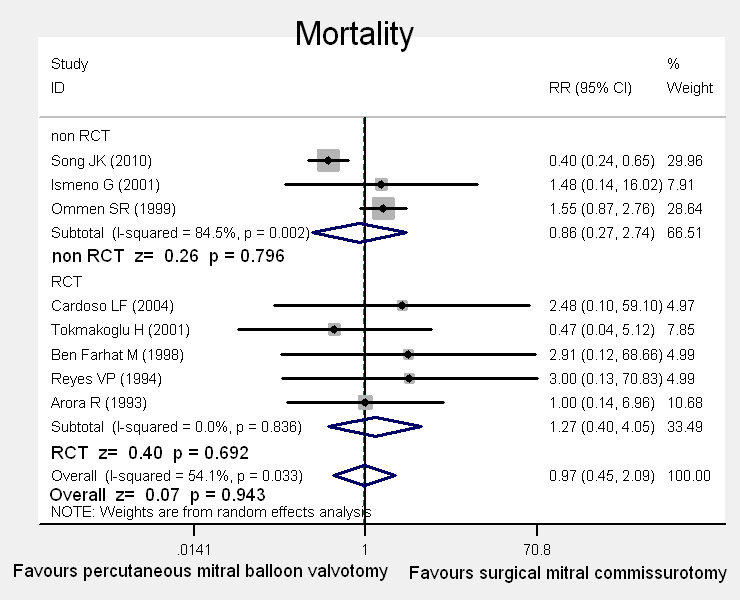
Figure 1
Forest plot showing the results from the meta-analysis of trials reporting all cause mortality after mitral valvulotomy using surgical and percutaneous balloon commissurotomy.
DOI: https://doi.org/10.4414/smw.2011.13180
Mitral stenosis (MS), usually caused by rheumatic fever, maintains a high prevalence in developing countries and among emigrants who have emigrated from areas where rheumatic fever is still endemic [1], hence, continued awareness of this condition is warranted. Percutaneous mitral balloon valvotomy, introduced by Inoue in 1984 [2], has evolved to be the ‘‘gold standard’’ treatment option in patients with mitral stenosis due to early morbidity and promising immediate haemodynamic benefits, whereas traditional thoracotomy surgery has been reserved for the minority of patients concomitant with atrial thrombi or unfavourable mitral valve morphologic features, such as heavy calcification. Due to the relatively “young” history application and a “blinded” approach to commissure splitting, many questions are still open regarding percutaneous mitral balloon valvotomy. Moreover, many comparative studies, performed between series of patients treated with these two techniques have produced some confusing, controversial results, even in the prospective randomised trials [3–5]. Therefore, a systematic review of the literature was performed to assess the efficacy and safety in patients undergoing percutaneous mitral balloon and surgical thoracotomy valvotomy.
A systematic literature retrieval was performed in Pubmed (1966 to 2010.9), EMBASE (1974 to 2010.9), and the Cochrane Library 2010, Issue 9. We employed the key words “(percutaneous, transvenous, balloon valvuloplasty, commissurotomy or valvotomy) and (mitral stenosis or mitral valve stenosis) and clinical trial”. In order to broaden the range of the retrieval, all clinical control trials of mitral stenosis comparing balloon and surgical commissurotomy were overviewed individually. Moreover, the abstracts from major cardiology and cardiac surgery meetings available between 2003 and 2010 were manually retrieved. References in the concerning papers were also reviewed irrespective of language, and we even attempted to correspond with authors of relevant research. The searches were not limited by language or publication year.
All clinical research (randomised controlled trials and case-control studies), evaluating mitral stenosis treated with percutaneous balloon intervention and thoracotomy surgery, were recorded. Studies were included regardless of population demography, publication year, conference proceedings or language. Studies were excluded if the research subjects included were confined in a frame of a particular population such as pregnancy and repeated patients. In addition, if the publication did not provide the outcomes of interest including main outcomes of mortality, complication, re-intervention, mitral regurgitation and mitral valve area, then the study was excluded. Otherwise, the pooling results could not be analysed from the presenting data. No control group, of course, was used within our exclusion criteria.
Two reviewers independently abstracted information from each study for study title, authors, publication year, institution, population profiles, study design, follow up, inclusion and exclusion criterion, and main outcomes of mortality, complications, re-intervention, mitral regurgitation and mitral valve area. If literature consisting of results at several different points in follow up were published by the same investigators, population profiles in the first report were included in our study, along with information for outcomes at subsequent follow up periods abstracted from the latter reports. When there were several reports with the identical results followed up at similar period ranges, by the same group, the literature with a better quality and containing more information was chosen for inclusion. Discordances were resolved by re-review or consensus review.
The quality of inclusive randomised trials was evaluated with predetermined criteria [6] by two reviewers independently. The assessment was based on the randomisation methods, the use of intention-to-treat analysis, the report of dropout rates, allocation concealment, and the extent to which valid results were depicted. Discordances were resolved by re-review or consensus review.
This systematic assessment was performed according to meta-analysis guidelines recommended by the Cochrane Collaboration and were met strictly [7]. We employed relative risk (RR) as the summary statistics for categorical data, demonstrating the adverse ratio in the study group (percutaneous balloon commissurotomy) relative to the control group (surgical commissurotomy). A relative risk with a value <1 was the favour of the study group, and the relative risk was taken as statistical significance when the p value was at 0.05. Furthermore, the 95% confidence intervals (CI) excluded 1. Continuous data were expressed as standardised mean difference (SMD) and an overall SMD was calculated. A fixed effect model was chosen on the presumption that variation in the individual trial results occurred about a true mean. Conversely, the random model was adopted. The heterogeneity for summary effects was calculated through the statistics of chi-square and I2, and I2 more than 50% regarded existing heterogeneity. In the analysis of sensitivity, repeating the analysis with another effect model or omitting data in low quality trials was performed. All statistical analyses were carried out with Stata 10 (StataCorp, College Station, Tex).
Our search for clinical trials, comparing the efficacy of managing mitral stenosis with percutaneous balloon intervention and thoracotomy surgery, yielded 119 potentially relevant articles. Of these, 98 articles were excluded for just concerning percutaneous intervention with different balloons as research procedures, or owing to not including a conventional surgery as a control arm, or due to not considering outcomes which the current study was focused on. Following this exclusion, a total of 21 [3–5, 8–25] articles reporting on clinical trials met our inclusion criterion initially, of which 5 articles [4, 9, 13, 24, 25] were ruled out for the cause of reporting the same trials with different perspectives, and 4 were excluded due to there been insufficient information for extraction [15–17, 20]. Finally, the data from 12 clinical studies between 1966 and 2010 [3–5, 8, 10–12, 14, 18–19, 21–23] with comparison of percutaneous balloon intervention and thoracotomy surgery (open or closed) in managing mitral stenosis were chosen to be overviewed in this study. Among these trials, some took open and closed surgical mitral valvotomy into consideration separately for comparison with percutaneous balloon intervention, and some in which open and closed surgery were merged into a surgical thoracotomy valvotomy group for comparison.
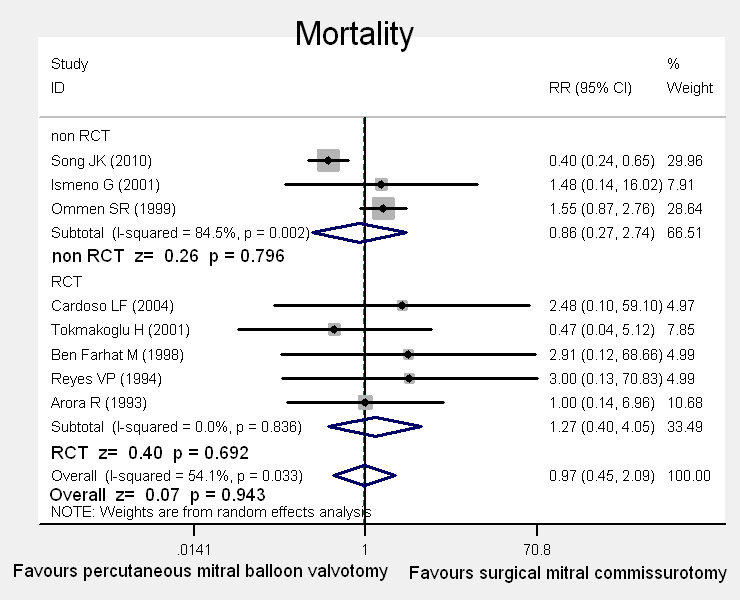
Figure 1
Forest plot showing the results from the meta-analysis of trials reporting all cause mortality after mitral valvulotomy using surgical and percutaneous balloon commissurotomy.
These studies used a total of 2029 patients. The age of study enrolment had a mean of 31 years, ranging from 17 to 60 years. Roughly, a majority of the population scored below 9 in the echocardiographic score, and the proportion of female subject enrolled in the research ranged from 16% to 44%. The study designs were prospectively randomised in seven groups, and another five studies were case control designed. See table 1.
The overall quality was roughly assessed on a three-point scale according to the Cochrane handbook [7]: all the inclusion articles scored B (moderate quality). These quality criteria included the method of randomisation, the use of intention-to-treat analysis, the report of dropout rates, allocation concealment and the extent to which valid outcomes were described.
| Table 1: Study and patient characteristics of studies included in the meta-analysis. | ||||||||
| First author | Publication year | Study design | Inclusion criteria | Number(S/P) | Follow up (month) | Mean age (S/P) | Baseline mitral area (S/P) | Echo score (S/P) |
| Song JK [3] | 2010 | case control | MS | 159/402 | 106 ± 27 | 52 ± 9/44 ± 11 | 0.86 ± 0.26/0.95 ± 0.21 | – |
| Rifaie O [5] | 2009 | random prospective | MS | 20/20 | 99 ± 12 | 25 ± 8/26 ± 9 | 1.1 ± 0.3/0.9 ± 0.4 | 6 ± 2.1/5.8 ± 2.1 |
| Cardoso LF [8] | 2004 | random prospective | MS | 37/44 | 60 | 32.5 ± 7.2/32.9 ± 9.5 | 0.94 ± 0.2/1.1 ± 0.2 | 7.1 ± 1.30/7.1 ± 1.1 |
| Ismeno G [10] | 2001 | case control | MS | 82/111 | 49.9 ± 28 | 48.9 ± 10/46.5 ± 13.8 | – | – |
| Tokmakoglu H [11] | 2001 | random prospective | MS | 280/300 | 12 | 50 ± 7/48 ± 11 | 1.1 ± 0.2/1.1 ± 0.2 | – |
| Ommen SR [12] | 1999 | case control | MS | 267/102 | 60 | 44 ± 10/54 ± 14 | – | – |
| Ben Farhat M [14] | 1998 | random prospective | MS | 60/30 | 84 | 27 ± 9/29 ± 12 | 0.9 ± 0.2/0.9 ± 0.16 | 6.1 ± 1.1/6.0 ± 1.0 |
| Reyes VP [18] | 1994 | random prospective | MS | 30/30 | 36 | 31 ± 9/30 ± 9 | 0.9 ± 0.3/0.9 ± 0.3 | 7.0 ± 1.1/6.7 ± 1.3 |
| Arora R [19] | 1993 | random prospective | MS | 100/100 | 22 ± 8.3 | 19.9 ± 6.4/19.4 ± 5.47 | 0.79 ± 0.2/0.85 ± 0.3 | – |
| Momomura S [22] | 1992 | case control | MS | 28/34 | 19 ± 11 | 31 ± 10/30 ± 9 | 1.1 ± 1.4/1.0 ± 0.3 | – |
| Shrivastava S [21] | 1992 | case control | MS | 20/20 | 12 | 28 ± 10/31 ± 13 | 0.62 ± 0.27/0.68 ± 0.24 | – |
| Patel JJ [23] | 1991 | random prospective | MS | 22/23 | 48h | 26 ± 10/30 ± 11 | 0.7 ± 0.2/0.8 ± 0.3 | 6 ± 2/6 ± 1 |
| MS indicates Mitral valve Stenosis; –, unavailable; S/P, Surgery / Percutaneous balloon | ||||||||
There were eight studies reporting mortality after percutaneous balloon intervention and thoracotomy surgery, among which five were randomised control trials (RCT), with follow-ups ranging from one year to seven years. This systematic assessment demonstrated comparable mortality in the follow-up period between the two groups (4.13% in percutaneous balloon intervention vs. 3.24% in thoracotomy surgery; relative risk 0.97, 95% confidence interval 0.45–2.09). In the sub-analysis, the pooling result in the subgroup for RCT was also consistent with the general comparison, which obtained a RR 1.27, 95%CI: 0.4―4.05, p = 0.693. See fig. 1.
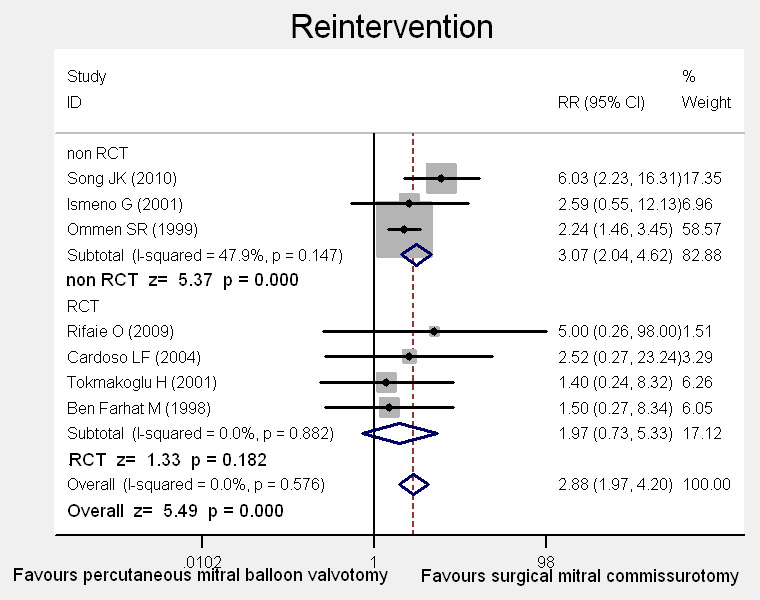
Figure 2
Forest plot showing the results from the meta-analysis of trials, reporting re-intervention and comparing surgical and percutaneous balloon commissurotomy.
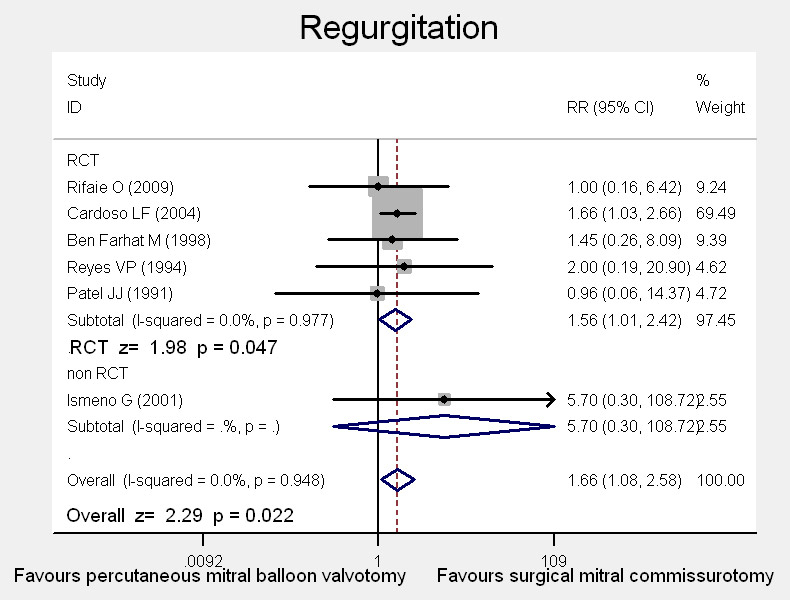
Figure 3
Forest plot showing the results from the meta-analysis of trials reporting new onset mitral regurgitation, and comparing surgical and percutaneous balloon commissurotomy.
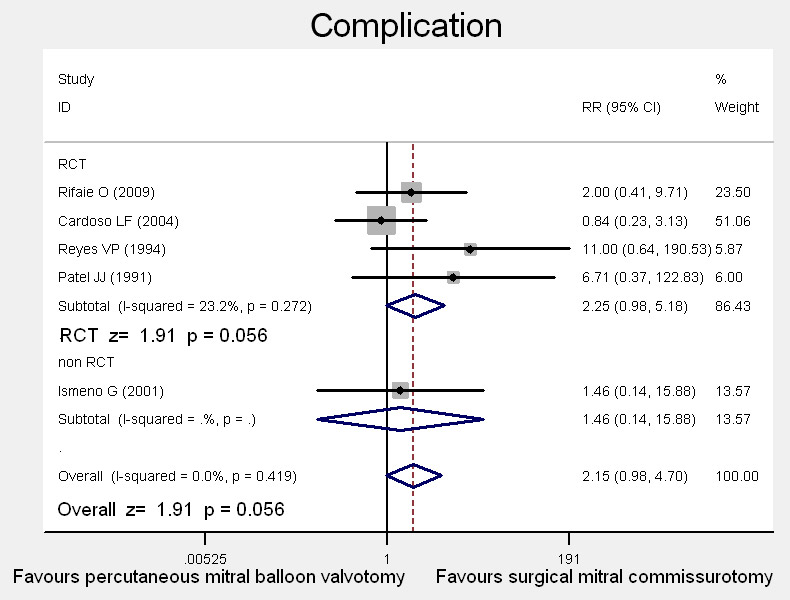
Figure 4
Forest plot showing the results from the meta-analysis of trials reporting significant surgical complications after mitral valvulotomy using surgical and percutaneous balloon commissurotomy.
Of the twelve studies, seven provided data on re-intervention including re-operation and repeated percutaneous balloon intervention for significant mitral valves dysfunction, with the outcome assessment time varying from one year to seven years. The pooling analysis obtained a higher relative risk of re-intervention in percutaneous balloon intervention compared to the thoracotomy surgery group of 2.88 (95% confidence interval 1.97–4.20; p <0.01), with no evidence to suggest statistical heterogeneity (p = 0.576). The variation in relative risk attributable to heterogeneity (I2) was 0 (see fig. 2). Although in the RCT stratification, there seemed comparable relative risks in re-intervention between groups, the small size sample limited the strength of RCT. Hence, by pooling these small size sample studies, the effective sample size is greatly increased in the meta analysis, and consequently more reliable outcomes can be obtained.
Mitral regurgitation caused by intervention was defined as new-onset or enhanced original insufficiency equal to or greater than grade 1 during the follow-up period. Six clinical trials, focusing on the mitral regurgitation related to intervention, demonstrated that there was a significantly higher occurrence of mitral regurgitation in patients with percutaneous balloon intervention relative to thoracotomy surgery. Fixed effect (Mantel-Haenszel) pooled relative risk was 1.66 (95%CI 1.08–2.58, p = 0.022). No heterogeneity was detectable (p = 0.948). Only by pooling the outcomes of RCT, did we also get the identical result in favour of surgery group (RR = 1.56, 95% CI 1.01–2.42). See fig. 3.
Besides operative mortality and mitral insufficiency, a variety of significant clinical complexities may be encountered such as haemopericardium, low-output state, intractable arrhythmia, cerebrovascular accident or excessive bleeding and so on. Data from studies that compared the percutaneous balloon intervention and thoracotomy surgery with regard to significant operative complications were available in five articles. Pooling the results yielded a non significant difference between the percutaneous balloon intervention and thoracotomy surgery group with a relative risk of 2.15, 95% confidence interval of 0.98–4.70, and p = 0.056. There was no statistical heterogeneity (fig. 4). The stratification for RCT and case-control trial did not affect the results.
Patient data recorded during echocardiographic monitoring in the assessment about the mitral valve orifice and the mitral valve area in diastole (MVA) were focused on commonly, in addition to any backflow. Compared to those for the thoracotomy surgery, patients undergoing percutaneous balloon intervention presented significantly a worse effect in preserving the MVA: SMD –0.30, 95% CI: –0.42- –0.18, p <0.01. In the sub-analysis, the result in the subgroup of RCT was also consistent with the general comparison, which obtained a SWD –0.30, 95%CI: –0.43 - –0.18, p <0.01 (fig. 5).
We did not identify any significant difference in the relative risk and heterogeneity for the outcome of interest, omitting the case control studies.
Nowadays, there are still a great number of patients with rheumatic mitral stenosis, accounting for the majority of heart valve diseases particularly in the clinical practice of developing countries [1]. Surgical treatment through open or closed mitral valvuloplasty has long been proven to be associated with excellent results with the late mortality rate around 3% [26]. From 1984, percutaneous balloon mitral commissurotomy was introduced to clinical practice for the management of patients with mitral stenosis. It is generally supposed that minimal invasiveness represents minor mortality and preferred event-free outcomes, which has also been confirmed in some clinical studies [11, 14]. However, according to the pooling data, this systematic assessment did not demonstrate any significant difference in terms of mortality in the follow-up period between the two groups (4.13% in percutaneous balloon intervention vs. 3.24% in thoracotomy surgery; relative risk 0.97, 95% confidence interval 0.45–2.09). Regarding this discrepancy, we considered that findings in previous trials may have been largely owing to insufficient statistical power, involving small numbers of inclusion subjects (less than 50 for each arm) and containing selection biases. Hence, this Meta analysis undertaken provides the increased statistical power resulting from a comprehensive pooling of subjects across studies, and produces a single large sample and increases the statistical power enough to identify the truth behind confounding variables. In addition, population demographics such as age and baseline echocardiographic score reflecting the mitral valve morphologic function are vital factors for long-term survival. As reported by Song [3], the observed (unadjusted) survival after percutaneous mitral valvuloplasty was significantly lower compared with after open heart surgery, whereas there was no significant difference after adjusting for age, gender, left atrial anteroposterior diameter and echocardiographic score.
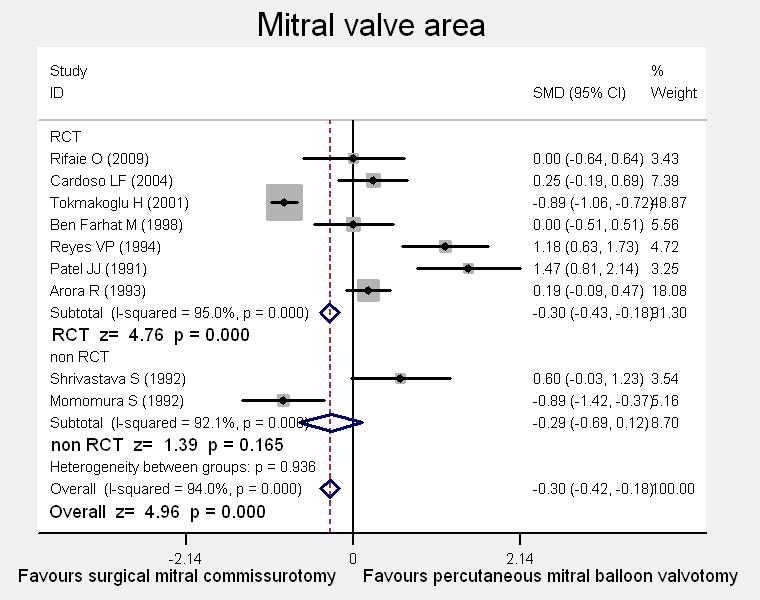
Figure 5
Forest plot showing the results from the meta-analysis of trials reporting mitral valve area and comparing surgical and percutaneous balloon commissurotomy.
It has been shown by series reporting long-term follow-ups after surgical and percutaneous balloon commissurotomy that progressive clinical deterioration occurs with a linear trend year over year. Mitral re-stenosis, which should be considered as re-intervention, is one of the main causes of progression after commissurotomy, and the other causes, being the consequence of unsatisfactory results of valvuloplasty, cover a residual stenosis or a severe mitral insufficiency. This re-intervention carries an inherent risk of morbidity, mortality and surgical-related complications, influencing the efficacy and safety of the procedure managing mitral stenosis. In this pooling analysis, we obtained a lower relative risk of re-intervention in the thoracotomy surgery group compared to percutaneous balloon intervention. Anatomical studies from selected patients with recurrent mitral stenosis [27] have shown that mitral restenosis after commissurotomy may be related to recurrent agglutination of the commissures, but also due to the rigidity of the leaflets and/or the morbid sub-valvular chordaes, with mitral orifice opening persisting from the original status. On the basis of these mechanisms, surgical commissurotomy has the inherent superiority over percutaneous balloon commissurotomy in providing the potential for additional surgical techniques to be performed to manage the mild calcium deposit fusion and the morbid sub-valvular apparatus, frequently accompanying mitral stenosis and being important prognostic factors for late re-intervention. Finally, it should be considered that rheumatic mitral valve disease is a continuously progressive lesion. Although both procedures achieved a satisfactory mitral valve area through splitting the morbid fusion even at long-term follow-ups, pathogenesis was not disrupted by this mechanical intervention. Due to the variation of force in the power and orientation imposed on the commissures, the efficacy might differ. It was demonstrated by Essop [28] that restenosis rates were 0.08 cm2 /year for percutaneous mitral valvuloplasty compared to 0.07 cm2/year for thoracotomy surgery.
Another point of discussion is the higher occurrence of new-onset post-procedure mitral regurgitation in patients with percutaneous mitral valvuloplasty compared to those with thoracotomy surgery. After percutaneous balloon mitral commissurotomy, approximately 30% to 50% of patients may experience mild mitral insufficiency [29]. According to the report from Acar C. [30], traumatic lesions could be the leading cause responsible for mitral regurgitation, which involved both leaflet tissue and the sub-valvular apparatus including tears of the anterior and posterior leaflet, paracommissural tears and papillary muscle ruptures. Some anatomical changes of the leaflets might be regarded as predisposing factors for the regurgitation including: 1) tight fibrotic mitral stenosis with very short chordate, and firm adhesions between the commissural area and the thickened underlying papillary muscle; 2) a unilateral commissural fusion; and 3) thin friable leaflet tissue. Hence, more caution should be made to prevent post-procedural mitral regurgitation, when this morphology is encountered. However, mitral insufficiency requiring surgical intervention occurs in only approximately 4% of patients undergoing percutaneous mitral valvuloplasty, indicating the decrease or even disappearance of mitral insufficiency at long-term follow-up. Gradual healing of over-split commissures or recovery of papillary muscle function might explain the regression of mitral regurgitation at follow-up. The experience of the catheteration technician, the appropriate selection of patients, and the improvement in the technique used should contribute to minimise the rate of this complication, comparable to that of direct vision surgery.
Due to data limitations, a further sub-analysis aiming to clarify the effects of different basic characteristics or concomitances in the efficacy and safety would be in vain. However, the control trials included all balanced the patients’ baseline characteristics with no significant difference between groups in the proportion of age or cardiac performance. In addition, in spite of best efforts made to choose clear outcomes, bias in the criterion-defining of events still could not be avoided. Taking the mitral valve area as an example, the pooling result suggested a significantly far better effect preserving the MVA in the surgical group, but demonstrating a significant heterogeneity. This might be attributed to the different methods applied in the practice. A global meta-analysis was not performed and the analysis concentrated on more homogeneous subgroups of patients by aggregating the data of studies conducted in similar patient populations. Nevertheless, it was impossible to go further to analyse papers in the subgroups due to the limited number of studies. However, there seems to be a consistency in the effect of sustaining the mitral valve area for surgical valvuloplasty in most of the included prospective random trials up to and over a follow-up period of 7 years. For this reason, we cautiously consider that the association is valid and can be generalised. In addition, publication bias should be always kept in mind. It was difficult to obtain complete raw data for some trials.
This is the first systematic review and meta-analysis on the topic of mitral commissurotomy. It offers an up-to-date and the most complete overview of all human clinical trials concerning the management for pure mitral stenosis using balloon interventions and surgery, because it is the result of an extensive search, including all studies regardless of region and population. In addition, maximum efforts were done to minimise missing or incomplete data by attempting to contact all authors. Although we tried to include a high number of quality studies, it turned out that the data were consistent at a certain extent and heterogeneity existed owing to a majority of case control trials. It should be stressed that the results need to be confirmed by an adequately designed prospective study, and the exact value of long term follow up needs to be calculated.
In conclusion, this Meta analysis did not show any significant differences in terms of operative, late mortality and complication between percutaneous balloon and surgical mitral commissurotomy. Incidences of new onset mitral regurgitation and late re-intervention were significantly higher in patients with balloon intervention. Therefore, percutaneous transvenous mitral commissurotomy (PTMC) should only be recommended in patients with high risk factors. Surgical mitral commissurotomy remains the treatment of choice for rheumatic mitral valve stenosis with pliable leaflets.
| Table 2: Quality assessment of randomised clinical studies inclusion. | ||||
| Study | Allocation Concealment | Blinding | Randomised procedure | Lost to Follow-Up |
| Rifaie O [5] | No | No | No | Yes |
| Cardoso LF [8] | No | No | Yes | Yes |
| Tokmakoglu H [11] | No | No | No | Yes |
| Ben Farhat M [14] | No | No | Yes | Yes |
| Reyes VP [18] | No | No | No | Yes |
| Arora R [19] | No | No | No | Yes |
| Patel JJ [23] | No | No | No | Yes |
No financial support and no other potential conflict of interest relevant to this article was reported.
No financial support and no other potential conflict of interest relevant to this article was reported.
1 Carapetis JR, McDonald M, Wilson NJ. Acute rheumatic fever. Lancet. 2005;366:155–68.
2 Inoue K, Owaki T, Nakamura T, Kitamura F, Miyamoto N. Clinical application of transvenous mitral commissurotomy by a new balloon catheter. J Thorac Cardiovasc Surg. 1984;87:394–402.
3 Song JK, Kim MJ, Yun SC, Choo SJ, Song JM, Song H, et al. Long-term outcomes of percutaneous mitral balloon valvuloplasty versus open cardiac surgery. J Thorac Cardiovasc Surg. 2010;139(1):103–10.
4 Cotrufo M, Renzulli A, Ismeno G, Caruso A, Mauro C, Caso P, De Simone L, Violini R. Percutaneous mitral commissurotomy versus open mitral commissurotomy: a comparative study. Eur J Cardiothorac Surg. 1999;15(5):646–51.
5 Rifaie O, Abdel-Dayem MK, Ramzy A, Ezz-El-Din H, El-Ziady G, El-Itriby A, et al. Percutaneous mitral valvotomy versus closed surgical commissurotomy. Up to 15 years of follow-up of a prospective randomized study. J Cardiol. 2009;53(1):28–34.
6 Jadad AR, Moore RA, Carroll D. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12.
7 Clarke M,OxmanAD. Cochrane reviewer’s handbook 4.1.3 [updated June 2001]. In: The Cochrane Library, Issue 3: Oxford: Update Software, 2001.
8 Cardoso LF, Grinberg M, Pomerantzeff PM, Rati MA, Medeiros CC, Vieira ML, et al. Comparison of open commissurotomy and balloon valvuloplasty in mitral stenosis. A five-year follow-up. Arq Bras Cardiol. 2004;83(3):248–52.
9 Cardoso LF, Grinberg M, Rati MA, Pomerantzeff PM, Medeiros CC, Tarasoutchi F, Martinez E. Comparison between percutaneous balloon valvuloplasty and open commissurotomy for mitral stenosis. A prospective and randomized study. Cardiology. 2002;98(4):186–90.
10 Ismeno G, Renzulli A, De Feo M, Della Corte A, Mauro C, Romano G, Mininni N, Cotrufo M. Surgery of rheumatic mitral stenosis: comparison of different techniques. Acta Cardiol. 2001;56(3):155–61.
11 Tokmakoglu H, Vural KM, Ozatik MA, Cehreli S, Sener E, Tasdemir O. Closed commissurotomy versus balloon valvuloplasty for rheumatic mitral stenosis. J Heart Valve Dis. 2001;10(3):281–7.
12 Ommen SR, Nishimura RA, Grill DE, Holmes DR Jr, Rihal CS. Comparison of long-term results of percutaneous mitral balloon valvotomy with closed transventricular mitral commissurotomy at a single North American Institution. Am J Cardiol. 1999;84(5):575–7.
13 Cardoso LF, Rati MA, Pomerantzeff PM, Medeiros CC, Tarasoutchi F, Rossi EG, et al. Comparison between percutaneous balloon valvuloplasty and open commissurotomy for mitral stenosis [Article in Portuguese] Arq Bras Cardiol. 1998;70(6):415–21.
14 Ben Farhat M, Ayari M, Maatouk F, Betbout F, Gamra H, Jarra M, et al. Percutaneous balloon versus surgical closed and open mitral commissurotomy: seven-year follow-up results of a randomized trial. Circulation. 1998;97(3):245–50.
15 Raju S Iyer, Rajnish Jain, Manoj Padmanabhan, Abha Chandra, Sanjeev Agarwal, et al. Closed Mitral Valvotomy Versus Balloon Valvuloplasty: A Comparison of 100 Cases. Asian Cardiovasc Thorac Ann. 1998;6:285–7.
16 Essop R, Rothlisberger C, Dullabh A, Sareli P. Can the long-term outcomes of percutaneous balloon mitral valvotomy and surgical commissurotomy be expected to be similar? J Heart Valve Dis. 1995;4(5):446–52.
17 Olmos A, Seguel I, Gajardo J, Ghyra A, Santander C, Alarcón E, et al. Percutaneous mitral valvuloplasty and open mitral commissurotomy: comparison of 2 techniques in immediate results [Article in Spanish] Rev Med Chil. 1994;122(3):274–82.
18 Reyes VP, Raju BS, Wynne J, Stephenson LW, Raju R, Fromm BS, et al. Percutaneous balloon valvuloplasty compared with open surgical commissurotomy for mitral stenosis. N Engl J Med. 1994;331(15):961–7.
19 Arora R, Nair M, Kalra GS, Nigam M, Khalilullah M. Immediate and long-term results of balloon and surgical closed mitral valvotomy: a randomized comparative study. Am Heart J. 1993;125(4):1091–4.
20 Cohen JM, Glower DD, Harrison JK, Bashore TM, White WD, Smith LR, et al. Comparison of balloon valvuloplasty with operative treatment for mitral stenosis. Ann Thorac Surg. 1993;56(6):1254–62.
21 Shrivastava S, Mathur A, Dev V, Saxena A, Venugopal P, SampathKumar A. Comparison of immediate hemodynamic response to closed mitral commissurotomy, single-balloon, and double-balloon mitral valvuloplasty in rheumatic mitral stenosis. J Thorac Cardiovasc Surg. 1992;104(5):1264–7.
22 Momomura S, Takenaka K, Serizawa T, Chikada M, Kotsuka H, Matsunoga H, Furuse A. Percutaneous transvenous, mitral commissurotomy versus open mitral commissurotomy. [Article in Japanese] Nippon Geka Gakkai Zasshi. 1992;93(9):1016–9.
23 Patel JJ, Shama D, Mitha AS, Blyth D, Hassen F, Le Roux BT, Chetty S. Balloon valvuloplasty versus closed commissurotomy for pliable mitral stenosis: a prospective hemodynamic study. J Am Coll Cardiol. 1991;18(5):1318–22.
24 Turi ZG, Reyes VP, Raju BS, Raju AR, Kumar DN, Rajagopal P, et al. Percutaneous balloon versus surgical closed commissurotomy for mitral stenosis. A prospective, randomized trial. Circulation. 1991;83(4):1179–85.
25 Kirklin JW. Percutaneous balloon versus surgical closed commissurotomy for mitral stenosis. Circulation. 1991;83(4):1450–1.
26 Grinberg M, Bellotti G, Pileggi F. Aspectos do planejamento terapêutico na estenose mitral. Arq Bras Cardiol. 1983;51:289–95.
27 Iung B, Garbarz E, Michaud P, Mahdhaoui A, Helou S, Farah B, et al. Percutaneous mitral commissurotomy for restenosis after surgical commissurotomy: late efficacy and implications for patient selection. J Am Coll Cardiol. 2000;35(5):1295–302.
28 Essop R, Rothlisberger C, Dullabh A, Sareli P. Can the long term outcomes of percutaneous ballon mitral valvotomy and surgical commissurotomy be expected to be similar? J Heart Valve Dis. 1995;4:446±45
29 Black MD, Campagna M, Bedard P, Marquis JF, Walley VM. Severe mitral insufficiency post-balloon valvuloplsty: The late changes found in a disrupted mitral valve. Cathet Cardiovasc Diagn. 1990;21:99–102.
30 Acar C, Jebara VA, Grare P, Chachques JC, Dervanian P, Vahanian A, Carpentier A. Traumatic mitral insufficiency following percutaneous mitral dilation: anatomic lesions and surgical implications. Eur J Cardiothorac Surg. 1992;6(12):660–3.