Incidence of acute myocardial infarction after implementation of a public smoking ban in Graubünden, Switzerland: Two year follow-up
DOI: https://doi.org/10.4414/smw.2011.13206
Summary
QUESTION UNDER STUDY: In the first year after implementation of a public smoking ban a significant decrease in the incidence of acute myocardial infarction (AMI) was observed in Graubünden. In the present study we analyzed the incidence of AMI in the second year of the ban. In addition, we investigated the contribution of smoking ban-unrelated factors to the reduced incidence of AMI incidence observed after enactment of the ban.
METHODS: Data of all AMI patients who underwent coronary angiography at the Kantonsspital Graubünden, the only tertiary care hospital with a cardiac catheterization laboratory in Graubünden, between March 1st, 2009 and February 28th, 2010 were collected prospectively. Data were compared with those of the three preceding 12-month periods. We also estimated AMI incidence during the corresponding time period in Lucerne, a region with no smoke-free legislation, using data of the AMIS Plus registry. The influence of outdoor air pollution was analyzed with the help of official measurements of PM10- and NO2-concentrations in Graubünden. The prescription of lipid-lowering drugs was estimated by using sales figures in Graubünden and Lucerne.
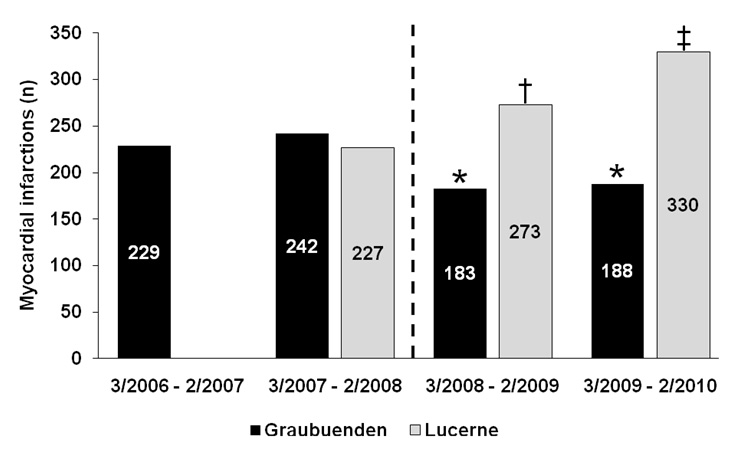
RESULTS: In Graubünden, the number of patients with AMI in the second year after adoption of the smoking ban was similar to that in the first year of the ban (188 vs. 183; P= ns) and significantly lower than in each of the two years preceding the ban (229 and 242, respectively; P<0.05 vs. each of the 12-month periods after the ban). Overall, the number of AMI patients in the two post-ban years was 21% lower than in the two pre-ban years. The reduction in the number of patients with AMI was most pronounced in non-smokers and individuals with known coronary artery disease. During the corresponding time period, no similar decrease in the incidence of AMI was observed in Lucerne. No association was found between the magnitude of outdoor air pollution and the incidence of AMI. During the observation period, the use of lipid-lowering drugs increased similarly in Graubünden and Lucerne.
CONCLUSIONS: Compared with the two years preceding the implementation of a smoking ban, the incidence of AMI remained significantly reduced in the second year of the ban in Graubünden, whereas no similar reduction was seen in a comparable area without smoke-free legislation. Changes in outdoor air pollution or the use of lipid-lowering drugs did not substantially contribute to the decrease in the incidence of AMI that occurred after adoption of the ban in Graubünden.
Introduction
Passive smoking is associated with an increased risk of coronary artery disease (CAD) and acute myocardial infarction (AMI) [1, 2]. Multiple studies in various countries indicated that reducing the exposure to second hand smoke (SHS) by implementation of regulations to ban smoking in public buildings is followed by a rapid reduction in the number of hospital admissions for acute coronary syndromes [3–7]. In line with these studies, we observed a significant decrease in the number of AMI patients admitted to our hospital in the first year after smoke-free legislation had been adopted on March 1st, 2008 in the Canton Graubünden, Switzerland [8].
However, despite the growing body of evidence from observational studies suggesting a beneficial effect of public smoking bans on the risk of AMI, the proof of a causal relationship between smoking bans and the reduction of AMI rates observed after their implementation remains challenging. Indeed, individual “before and after” studies are hampered by the fact that time trends of acute coronary syndrome incidence may be affected by various factors other than SHS exposure. Natural fluctuation of AMI rates, a general trend towards a lower AMI risk over time, variation of the size of the population at risk and changes in preventive measures (e.g. prevalence of lipid-lowering therapy) represent examples for such smoking ban-unrelated factors. Given the well-established association between air pollution and cardiovascular events, a reduction in outdoor particulate matter concentrations might also contribute to the decrease in the incidence of AMI observed after enactment of public smoking bans [9, 10].
Therefore, we performed the present analysis in order to further elucidate the influence of such smoking ban-unrelated factors, including air pollution and lipid-lowering therapy, on the incidence of AMI after implementation of smoke-free legislation in Graubünden.
Patients and methods
Setting and study population in Graubünden
Details on the Canton Graubünden and its medical logistics have been reported previously [8]. In brief, Graubünden covers an area of 7106 km2 and has a resident population of 190,000. Graubünden represents the largest holiday destination of Switzerland, recording approximately six million tourist overnight stays every year.
The Kantonsspital Graubünden serves as a tertiary care hospital possessing the only cardiac catheterization laboratory in Graubünden and offers a 24-hour emergency service for primary percutaneous coronary intervention for AMI patients in Graubünden. Based on current treatment guidelines, coronary angiography is recommended in all patients with AMI. Given a well functioning network including all hospitals of Graubünden and excellent transportation capacities either by ambulance or by helicopter, patients experiencing an AMI in Graubünden are transferred to the Kantonsspital Graubünden for either acute (patients with STEMI or unstable patients with NSTEMI) or early (other patients with NSTEMI) coronary angiography. Hence, the vast majority of AMI patients admitted to one of the hospitals in Graubünden undergo coronary angiography at the Kantonsspital Graubünden during their index hospitalization. Therefore, the number of AMI patients undergoing coronary angiography at the Kantonsspital Graubünden may be viewed as representative for the overall incidence of AMI in Graubünden.
Data of all patients who suffered from an AMI in Graubünden and underwent coronary angiography at the Kantonsspital Graubünden within the first and second year after implementation of the public smoking ban (between March 1st, 2008 and February 28th, 2010) were collected prospectively. These data were compared with those of all patients who had suffered from an AMI in Graubünden and had undergone coronary angiography at our hospital during the two corresponding 12 month time periods preceding implementation of the public smoking ban (between March 1st, 2006 and February 28th, 2007, and between March 1st, 2007 and February 29th, 2008, respectively), whereby these patients were identified by their diagnoses at hospital discharge (ICD-10 codes) and by analyzing various local databases (coronary angiography database, intensive care unit database). According to the universal definition of myocardial infarction, AMI was defined as a detectable level of cardiac troponin in a clinical setting consistent with myocardial ischaemia [11].
Setting and study population at the comparison site Lucerne
To investigate possible general temporal trends affecting the incidence of AMI in Switzerland, we also assessed the number of patients hospitalized because of AMI in the Canton Lucerne. Importantly, in Lucerne no smoke-free legislation existed until a nationwide regulation was enacted on May 1st, 2010. The Canton Lucerne covers an area of 1493 km2 and has a resident population of 368,000.
To estimate the incidence of AMI in Lucerne, data of the Acute Myocardial Infarction and Unstable Angina in Switzerland (AMIS Plus) registry, a large nationwide prospective registry of patients with acute coronary syndromes admitted to Swiss hospitals, were used. The structure and design of this registry have been reported recently [12]. Since January 1st, 2007, all three public hospitals in the Canton Lucerne (LUKS Luzern, LUKS Sursee, LUKS Wolhusen) participated in the AMIS Plus registry, providing comparison data on the incidence of AMI in Lucerne for the last three 12 month observation time periods of our study.
Assessment of air quality in Graubünden
As a measure of outdoor air pollution, concentrations of particulate matter with an aerodynamic diameter of less than 10 mm (PM10) and of nitrogen dioxide (NO2) are regularly monitored by the Department of Nature and Environment (Amt für Natur und Umwelt Graubünden) at different sites in Graubünden. For two distinct measuring sites located at the main traffic axis (Chur and Rothenbrunnen) virtually continuous data of daily PM10- and NO2-concentrations since September 2006 are available ( http://www.gr-luft.ch ). Based on these data, we estimated the magnitude of average monthly outdoor air pollution in Graubünden by calculating average concentrations of PM10 and NO2 for every month from September 2006 to February 2010.
Assessment of sales figures of lipid lowering drugs
Data on sales figures of lipid-lowering drugs (statins, ezetimibe, fibrates, nicotinic acid, ion-exchange resins) in Graubünden and Lucerne were provided by IMS Health GmbH, Switzerland.
Statistical analysis
In order to compare the numbers of AMI cases between the four 12 month time periods, 2 x 2 tables were set up to check for equal distribution. Pearson’s correlation test was used to investigate a possible relationship between monthly incidence of AMI and the magnitude of average monthly ambient air pollution. A P-value of <0.05 was considered statistically significant. Statistical analyses were performed using STATISTICA software, version 8.0 (StatSoft Inc., Tulsa, OK, USA).
Results
In Graubünden, the number of patients with AMI in the second year after adoption of the smoking ban was similar to that in the first year of the ban and significantly lower than in each of the two years preceding the ban (fig. 1). Some of the data had already been published in our first report [8]. Overall, the number of patients with AMI was 21% lower in the two years after implementation of the ban compared with the two year period preceding the ban.
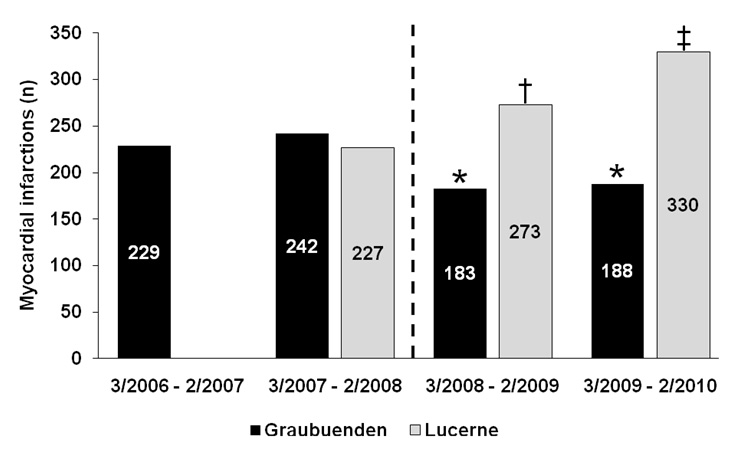
Figure 1
Numbers of myocardial infarctions in Graubünden (black bars) and Lucerne (grey bars) in the year(s) before and the years after implementation of a public smoking ban in Graubünden (dashed line). Note that no data were available for Lucerne for the first 12-month period because not all public hospitals in Lucerne participated in the AMIS Plus registry at that time. * P<0.05 vs. each of the 2 previous 12-month periods in Graubünden. † P<0.05 vs. the previous 12-month period in Lucerne. ‡ P<0.05 vs. each of the 2 previous 12-month periods in Lucerne.
In contrast to Graubünden, no decrease in the incidence of AMI was observed in Lucerne after March 1st 2008. On the contrary, the number of AMI patients in Lucerne increased during the two corresponding 12 month periods in which the smoking ban was effective in Graubünden (fig. 1).
The number of myocardial infarctions in the four 12 month study periods in various populations in Graubünden is shown in figure 2. Similar to the first year (reported previously [8]), the decrease in the incidence of AMI in the second year of the ban was limited to non-smokers, whereas the number of smokers presenting with AMI was similar before and after enactment of smoke-free legislation. The number of female AMI patients showed a more pronounced drop in the second year of the ban than during the first year. In contrast, the magnitude of the decrease in the incidence of AMI in male patients diminished in the second year of the ban compared with the previous year. Overall, however, when compared with the average of the two years preceding the ban a significant reduction in both male (–18%; P<0.05) and female (-30%; P<0.05) AMI patients could be observed in the 24 months following implementation of the ban. The numbers of resident patients with AMI were virtually identical in both post-ban years. Population-based incidences of AMI were 89.4, 93.8, 69.8, and 68.8 per 100000 residents in the four consecutive 12-month observation periods, respectively. On the other hand, the number of non-resident AMI patients was somewhat higher in the second year after adoption of the ban compared with the first post-ban year despite a similar number of visitor overnight stays in all 12 month observation periods (indexed incidences of AMI in non-residents during the four 12 month observation periods: 10.5, 10.8, 8.3, and 9.6 per million visitor overnight stays). When taking both pre- and post-ban 12 month observation periods together, overall reduction in AMI incidence was primarily caused by a significant 23% decrease in the number of AMIs in the resident population, whereas no significant reduction was present in non-residents. In both post-ban years, the most pronounced reduction in the number of AMIs was found in patients with documented CAD, including those with prior AMI and prior percutaneous coronary intervention and/or coronary artery bypass graft surgery.
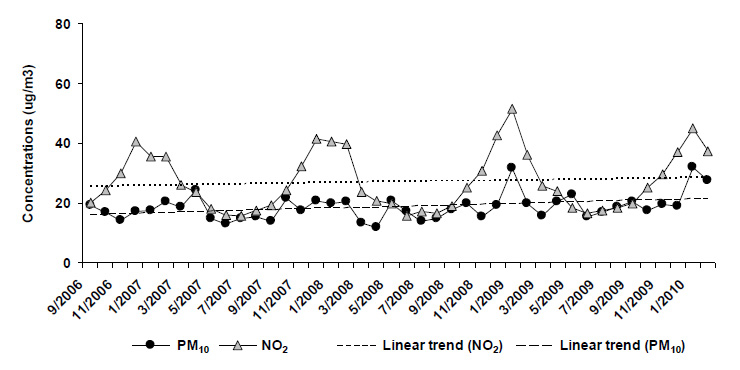
Markers of outdoor air pollution (PM10 and NO2) measured in Graubünden showed typical annual variability with peak values in the winter months during the entire observation period (fig. 3). Overall, concentrations of air pollutants tended to slightly increase over the years. There was no relationship between the magnitude of monthly AMI rates and average monthly PM10- or NO2-concentrations (r = 0.211, P= 0.181 for PM10; r = 0.251, P= 0.109 for NO2).
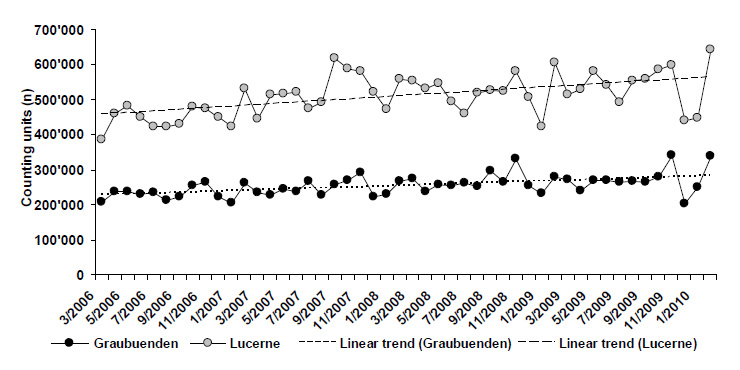
Sales figures of lipid-lowering drugs increased similarly in Graubünden and Lucerne during the study period (fig. 4).
Discussion
The present study extends and confirms our previous observation [8] of a significant decrease in the incidence of AMI up to two years after the implementation of a public smoking ban in Graubünden. Similar to the first year after enactment of the ban, the decrease in the number of patients with AMI in the second year after introduction of the ban was limited to non-smokers and the most pronounced reduction was observed in individuals with established CAD. Moreover, our results suggest that smoking ban-unrelated factors such as natural variability of AMI incidence, a general Swiss trend towards a lower incidence of AMI over the last years, a reduction of the magnitude of outdoor air pollution and prescription of lipid-lowering drugs cannot explain the decrease in the incidence of AMI observed after implementation of a public smoking ban in Graubünden.

Figure 2
Numbers of myocardial infarctions in various subpopulations in Graubünden in the two 12-month periods before (3/2006 – 2/2007 and 3/2007 – 2/2008) and the two 12-month periods after (3/2008 – 2/2009 and 3/2009 – 2/2010) implementation of a public smoking ban. * P<0.05 vs. each of the two 12-month periods preceding the ban. CAD, coronary artery disease; AMI, acute myocardial infarction; PCI, percutaneous coronary intervention; CABG, coronary artery bypass graft surgery.
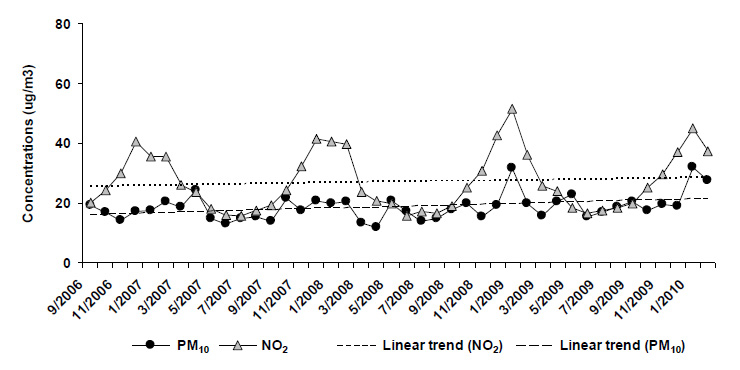
Figure 3
Average monthly outdoor concentrations of PM10 and NO2 in Graubünden from September 2006 to February 2010. The dashed lines show the overall trends in the concentrations of the respective parameter over time.
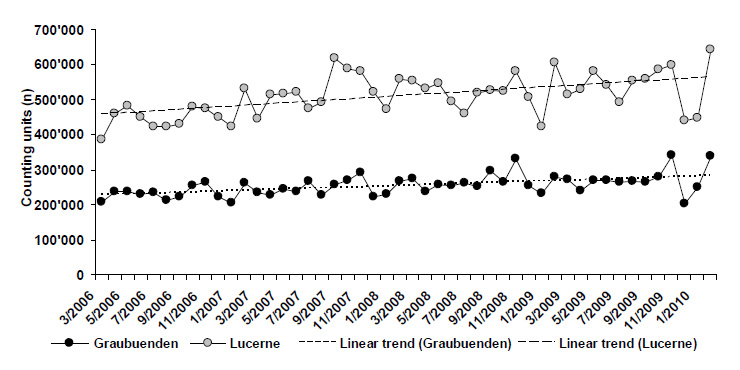
Figure 4
Numbers of lipid-lowering drugs (counting units; tablets) sold in Graubünden and Lucerne from March 2006 to February 2010. The dashed lines show the overall trends in sales figures for the respective region over time. (Data are courtesy of IMS Health GmbH, Switzerland)
In our analysis we found that the number of patients with AMI admitted to the Kantonsspital Graubünden was virtually identical in the first and the second year after implementation of the public smoking ban and was significantly lower than in each of the two years preceding the adoption of smoke-free legislation. Thus, the relatively stable AMI rates in the two years before and the two years after implementation of the ban, respectively, suggest that the significant decrease in the number of AMI patients observed in the first post-ban year [8] was not primarily caused by a more pronounced natural annual fluctuation of AMI rates.
In order to rule out a general trend towards a decrease in the incidence of AMI in Switzerland, we assessed the number of patients who were hospitalized with a diagnosis of AMI between March 1st, 2007 and February 28th, 2010 in the Canton Lucerne, a Swiss area without smoke-free legislation until May 1st, 2010. Based on data from the AMIS Plus registry, an increase rather than a decrease in the AMI incidence was found in Lucerne during the observation period, arguing against the presence of a general trend towards a lower incidence of AMI in Switzerland during the last years.
Despite the well-known association between air pollution and the risk of cardiovascular events [9, 10], we found no relationship between the incidence of AMI and the magnitude of outdoor PM10- or NO2-concentrations in our study. However, it must be emphasized that although parameters of air quality were assessed along the main traffic axis of Graubünden, Swiss national maximal daily limits for PM10 (50 ug/m3) and NO2 (80 ug/m3) were only rarely exceeded during the observation period. Thus, given the rather low overall degree of air pollution observed during the study period, it may be speculated that, compared with urban areas, air pollution does not represent a major contributor to the risk of AMI in rural and mountainous Graubünden.
Dyslipidaemia represents one of the most important risk factors for CAD and lipid-lowering therapy was convincingly shown to reduce the risk of cardiovascular events in both primary and secondary prevention [13, 14]. Thus, it is conceivable that broadening the prescription of lipid-lowering drugs would also translate into a decrease in the incidence of AMI in the respective population. In Graubünden, however, the sales figures of lipid-lowering drugs increased slowly and steadily during the observation period and there was no step-wise change in 2008, which could explain the sudden decrease in the number of patients with AMI observed after March 1st, 2008. Furthermore, the fact that sales figures of lipid-lowering drugs showed a similar increase during the same time period in Lucerne, where no decrease in the incidence of AMI was noted, argues against a correlation between the prescription rate of lipid-lowering drugs and the decrease in the risk of AMI observed after enactment of the smoking ban in Graubünden.
Two recently published meta-analyses [3, 4] concluded that there is a significant positive relationship between the duration of a smoking ban and the reduction in the incidence of AMI. This conclusion was based on two US-studies with a follow-up duration of three years [15, 16]. In our study, no further reduction in the incidence of AMI was observed in the second year of the ban. About the reasons for this lack of an additional benefit with time can be speculated. According to local authorities, compliance with the smoking ban has been good since its implementation in Graubünden on March 1st, 2008. However, given the consistent but quite variable early benefit of smoking bans in different populations [3], it is possible that population-dependent factors might also affect the magnitude of the long-term benefit of such bans. On the other hand, given the rather small number of cases in our study, the possibility that slight natural fluctuations of AMI incidence might have masked a further reduction in AMI incidence in the second year of the ban must also be taken into account.
Our analysis has some limitations. First of all, it must be emphasized that our observational results do not allow the inference of a causal relationship between the implementation of a smoking ban and the reduction of AMI incidence observed thereafter. However, by ruling out a substantial effect of various smoking ban-unrelated factors on the incidence of AMI in Graubünden and together with the ever growing number of observational studies showing a decrease in the rates of AMI after enactment of smoke-free legislation all over the world, our results suggest that such a relationship does, indeed, exist.
Our analysis is limited to a relatively small area and population and, thus, a relatively low number of AMI cases. As a consequence, small differences in the numbers of cases among the different time periods may result in large percentage differences. Thus, the magnitude of the relative reduction in the number of AMI patients overall and in the various subgroups observed in the two years after implementation of the ban must be interpreted with caution. However, it must also be emphasized that despite the relatively low number of cases a statistically significant difference with regard to the number of AMI cases before and after implementation of the ban was found even in some rather small subgroups (e.g. patients with known CAD).
The incidence of AMI in Lucerne was estimated using data of the AMIS Plus registry, a large, prospective national registry endorsed by the Swiss Societies of Cardiology, Internal Medicine and Intensive Care [12]. The AMIS Plus registry collects data on the whole spectrum of patients with acute coronary syndrome from voluntarily participating hospitals of different sizes including all three public hospitals in the Canton of Lucerne. Participating centres are strongly encouraged to enrol all patients fulfilling the inclusion criteria to avoid selection bias. However, given the fact that participation is voluntary, a certain selection bias cannot be ruled out. Thus, the absolute numbers of AMIs reported in Lucerne must be interpreted with caution. Nevertheless, the magnitude of the increase in the number of patients with AMI in Lucerne over the last three 12 month periods in Lucerne argues against a general nationwide downward trend of AMI incidence during the last years.
In summary, the results of the present analysis further support the assumption that the implementation of a public smoking ban itself was the leading cause for the decrease in the number of patients with AMI observed after adoption of smoke-free legislation in Graubünden. Thus, together with recently published data from Canada, England and the USA [5–7], our data contribute to the growing body of evidence indicating that reducing SHS exposure by implementation of public smoking bans represents an effective method to reduce the risk of AMI in the general population.
References
1 Barnoya J, Glantz SA. Cardiovascular effects of second hand smoke: nearly as large as smoking. Circulation. 2005;111(20):2684–98.
2 He J, Vupputuri S, Allen K, Prerost MR, Hughes J, Whelton PK. Passive smoking and the risk of coronary heart disease – a meta-analysis of epidemiologic studies. N Engl J Med. 1999;340(12):920–6.
3 Meyers DG, Neuberger JS, He J. Cardiovascular effect of bans on smoking in public places. J Am Coll Cardiol. 2009;54(14):1249–55.
4 Lightwood JM, Glantz SA. Declines in acute myocardial infarction after smoke-free laws and individual risk attributable to second hand smoke. Circulation. 2009;120(14):1373–9.
5 Naiman A, Glazier RH, Moineddin R. Association of anti-smoking legislation with rates of hospital admission for cardiovascular and respiratory conditions. CMAJ. 2010;182(8):761–7.
6 Sims M, Maxwell R, Bauld L, Gilmore A. Short term impact of smoke-free legislation in England: retrospective analysis of hospital admissions for myocardial infarction. BMJ. 2010;340:c2161.
7 Herman PM, Walsh ME. Hospital admissions for acute myocardial infarction, angina, stroke, and asthma after implementation of Arizona’s comprehensive statewide smoking ban. Am J Public Health. Published online ahead of print May 13, 2010.
8 Trachsel LD, Kuhn MU, Reinhart WH, Schulzki T, Bonetti PO. Reduced incidence of acute myocardial infarction after implementation of a public smoking ban in Graubünden, Switzerland. Swiss Med Wkly. 2010;140(9–10):133–8.
9 Brook RD, Franklin B, Cascio W, Hong Y, Howard G, Lipsett M, et al. Air pollution and cardiovascular disease. A statement for healthcare professionals from the expert panel on population and prevention science on the American heart association. Circulation. 2004;109(21):2655–71.
10 Sun Q, Hong X, Wold LE. Cardiovascular effects of ambient particulate air pollution exposure. Circulation. 2010:121(25);2755–65.
11 Thygesen K, Alpert JS, White HD on behalf of the joint ESC/ACCF/AHA/WHF Task Force for the Redefinition of Myocardial Infarction. Universal definition of myocardial infarction. Eur Heart J. 2007;28:2525–38 and Circulation. 2007;116(22):2634–53.
12 Radovanovic D, Urban P, Simon R, Schmidli M, Maggiorini M, Rickli H, et al; AMIS Plus Investigators. Outcome of patients with acute coronary syndrome in hospitals of different sizes. A report from the AMIS Plus Registry, Swiss Med Wkly. 2010;140(21–22):314–22.
13 National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106(25):3143–421.
14 Grundy SM, Cleeman JI, Merz CN, Brewer HB, Clark LT, Hunninghake DB, et al; for the Coordinating Committee of the National Cholesterol Education Program; Endorsed by the National Heart, Lung, and Blood Institute, American College of Cardiology foundation, and American Heart Association. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004;110(2):227–39.
15 Centers for Disease Control and Prevention. Reduced hospitalizations for acute myocardial infarction after implementation of a smoke-free ordinance. City of Pueblo, Colorado, 2002–2006. MMWR Morb Mortal Wkly Rep. 2009;57(51):1373–7.
16 Khuder SA, Milz S, Jordan T, Price J, Sivestri K, Butler P. The impact of a smoking ban on hospital admissions for coronary artery disease. Prev Med. 2007;45(1):3–8.