
Figure 1
Main entrance to BPKIHS hospital.
DOI: https://doi.org/10.4414/smw.2011.13174
Ischemic heart disease (IHD) continues to be a major contributor of mortality and morbidity globally. In 2001, 7.3 million deaths were reported due to IHD worldwide and three quarters of these deaths occurred in the low and middle income countries [1].
In developed countries, although there is an increase in the overall prevalence of IHD, there has been a decline in the age-adjusted death rates due to IHD. This decline is primarily due to an increased awareness concerning cardiovascular risk factors, better compliance with life-style and pharmacological prevention measures, and the availability of improved medical, interventional and surgical treatment for patients with acute coronary syndrome (ACS) and established chronic IHD [2].
In contrast, there has been a marked increase in the burden of IHD in developing countries and an increasing trend in the age-adjusted death rates, which are primarily due to the social and economic changes that have occurred with urbanisation and industrialisation, leading to a higher prevalence of the main cardiovascular risk factors [2]. Moreover, this is coupled with a low availability of evidence-based therapies and interventions for the great majority of patients, and their outcome, both in terms of morbidity and mortality, is thus often poor. It has also been noted that patients in South Asia are often afflicted with IHD at a relatively young age, thus impacting the working-age population more severely, with majorconsequences for families who lose wage earners, while the resultingloss in productivity adversely affects national development [3].
Several studies have demonstrated that low socioeconomic groups have the highest risk of IHD [4–6]. These people have less access to health care, are uneducated, and their risk factors are often not recognised. When they develop clinical symptoms, they often do not receive effective treatment because of lack of financial resources, because no facilities exist in their area, and because the public health resources, when available, are generally mainly targeted to the prevention and treatment of infectious diseases [3].
Nepal has an estimated population of 29 million inhabitants with 25% living below the poverty threshold (defined as living on less than USD 1.25 per day, World Bank 2005). The average life expectancy has risen from 54 years in 1990 to approximately 67 years today. There is no national health insurance system in Nepal, and therefore the vast majority of people must pay for medical services and treatment themselves.
Most of the major hospitals in Nepal are in the capital, Kathmandu, and there are few medical colleges, and district and zonal hospitals providing health care services to those living elsewhere. Over 8 million people live in eastern Nepal. To assess the contemporary mode of presentation, hospital treatment and short-term outcomes of patients with ACS in this area, we prospectively collected information concerning all patients admitted for ACS in 2008 to the only tertiary teaching referral centre in eastern Nepal.
B.P. Koirala Institute of Health Sciences (BPKIHS) is a university hospital in Dharan, eastern Nepal, established in 1993 with undergraduate and postgraduate medical and paramedical programs (fig. 1). The hospital has 750 beds and hosts over 30’000 patients per year. About 180’000 patients consult the out-patient department yearly. The town of Dharan has a population of 1.2 million, and the hospital is the only referral centre outside Kathmandu for the inhabitants in eastern Nepal, and also serves parts of the neighbouring states of West Bengal and Bihar in India (fig. 2).

Figure 1
Main entrance to BPKIHS hospital.

Figure 2
Map of Nepal.
A cross sectional descriptive study was conducted on consecutive patients presenting to BPKIHS with ACS from 1st January 2008 to 31st December 2008. All patients admitted to the 6-bed Coronary Care Unit (CCU) and the medicine ward of the hospital with a clinical diagnosis of ACS were included, and assigned to one of 3 groups: ST Segment Elevation Myocardial Infarction (STEMI), Non ST Segment Elevation Myocardial Infarction (NSTEMI) and Unstable Angina (UA).
We recorded age, gender, educational status, direct admission through emergency room (ER) versus referral, time delays (symptom onset, medical contact, literacy, admission to the BPKIHS, thrombolysis), treatment during hospital stay, transfer for invasive evaluation and treatment, and in-hospital outcome.
Patients with a typical clinical presentation, and/or ECG changes together with total creatine kinase (CK) at least once above 2.5 x the upper limit of normal (ULN) were considered as STEMI or NSTEMI. Patients with all measurements of total CK <2.5x the ULN were considered as suffering from UA. Patients who had an alternate diagnosis for the chest pain were excluded (The ULN for CK in Dharan is 190 UI/l). The study was approved by the ethical committee of the institution. After obtaining informed consent from the subjects, a questionnaire was filled in for each patient.
All analyses were conducted with SPSS version 15 (SPSS Inc, Chicago, Ill). Categorical variables are presented as frequencies and were compared by means of a chi-square test. Continuous variables are presented as means, and ANOVA-test was used for comparison between the three groups. A two-sided value of p <0.05 was considered statistically significant.
During the 12-month study period, 153 patients were enrolled after having been admitted with a diagnosis of ACS. A diagnosis of STEMI was made in 58 patients (38%), NSTEMI in 28 patients (18%) and UA in 67 patients (44%). These 153 patients represented 16% of all hospital admissions to a medical ward with cardiovascular disease at the BPKIHS in 2008.
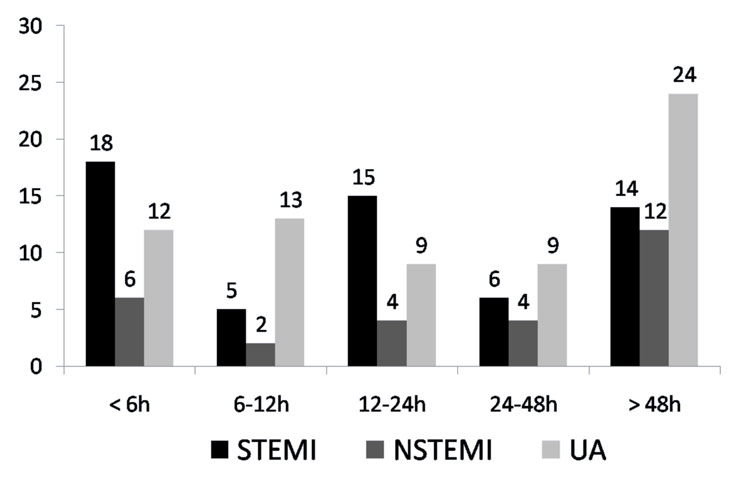
Figure 3
Time to presentation from onset of symptoms (number of patients).
Table 1 shows the baseline characteristics of the patients. Their mean age was 62 years. A total of 26 (17%) patients diagnosed with ACS were less than 50 years of age of which 9 presented with STEMI, 4 with NSTEMI and 13 with UA. A majority of patients were male.
33% of all patients with ACS presented to the hospital after more than 48 hours of chest pain. 24% of all patients came in within 6 hours of the onset of symptoms of which nearly one third had STEMI (fig. 3). It is also noteworthy that among the patients who presented with ACS, 52% were illiterate and also had poor access to the hospital because of distance and/or financial constraints: they thus presented significantly later to the hospital than those who were literate (fig. 4).
Heart failure (class Killip II-IV) was present in 47% of all patients admitted with ACS and among those with STEMI it was present in 57% compared to 29% and 46.3% in the NSTEMI and UA groups respectively (p <0.04). Heart failure was more common among those who were illiterate (61% vs. 44%, p<0.02).
All patients were treated with acetylsalicyclic acid except for one patient in the STEMI group who was having an active esophageal variceal bleed at the time of hospital admission and did not receive clopidogrel either. Among those who had STEMI, only 20 (34%) received thrombolysis with Streptokinase. Most patients (77%) received angiotensin-converting-enzyme inhibitors, 32% received betablockers and 61% received statins (table 4).
A total of 125 (82%) patients were discharged home after a mean hospital stay of 5 days, 22 (14%) patients died in hospital and 6 (4%) were referred to Kathmandu for coronary angiography and revascularisation. Mortality was highest in the STEMI patients (17%), but was also high for NSTEMI (14%) and UA (12%) (fig. 5).
| Table 1:Baseline characteristics. | |||||
| Total | STEMI | NSTEMI | UA | P value | |
| N | 153 (100%) | 58 (38%) | 28 (18%) | 67 (44%) | |
| Age (years±SD) | 62 ± 12 | 62 ± 12 | 62 ± 11 | 63 ± 12 | ns |
| Sex Male Female | 91 (60%) 62 (41%) | 43 (74%) 15 (26%) | 17 (61%) 11 (39%) | 31 (46%) 36 (54%) | 0.007 |
| Admission Admission via ER Admission via OPD Referral * | 111 (73%) 14 (9%) 28 (18%) | 42 (72%) 2 (3%) 14 (24%) | 22 (79%) 1 (4%) 5 (18%) | 47 (70%) 11 (16%) 9 (13%) | 0.06 |
| Time to presentation since onset of symptoms <6 hours 6–12 hours 12–24 hours 24–48 hours >2 days | 36 (24%) 20 (13%) 28 (18%) 19 (12%) 50 (33%) | 18 (31%) 5 (9%) 15 (26%) 6 (10%) 14 (24%) | 6 (21%) 2 (7%) 4 (14%) 4 (14%) 12 (43%) | 12 (18%) 13 (19%) 9 (13%) 9 (13%) 24 (36%) | |
| Key Risk factors Hypertension Diabetes Smoking Sedentary lifestyle | 60 (39%) 21 (14%) 93 (61%) 17 (11%) | 20 (35%) 10 (17%) 35 (60%) 6 (10%) | 16 (57%) 2 (7%) 19 (68%) 6 (22%) | 24 (36%) 9 (13%) 39 (58%) 5 (8%) | ns ns ns ns |
| Educational status Literate Illiterate | 73 (48%) 80 (52%) | 35 (60%) 23 (40%) | 14 (50%) 14 (50%) | 24 (36%) 43 (64%) | 0.023 |
| * Referral from another hospital. ER: emergency room, OPD: outpatient Department | |||||
| Table 2: Clinical features. | ||||
| Overall | STEMI | NSTEMI | UA | |
| Chest pain (n/%) | 115 (75%) | 44 (76%) | 19 (68%) | 52 (78%) |
| Shortness of breath (n/%) | 108 (71%) | 39 (67%) | 22 (79%) | 47 (70%) |
| Diaphoresis | 80 (52%) | 33 (57%) | 14 (50%) | 33 (49%) |
| Nausea | 38 (25%) | 18 (31%) | 11 (39%) | 9 (14%) |
| Syncope | 19 (13%) | 11 (19%) | 2 (8%) | 6 (9%) |
| SBP (mm Hg) | 135 ± 30 | 136 ± 29 | 129 ± 32 | 136 ± 30 |
| DBP (mm Hg) | 87 ± 21 | 89 ± 23 | 83 ± 19 | 87 ± 20 |
| Heart failure > Killip 1 | 72 (47%) | 33 (57%) | 8 (29%) | 31 (46%) |
| Table 3: Laboratory findings on hospital admission. | ||||
| Overall | STEMI | NSTEMI | UA | |
| Hb (g/dl) | 14 ± 10 | 13 ± 2 | 13 ± 2 | 14 ± 15 |
| TLC (WBC/mm3) | 11910 ± 5305 | 13969 ± 5253 | 12607 ± 6390 | 9836 ± 3998 |
| RBG (mmol/l) | 8 ± 4 | 9 ± 4 | 7 ± 3 | 8 ± 4 |
| Urea (mmol/l) | 16 ± 12 | 17 ± 14 | 15 ± 7 | 15 ± 11 |
| Creatinine (mmol/l) | 120 ± 95 | 136 ± 133 | 113 ± 46 | 109 ± .64 |
| CK Total (U/l) | 1311 ± 4680 | 2286 ± 7423 | 1637 ± 1479 | 331 ± 334 |
| CK-MB (U/l) | 109 ± 346 | 178 ± 548 | 156 ± 104 | 29 ± 18 |
| Cholesterol (mmol/l) | 4.3 ± 1.2 | 4.3 ± 0.9 | 4.2 ± 1.3 | 4.4 ± 1.3 |
| HDL (mmol/l) | 0.9 ± 0.08 | 0.9 ± 0.09 | 1.0 ± 0.09 | 1.0 ± 0.08 |
| TAG (mmol/l) | 1.8 ± 0.8 | 1.8 ± 0.8 | 1.7 ± 0.6 | 1.8 ± 0.8 |
| LDL (mmol/l) | 2.5 ± 0.9 | 2.5 ± 0.7 | 2.4 ± 1.4 | 2.5 ± 0.9 |
| TLC: total lymphocyte count, RBG: random blood glucose, CK: creatine kinase, CK-MB: creatine kinase myocadial band isoenzyme, HDL: high density lipoprotein, TAG: triglycerides, LDL: low density lipoprotein | ||||
| Table 4: Treatment received. | ||||
| Overall | STEMI | NSTEMI | UA | |
| Aspirin | 152 (99%) | 57 (98%) | 28 (100%) | 67 (100%) |
| Clopidogrel | 151 (99%) | 57 (98%) | 27 (96%) | 67 (100%) |
| Thrombolysis (STK) | 20 (13%) | 20 (34%) | ||
| LMWH | 77 (50%) | 25 (43%) | 9 (32%) | 43 (64%) |
| Betablockers | 49 (32%) | 14 (24%) | 8 (29%) | 27 (40%) |
| ACE I | 117 (77%) | 47 (81%) | 20 (71%) | 50 (75%) |
| ARBs | 3 (2%) | 1 (4%) | 2 (3%) | |
| Statins | 94 (61%) | 34 (59%) | 18 (64%) | 42 (63%) |
| STK: streptokinase, LMWH: low molecular heparin, ACEI: angiotensin converting enzyme inhibitor, ARB: angiotensin receptor blocker | ||||
The two most common causes of death worldwide are ischemic heart disease and stroke, and among them, 80% of deaths and 85% of disability from cardiovascular disease (CVD) occur in developing countries [1, 3, 7]. The Indian subcontinent (India, Nepal, Bangladesh, Pakistan, Sri Lanka and Bhutan) is home to 20% of the world’s population and may be one of the regions with the highest burden of CVD in the world [8].
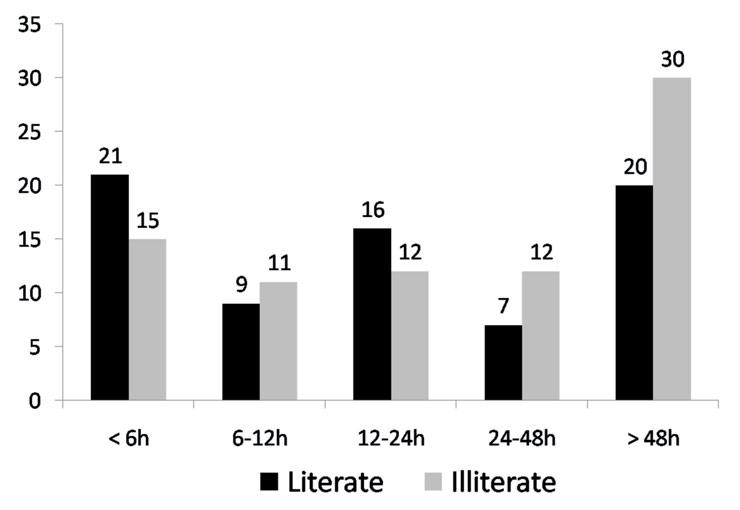
Figure 4
Educational status and time to presentation from onset of symptoms (number of patients).
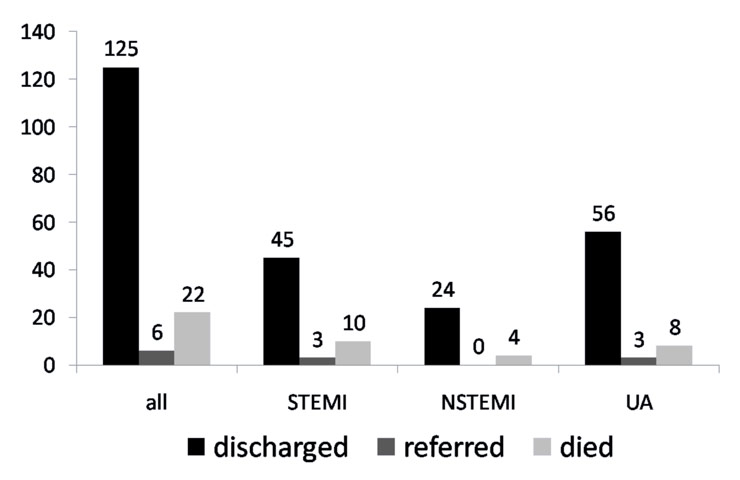
Figure 5
In-hospital outcome (number of patients).
Despite this background, the present study documents that only 153 patients were admitted with the diagnosis of ACS to the single CCU available in eastern Nepal. It is thus fair to assume that this patient group only represents the tip of an iceberg, and that the overall incidence of ACS must be larger by several orders of magnitude. In a resource-poor country, such as Nepal, where health care costs are paid by the patients themselves, as there is no widely available insurance system, and a large majority of the people live below the poverty line, lack of early diagnosis and timely referral hinder identification and proper management of ACS. Even among the patients in the present cohort, who by definition were eventually able to afford the cost of hospital care, a large proportion (63%) presented to the hospital 12 hours or more after the onset of symptoms. This reflects a lack of awareness by the patients and their families about the potential consequences of chest pain, together with the inability to diagnose possible ACS in health posts and district hospitals. These elements often combine to delay or inhibit referrals to a centre equipped with diagnostic and management facilities. Above all, the problem of transportation of the patient to the hospital is one of the most important causes of delay in our study. The BPKIHS does not operate its own ambulance service and the available ambulances (without paramedical staff or basic resuscitation facilities such as oxygen, defibrillators or medication) are run either by private hospitals or non government organisations, and the cost of transportation also has to be borne by the patients themselves. Since this is expensive, patients often travel by bus or taxi and sometimes ride pillion on a motorcycle or a bicycle to reach the emergency room. Most of the patients in this series presented directly to the emergency room (73%), and only 18% were admitted through referral from another hospital or health post.
The mean age of patients in our study was 62 years and only 17% of patients were less than 50 years of age. This is not very different from what is observed in registries of ACS patients from western Europe [9], while studies from the Indian subcontinent have reported that patients presenting with ACS were often younger (53–58 years) [4, 10] The reason for this difference is not known, but it can be speculated that it is due to a selection bias, as there is a large population of retired Gurkhas soldiers from the British army living in Dharan. A prior study, done by Acharya et al a year earlier at the BPKIHS, also found that the mean age of patients presenting with ACS was 62 years and 18% were less than 50 years old [11].
Only 40% of patients with STEMI presented within 12 hours after the onset of symptoms, and thus had a “classical” indication for thrombolysis. Given the lack of alternative modes of reperfusion, however, we usually considered thrombolysis for all patients who presented within 24 hours of symptom onset. 53% of all patients presenting within this broadened time window were thus thrombolysed with streptokinase. Despite this, several patients did not receive thrombolysis, as they were unable to pay for it (the cost of 1.5 million units of streptokinase in 2008 was approximately Nepali Rupees 4000, i.e. CHF 60). Beta-blockers were only used for 32% of patients, probably because 47% had evidence of heart failure at admission. Most patients would usually have received them at the time of discharge or at a follow-up visit.
Nepal currently has only two centres where percutaneous coronary interventions (PCI) are performed and they are both in Kathmandu, which is 500 kilometres west from BPKIHS. Thus the only way that a patient can be referred for a primary PCI is to be airlifted by a helicopter, as road travel would take 10 hours at least. Transferring a patient by helicopter in Nepal is very expensive and time consuming. There are no air-ambulances and therefore helicopters have to be chartered from private companies to fly out from Kathmandu to Dharan and then back, a process that thus delays treatment by at least three hours. We were only able to refer six patients to Kathmandu for a PCI, which was semi-elective in all cases.
The high in-hospital mortality (14%) that was observed in our study can thus be ascribed to markedly delayed presentation, lack of resources for the best possible available care, and major logistic difficulties to organise timely PCI.
It was also noted that patients who were illiterate had a trend towards a higher mortality rate than those who were literate, but this did not reach statistical significance (19% vs. 10%). Low education status has been shown to be the most consistent socioeconomic marker associated with risk and mortality in ACS [12, 13].
| Table 5: Baseline characteristics and outcome of ACS as a function of educational status. | |||
| Literate | Illiterate | p | |
| Overall (n = 153) | 73 (48%) | 80 (52%) | |
| Mean age | 63 ± 11 | 61 ± 12 | ns |
| Females | 11 (15%) | 51 (64%) | 0.001 |
| Smoking | 43 (59%) | 50 (62%) | ns |
| Diabetes | 12 (16%) | 9 (11%) | ns |
| Hypertension | 37 (51%) | 23 (29%) | 0.004 |
| Sedentary lifestyle | 11 (15%) | 6 (8%) | ns |
| Heart failure > Killip 1 | 32 (44%) | 49 (61%) | 0.02 |
| STEMI | 35 (48%) | 23 (29%) | 0.02 |
| NSTEMI | 14 (19%) | 14 (18%) | ns |
| UA | 24 (16%) | 43 (54%) | 0.02 |
| Thrombolysis | 13 (18%) | 7 (9%) | ns |
| Mortality | 7 (10%) | 15 (19%) | ns |
Although the quality of care and compliance with guidelines was generally good for those patients with ACS who reached the BPKIHS, there is an obvious need for major improvements. Ideally, this should include 1) better awareness of the general public regarding preventive measures, lifestyle modification and potential pharmacological treatment of cardiovascular risk factors; 2) information campaigns concerning the clinical symptoms of coronary disease; 3) improved training of primary health care professionals and ECG availability at local health centres; 4) established referral patterns and transport to treatment centres; 5) availability of financial support for those patients with insufficient means; and 6) availability of coronary angiography and angioplasty on site, at least for those selected patients at high risk most likely to benefit.
In the course of 2011 a coronary angiography laboratory should become operational in the BPKIHS, and it is hoped that this will help catalyse an improved chain of treatment for patients with ACS in eastern Nepal. A future comparison of patient numbers, applied treatment, and hospital outcomes with the present data should help to identify any potential benefits.
Dr. Shreshta was funded by the “Fondation pour la Recherche Cardiovasculaire de l’Hôpital de la Tour”, and was training as a fellow in interventional cardiology at the Inselspital, Bern in 2010, when he authored this work. None of the authors have any conflicts of interest to declare.
1 WHO, The World Health Report 2002: Reducing Risks, Promoting Healthy Life, World Health Organization, Geneva (2002).
2 Gaizano TA, Bitton A, Anand S, Abrahams-Gessel S, Murphy A. Growing epidemic of coronary heart disease in low- and middle-income countries. Curr Probl Cardiol. 2010;35(2):72–115.
3 Reddy KS. Cardiovascular Disease in Non-Western Countries. N Engl J Med. 2004;350:2438–40.
4 Xavier D, Pais P, Devereaux PJ, Xie C, Prabhakaran D, Reddy KS, et al; CREATE registry investigators. Treatment and outcomes of acute coronary syndromes in India (CREATE): a prospective analysis of registry data. Lancet. 2008;371(9622):1435–42.
5 Joshi P, Islam S, Pais P, Reddy S, Dorairaj P, Kazmi K, et al. Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. JAMA. 2007;297(3):286–94.
6 Mohan V, Deepa R, Rani SS, Premalatha G; Chennai Urban Population Study (CUPS No.5). Prevalence of coronary artery disease and it relationship to lipids in a selected population in South India: The Chennai Urban Population Study (CUPS no.5). J Am Coll Cardiol. 2001;38(3):682–7.
7 Murray CJ, Lopez AD, editors. The global burden of disease. A comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020. Cambridge, MA: Harvard University Press; 1996.
8 Goyal A, Yusuf S. The burden of cardiovascular disease in the Indian subcontinent. Indian J Med Res. 2006;124:235–44.
9 Radovanovic D, Urban P, Simon R, Schmidli M, Maggiorini M, Rickli H, et al. Outcome of patients with acute coronary syndrome in hospitals of different sizes. A report from the AMIS plus registry. Swiss Med Wkly. 2010;140: 314–22.
10 Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas Fe, et al; INTERHEART Study Investigators. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364(9438):937–52.
11 Acharya P, Adhikari RR, Bhattarai J, Shrestha NR, Sharma SK, Karki P. Delayed presentation of acute coronary syndrome: a challenge in its early management. JNMA J Nepal Med Assoc. 2009;48(173):1–4.
12 Rosengren A, Subramanian SV, Islam S, Chow CK, Avezum A, Kazmi K et al; INTERHEART Investigators. Education and risk for acute myocardial infarction in 52 high, middle and low-income countries: INTERHEART case-control study. Heart. 2009;95(24):2014–22.
13 Gerber Y, Weston SA, Killian JM, Therneau TM, Jacobsen SJ, Roger VL. Neighborhood income and individual education: effect on survival after myocardial infarction. Mayo Clin Proc. 2008;83(6):663–9.