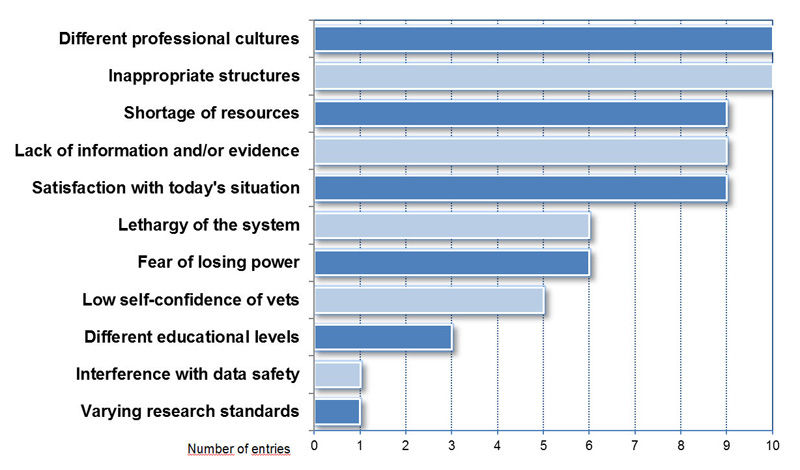
Figure 1
Differentiation of barriers against implementation of One Health in Switzerland (N = 69).
DOI: https://doi.org/10.4414/smw.2011.13201
“A better collaboration between physicians and veterinarians would prevent such outbreaks in the future.” This statement was made in 1983 on a Q-fever epidemic in Valais, Switzerland, involving 415 human cases and infection in sheep flocks [1]. In 2009 the Dutch media reported a Q-fever outbreak originating from goats and affecting over 2000 human patients. Again, 26 years later, professionals and the public are complaining of the lack of communication between the veterinary and human medical professions [2]. An international conference entitled „One Health in relation to Q-fever“ was subsequently organised in the Netherlands with the aim of strengthening cooperation between the two sectors [3]. One Health postulates the indivisibility of health as a public good: the inextricable interdependences between the health of humans, animals and the ecosystem justify a more open and intensive dialogue among all the relevant sectors. One Health can be seen as a metaphor of a common umbrella for targeted inter- and transdisciplinary cooperation in aid of better health with remarkable added value. Facing the world's increasingly complex changes, more than 650 participants in the 1st International One Health Congress in Melbourne, Australia, in February, 2011 [4], demonstrated their commitment to improved and more intensive cooperation.
One Health is currently in a process of dynamic development, although it involves the revival of traditionally accepted cooperation models rather than a new idea. According to Kahn et al. [5, 6], Rudolf Virchow was the first to rebuild a bridge over the divide between human and animal medicine. Calvin Schwabe used the term “One Medicine” in his book “Veterinary Medicine and Human Health” [7]. In their remarkable study “From One Medicine to One Health and systemic approaches to health and well-being”, Zinsstag et al. [8] provide a comprehensive historical sketch. A milestone for the ongoing internationally coordinated activities to further develop the One Health concept was set in October 2008, when the Food and Agriculture Organization of the United Nations (FAO), the World Health Organization (WHO) and the World Organisation for Animal Health (OIE) drafted a document entitled “Contributing to One World, One Health™ – A Strategic Framework for Reducing Risks of Infectious Diseases at the Animal-Human-Ecosystems Interface” [9]. Follow-up conferences in Winnipeg, Canada [10] and Stone Mountain, Georgia [11] were held to transform these strategic ideas into action. The recently published report of the World Bank, “People, Pathogens and Our Planet, Towards a One Health Approach for Controlling Zoonotic Diseases” [12] acknowledges the past activities and recommends One Health as a crucial investment for better achievement of the Millennium Development Goals. In August 2009, a national “One Health Commission” was appointed in the United States, whereas in October 2009, the participants of a global forum on “Evolving Veterinary Education for a Safer World” [13] held by the OIE declared One Health to be the basis of their recommendations for veterinary medicine curricula. The European Union and the Federation of Veterinarians of Europe (FVE) launched the EU Veterinary Week with a conference entitled “animals + humans = one health” [14]. In Switzerland, One Health was highlighted at the 2009 annual meetings of the Swiss Society for Public Health and the Swiss Veterinary Association.
Most publications on One Health refer to cooperation in the field of zoonosis. This is not surprising, given that 60% of human infectious diseases are zoonotic and that this proportion ranges up to 72% for emerging infectious diseases [15]. In the face of serious “brewing storms” such as the SARS, H5N1 or H1N1 pandemic, Kaplan et al. [16] advocated a radical paradigm shift to address future health care threads. Economic evidence from developing countries is demonstrated: in Mongolia, Roth et al. [17] showed that “if the costs of vaccination of livestock against brucellosis were allocated to all sectors in proportion to the benefits, the intervention might be profitable and cost-effective for the agricultural and health sectors.” In Chad, Zinsstag et al. [18] proved that the combination of post-exposure treatment (PEP) of rabies-infected human patients with a dog vaccination campaign broke even with cost-effectiveness of PEP alone after 5 years, and was more cost-effective after 7 years. Schelling et al. [19] reported on the success and cost savings of joint vaccination campaigns for livestock and people among nomadic pastoralists. They demonstrated that cooperation between public health and veterinary services could expand coverage for essential health interventions for people and livestock in remote rural areas. More examples, all of which validate One Health by demonstrating added value in terms of health or economic benefit can be found in a recently published document of Canada’s Vets Without Borders [20]. ”Human-Animal Medicine” by Peter Rabinowitz and Lisa Conti [21] is a comprehensive guide through the fascinating pieces of the One Healthpuzzle. Despite the current focus on One Health, many authors [22–26] complain of the still existing divide between human and veterinary medicine.
In Switzerland, three of the seven ministries are responsible for the health of people, animals and the ecosystem: i) The Federal Department of Home Affairs (EDI) with its Federal Office of Public Health (BAG), ii) the Federal Department of Economic Affairs (EVD) with the Federal Veterinary Office (BVET) and the Federal Office for Agriculture (BLW), and iii) the Federal Department of the Environment, Transport, Energy and Communications (UVEK) with its Federal Office for the Environment (BAFU). The Wildlife and Forest Biodiversity Management Section of the BAFU is in charge of the health of aquatic animals and wildlife. A very similar situation exists among the 26 cantons. Nevertheless, an exemplary exception can be found in the canton of Ticino, where the “Divisione della salute pubblica” as the leading agency hosts all cantonal health professionals. The collaboration of the cantons between themselves and between them and the Confederation is coordinated at institutionalised directors’ meetings such as the Swiss Conference of the Cantonal Ministers of Public Health (GDK). This organisational structure is complemented by various horizontally or vertically interconnected platforms, such as the “Dialog Nationale Gesundheitspolitik”, the Federal Food Chain Unit (BLK) or the Campylobacter-Platform. The most recent report of the Swiss Health Observatory (Obsan) [27] lists 65 Swiss databases related to human health, though none covering animal or environmental health.
The numerous activities of the past two years have considerably increased the visibility of One Health in industrialised countries and provided the impetus for further action.
Zinsstag, Schelling and Tanner [28] postulate a comprehensive improvement in the well-being of the Swiss population at an impressive cost-benefit ratio related to One Health. What situation can we therefore expect for Switzerland? What does the existing or planned cooperation look like? Are there significant barriers impeding this process? Has the global spirit of optimism towards a paradigm shift in collaboration also affected Swiss health specialists?
To answer these questions, interviews were conducted with key experts ranging from a variety of stakeholders, opinion leaders and policy makers equally representing the fields of human and veterinary medicine. Included in the sampling frame were leading professionals from the federal and cantonal authorities, the faculties of medicine and veterinary medicine and relevant professional associations. The main inclusion criterion consisted of the expert’s authority to initiate action related to the implementation of One Health: Additional data on the sample of experts is shown in table 1.
Twenty-one candidates were briefed on the objectives of the study, the planned procedure and the safety of their data, and invited to participate. Of these, 17 implicitly declared their willingness to be interviewed, 2 nominated competent delegates from within the respective institution, and 2 others declined to participate in the study. One of the latter two was shortly retiring and the other thought himself not sufficiently competent. The schedule for the interview was confirmed by separate mail also containing an informed consent form. No compensation was paid for taking part in the study. Sixteen semi-structured interviews (i.e. using an interview guide) were conducted between April and August 2010. The sessions lasted from 35 to 69 minutes. We placed the emphasis on problem-oriented interviews that were as open and flexible as possible, to obtain a broad range of judgements and ideas. An interview protocol had been prepared, validated and adapted to the results of a pre-test. All interviews were conducted by the first author, either in Swiss German or in German. The dialogues were audio recorded and transcribed by the interviewer. The names of persons or institutions mentioned in the interviews were anonymised. Audio file and transcribed text were imported into atlas.ti (Version 6.2) and processed with this software. Template analysis was used to identify themes [29]. Every interview was analysed and coded to collect all ideas, opinions and processes reported in the interviews. The coding list was redefined and reordered as additional themes emerged during the coding process. Finally, an evaluation and validation of the coding system complemented by random tests of audio recordings and transcripts were done by fellow researchers.
| Table 1: Demographic data of the interviewees (N = 16). | ||||
| Experts for | Total | |||
| Human health | Animal health | |||
| Gender | Male | 7 | 7 | 14(87.5%) |
| Female | 2 | 2(12.5%) | ||
| Age | Mean | 52.6 | 55.7 | 53.9 |
| Range | 46–65 | 43–62 | 43–65 | |
| Educational background | Human Medicine | 6 | 6(37.5%) | |
| Veterinary Medicine | 6 | 6(37.5%) | ||
| Other (Economy, Ethology, Food Science, Physics) | 3 | 1 | 4(25.0%) | |
| Position at | Federal Parliament | 2 | 2(12.5%) | |
| Federal Administration | 1 | 1 | 2(12.5%) | |
| Cantonal Administration | 2 | 1 | 3(18.8%) | |
| Professional Organisation | 2 | 2 | 4(25.0%) | |
| University | 2 | 3 | 5(31.3%) | |
| Language areas of Switzerland | German | 8 | 5 | 13(81.3%) |
| French | 2 | 2(12.5%) | ||
| Italian | 1 | 1( 6.3%) | ||
Twelve of the 16 participants had already heard of One Health before the interviews were conducted, while the topic was entirely new for one interviewee with animal-health and three with human-health backgrounds. Six experts had a more in-depth understanding of One Health as a concept. Among those who had heard of the concept, almost all knew of it from developing country examples. Respondents were unanimous that One Health includes human and veterinary medicine, while only a third considered the environment part of the concept. The pressing need for closer cooperation between health professionals was clearly stressed. Nevertheless, this cooperation should not go as far as physicians treating animals or veterinarians treating people. One Health would represent a countermovement to increasing specialisation. Economic considerations represented a recurring discussion point in all interviews. Some experts emphasised that the added value created by One Health should be regarded as inherent to the concept:
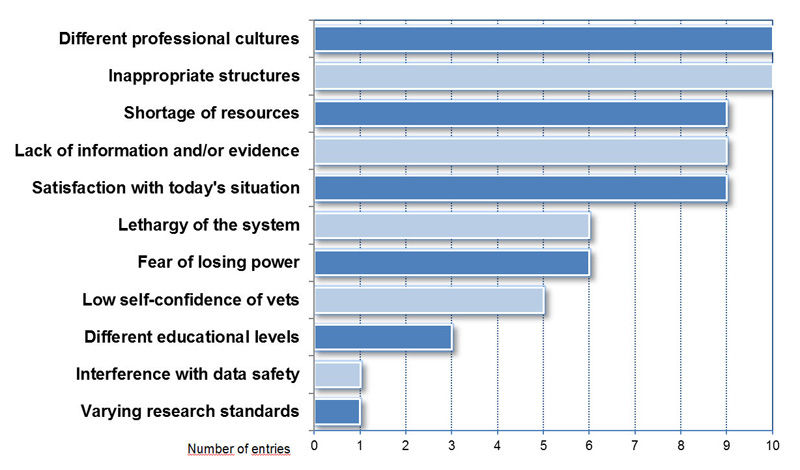
Figure 1
Differentiation of barriers against implementation of One Health in Switzerland (N = 69).
“… if someone speaks about One Health and cannot show how he or she saves money or creates more health, he or she should actually not talk about it.”
The following main categories emerged during the analyses of the interviews: i) Current cooperation between sectors in Switzerland; ii) Assessment of the potential of One Health; iii) Barriers and bridges; and iv) Proposals for further action.
The current cooperation between human and veterinary medicine in Switzerland was judged by 14 experts from “not so bad” to “very positive”. As examples of past and ongoing cooperation in Switzerland, bovine spongiform encephalopathy (BSE) and bird flu (H5N1) were cited repeatedly, while H1N1 no longer triggered the same spirit of cooperation. Several interviewees stated that cooperation tends to be weaker in the absence of a (seemingly) severe threat to the public. In addition to zoonosis control, various other examples of specific cooperation between faculties, institutes or agencies were highlighted. These were particularly the National Research Programmes on “Antibiotic Resistance” (NRP 49) and “Endocrine Disruptors; Relevance to Humans, Animals and Ecosystems” (NRP 50) mentioned by several participants. Both projects emerged as veritable One Healthprojects, despite the fact that this concept was not explicitly known at that time. The tasks of NRP 49 (2001–2006) were to establish an overview on the status of antibiotic resistance in humans, domestic animals and wildlife. On the basis of these results the project was to propose an effective surveillance system for antibiotic resistance. NRP 50 (2002–2007) investigated the burdens of hormonally active agents for humans, domestic and wild animals, and the environment. One of the participants described impressive early examples of One Healthscenarios related to both biodefense and the coordinated medical services of the Swiss army. Representatives of faculties indicated that cooperation between health sectors was either successfully established or in planning: the Veterinary Public Health Institute (VPHI), a joint venture of the Vetsuisse Faculty of Berne and the Federal Veterinary Office, and the declaration of intent by the Vetsuisse Faculty of Zurich to establish a One Health institute.
Ten interviewees emphasised an existing potential for One Health in Switzerland. One participant did not support this view, while five tended to adopt a more cautious and neutral position. Amongst the strongest supporters were participants working at a university institution, although the one rejectionist view also came from this environment. Eleven experts saw the greatest potential in the area of monitoring of communicable diseases. Several referred to existing information exchange platforms. The idea of a better coordination and mobilisation of information raised additional wishes, for example in the field of non-communicable chronic diseases. However, information exchange should go beyond the technical linking of the databases. There also needs to be appropriate networking of the specialised personnel who would use this combined data. A clear vision for the future of monitoring was presented in the following statement:
“Every case of a notifiable disease in animals or humans is automatically communicated to the authorities of the other sector. There is only one surveillance system (…), where each infectious disease is localised spatiotemporally, and the authorities of both veterinary and public health sectors can access electronic maps where these cases light up and really allow the space-time association in real time.”
In addition, participants have stated a substantial potential for enhanced cooperation in the field of antibiotic resistance. The ongoing revision of the national legislation on epidemics was mentioned repeatedly as an opportunity to review the legislative basis. Also the health-promoting aspects of the human-animal bond were highlighted as an attractive and promising aspect of the One Health framework. A distinct opportunity was seen in the expected facilitation of social integration and an increase of activity/mobility in the elderly. Growing importance was attributed to the role of animals as sentinels for human health hazards; and even the possibility of a combined cancer registry for humans and animals was considered.
In descending order of frequency, the following items were identified as obstacles to successful implementation of One Health in Switzerland (fig. 1): Different cultures of the professions involved (10 statements); unsuitable structures (10); lack of resources (9); inadequate information and missing evidence (9); satisfaction with the current situation (9). Less frequently, but still considered crucial, were the following barriers: resistance from the system towards change (6); fear of losing power (6); low self-confidence of veterinarians (5); wide educational differences (3); protection of privacy (1); different research standards between disciplines (1).
According to the interviewees, the perceived cultural differences between physicians and veterinarians, but also, for example, between psychiatrists and psychologists, are often based on prejudice that has remained uncorrected since university. Subsequently, due to the lack of communication between the members of the different professions, the prejudices could never be revisited.
“…one speaks completely different languages! I have tried again and again (…), we talk … but do not understand each other.”
In contrast, the view was also expressed that neither cultural differences nor contact problems would be relevant. There would simply be no mutual interest and no obvious need to cooperate. The fact that the structural organisation of Switzerland is not tailored to working together in the sense of One Health and that the federal structure in general would somehow obstruct the development of common health strategies in Switzerland were obvious for representatives of all types of institutions. Nevertheless, the system was not fundamentally questioned, and its advantages were recognised. While direct relations with world organisations such as WHO and OIE would exist, access to the EU bodies was portrayed as more problematic.
Nine experts (4 work in the administration, 3 at the University and 2 in politics) have mentioned the lack of resources (financial, temporal, and human resources) as a considerable problem. The inadequacy of resources forces them to prioritise their activities according to the current legislation. An oft-mentioned obstacle facing the desire for change was the current absence of more serious problems in Switzerland. Interviewees perceived One Health as sort of a “luxury issue”, and the low level of suffering would further favour a certain inertia of the system.
“...because we are actually on such a [high] level, where (...) all bigger problems have simply been solved (…) one must say: What is there still to solve?”
Suggestions for overcoming the barriers identified were mainly: improving information flows, strengthening communication, and building trust. Demonstration of technical or financial advantages with the help of pragmatic examples would heighten the motivation of all parties involved. A mutually agreed national health strategy and clear mandates would assist the process and encourage its implementers. The experts agreed that the fundamental question of leadership needed to be clarified; and a more general view was:
“We must be aware that any change in the system encounters resistance, and that we look at this resistance as quasi part of the process. I think the fact that we encounter resistance is actually a good sign. It shows that there is something. If something is simply being taken up, then it either was not new or not a really burning issue.”
The experts’ impressive knowledge base helped to create a road map for the development and implementation of One Health. How should activities be arranged and what is their sequence to successfully accomplish a further step towards One Health? Interviewees agreed that the first step would be the promotion of the relationships and interconnections in health and the idea of One Health in the general population, in the relevant institutions, and with the politicians. The appropriate information would be concise and with comprehensible examples, impressive enough to stimulate the desire for change towards One Health. All the experts interviewed wished to see more examples in Switzerland which would provide the best evidence on One Health. Below is a typical quote on this:
“The concept is admittedly nice, but that doesn’t say anything to a politician, (...) concise examples are most effective in politics. (…) he or she wants to know: what is the difference between the application of this concept and non-application of the concept to a situation. And if (...) they recognise an advantage on the basis of an example, it remains in their heads. Then it makes sense to them.”
The greatest opportunities would exist where there was already awareness of the problem, where the smallest additional costs or the largest savings could be expected, and where cooperation between the authorities could be strengthened and improved in a relatively uncomplicated way. Hence an intensification of research activities was postulated by a large proportion of participants. Funding for future research would be easiest to generate where major economic gains could be achieved. But funding for a new project may be hard to come by. Several experts suggested concentrating and coordinating research within a new National Research Programme (NRP). One Health, which is inherently interdisciplinary research, would be exceptionally well suited to an NRP of this kind. As research priorities, interviewees mentioned economic questions and the development of models for joint monitoring systems, including infectious and non-communicable chronic diseases, and the comprehensive range of the human-animal relationship and its socio-economic impact on health. Seven participants suggested a transfer of One Health evidence from developing to industrialised countries.
Nine experts proposed to deepen these issues in a workshop where concepts for the further procedure (road map) could be discussed and a new network established.
Form begins:
“…first, one would need to re-rail the problem (...). Then, once the problem is defined, one would have to develop a strategy and most likely one would need the political will. Thus, it is not enough to detect the problem and recognise a particular approach to a solution or an action, but it needs the political will. Finally, it needs a political sponsor (...).”
The building and strengthening of trust between members of professions who would not yet know each other well enough was designed as a pivotal accompanying measure during this process. Likewise, the idea that One Health should as soon as possible be added to the education of all health professionals was considered. All respondents agreed that such a profound paradigm shift would require time:
“I also do not have the feeling that I must implement this in my lifetime, but I think we will start a process that may need more than twenty years until first results become evident, when one can then say: why didn’t we do this long ago?”
Fifteen leading experts from animal and human health see a potential in implementing the One Health concept in Switzerland. This is an encouraging sign that we should continue the process recently started. One participant did not share this view, given the notion that nowadays people rather concentrate on themselves than on a broader understanding of their role in an ecosystem. Despite their general acceptance, one third of the 15 interviewees were reluctant to embrace the global spirit of optimism. The definition compiled in this study, namely “a closer interdisciplinary cooperation of all relevant sectors for better health for humans, animals and the environment and to achieve a remarkable added value” is in agreement with the relevant literature. The One Health initiative task force, to pick just one, defined One Health as “the strategy to better understanding and addressing the contemporary health issues created by the convergence of the human, animal, and environmental domains” [30].
The One Health concept seems clear and somehow trivial, which might be one of the reasons why the idea has not attracted more attention so far. Every single expert could spontaneously cite one or more Swiss examples of existing inter- or transdisciplinary projects that would easily match the definitions. The National Research Programmes NRP 49 and NRP 50 were often cited as showcase projects in the sense of One Health, without using the term – without even knowing it. There were numerous complaints of vast cultural differences between the various sectors, disciplines and professions involved in health issues. Physicians and veterinarians, for example, would speak different languages and not even try to find a common denominator of communication. Or, psychiatrists would complain that mental illnesses had a lower status in medicine than “real diseases”. As to the organisational structures: how can the now grown silo-like conglomerate of health systems promote closer cooperation in the sense of One Health while the responsibility for human, animal and environmental health is split into a multitude of ministries and offices? Such barriers seem to militate against timely and uncomplicated implementation of an operational One Health concept in Switzerland, although they were not considered insurmountable.
The bulk of the interviews concentrated on finding practicable approaches to successful implementation. The three pivotal processes emerged: capacity building; strengthening of the evidence base for the expected added value; and a stakeholder process to develop and adopt a road map. As the first step, participants suggested a carefully planned broad information campaign engaging the political community.
Capacity building involves information and communication, and particularly education, training, research, administration and the provision of infrastructure such as IT facilities. Will it be possible to find the appropriate leader(s) dedicated to this process? While on a global level the lead is within WHO, FAO and OIE, in Switzerland it will be more complicated to allocate the responsibility for a mutually agreed One Health strategy to a specific authority. The Confederation has no constitutional basis to set strategic health standards, while most of the cantons wait for “specifications from above”; a difficult situation indeed, which not only involves One Health. The ongoing revision of the relevant legislation is seen as an opportunity to make changes. The question of leadership remains, and for the time being either the already existing “Dialog Nationale Gesundheitspolitik” or the Federal Office of Public Health (BAG) and the Federal Veterinary Office (BVET) should share the lead. To expand and further strengthen the evidence base for One Health, more research is needed. With the example of air pollution, Künzli and Perez [31] provide a practical model on how Evidence Based Public Health (EBPH) can be achieved. Optimised coordination and appropriate backing up by science, politics and other institutions, could be obtained through a National Research Programme (NRP) or another large interdisciplinary One Health project. The research priorities mentioned in the interviews reflected the broad range from monitoring of emerging infectious diseases and increased integration of environmental aspects, to better understanding of various contributions of animals to human health in early warning, diagnostics, therapy and prevention. Socio-economic data for this successful partnership are virtually lacking. Still, some figures may highlight the potential: according to the Swiss Health Survey of 2002 [32], 2.2 million people above the age of 15 years were either overweight or obese. The costs related to overweight and obesity and their subsequent diseases for Switzerland were estimated to total CHF 2.2 to 3.2 billion per year [33]. Results from the Survey of Health, Ageing and Retirement in Europe (SHARE) showed the considerable burden of obesity-related health problems for adults aged over 50 years, and the economic effects [34]. The association of pet ownership with physical activity and its contribution to a weight-loss strategy is one example that seems obvious but needs further investigation. A study of the State Secretariat for Economic Affairs (SECO) [35] expected the annual costs of the stress-burnout-depression complex in the working population to reach approximately CHF 4.2 billion. These impressive figures show that even a comparatively small contribution of pet ownership to the prevention of depression or the promotion of physical activity would reduce health care costs. One of the experts claimed yearly savings of CHF 1 to 2 billion would be associated with the implementation of the One Health concept in Switzerland. This corresponds to 1.5–3 % of the annual health costs. The rather euphoric headline of a recent FAO press release reads: “Improved disease prevention in animal health could save billions of dollars. One Health approach (…) is gaining strength” [36] and thus supports the hypothesis of major economic savings. Currently, there are more economic assessments for developing than for industrialised countries. Research, however, should not only focus on money but also on interconnectivity within an ecosystem, and on models for incentives to behavioural changes. Research will add to capacity building, assist in building trust, and generate convincing evidence for the value of One Health needed to engage politicians.
A stakeholder process to evaluate the next appropriate steps and to strengthen the political will for the implementation of the One Health concept in Switzerland must be started soon. It would be highly desirable if, from a first workshop in this process, a working group would emerge, which then could accompany the process as an expert team.
There were some limitations to this study. The first is the small sample size of 16 experts. Although competent and respected health experts working in different fields, they are inevitably not fully representative of all players in the Swiss health system. In particular, no federal or cantonal ministers or practising physicians and veterinarians were included. Secondly, these results are exclusively valid for Switzerland with its structures and processes, and cannot readily be extrapolated to other countries. Thirdly, the selection of participants was from a list of experts preferred by the authors. There was thus a selection bias, a fact that seemed justifiable given the intention of evaluating more general views of the key experts on the topic of One Health and to refrain from comparing different groups.
Visionary concepts rarely emerge in the cost-driven discussions on health systems. This study suggests that experts perceive sufficient potential in One Health to support the opinion leaders in their search for new solutions. The majority of Swiss health experts included in this study expressed their willingness to actively participate in steps towards a broader implementation of One Health, and have expounded their ideas on these steps. The detailed presentation of potential barriers and a guide for a tailored road map represent a practicable way forward. Nevertheless, finding committed leaders to promote implementation remains a challenge. Also, building bridges between sectors and disciplines requires an empathic approach. The experiences and lessons learnt in Switzerland may be of interest to other countries and help communicate and further promote the One Health concept.
1 Dupuis G, Petite J, Péter O, Vouilloz M. An Important Outbreak of Human Q Fever in a Swiss Alpine Valley. Int J Epidemiol. 1987;16(2):282–7.
2 Enserink M. Humans, Animals – It’s One Health. Or Is It? Science. 2010;327(5963):266–7.
3 Wageningen Central Veterinary Institute. International conference: One health in relation to q-fever (in humans and animals) [Internet]. [cited 2010 Oct 29];Available from: http://www.cvi.wur.nl/nl/nieuwsagenda/archief/agenda/2010/Qfeverconference.htm
4 1st International One Health Congress [Internet]. [cited 2010 Oct 29];Available from: http://www.onehealth2011.com/
5 Kahn LH, Kaplan B, Steele JH. Confronting zoonoses through closer collaboration between medicine and veterinary medicine (as “one medicine”). Vet Ital. 2007;43(1):5–19.
6 Kahn L, Kaplan B, Monath T, Steele J. Teaching “One Medicine, One Health”. Am J Med. 2008;121(3):169–70.
7 Schwabe CW. Veterinary Medicine and Human Health. 3. ed. Baltimore: Williams and Wilkins; 1984.
8 Zinsstag J, Schelling E, Waltner-Toews D, Tanner M. From “one medicine” to “one health” and systemic approaches to health and well-being. Preventive Veterinary Medicine [Internet]. 2010 9;Available from: http://linkinghub.elsevier.com/retrieve/pii/S0167587710002023
9 Contributing to One World, One Health: A Strategic Framework for Reducing Risks of Infectious Diseases at the Animal–Human–Ecosystems Interface [Internet]. FAO - WHO - OIE - Worldbank - UNICEF; 2008. Available from: http://www.oie.int/downld/AVIAN%20INFLUENZA/OWOH/OWOH_14Oct08.pdf
10 Public Health Agency of Canada. One World One Health: from ideas to action [Internet]. [Ottawa]: Public Health Agency of Canada,; 2009. Available from: http://www.phac-aspc.gc.ca/publicat/2009/er-rc/index-eng.php
11 CDC, in collaboration with OIE, FAO, WHO. Operationalizing “One Health”: A Policy Perspective – Taking Stock and Shaping an Implementation Roadmap [Internet]. Atlanta GA: 2010. Available from: http://www.cdc.gov/onehealth/pdf/atlanta/brief_overview.pdf
12 The World Bank. People, Pathogens, and Our Planet Volume 1: Towards a One Health Approach for Controlling Zoonotic Diseases [Internet]. 2010;Available from: http://siteresources.worldbank.org/INTARD/Resources/PPP_Web.pdf
13 World Organisation for Animal Health OIE. Evolving veterinary education for a safer world [Internet]. 2009 [cited 2009 Oct 18];Available from: http://www.oie.int/eng/press/en_091014.htm
14 European Union. The EU Veterinary Week 2009 Summary of events organised in the EU by Veterinary Faculties [Internet]. 2010;Available from: http://ec.europa.eu/food/animal/diseases/strategy/pillars/docs/sum_events_EU_vet_faculties_en.pdf
15 Jones KE, Patel NG, Levy MA, Storeygard A, Balk D, Gittleman JL, et al. Global trends in emerging infectious diseases. Nature. 2008;451(7181):990–3.
16 Kaplan B, Kahn LH, Monath TP. The brewing storm. Vet Ital. 45(1):9–18.
17 Roth F, Zinsstag J, Orkhon D, Chimed-Ochir G, Hutton G, Cosivi O, et al. Human health benefits from livestock vaccination for brucellosis: case study. Bull World Health Organ. 2003;(81):867–76.
18 Zinsstag J, Dürr S, Penny MA, Mindekem R, Roth F, Menendez Gonzalez S, et al. Transmission dynamics and economics of rabies control in dogs and humans in an African city. Proc. Natl. Acad. Sci. U.S.A [Internet]. 2009 Aug 17;Available from: http://www.ncbi.nlm.nih.gov/pubmed/19706492
19 Schelling E, Wyss K, Béchir M, Moto DD, Zinsstag J. Synergy between public health and veterinary services to deliver human and animal health interventions in rural low income settings. BMJ. 2005;331(7527):1264–7.
20 Waltner-Toews D. One Health for One World: A Compendium of Case Studies [Internet]. 2010 Apr [cited 2010 Jun 14]; Available from: http://www.vwb-vsf.ca/english/index.shtml
21 Rabinowitz P, Conti L. Human-animal medicine: clinical approaches to zoonoses, toxicants, and other shared health risks. Maryland Heights Mo.: Saunders/Elsevier; 2010.
22 Gibbs EPJ. Emerging zoonotic epidemics in the interconnected global community. The Veterinary Record. 2005;157(22):673–9.
23 King LJ. One world of veterinary medicine. Rev. sci. tech. Off. int. Epiz. 2009;28(2):463–7.
24 Zessin KH. Was ist Veterinary Public Health? – Zeit für eine nützliche Diskussion. Dt Tierärztebl. 2008;(11):1468–77.
25 Zinsstag J, Schelling E, Wyss K, Mahamat MB. Potential of cooperation between human and animal health to strengthen health systems. Lancet. 2005;366(9503):2142–5.
26 Fisman DN, Laupland KB. The “One Health” paradigm: Time for infectious diseases clinicians to take note? Can J Infect Dis Med Microbiol. 2010;21(3):111–4.
27 Roth M, Schmidt V. Inventar ausgewählter Gesundheitsdatenbanken in der Schweiz. Aktualisierung und Erweiterung 2010 (Obsan Bericht 38) [Internet]. 2010;Available from: http://www.obsan.admin.ch/bfs/obsan/de/index/05/publikationsdatenbank.html?publicationID=3842
28 Zinsstag J, Schelling E, Tanner M. “One medicine – one health” und die Tiermedizin in der Schweiz. Schweiz Arch Tierheilkd. 2009;151(7):354–5.
29 King N. The School of Human & Health Sciences – Template Analysis [Internet]. 2007 [cited 2009 Oct 17]; Available from: http://www.hud.ac.uk/hhs/research/template_analysis/index.htm
30 One Health Initiative Task Force. One Health: A New Professional Imperative [Internet]. American Veterinary Medical Association AVMA; 2008 [cited 2009 Oct 7]. Available from: http://www.avma.org/onehealth/
31 Künzli N, Perez L. Evidence based public health – the example of air pollution. Swiss Med Wkly. 2009;139(17-18):242–50.
32 Statistik Schweiz – CD-Rom Publikationen des BFS [Internet]. [cited 2010 Nov 3];Available from: http://www.bfs.admin.ch/bfs/portal/de/index/dienstleistungen/publikationen_statistik/cd_roms/uebersicht.html?publicationID=1358
33 Schneider H, Venetz W, Gallani Berardo C. Federal Office of Public Health – Costs of obesity in Switzerland [Internet]. 2009 Apr 29 [cited 2010 Nov 9];Available from: http://www.bag.admin.ch/themen/ernaehrung_bewegung/05207/05218/05232/index.html?lang=en
34 Peytremann-Bridevaux I, Santos-Eggimann B. Health correlates of overweight and obesity in adults aged 50 years and over: results from the Survey of Health, Ageing and Retirement in Europe (SHARE). Obesity and health in Europeans aged > or = 50 years. Swiss Med Wkly. 2008;138(17-18):261–6.
35 Ramaciotti D, Perriard J. Die Kosten des Stresses in der Schweiz [Internet]. 2003 März;Available from: http://www.seco.admin.ch/dokumentation/publikation/00008/00022/01511/index.html?lang=de
36 FAO Media Centre: Improved disease prevention in animal health could save billions of dollars [Internet]. [cited 2010 Nov 2];Available from: http://www.fao.org/news/story/en/item/44327/icode/
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article was reported.