-sectional study took place in April 2009 in Geneva, where Switzerland’s largest and most overcrowded (184% in 2009) pre-trial prison accommodates 540 prisoners, 243 prison officers and 37 health care workers.
In April 2009, the opportunity to investigate the susceptibility to measles was taken when all prisoners in contact with an index case of chickenpox, regardless of their origin or other criteria, had a blood test [18]. Measles IgG antibody titers were measured by enzyme-linked fluorescent assay (Vidas, BioMérieux). A structured questionnaire was used to collect self-reported information on socio-demographic characteristics (nationality, place of main schooling, year of arrival on the Western European Continent / in Switzerland) and questions related to history of measles and vaccination (Have you ever been infected by measles? Are you vaccinated against measles?). No vaccination card was available to ascertain immunisation status.
All inmates gave written consent. The study was approved by the ethical research committee (CER 09-137) of the University Hospitals of Geneva. Univariate analyses were used to assess risk factors associated with measles-susceptibility. Risk factors and confounders were established a priori. For age, the cut-off year (1981) corresponded to the start of widespread mass vaccination campaigns in various regions of the world (e.g. Balkans, North Africa). For sub-Saharan Africans, this cut-off was not adopted as large-scale vaccination campaigns were generally ineffective until the turn of the 21st century in their origin country. Categorical variables were statistically compared with chi-square test or Fisher’s exact test, when appropriate (using OpenEpi, version 2.3). In order to investigate the hypothesis postulating that people from sub-Saharan Africa, as well as older people from other regions have higher acquired immunity to measles, one-tailed tests were used. The presented 95% intervals for proportion are the so called exact (Clopper-Pearson) confidence interval (CI) calculation (Stata release 11, College Station, TX). A multivariate analysis was not feasible given the seroprevalence of 100% among those born before 1981, regardless of origin. We therefore proposed a stratified analysis according to age.
We identified 116 male inmates who had been in contact with the index case of chickenpox. All consented to participate in the study. As shown in table 1, median age was 27 years (range 20–57) and emigration from their country of origin occurred on average 6 years before incarceration (range 0–23). Africa and the Balkans were the main regions of origin, whereas a minority of inmates originated in Western Europe, Latin America or Asia.
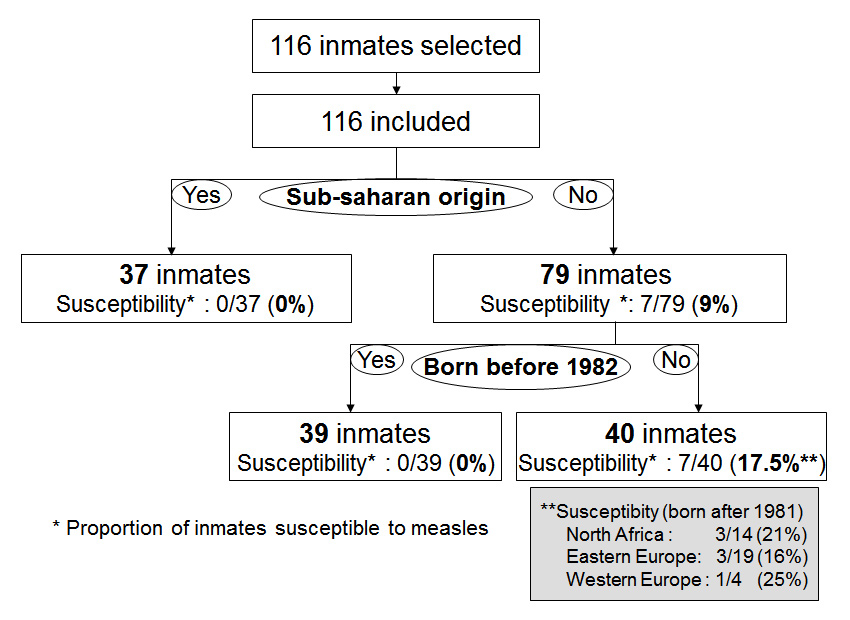
Figure 1
Flowchart: measles susceptibility according to origin and age in a pre-trial prison, 2009, Geneva, Switzerland.
This cross-sectional prevalence study identified a negative serology, hence a susceptibility to measles, for 7 out of 116 prisoners (6% CI95% 2.5–12.0).
All 37 inmates from sub-Saharan Africa were immune (CI95% 0–9.5) (table 2). Considering only people native from regions other than sub-Saharan Africa, 7 out of 40 inmates (18.5%, CI95% 7.3–32.8) born after 1981 were susceptible, whereas none of the 39 inmates born in 1981 or before (CI95% 0–9.0) were susceptible, which is a statistically significant difference (p = 0.006) (table 3). Susceptibility by origin was also significant when considering people from all regions (p = 0.034). The proportion of young people (born after 1981) was higher among inmates from sub-Saharan Africa (62%) than from other regions (51%). If age were a confounding factor, we would expect seroprevalence to be lower (not higher as was observed) in the sub-Saharan group (table 2).
All 17 inmates who reported a history of measles vaccination and all 13 with a positive self reported history of measles were immune. Seven responded positively to both questions. The positive predictive value (PPV) of these two questions was 100%.
A total of 46% of the prisoners were born before 1982 and only 3% before 1964. 32% were of sub-Saharan Africa origin. None had proof of vaccination (vaccination card). Swiss recommendations advocate 2 doses of vaccine for every person born after 1963, in the absence of proof of vaccination. Therefore, according to the Swiss immunisations guidelines, 97% of inmates should be vaccinated at entry. If detainees from countries outside Western Europe born before 1982 and all prisoners from sub-Saharan Africa were considered sufficiently immune against measles, only 35% of inmates would need measles immunisation (fig. 1). In our prison, for example, this 62% reduction of vaccinations for 3000 prisoners yearly would imply annual cost savings of 72’000 Euros.
| Table 1: Sociodemographic characteristics of 116 inmates in a pre-trial prison, 2009, Geneva, Switzerland. | |
| Factors | n (%) |
| Gender | |
| - Male | 116 (100%) |
| Age | |
| - Mean (SD) | 28.4 (7.1) |
| Duration of stay in Western Europe before incarceration* (years) | |
| - Mean (SD) | 6.6 (5.2) |
| Region of origin | |
| - Sub-Saharan Africa | 37 (31.9%) |
| - Balkans and Eastern Europe | 42 (36.2%) |
| - North Africa | 25 (21.6%) |
| - Western Europe (including 3 Swiss nationals) | 8 (6.9%) |
| - South America | 3 (2.6%) |
| - Asia | 1 (0.9%) |
| * Includes inmates originating outside Western Europe | |
| Table 2: Inmates’ susceptibility to measles by origin. Stratified analysis according to age in a pre-trial prison, 2009, Geneva, Switzerland. | |||||
| Age | Born in or before 1981 | Born after 1981 | |||
| Origin | IgG pos | IgG neg | IgG Pos | IgG neg | p |
| - Sub-Saharan Africa | 14 | 23 | 0.034 | ||
| - Other regions | 39 | 33 | 7 | ||
| Table 3: Inmates’ susceptibility to measles by age among inmates not native to sub-Saharan Africa in a pre-trial prison, 2009, Geneva, Switzerland. | ||||
| IgG+ n | IgG– n(%) | p | ||
| Age | ||||
| - Born in or before 1981 | 39 | 0.006 | ||
| - Born after 1981 | 33 | 7 (18.5%) | ||
| North Africa Balkans & Eastern Europe Western Europe | 3/19(16%) 3/14 (21%) 1/4 (25%) | |||
This is the first study of measles susceptibility in a prison setting and amongst adult migrants in Switzerland. In this rather young and cosmopolitan prison population, susceptibility to measles was fairly low (6%).
In our study, inmates susceptible to measles were only found among people born after 1981 and originating from regions other than sub-Saharan Africa. These results are coherent with the expected impact of vaccination campaigns according to the region of the world [19–24] and with the susceptibility observed among adult migrants in Canada [25].
Measles epidemiology varies greatly throughout the world. The origin of a person is an important factor to consider in institutions such as prisons where the majority of inmates come from countries outside of Western Europe. Depending on the region of the world, we can expect differences among age groups due to heterogeneity in the implementation of vaccination campaigns, particularly in terms of the timing of introduction and the level of vaccine uptake.
In the Balkans, vaccination campaigns against measles were implemented in the early 1970s. Although, vaccination coverage rates were below 90% for the first dose of measles in ex-Yugoslavia until the mid-1980s [19]. In this region, epidemics have virtually disappeared, giving way in recent years to a few resurgences within Rom populations whose vaccination coverage was low [19, 20]. In Northern Africa, large-scale measles vaccination campaigns started in the 1980s. In 1990, the immunisation coverage rate was 84% according to United Nations data [21]. This corroborates our findings: 16% and 21% of young adults from the Balkans and from Northern Africa, respectively, were susceptible whereas all older adults native from these regions were immune.
In our study, all people from sub-Saharan Africancountries were immune against measles. This reflects the fact that in most of these countries, large-scale vaccination campaigns were generally ineffective until the turn of the 21st century [22]. Poor vaccination coverage throughout the past century resulted in large-scale epidemics. Almost everyone was infected in childhood and thus acquired immunity. However, changes might be coming: in 2001, the countries of the WHO African Region took part in a global initiative aimed at reducing the number of measles deaths. Between 2001 and 2008, the estimated coverage for the first dose of measles vaccine increased from 57% to 73%. Concomitantly, the number of reported measles cases decreased by 93% [22]. Currently, all adult sub-Saharan African populations generally have excellent immunity regardless of age. However, even if the vaccination campaigns currently ongoing in sub-Saharan Africa continue to be effective, susceptibility to measles will probably paradoxically increase from 2020 onwards among unvaccinated, less exposed young adults.
Only few inmates in our prison were from Latin America or Asian countries. According to the analysis of the implementation of vaccination campaigns in these regions [23, 24], susceptibility among South American adult migrants is expected to be comparable to Northern African or Eastern European populations, and among Asians there is quite a similar situation to sub-Saharan Africans migrants.
Studies estimating the susceptibility to measles amongst adults in developing and transitional countries are scarce and incomplete. Only one study has investigated this parameter among immigrants. In a study on migrants and refugees in Canada, Greenaway reported heterogeneity depending on the regions of origin. For example, a significant difference of susceptibility was noticed between adults from the Balkans and Eastern Europe compared to adults from sub-Saharan Africa (8% versus 1%) [25].
We identified that all individuals who stated they had been vaccinated and/or had had measles were seropositive (PPV 100%). Nevertheless, recall bias has to be considered. The literature reports conflicting results: some studies suggest a positive correlation between history and seroprotection [26], while other studies report a lack of reliability for this information [27–29]. To our knowledge, no previous studies have evaluated this topic in prison settings. Confirmation of our observations would possibly further improve the targeting of susceptible populations.
A strength of this study is the ideal participation rate of 100% and the fact that an important health issue was investigated in an underserved population. Limitations relate to the sample size, which limits the power of the study, in particular the data concerning self-reported history of disease and vaccination. In addition, a multivariate analysis was not feasible because of seroprevalence of 100% in some subgroups. Nevertheless, our results were reinforced by a stratified analysis and are consistent with relevant data documented in the literature, particularly amongst migrants and refugees in Canada. This study consisted entirely of male participants. Results can therefore not be readily applied to females. Additionally, we studied a single facility in one country. Thus our findings may not necessarily be generalisable to other detention centres in other countries. Yet we hypothesise that the immunity profile described here would be comparable to other detention centres where the sociodemographic profile corresponds to that described here. The study population was similar to that of other pre-trial prisons in Switzerland, which are also characterised by high proportions of migrants (81.4%) and males (94%) [30]. Another limitation relates to the study design, as this was a convenience sample and not a random sample. Country of origin or age would not be possible to randomise, so the observational versus randomised statement is less relevant than the sampling method. Recruitment bias was probably minor as the prisoners included in the study concerned an entire section of the prison and represented one fifth of the prison population. Furthermore, all agreed to participate and no policy of attribution of cells according to the origin of the prisoners or any other criterion exists. Although the representativeness is not guaranteed for all Swiss prisons, the discussed reasons lead us to believe that this convenience sample was representative for the largest pre-trial prison in Switzerland.
Epidemiologic heterogeneity enables targeted measles vaccinations of people according to their region of origin and their age, particularly amongst migrant adults in confined institutions whose characteristics differ from the general population. This allows vaccination efforts to be focused on individuals with the highest risk in order to achieve optimal herd immunity, to reduce the risk of measles outbreaks and lower vaccination costs. Our case study of a Swiss prison suggests that measles vaccinations must be targeted specifically on adult migrants born after 1981 originating from transitional and developing countries outside sub-Saharan Africa. This is the current reality and will evolve in the future: for example from 2020, a catch-up vaccination should be proposed to young unvaccinated sub-Saharan African adults. Large-scale immunisation campaigns were initiated in 2001 in their home country and unvaccinated people often remain susceptible due to a lowered virus circulation after vaccination is introduced. This is the only data available in Switzerland concerning measles immunity among inmates. Data collection should be repeated and confirmed in larger studies with broader prison populations, including post-trial prisons. Standard guidelines continue to apply to all Western Europeans born after 1963. Strategies to update vaccination programmes for foreign-born adults must be developed. Efforts to improve immunity rates within the migrant populations not only limit the risk of outbreaks within closed institutions, but also help in protecting the community outside the prison.
The authors would like to thank the medical and nurses’ team as well as the director Mr Constantin Franziskakis of the prison Champ-Dollon for their active collaboration, Agnès Lehmann, Giuseppe Togni (Laboratory Unilabs, Geneva) and Dr Francesca Savioli for proofreading the manuscript.
1 Simpson RE. Infectiousness of communicable diseases in the household (measles, chickenpox, and mumps). Lancet. 1952;2(6734):549–54.
2 Van den Hof S, Conyn-van Spaendonck MA, van Steenbergen JE. Measles epidemic in the Netherlands, 1999–2000. J Infect Dis. 2002;186(10):1483–6.
3 Forni AL, Schluger NW, Roberts RB. Severe measles pneumonitis in adults: evaluation of clinical characteristics and therapy with intravenous ribavirin. Clin Infect Dis. 1994;19(3):454–62.
4 Wong RD, Goetz MB. Clinical and laboratory features of measles in hospitalized adults. Am J Med. 1993;95(4):377–83.
5 Ackerman Z, Ackerman E, Shouval D. Measles: clinical and laboratory observations in young adults during an epidemic. South Med J. 1988;81(11):1396–400.
6 Muscat M, Bang H, Wohlfahrt J, Glismann S, Molbak K. Measles in Europe: an epidemiological assessment. Lancet. 2009;373(9661):383–9.
7 Richard JL, Masserey S, V. Large measles epidemic in Switzerland from 2006 to 2009: consequences for the elimination of measles in Europe. Euro Surveill. 2009;14(50).
8 Ramsay M. A strategic framework for the elimination of measles in the European Region. Copenhagen: World Health Organization Regional Office for Europe (document EUR/ICP/CMDS 01 01 05). 1999.
9 Gay NJ. The theory of measles elimination: implications for the design of elimination strategies. J Infect Dis. 2004;189(Suppl 1):S27–S35.
10 Choi YH, Gay N, Fraser G, Ramsay M. The potential for measles transmission in England. BMC Public Health. 2008;8:338.
11 Bolker BM, Grenfell BT. Impact of vaccination on the spatial correlation and persistence of measles dynamics. Proc Natl Acad Sci U S A 1996;93(22):12648–53.
12 Coetzee N, Hussey GD, Visser G, Barron P, Keen A. The 1992 measles epidemic in Cape Town – a changing epidemiological pattern. S Afr Med J. 1994;84(3):145–9.
13 Jani JV, Holm-Hansen C, Mussa T, Zango A, Manhica I, Bjune G, et al. Assessment of measles immunity among infants in Maputo City, Mozambique. BMC Public Health. 2008;8:386.
14 Nouvelle vague de l’épidémie de rougeole en début d'année 2009: description et mesures. Bull OFSP. 2009;27:484–91.
15 Testa A. Spot on: measles and prison. Infection Inside. 2006;2(2).
16 Sprauer MA, Markowitz LE, Nicholson JK, Holman RC, Deforest A, Dales LG, et al. Response of human immunodeficiency virus-infected adults to measles-rubella vaccination. J Acquir Immune Defic Syndr. 1993;6(9):1013–6.
17 Steffens I, Martin R, Lopalco P. Spotlight on measles 2010: measles elimination in Europe – a new commitment to meet the goal by 2015. Euro Surveill. 2010;15(50).
18 Getaz L, Siegrist CA, Stoll B, Humair JP, Scherrer Y, Franziskakis C, et al. Chickenpox in a Swiss prison: susceptibility, post-exposure vaccination and control measures. Scand J Infect Dis. 2010;42(11-12):936–40.
19 Kaic B, Gjenero-Margan I, Kurecic-Filipovic S, Muscat M. A measles outbreak in Croatia, 2008. Euro Surveill. 2009;14(1).
20 Seguliev Z, Duric P, Petrovic V, Stefanovic S, Cosic G, Hrnjakovic IC, et al. Current measles outbreak in Serbia: a preliminary report. Euro Surveill. 2007;12(3):E070315.
21 Northern Africa makes strides towards most Millennium Development Goals. UN Department of Public Information MDG Report 2008[DPI/2517 O]. 2008.
22 Progress toward measles control – African region, 2001–2008. MMWR Morb Mortal Wkly Rep. 2009;58(37):1036–41.
23 Progress toward elimination of measles from the Americas. MMWR Morb Mortal Wkly Rep. 1998;47(10):189–93.
24 Global eradication of measles: Report by the Secretariat. Sixty-third World Health Assemble, Provisional agenda item 11 15 2010; A63/18.
25 Greenaway C, Dongier P, Boivin JF, Tapiero B, Miller M, Schwartzman K. Susceptibility to measles, mumps, and rubella in newly arrived adult immigrants and refugees. Ann Intern Med. 2007;146(1):20–4.
26 Ferson MJ, Robertson PW, Whybin LR. Cost effectiveness of prevaccination screening of health care workers for immunity to measles, rubella and mumps. Med J Aust. 1994;160(8):478–82.
27 Ziegler E, Roth C, Wreghitt T. Prevalence of measles susceptibility among health care workers in a UK hospital. Does the UK need to introduce a measles policy for its health care workers? Occup Med. (Lond) 2003;53(6):398–402.
28 Stover BH, Adams G, Kuebler CA, Cost KM, Rabalais GP. Measles-mumps-rubella immunization of susceptible hospital employees during a community measles outbreak: cost-effectiveness and protective efficacy. Infect Control Hosp Epidemiol. 1994;15(1):18–21.
29 Struewing JP, Hyams KC, Tueller JE, Gray GC. The risk of measles, mumps, and varicella among young adults: a serosurvey of US Navy and Marine Corps recruits. Am J Public Health. 1993;83(12):1717–20.
30 Swiss Federal Statistical Office. Prisons, pre-trial detention: data, indicators. http://www.bfs.admin.ch/bfs/portal/en/index/themen/19/03/05/key/untersuchungshaft.html. 2010.
Funding / potential competing interests: This work was supported by the Federal Office of Public Health (grant number 09.003678), Bern, Switzerland, and by the Medical Direction of the Geneva University Hospitals. No conflict of interest declared.