Smoking ban in the Alps – any wonder?
DOI: https://doi.org/10.4414/smw.2011.13219
Graubünden – heavily dependent on sport-oriented tourism – was one of the first Swiss cantons to adopt a workplace smoking ban also including the hospitality business. In this issue Bonetti et al. [1] confirm what they already observed one year after the ban [2]: compared to the two years prior to the ban, hospitalisations due to acute myocardial infarction (AMI) were 21% lower in the following two years (or 22% in the first year after the ban [2]).
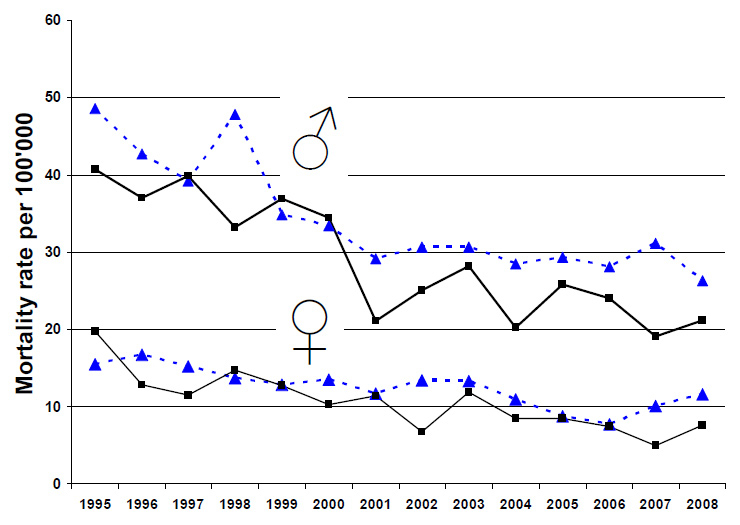
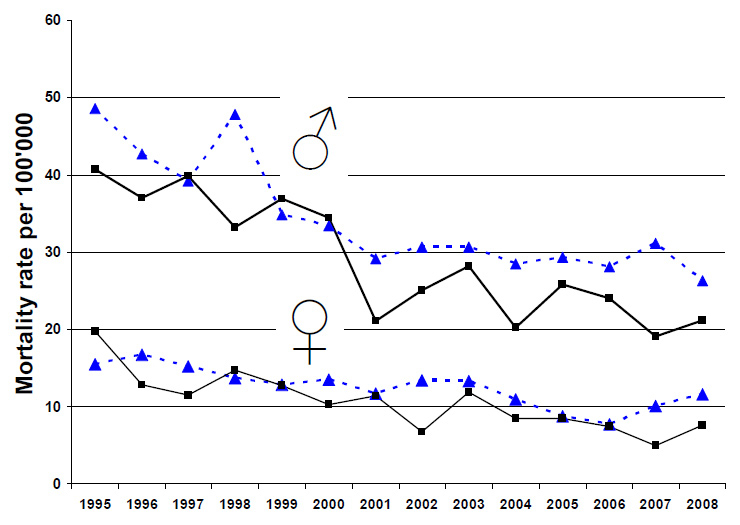
Figure 1
Age-standardised mortality rate (per 100'000 inhabitants) for myocardial infarction in the Cantons of Lucerne (triangles; dashed line) and Graubünden (squares; solid lines), 1995–2008, for men and women. Age standard: WHO world population. Mortality data: from death statistics of the Swiss Federal Statistical Office (FSO). Standardisation and graph: by Verena Jürgens, Swiss TPH Basel.
Can this reduction plausibly be considered a consequence of the smoking ban? The combustion of tobacco – exactly as the combustion of other biomasses – is associated with hundreds of toxic pollutants including large amounts of particulate matter (PM). Combustion-related PM have wide-ranging non-specific health effects [3]. Half a century ago, the lack of specificity of those effects was the subject of prolonged debate [4]. In the meantime these effects have become fully explicable by the prevailing biological paradigm that many chronic diseases share common pathological pathways [5]. The strong oxidative capacity of PM, the ability to induce local and systemic inflammation, myocardial hypoxaemia, clotting of the blood, and modulations in heart rate are just a few mechanisms which explain why even myocardial infarction rates correlate with PM exposure [6]. Best described is the dose-response curve for PM and mortality: the logarithm of the number of inhaled particles is linearly associated with mortality all across the range from low to moderate exposures to ambient PM or passive smoking, to the usually higher indoor exposures in households with biomass combustion, up to the extreme PM doses active smokers opt for [7–8].
But can the impact of a smoking ban be that large – 21%? Richiardi et al. derived all the necessary information from the best available scientific literature to predict the impact of smoking bans [9]. They reported a fall of 5–15%. A major source of variation in these estimates related to the time people are assumed to spend in smoky environments. The "average model" used 1 hr/day. This is close to the mean daily duration (1 hr 08 min) of secondhand smoking exposure out-of-home reported on any day by 48% of non-smokers in the Swiss city of Basel at times of no smoking bans [10]. Thus, the 21% fall observed in Graubünden seems to be substantially higher than expected. However, a systematic review of 11 observational studies concluded that smoking bans reduced AMI by 8–25% – an estimate more supportive of the Alpine results [11].
Should we believe risk prediction models or pre-/post-comparisons of AMI frequencies? Comparisons of aggregated crude data are prone to a broad range of biases that could result in over- orunderestimations of the true (unknown) attributable impact. In fact, in epidemiological science such “ecological studies” have a bad reputation similar to “case reports” in clinical research. The two-year follow-up made efforts to address some of the inherent limitations of the previous one-year assessment. Most importantly, the update compares results with the Canton of Lucerne. During the study period Lucerne had no smoking ban and AMI hospitalisations as reported to the Swiss AMI registry (AMIS [12]) increased some 20% per year. The population of Lucerne increased by 4.7% from 2006 to 2009, while Graubünden’s grew 2.1% over the same period, so population changes cannot fully account for differences between the cantons’ AMI frequency. Trends in age-adjusted mortality rates due to AMI were similar in the two cantons (fig. 1), showing a steady decrease from 1995 to 2001, particularly in men, with no strong patterns thereafter (fig. 1). This raises the question whether the Lucerne trend as observed in AMIS could be due in part to improved reporting compliance in the first years after joining the (voluntary) registry.
Trends in lipid-lowering treatment were very similar in both cantons, with no evidence of a sudden increase or fall that would coincide with the ban. There was neither a trend nor a sudden change in ambient air pollutants. Nor, however, was there an association between the monthly mean ambient pollution and the monthly frequency of AMI. As this is inconsistent with established evidence [6], does it indicate that the study is flawed altogether? Not exactly: with fewer than one AMI admission per day, and with very minor fluctuations in the monthly mean levels of PM10, it is not possible by the chosen analytic approach to confirm the well-known association between air pollution and AMI in this data set. The impact of the (low) air pollution in the Alps could instead be estimated from other studies: for example, the recently published comparison of triggers of AMI [13] leads to a crude rule-of-thumb that a 10 µg/m3 reduction in PM10 would result in a 2% reduction in AMI. This is far less than the fall observed after the smoking ban. However, a sustained 10 µg/m3 reduction in ambient PM would also reduce the development of chronic pathologies [14]; thus, the long-term benefit of a “ban on ambient air pollution” would be substantially larger than expected in the first year [15].
Does a smoking ban only prevent acute cardiovascular events or does it abate chronic pathologies such as atherosclerosis as well? The latter benefits would not be seen immediately, whereas acute effects would be expected from the first day of the regulation. Given the short time spent in smoky air [10] I would see the ban first and foremost as a strategy to remove an AMI trigger among non-smokers. The results of the study (fig. 2 in [1]) are in line with this thought as the fall was observed almost entirely among those with known cardiovascular problems, and restricted to non-smokers. Declines of AMI among smokers would rather be related to long-term benefits of a decrease in the amount of cigarettes smoked among smokers – a side effect of smoking bans observed elsewhere [11]. It would be interesting to know whether, when and how far the ban affected the smoking habits among smokers in Graubünden. Combining all relevant co-factors with data from AMIS – a visionary initiative for a voluntary registry taken in a country with no tradition of morbidity registries (http://www.amis-plus.ch/) – will provide opportunities to rigorously investigate and quantify the acute and long-term impact of the complex Swiss smoking ban landscape. Novel approaches may be applied to control for temporal and spatial trends. Such analyses may reveal to what extent the observed 21% fall in AMI can be attributed to the various consequences of the smoking ban.
However, the proposal for further research raises the question whether such confirmatory studies should still be done? And why should a scientific journal publish them, even with an invited commentary? Smoking bans are a highly effective, simple, and cheap structural prevention with public health benefits far exceeding the prevention of AMI [16]. However, structural prevention requires policies, and thus decisions of legislatures, governments, and the public – constituencies not necessarily motivated by public health concerns but heavily pressured by various lobbies spreading fictions as much as facts. As a result, Swiss Federal regulations came not only late (May 2010) but with the same loose ends and exceptions e.g., Spanish policies kept alive for several years. Only recently did Spain adopt the policy that works: a clear smoke-free policy applied to all workplaces, including big and small hospitality businesses [17–18]. In Switzerland there are currently 15 cantons, including Graubünden, with better policies than the Federal ones. A complicated policy carpet of partial and complete bans is spreading across the (often very small) 26 Swiss cantons. As some cantonal borders pass through local communities, policies may even differ as one crosses the street. But Swiss lawmakers are unlikely to go for more consistent policies. Thus, >130'000 people have signed an initiative asking for clear science-based Federal policies. The ballot is pending (http://www.rauchfrei-ja.ch/). In such a climate it is indeed important to monitor pre/post changes despite inherent weaknesses and the limited "novelty factor" of such confirmatory exercises. Confirming "the obvious" with less than perfect local data is – unfortunately – often more important for local policymakers than some "rocket science" done elsewhere. Studies from abroad have received far less attention while reactions to data from the Alps were – and will again – trigger committed discussions. Populist media will of course weigh in with arguments originating from the gut rather than the brain [19] and weaknesses of the follow-up study will be highlighted with the (false) notion that methodological flaws would always lead to false positive findings. However, pseudoscientific uproars are unlikely to turn public opinion round. According to surveys done in 14 countries and the many successes of canton-based initiatives in Switzerland, it is fairly clear that many societies have overcome the smoky fashions of the 20th century and now defend the pleasure of smoke-free public environments [20–21]. A Swiss smoking ban was estimated to reduce health costs by some 330 Mio. Swiss francs – certainly good news at times of constantly increasing health care costs [22]. A solid majority that values the protection of health and wellbeing more than the ill-defined "freedom" or "right" to harm others will prevail.
No wonder! A fresh meal with a good glass of wine tastes far better in a smoke-free environment – not only in Graubünden!
References
1 Bonetti PO, Trachsel L, Kuhn MU, et al. Incidence of acute myocardial infarction after implementation of a public smoking ban in Graubünden, Switzerland: 2-year follow-up. Swiss Med Weekly. 2011;in press.
2 Trachsel LD, Kuhn MU, Reinhart WH, Schulzki T, Bonetti PO. Reduced incidence of acute myocardial infarction in the first year after implementation of a public smoking ban in Graubuenden, Switzerland. Swiss Med Wkly. 2010 Jan 12.
3 Künzli N, Perez L, Rapp R. Air Quality and Health. Lausanne, Switzerland: ERS; 2010 September 2010.
4 Poole C. On the origin of risk relativism. Epidemiology. 2010;21(1):3–9.
5 Probst-Hensch NM. Chronic age-related diseases share risk factors: do they share pathophysiological mechanisms and why does that matter? Swiss Med Wkly. 2010;140:w13072.
6 Brook RD, Rajagopalan S, Pope CA, 3rd, et al. Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation. 2010;121(21):2331–78.
7 Pope CA, 3rd, Burnett RT, Krewski D, et al. Cardiovascular mortality and exposure to airborne fine particulate matter and cigarette smoke: shape of the exposure-response relationship. Circulation. 2009;120(11):941–8.
8 Smith KR, Peel JL. Mind the gap. Environ Health Perspect 2010;118(12):1643–5.
9 Richiardi L, Vizzini L, Merletti F, Barone-Adesi F. Cardiovascular benefits of smoking regulations: The effect of decreased exposure to passive smoking. Prev Med. 2009;48(2):167–72.
10 Schweizer CB-O, L; Edwards, RD; Gaudermann, J; Ilacqua, V; Jantunen, MJ; Lai, HK; Nieuwenhuijsen, M; Künzli, N;. Indoor time-microenvironment-activity patterns in seven regions of Europe. J Exp Anal Environ Epidemiol. 2007;17:170–81.
11 Meyers DG, Neuberger JS, He J. Cardiovascular effect of bans on smoking in public places: a systematic review and meta-analysis. J Am Coll Cardiol. 2009;54(14):1249–55.
12 Urban P, Bernstein M, Costanza MC, Simon R, Frey R, Erne P. An internet-based registry of myocardial infarction in Switzerland. Kardiovask Med. 2003 2000;3:430–40.
13 Nawrot TS, Perez L, Kunzli N, Munters E, Nemery B. Public health importance of triggers of myocardial infarction: a comparative risk assessment. Lancet. 2011;377(9767):732–40.
14 Perez L, Rapp R, Kunzli N. The Year of the Lung: outdoor air pollution and lung health. Swiss Med Wkly. 2010;140:w13129.
15 Ballester F, Medina S, Boldo E, et al. Reducing ambient levels of fine particulates could substantially improve health: a mortality impact assessment for 26 European cities. J Epidemiol Community Health. 2008;62(2):98–105.
16 Goodman PG, Haw S, Kabir Z, Clancy L. Are there health benefits associated with comprehensive smoke-free laws. Int J Public Health. 2009;54(6):367–78.
17 Schikowski T, Kunzli N. A little bit is not good enough: comprehensive smoking control is needed. Int J Public Health. 2009 Oct 27.
18 Lopez MJ. The Spanish smoking law: a model to be followed? Int J Public Health. 2010;55(3):231–2.
19 Stadler B. Es ist ein Wunder. Weltwoche. 2010;14. Januar: 13.
20 Halpern MT, Taylor H. Beliefs regarding smoking in the workplace: results from the Global Workplace Smoking Survey. Int J Public Health. 2009;54(6):391–401.
21 Lazuras L, Rodafinos A, Panagiotakos DB, Thyrian JR, John U, Polychronopoulos E. Support for smoke-free policies in a pro-smoking culture: findings from the European survey on tobacco control attitudes and knowledge. Int J Public Health. 2009;54(6):403–8.
22 Hauri DD, Lieb CM, Rajkumar S, Kooijman C, Sommer HL, Roosli M. Direct health costs of environmental tobacco smoke exposure and indirect health benefits due to smoking ban introduction. Eur J Public Health. 2011;21(3):316-22.