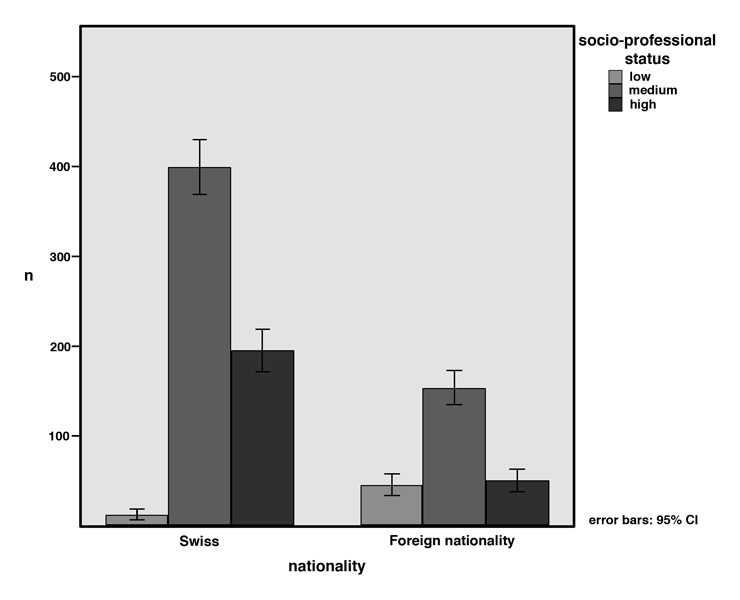
Figure 1
Socio-professional status in relation to nationality (p <0.001, chi-square test)
DOI: https://doi.org/10.4414/smw.2011.13190
Despite a study suggesting that racial and ethnic disparities in brain injury severity, mortality and medical disposition do not exist in paediatric health care treatment [1], there is evidence from studies in the United States of America that racial and ethnic disparities in health care are significant predictors of the quality of health care received, even after controlling for previously known factors such as access to care and other socioeconomic circumstances [2]. A large number of these studies look into disparities in adult health care, but some recent studies also discuss variations in paediatric health care treatment by race, ethnicity and insurance status [3–7].
In a previous study in our paediatric intensive care unit (PICU) we found, that children under the age of 16 with immigrant background and parents with a lower socio-professional status were overrepresented in a group of patients suffering from head injuries and multiple trauma due to falls from windows and balconies [8]. This led us to the assumption that immigrant background and socio-professional status may have an impact on severity of illness of the patients at admission to the PICU. In the present study we also wanted to evaluate the mother tongue in order to define a more specific criterion for the cultural background, as many children living in Switzerland with foreign parents have dual citizenship.
The objectives of this study were to evaluate the severity of illness of immigrants at admission to PICU, their proportion in PICU compared to the general population, the quality of care they received and their outcome (standardised mortality ratio).
The study was performed in the multidisciplinary, 19-bed, paediatric intensive care unit (PICU) of the University Children’s Hospital of Zurich. Data of all patients admitted to intensive care in 2007 (1251 admissions) were recorded. In patients with multiple PICU admissions, only the first admission was taken for analysis.
Following data were prospectively collected (minimal data set, Swiss Society of Intensive Care): (a) demographic parameters: age, sex, nationality, mother tongue, religious denomination and socio-professional status; (b) factors relating to severity of illness: length of stay in PICU, principal diagnosis, artificial ventilation, admission form (elective/urgent), illness severity score at admission (PIM2: Paediatric Index of Mortality [9]), and mortality in PICU. PIM2 relates to PICU admission (first contact with intensive care personnel) to maximum one hour thereafter. PIM2 score is based on ten variables [9]. For diagnostic classification we used the Australian and New Zealand Paediatric Intensive Care Registry (ANZPIC) [10]. Number of drugs applied in the first 24 hours of admission was retrospectively evaluated.
The socio-professional status of the parents was defined according to the classification of the Swiss Federal Office of Statistics [11]. Criteria for classification into different categories were occupation, professional position and education. The classification consists of nine socio-professional categories including top management, independent professions with graduate degree, self-employed, academic professions and chief officers, officers, qualified non-manual labour, qualified manual labour, and unskilled employees and workers. As the hierarchy differs depending on which criteria (e.g. social status, education, earnings) greatest weight is laid on, it seems reasonable to sort the different categories into three groups including high (top management, independent professions with graduate degree, self-employed, academic professions and chief officers), middle (officers, qualified non-manual labour, qualified manual labour), and low (unskilled employees and workers) status. Between parents the higher status was considered as representative. The statistical office of the canton of Zurich provided data of the general population of the canton of Zurich regarding nationality and age [12]. The canton of Zurich is the main catchment area of the PICU.
Statistical calculations were performed with SPSS Statistics 18.0 (SPSS Inc., Chicago, USA). Patients were subdivided into four different PIM strata representing 0 to <1%, 1 to <10%, 10 to <50% and 50 to <100% respectively, of patients’ expected mortality. Chi-square test for trend was used to compare differences of gender, immigrant background (Swiss vs. other), mother tongue (native Swiss speakers vs. other), religious denomination (Christian vs. other) and socio-professional status (low vs. other) along the four PIM strata. Patients of immigrant background were compared with Swiss patients regarding: age, sex, socio-professional status, length of stay in PICU, length of artificial ventilation, emergency admission, PIM score, mortality, principal diagnosis, and number of drugs in the first 24 hours (chi-square test, unpaired t-test or Wilcoxon rank sum test, as appropriate).
The association between “death in PICU” (dependent variable) and PIM, age, sex, numbers of drugs, immigrant background, religious denomination, and socio-professional status of parents was calculated with logistic regression analysis. The ratios of observed number of deaths to expected number of deaths (standardised mortality ratio) were compared regarding sex, age groups, nationality, mother tongue, socio-professional status and religious denomination. A parametric approach according to Rapoport J, et al. was used to construct the 95% confidence interval (CI) of standardised mortality ratio [13]. A p<0.05 was considered significant.
Data on 1009 admissions were included, 242 admissions were excluded as they were not first admissions. Table 1 shows the demographic characteristics of the patients. The majority of the patients were male (58.7%) and Swiss citizens (68.3%). One of the four national languages (German, French, Italian, Rhaeto-Romanic) was spoken by 96.2% of the patients including 93.2% German speakers. The majority of the parents had a medium socio-professional status (54.8%). The number of unknown socio-professional status was relatively high (15.7%) due to unclear occupational description or difficulties in classifying the different occupations. Fifty-three percent of the patients were of Christian denomination, 22.4% of other than Christian denomination with a majority of Moslems (12.6%). Fifty-two percent of the patients stem from the canton of Zurich. In this subpopulation 67.1% were Swiss citizens. Of the patients living outside of the canton of Zurich 69.6% were Swiss citizens. Table 2 provides data on principal diagnosis, mode of admission, length of stay, need of ventilation and duration of ventilation of Swiss and immigrant children.
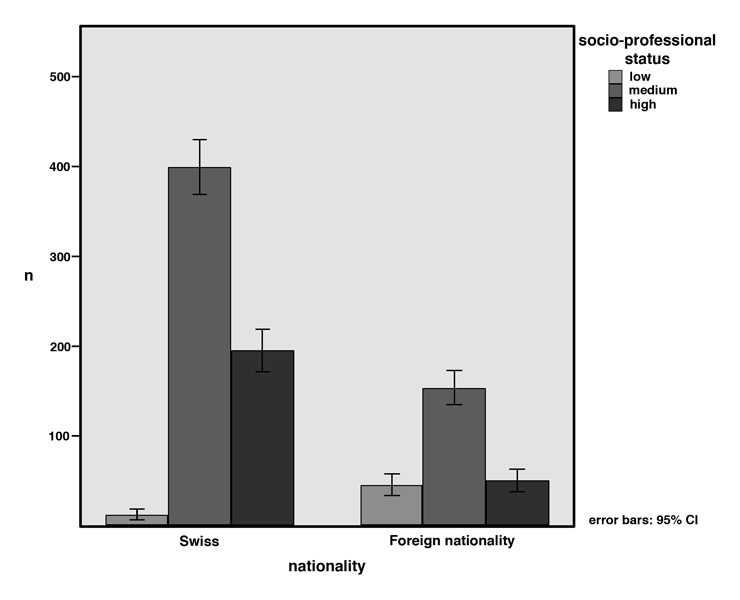
Figure 1
Socio-professional status in relation to nationality (p <0.001, chi-square test)
Chi-square test showed a highly significant difference in the proportion of immigrant children admitted to PICU compared with their proportion in the general population of the canton of Zurich (p <0.0001) (table 3). The same results were shown for the subpopulation of children living in the canton of Zurich (chi-square test, p <0.0001). Readmission rates compared with first admission did not differ by nationality (chi-square test, p = 0.59). There was no significant difference in the proportion of immigrant children in a regular ward compared with their proportion in PICU. Immigrant children are also overrepresented in the general ward compared to the general population.
Figure 1 shows the distribution of different socio-professional levels of the parents of Swiss children and of children with an immigrant background. Chi-square test showed a highly significant difference in socio-professional status by nationality (p <0.001). An immigrant child in PICU is 9.82 times (95% CI 5.16 to 18.7) more likely to have parents belonging to the lowest strata of socio-professional status (unskilled employees and workers) than a Swiss child.
There was a significant difference between immigrant and Swiss children for sex, religious denomination and mother tongue other than Swiss languages (chi-square test). An immigrant child admitted to PICU was 1.12 times (95% CI 1.01 to 1.25) more likely to be male than a Swiss child admitted to PICU. In the general population there is no significant difference in gender by nationality (p = 0.18, chi-square test). No significant differences between immigrant and Swiss children were shown for age, artificial ventilation, principal diagnosis, length of stay in PICU and number of drugs applied in the first 24 hours. No significant difference was shown for sex by religious denomination (chi-square test).
No significant differences by socio-professional status were shown for PICU survival, principal diagnosis, admission form, length of stay and number of drugs applied in the first 24 hours. No significant differences by socio-professional status or between immigrant and Swiss children were shown for admission due to trauma or other injuries (burns, ingestion, electrocution, immersion) (chi-square test).
| Table 1:Characteristics of the patients. N = 1009; sex, age, PIM2 and mortality are known for all patients. | |||
| Characteristic | n | (%) | |
| Sex | Female | 417 | (41.3) |
| Male | 592 | (58.7) | |
| Age category (years) | <1 | 412 | (40.8) |
| 1–5 | 224 | (22.2) | |
| 5–10 | 145 | (14.4) | |
| 10–15 | 142 | (14.1) | |
| >15 | 86 | (8.5) | |
| Mother tongue | National language | 756 | (74.9) |
| Other than a national language | 37 | (3.7) | |
| Bilingual with one national language | 215 | (21.3) | |
| Unknown | 1 | (0.1) | |
| Nationality | Swiss | 689 | (68.3) |
| Immigrant background | 316 | (31.3) | |
| Unknown | 4 | (0.4) | |
| Socio-professional status | High | 243 | (24.1) |
| Medium | 553 | (54.8) | |
| Low | 55 | (5.5) | |
| Unknown | 158 | (15.7) | |
| Denomination | Christian denomination | 536 | (53.1) |
| Other than Christian denomination | 226 | (22.4) | |
| Undenominational | 100 | (9.9) | |
| Unknown | 147 | (14.6) | |
| PIM2 probability strata (%) a | 0–0.99 | 360 | (35.7) |
| 1–9.99 | 563 | (55.8) | |
| 10–49.99 | 75 | (7.4) | |
| 50–100 | 11 | (1.1) | |
| Survival | Deceased | 33 | (3.3) |
| Survived | 976 | (96.7) | |
| Total sample | 1009 | (100) | |
| a PIM2 strata relate to mortality risk. | |||
| Table 2: Principal diagnosis, mode of admission, length of stay, need of ventilation, length of ventilation by nationality. | |||||||||||||||||||||||||||||
| Principal diagnosis a | |||||||||||||||||||||||||||||
| Nationality b | Cardiovas- cular surgery | Other sugery | Trauma | Other injuries | Cardio- vascular | Respiratory | Neuro- logical | Renal | Gastro-intestinal | Sepsis | Miscella- neous | ||||||||||||||||||
| n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | ||||||||
| Swiss | 148 | (75.9) | 128 | (67.0) | 41 | (68.3) | 24 | (64.9) | 52 | (73.2) | 104 | (66.2) | 51 | (61.4) | 11 | (73.3) | 24 | (66.7) | 27 | (73.0) | 74 | (64.3) | |||||||
| Immigrant background | 47 | (24.1) | 63 | (33.0) | 19 | (31.7) | 13 | (35.1) | 19 | (26.8) | 53 | (33.8) | 32 | (38.6) | 4 | (26.7) | 12 | (33.3) | 10 | (27.0) | 41 | (35.7) | |||||||
| Mode of admission | ||||||
| Urgent | Elective | Unknown | ||||
| n | (%) | n | (%) | n | (%) | |
| Swiss | 401 | (68.0%) | 255 | (70.4%) | 33 | (62.3) |
| Immigrant Background | 189 | (32.0%) | 107 | (29.6%) | 20 | (37.7) |
| Artificial ventilation | |||||||
| Artificial ventilation | Duration of ventilation (hours) | ||||||
| No | Yes | Mean | Standard error of the mean | Median | |||
| n | (%) | n | (%) | ||||
| Swiss | 397 | (69.8) | 292 | (67.0) | 69.6 | 7.7 | 25.6 |
| Immigrant background | 172 | (30.2) | 144 | (33.0) | 75.0 | 11.5 | 29.7 |
| Length of stay (days) | |||
| Mean (days) | Standard error of the mean | Median | |
| Swiss | 3.42 | 0.23 | 1.43 |
| Immigrant background | 3.44 | 0.42 | 1.36 |
| a Principal diagnosis was unknown for 8 children (5 Swiss, 3 immigrant background). b Nationality was unknown for 4 children. | |||
| Table 3:Age distribution of immigrants in PICU and in the general population of the canton of Zurich. | |||||||||
| PICU admissions 2007 | General population | ||||||||
| Swiss | Immigrant background | Swiss | Immigrant background | ||||||
| n | (%) | n | (%) | n | (%) | n | (%) | ||
| Age category (years) | <1 | 289 | (70.5) | 121 | (29.5) | 10090 | (72.9) | 3747 | (27.1) |
| 1–5 | 136 | (60.7) | 88 | (39.3) | 38346 | (73.2) | 14064 | (26.8) | |
| 5–10 | 92 | (64.3) | 51 | (35.7) | 47767 | (75.3) | 15648 | (24.7) | |
| 10–15 | 106 | (74.6) | 36 | (25.4) | 52019 | (79.7) | 13222 | (20.3) | |
| >15 | 66 | (76.7) | 20 | (23.3) | 33843 | (83.9) | 6482 | (16.1) | |
| Total | 689a | (68.6) | 316a | (31.4) | 182065a | (77.4) | 53163a | (22.6) | |
| a p <0.0001, chi-square test Total excludes 4 children for whom nationality was unknown. Regular ward population: 5040 Swiss children (67%), 2463 children with immigrant background (33%). | |||||||||
Table 4 and 5 provide data on the illness severity score at admission (PIM 2), observed mortality and standardised mortality ratio by nationality categorised into geographical regions (table 4) and by sex, age, nationality, mother tongue, socio-professional status and religious denomination (table 5).
Chi-square test for trend showed no significant difference along the four PIM 2 strata for sex, nationality other than Swiss, mother tongue other than native speakers of Swiss languages, religious denomination other than Christian denominations, and lower socio-professional status of the patients’ parents. Trend analysis in PIM 2 strata revealed highly significant results (p <0.001) for survival, need of artificial ventilation, principal diagnosis, and patients younger than one year.
According to binary logistic regression analysis, the independent variables PIM 2 (OR 1.056, 95% CI 1.024–1.088, p = 0.001), length of stay (OR 1.048, 95% CI 1.001–1.098, p = 0.047), and number of drugs applied in the first 24 hours (OR 1.134, 95% CI 1.01–1.273, p = 0.034) predicted “death in PICU”. All other independent variables (sex, age, nationality, mother tongue, socio-professional status, religious denomination, artificial ventilation, admission form, and principal diagnosis) did not show any predictive value for “death in PICU”.
| Table 4:Expected mortality (PIM2), observed mortality and standardized mortality ratio by nationality categorised into geographical regions. | |||||||
| Expected mortality (PIM 2, %) | Observed mortality | Standardised mortality ratio | |||||
| n | Mean (%) | Standard error of the mean | Deceased (n) | (%) | Observed/expected mortality (95% CI) | ||
| Regions | Switzerland | 689 | 4.02 | 0.39 | 20 | (2.9) | 0.72 (0.41–1.03) |
| Western Europe | 102 | 4.87 | 1.35 | 5 | (4.9) | 1.01 (0.34–1.67) | |
| Balkan States | 94 | 3.08 | 0.47 | 2 | (2.1) | 0.68 (0–1.78) | |
| Turkey | 37 | 2.20 | 0.48 | (0) | 0 (0–2.11) | ||
| Asia | 23 | 5.50 | 2.28 | 3 | (13.0) | 2.36 (0.96–4.25) | |
| Africa | 16 | 17.31 | 8.30 | 2 | (12.5) | 0.72 (0.16–1.29) | |
| Eastern Europe | 15 | 1.51 | 0.36 | 1 | (6.7) | 4.44 (0.35–8.48) | |
| Middle East | 10 | 3.45 | 1.60 | (0) | 0 (0–3.16) | ||
| Latin America | 10 | 1.56 | 0.38 | (0) | 0 (0–4.9) | ||
| Northern America | 3 | 1.27 | 0.32 | (0) | 0 (0–9.95) | ||
| Others | 6 | 1.10 | 0.36 | (0) | 0 (0–7.56) | ||
| Total | 1005 | 4.11 | 0.34 | 33 | (3.3) | 0.80 (0.55–1.05) | |
| Total excludes 4 children for whom nationality was unknown. | |||||||
| Table 5:Expected mortality (PIM2), observed mortality and standardised mortality ratio by sex, age, nationality, mother tongue, socio-professional status and religious denomination. | |||||||
| Expected mortality (PIM2 %) | Observed mortality | Standardised mortality ratio | |||||
| n | Mean (%) | Standard error of the mean | Deceased (n) | (%) | Observed/expected mortality (95% CI) | ||
| Sex | Female | 417 | 3.67 | 0.37 | 10 | (2.4) | 0.65 (0.2–1.1) |
| Male | 592 | 4.40 | 0.51 | 23 | (3.9) | 0.89 (0.58–1.18) | |
| Age (years) | <1 | 412 | 5.46 | 0.55 | 20 | (4.9) | 0.90 (0.54–1.24) |
| 1–5 | 224 | 3.22 | 0.66 | 4 | (1.8) | 0.56 (0–1.15) | |
| 5–10 | 145 | 4.03 | 1.19 | 5 | (3.4) | 0.84 (0.31–1.4) | |
| 10–15 | 142 | 2.12 | 0.39 | (0) | 0 (0–1.06) | ||
| >15 | 86 | 3.22 | 1.11 | 4 | (4.7) | 1.46 (0.5–2.39) | |
| Nationality | Swiss | 689 | 4.02 | 0.39 | 20 | (2.9) | 0.72 (0.41–1.03) |
| Immigrant background | 316 | 4.29 | 0.66 | 13 | (4.1) | 0.96 (0.54–1.38) | |
| Mother tongue | National language | 756 | 4.03 | 0.38 | 26 | (3.4) | 0.84 (0.56–1.15) |
| Other than national language | 37 | 2.31 | 0.58 | 1 | (2.7) | 1.17 (0–3.21) | |
| Bilingual with one national language | 215 | 4.62 | 0.81 | 6 | (2.8) | 0.61 (0.1–1.11) | |
| Denomination | Christian denomination | 536 | 3.74 | 0.43 | 13 | (2.4) | 0.64 (0.28–1.01) |
| Other than Christian denomination | 226 | 4.10 | 0.70 | 7 | (3.1) | 0.76 (0.22–1.29) | |
| Undenominational | 100 | 3.65 | 0.76 | 2 | (2.0) | 0.55 (0–1.47) | |
| Socio-professional status | High | 243 | 3.90 | 0.71 | 8 | (3.3) | 0.85 (0.33–1.36) |
| Medium | 553 | 3.90 | 0.40 | 13 | (2.4) | 0.62 (0.24–0.96) | |
| Low | 55 | 3.49 | 0.87 | 1 | (1.8) | 0.52 (0–1.82) | |
| Unknown: nationality for 4 children, mother tongue for 1 child, denomination for 147 children, socio-professional status for 158 children. | |||||||
Children with an immigrant background are overrepresented in the PICU of the University Children’s Hospital Zurich compared with their proportion in the general population of the canton of Zurich. Parents of these children have a lower socio-professional status than parents of Swiss children hospitalised in PICU. However, the distribution of immigrant children and Swiss children along the strata of illness severity is equal and there is no difference between the two groups in relation to the ratio of observed to expected mortality, a measure of quality of care in PICU.
Since 2003 the National Healthcare Disparities Report provides data every year on disparities regarding health care in the United States of America. “While some of the biggest disparities in quality remain, progress has been made in reducing disparities” [14]. Evaluating disparities in (access to) health care is an important factor in improving health care quality in the general population. Studies documenting disparities in health care are largely based on surveys in adult chronic care [15]. There are only few reports studying the same question in the paediatric population, although the question is equally important.
Variations in socio-professional status by nationality has also been reported for the general population in Switzerland, where major differences depending on the country of origin have been found [16]. Regarding admission rates to PICU, increased rates for more deprived children, as we found in our study, have been reported in the UK [5] and in the United States [17]. Illness severity and PICU-outcome, however, did not differ between Swiss and immigrant children in our study. These findings are supported by some studies [1, 3, 18], but are in contrast to studies from the UK, United States and Canada reporting variations in mortality in relation to nationality [5, 6, 19, 20]. In primary adult care in Switzerland, the health of the immigrant population is poorer than the health of the Swiss population [21]. Our finding of an overrepresentation of children with an immigrant background in admission rate to PICU, despite comparable illness severity and outcome parameters once admitted to tertiary care, could be indicative of disparities in primary health care or for their disadvantage in general health status. This conclusion is only speculative and as has been pointed out in former studies, “the pathways through which socioeconomic position and race affect health care are complex” [22]. Several other reasons for disparities in health care by race and socioeconomic status are mentioned in the literature, such as health care affordability [23], education [23, 24], knowledge [25], literacy [26], competing demands including work and child care [27], patient attitudes [28], health beliefs [29, 30], racial concordance between physician and patient [31], patient preferences [32, 33], provider bias [34], geographic access and transportation [35] (controversial [24]). A number of studies point out, that the insurance status has an influence on mortality [19, 36–39] and severity of illness [3]. In Switzerland health insurance is compulsory, so this specific causal factor does not apply.
Most of the studies to which we are referring were carried out in Anglo-Saxon countries, where health care system and socioeconomic situation are different from Switzerland. However, there are a few studies listing reasons for disparities in Switzerland [21, 40].
PICU-admission already represents a critical status of illness severity, in which there are no further differences defined by nationality or socio-professional status. Data from our tertiary hospital (PICU and general ward) indicate that disparities may also be found at a lower level of illness severity. The results of our study on disparities in a PICU are important, although our study focuses only on a specific part of the health care system. Variations may begin earlier, respectively at a lower level of illness severity.
Nationality correlated with gender in our study. An immigrant child admitted to PICU was 1.12 (95% CI 1.01 to 1.25) more likely to be male than a Swiss child. Since religious denomination correlated with nationality, we investigated whether the reason might be found there, but found no evidence for this assumption. Overall there were more male (58.7%) than female patients in PICU. A similar distribution has been reported in adult care [41]. In addition, in adult care, men receive an increased level of care and undergo more invasive procedures, even though there is a higher severity of illness in women. Despite these differences men do not have a better outcome [41]. Regarding the association between treatment intensity and gender in PICU, there is a study showing a positive correlation between drug exposure and male gender [42]. Our data, however, did not show significant differences in the number of drugs applied in the first 24 hours after admission and in the rate of artificial ventilation between girls and boys.
In conclusion, at the PICU of the University Children’s Hospital Zurich there are no variations in severity of illness, mortality and standardised mortality ratio by nationality, mother tongue and socio-professional status. Related to standardised mortality ratio, children from all nations receive the same quality of care, although there are variations by nationality and socio-professional status regarding gender and admission rate. Children with an immigrant background are overrepresented in PICU and among these children there are more boys and their parents have a lower socio-professional status than Swiss children. These findings indicate that disparities may exist at a lower level of illness severity, due to many possible reasons (for example shortcomings in primary health care). However, once a child enters tertiary, highly specialized health care (such as intensive care), nationality and socio-economic factors no longer influence quality of health care delivery.
We thank Ueli Frey for his ideas he contributed to the design of the study.
1 Howard I, Joseph JG, Natale JE. Pediatric traumatic brain injury: do racial/ethnic disparities exist in brain injury severity, mortality, or medical disposition? Ethn Dis. 2005;15:S5-51–6.
2 Unequal treatment: confronting racial and ethnics disparities in health care. Washington, DC, Institute of Medicine, 2002.
3 Lopez AM, Tilford JM, Anand KJ, Jo CH, Green JW, Aitken ME, et al. Variation in pediatric intensive care therapies and outcomes by race, gender, and insurance status. Pediatr Crit Care Med. 2006;7:2–6.
4 Haider AH, Efron DT, Haut ER, DiRusso SM, Sullivan T, Cornwell EE. Black children experience worse clinical and functional outcomes after traumatic brain injury: an analysis of the National Pediatric Trauma Registry. J Trauma. 2007;62:1259–62; discussion 1262–3.
5 Parslow RC, Tasker RC, Draper ES, Parry GJ, Jones S, Chater T et al. Paediatric Intensive Care Audit Network. Epidemiology of critically ill children in England and Wales: incidence, mortality, deprivation and ethnicity. Arch Dis Child. 2009;94:210.
6 Office for National Statistics UK. Large differences in infant mortality by ethnic group, 2008. Available from http://www.statistics.gov.uk/pdfdir/imeth0608.pdf (accessed 14 June 2010)
7 Claydon JE, Mitton C, Sankaran K, Lee SK. Ethnic differences in risk factors for neonatal mortality and morbidity in the neonatal intensive care unit. J Perinatol. 2007;27:448–52.
8 Mayer L, Meuli M, Lips U, Frey B. The silent epidemic of falls from buildings: analysis of risk factors. Pediatr Surg Int. 2006;22:743–8.
9 Slater A, Shann F, Pearson G. PIM2: A revised version of the Paediatric Index of Mortality. Intensive Care Med. 2003;29:278–85.
10 Slater A, Shann F, McEniery J. The ANZPIC Registry diagnostic codes: a system for coding reasons for admitting children to intensive care. Intensive Care Med. 2003;29:271–7.
11 Joye D, Schuler M, Meier U. Sozialstruktur der Schweiz. Bundesamt für Statistik, Bern, Switzerland, 1996.
12 Statistisches Amt des Kantons Zürich, http://www.statistik.zh.ch . (accessed 14 June 2010).
13 Rapoport J, Teres D, Lemeshow S, Gehlbach S. A method for assessing the clinical performance and cost-effectiveness of intensive care units: a multicenter inception cohort study. Crit Care Med. 1994;22:1385–91.
14 Agency for Healthcare Research and Quality. 2007 National Healthcare Disparities Report. Rockville, MD: U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality; February 2008. AHRQ Pub. No. 08-0041.
15 Dougherty D, Meikle SF, Owens P, Kelley E, Moy E. Children’s Health Care in the First National Healthcare Quality Report and National Healthcare Disparities Report. Med Care. 2005;43(3 Suppl):I58–63.
16 Eidgenössische Volkszählung 2000, Ausländerinnen und Ausländer in der Schweiz. Bundesamt für Statistik, 2004. Available from http://www.bfs.admin.ch/bfs/portal/de/index/regionen/22/publ.Document.68548.pdf (accessed 14 June 2010).
17 Naclerio AL, Gardner JW, Pollack MM. Socioeconomic factors and emergency pediatric ICU admissions. Ann N Y Acad Sci. 1999;896:379–82.
18 Petrova A, Mehta R, Anwar M, Hiatt M, Hegyi T. Impact of race and ethnicity on the outcome of preterm infants below 32 weeks gestation. J Perinatol. 2003;23:404–8.
19 Abdullah F, Zhang Y, Lardaro T, Black M, Colombani PM, Chrouser K, et al. Analysis of 23 million US hospitalizations: uninsured children have higher all-cause in-hospital mortality. J Public Health (Oxf). 2010;32(2):236–44.
20 Gornick ME, Eggers PW, Reilly TW, Mentnech RM, Fitterman LK, Kucken LE, et al. Effects of race and income on mortality and use of services among Medicare beneficiaries. N Engl J Med. 1996;335:791–9.
21 Althaus F, Paroz S, Renteria S-C, Rossi I, Gehri M, Bodenmann P. Gesundheit von Ausländern in der Schweiz. Schweiz Med Forum. 2010;10:59–64.
22 Fiscella K, Franks P, Gold MR, Clancy CM. Inequality in quality: addressing socioeconomic, racial, and ethnic disparities in health care. JAMA. 2000;283:2579–84.
23 Potosky AL, Breen N, Graubard BI, Parsons PE. The association between health care coverage and the use of cancer screening tests. Results from the 1992 National Health Interview Survey. Med Care. 1998;36:257–70.
24 Pincus T, Esther R, DeWalt DA, Callahan LF. Social conditions and self-management are more powerful determinants of health than access to care. Ann Intern Med. 1998;129:406–11.
25 Brown ML, Potosky AL, Thompson GB, Kessler LG. The knowledge and use of screening tests for colorectal and prostate cancer: data from the 1987 National Health Interview Survey. Prev Med. 1990;19:562–74.
26 Ad Hoc Committee on Health Literacy for the Council on Scientific Affairs, American Medical Association. Health literacy. JAMA. 1999;281:552–7.
27 Lannon C, Brack V, Stuart J, Caplow M, McNeill A, Bordley WC, et al. What mothers say about why poor children fall behind on immunizations. A summary of focus groups in North Carolina. Arch Pediatr Adolesc Med. 1995;149:1070–5.
28 Fiscella K, Franks P, Clancy CM. Skepticism toward medical care and health care utilization. Med Care. 1998;36:180–9.
29 Lannin DR, Mathews HF, Mitchell J, Swanson MS, Swanson FH, Edwards MS. Influence of socioeconomic and cultural factors on racial differences in late-stage presentation of breast cancer. JAMA. 1998;279:1801–7.
30 Thomas LR, Fox SA, Leake BG, Roetzheim RG. The effects of health beliefs on screening mammography utilization among a diverse sample of older women. Women Health. 1996;24:77–94.
31 Cooper-Patrick L, Gallo JJ, Gonzales JJ, Vu HT, Powe NR, Nelson C, et al. Race, gender, and partnership in the patient-physician relationship. JAMA. 1999;282:583–9.
32 Whittle J, Conigliaro J, Good CB, Joswiak M. Do patient preferences contribute to racial differences in cardiovascular procedure use? J Gen Intern Med. 1997;12:267–73.
33 Oddone EZ, Horner RD, Diers T, Lipscomb J, McIntyre L, Cauffman C, et al. Understanding racial variation in the use of carotid endarterectomy: the role of aversion to surgery. J Natl Med Assoc. 1998;90:25–33.
34 van Ryn M, Burke J. The effect of patient race and socio-economic status on physicians' perceptions of patients. Soc Sci Med. 2000;50:813–28.
35 Heckman TG, Somlai AM, Peters J, Walker J, Otto-Salaj L, Galdabini CA, et al. Barriers to care among persons living with HIV/AIDS in urban and rural areas. AIDS Care. 1998;10:365–75.
36 Moss N, Carver K. The effect of WIC and Medicaid on infant mortality in the United States. Am J Public Health. 1998;88:1354–61.
37 Currie J, Gruber J, Fischer M. Physician payments and infant mortality: evidence from Medicaid fee policy. Am Econ Rev. 1995;85:106–11.
38 Hanratty M. J. Canadian national health insurance and infant health. AmEcon Rev. 1996;86: 276–84.
39 Braveman P, Oliva G, Miller MG, Reiter R, Egerter S. Adverse outcomes and lack of health insurance among newborns in an eight-county area of California, 1982 to 1986. N Engl J Med. 1989;321:508–13.
40 Fontana M, Bischoff A. Uptake of breast cancer screening measures among immigrant and Swiss women in Switzerland. Swiss Med Wkly. 2008;138:752–8.
41 Valentin A, Jordan B, Lang T, Hiesmayr M, Metnitz PG. Gender-related differences in intensive care: a multiple-center cohort study of therapeutic interventions and outcome in critically ill patients. Crit Care Med. 2003;31:1901–7.
42 Warrier I, Du W, Natarajan G, Salari V, Aranda J. Patterns of drug utilization in a neonatal intensive care unit. J Clin Pharmacol. 2006;46:449–55.
No financial support and no other potential conflict of interest relevant to this article was reported.