Figure 1
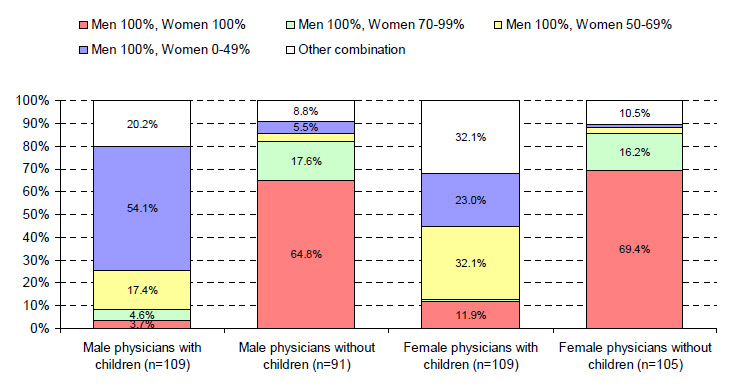
Couples’ arrangements regarding employment status by gender and parenthood status.
DOI: https://doi.org/10.4414/smw.2011.13179
Interest in how both partners in a couple coordinate their careers and private lives has been increasing over the past few years [1, 2]. This growing interest can be explained by the fact that more and more women – and especially women with children – are pursuing careers in their own right. Due to the expansion in tertiary education, the number of highly qualified women as well as the number of couples in which both partners hold an academic degree has increased considerably [3]. In cases where both partners are working, they can be referred to as dual-earner couples or dual-career couples [4]. In the case of dual-career couples, both partners are highly educated, focus strongly on their careers when planning for the future, and pursue their own individual careers [2]. Dual-earner and dual-career couples are faced with high professional and private demands and must coordinate their careers, relationships and family goals. According to the theoretical framework posited by Rusconi and Solga [5], two kinds of external factors affect how couples negotiate and coordinate their careers: (1) career opportunities for women and men independent of the relationship; and (2) external factors relating to the relationship, such as childcare options.
In physicians’ lives, their profession generally plays a central role. Very few physicians consider working in their profession not for any length of time [6]. Consequently, both male and female physicians must find a way to coordinate their own careers with those of their partners, as well as with their personal goals such as having a family. From society’s point of view, it is desirable for physicians to exercise their professions to a large extent in order to ensure healthcare provision for the population and so as not to waste the investment made in their education. As an increasing number of women train as physicians, the career arrangements of female physicians are of particular interest. Previous research on academic couples shows that women are likely to scale back their careers, at least temporarily, after having a baby [3, 6, 7]. Female physicians consider the issues of combining a career and family both when planning their careers and after having children: they concentrate on a few specialties regarded as family-friendly, hesitate to go into an academic career or to aspire to have a senior position in hospital medicine, and work shorter hours [6, 8–11]. Female physicians are more likely than their male counterparts to live in a dual-physician relationship [6, 12, 13]. This couple type seems to be favourable for women physicians: reports on dual-doctor couples indicate that they give both careers equal priority, that both partners tend to reduce their working hours, and that the careers of female physicians seem to benefit more than those of women married to non-physician spouses [13, 14].
The aim of this study was to analyse several issues regarding career arrangements in a cohort of Swiss physicians and their partners. The first question of the study addressed the occupational situation of male and female physicians with and without children, eight years after graduation. We assumed that parenthood slows down career advancement in female physicians, but not in their male colleagues [11, 15–17]. The second question addressed the age, educational level and employment status of the physicians’ partners. Based on previous studies [2, 12], we expected more female physicians than male physicians to have a partner with an academic degree. The third question of the study focused on career arrangements within the couples. As reported by Schiebinger [18], priority is more often given to the career of the male partner, even if both partners have the same educational status. We therefore hypothesised that male physicians most often consider their own career to be of prime importance, while female physicians most often consider either both careers to be of equal importance, or consider their partner’s career to have priority. The last study question addressed the situation of dual-physician couples vis-à-vis physician/academic and physician/non-academic couples. Based on reports of other studies [13, 14], our hypothesis was that female and male physicians in dual-physician couples or physician/academic couples more often rate both careers as equal than female and male physicians with non-physician or non-academic partners.
This study is part of an ongoing prospective survey (SwissMedCareer Study) of a cohort of graduates of the three medical schools in German-speaking Switzerland (Basel, Bern, and Zurich) begun in 2001 [6]. A total of 71% (n = 711) of all registered final-year students (n = 1004) participated in the first assessment. The participants were surveyed six times. This paper focuses on the results of the sixth assessment conducted in 2010, eight years after graduation. A total of 703 subjects were addressed by mail-out questionnaires; 526 questionnaires were returned (response rate: 74.8%) [12]. To ensure participants’ anonymity, the collected questionnaires were identified only by a code. Respondents sent their addresses to an independent address-administration office, which allowed for a follow-up. The study was approved by the Ethical Committee of Zurich University.
The sample of this study comprised of 414 physicians living in a stable partnership (214 females, 51.7%; 200 males, 48.3%) and participating at T6 with a full data set. Excluded were 24 physicians living in a same-sex partnership, due to their potentially different career and family arrangements. The mean age of the physicians was 36.1 years (SD 2.2 years, range 32–50 years). A total of 264 physicians (63.8%) were married, and 109 (50.9%) of the females and 109 (54.5%) of the males had children. The mean age of the female physicians’ first born children was 3.3 years (range 0–14 years) and the mean age of the male physicians’ first born children was 3.7 years (range 0–14 years).
This study investigated the occupational and personal situation of the participants by assessing the socio-demographic data, occupational position (residency physician in a hospital, senior physician in a hospital, physician in private practice, other position), and employment status (percent of full-time employment broken down into the four categories 0–49%, 50–69%, 70–99%, 100%) of the physicians. The socio-demographic data, educational level and employment status of the physicians’ partners were also assessed. Career priority was assessed with the question “In your relationship, whose career is considered of primary importance?” (possible answers: My own career; Both careers are equally important; My partner’s career), as well as with the question “In your relationship, did either of you cut back on your career?” (possible answers: No, yes; if yes: Me, Both, My partner).
All analyses were carried out with SPSS for Windows, release 15. Descriptive statistics are given in terms of means and standard deviations on the one hand, and counts and percentages on the other. Differences between groups in categorical variables such as occupational position and employment status were analysed with Chi-square tests. p-values lower than 0.05% were deemed to be significant.
Eight years after graduation, both male and female physicians worked most frequently as resident or senior physicians in a hospital (table 1). Their positions differed significantly depending on parenthood status. Male and female physicians with children were less likely to hold the position of senior physician in a hospital, and worked in a private practice more often than physicians without children. With regard to their position in private practice, female physicians were more often employees and less often owners or co-owners of the practice, while male physicians were employees or owners approximately equally often. The category ‘other position’ comprised of postdoctoral fellowship, senior staff, medical management, telemedicine, medical field outside hospital, dental medicine and temporary career break. More females with children than without were found in the ‘other occupational position’ category.
The employment status of male and female physicians differed significantly according to whether or not they had children (table 2). Male physicians with children did not work full-time as often as male physicians without children. With female physicians, the difference in employment depending on parenthood status was even more pronounced, with just 18.3% of female physicians with children working full-time compared to 74.3% of female physicians without children.
In terms of position and degree of employment with regard to parenthood status, male physicians without children most often worked full-time as residents (41.8%) or as senior physicians (40.7%); of the physician-fathers, two thirds were full-time residents (37.6%) or full-time senior physicians (30.3%). With regards to female physicians without children, three quarters worked as full-time residents (40.0%) or as full-time senior physicians (31.4%). The group of physician-mothers showed a wide variety of degree of employment and position: among the residents, only 12.8% of them worked full-time and 22.9% were employed between 50 and 69%; 11.9% of the physician-mothers occupied a senior chief position with an employment level of 50–69%; of physician-mothers in private practice, another 11.9% worked between 50–69%. These data showed that the majority of physician-fathers continued to work full-time in a hospital position. The preferred occupational situation of physician-mothers was a position in a hospital or in private practice with a degree of employment of 50 to 69%.
With regard to specialty training and parenthood, 126 male physicians (63.0%), irrespective of parenthood status, had received their board qualification; of the female physicians without children, 72 (68.6%) had completed their specialty training, while just 57 physician-mothers (52.3%) had been awarded their specialty title (p ≤0.05).
A career breakwas reported by one third of the female physicians and by 11.5% of the male physicians. Physician-mothers took career breaks significantly more often than females without children (p ≤0.001); in the male physician group there was no significant difference in career breaks with respect to parenthood.
| Table 1: Occupational position of male and female physicians with and without children (N = 414). | ||||||||
| Male physicians | Female physicians | |||||||
| Position | With children(n = 109) | Without children (n = 91) | Total (n = 200) | With children (n = 109) | Without children (n = 105) | Total (n = 214) | ||
| Resident physician in a hospital | 42.2% | 44.0% | 43.0% | p ≤0.05 | 45.9% | 43.8% | 44.9% | p ≤0.001 |
| Senior physician in a hospital | 36.7% | 47.3% | 41.5% | 23.9% | 44.8% | 43.1% | ||
| Physician in private practice | 16.5% | 3.3% | 10.5% | 20.2% | 9.5% | 15.0% | ||
| Other position | 4.6% | 5.5% | 5.0% | 10.1% | 1.9% | 6.1% | ||
| Total | 100.0% | 100.0% | 100.0% | 100.0% | 100.0% | 100.0% | ||
| Table 2: Employment status of male and female physicians with and without children (N = 414). | ||||||||
| Employment | Male physicians | Female physicians | ||||||
| With children (n = 109) | Without children (n = 91) | Total (n = 200) | With children (n = 109) | Without children (n = 105) | Total (n = 214) | |||
| 0–49% | 1.8% | 3.3% | 2.5% | p ≤0.05 | 28.4% | 1.9% | 15.4% | p ≤0.001 |
| 50–69% | 8.3% | 1.1% | 5.0% | 48.6% | 3.8% | 26.6% | ||
| 70–99% | 10.1% | 4.4% | 7.5% | 4.6% | 20.0% | 12.1% | ||
| 100% | 79.8% | 91.2% | 85.0% | 18.3% | 74.3% | 45.8% | ||
| Total | 100.0% | 100.0% | 100.0% | 100.0% | 100.0% | 100.0% | ||
The male physicians’ partners were on average 33.8 years old (SD = 3.7 years, range: 24–46 years); the female physicians’ partners were about five years older, with an average age of 38.5 years (SD = 4.7 years, range: 30–55 years; p ≤0.001). The length of the relationship was 8.1 years on average (SD 4.7 years, range: 0–23 years) and did not differ significantly according to gender. Female physicians were more likely than male physicians to have a physician partner (n = 87, 40.7% versus n = 60, 30.0% respectively) or a partner with another academic degree (n = 86, 40.2% versus n = 70, 35.0% respectively). Male physicians were more likely than female physicians to have a partner without an academic degree (n = 70, 35.0% versus n = 41, 19.2% respectively).
The most prevalent arrangement in terms of the employment status of male physicians with children was that they worked full-time, and their partners were unemployed or worked less than 50% time (fig. 1), while the most common arrangement for male physicians without children was that both partners worked full-time. For female physicians with children, the most frequent arrangement was that they worked 50–69% and their partners worked full-time, while the most common arrangement for female physicians without children was that of both partners working full-time.
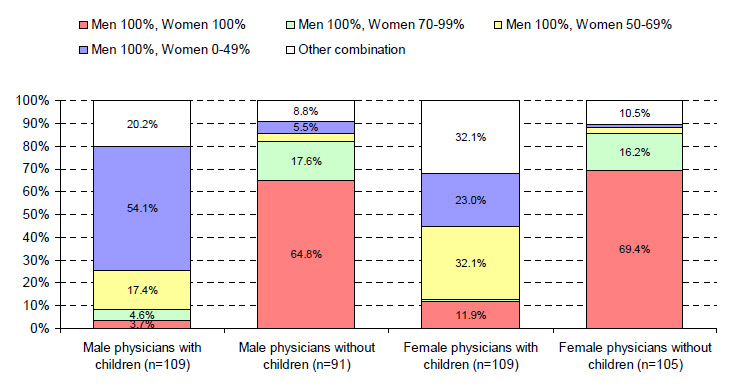
Figure 1
Couples’ arrangements regarding employment status by gender and parenthood status.
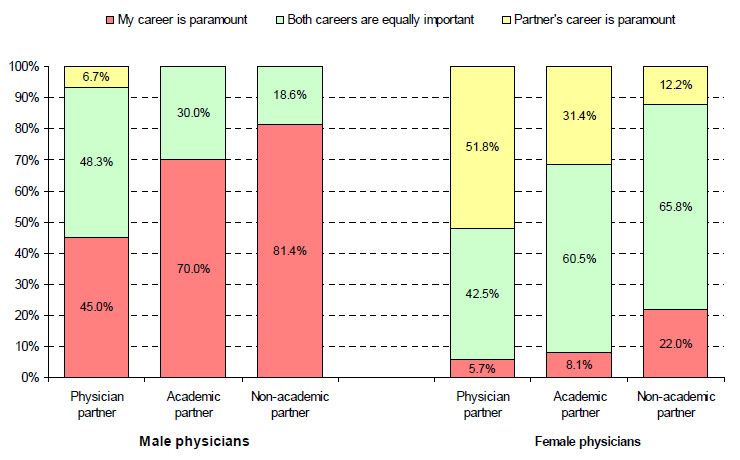
Figure 2
Career priority by gender and partner type.
Male and female physicians differed significantly with respect to the assessment of career priority within the couple (p ≤0.001). Male physicians more frequently considered their own career to be more important (n = 133, 66.5%), or both careers to be equally important (n = 63, 31.5%), while female physicians more frequently considered both careers to be equally important (n = 116, 54.2%) or their partner’s career to be more important (n = 77, 36.0%). Comparing couples with and without children, a trend towards a more traditional career arrangement could be seen in couples with children. Male physicians with children were more likely than those without children to rate their own careers as more important, while female physicians with children were more likely than those without children to rate their partners’ careers as more important.
Male and female physicians also differed significantly with respect to compromising on career (table 3), with fewer male than female physicians reporting that they had compromised on their own careers (1.0% versus 29.4%, respectively).
Dual-physician couples (n = 147, 35.5%), physician/academic couples (n = 156, 37.7%), and physician/non-academic couples (n = 111, 26.8%) did not differ significantly with respect to having children, although dual-physician couples tended to have a family less often than physician/academic couples and physician/non-academic couples (47.6%, 53.8% and 57.7%, respectively).
The three types of couples differed in terms of assessment of career priority, however (fig. 2). Male physicians with a physician partner most frequently considered both careers to be of equal importance, while male physicians with an academic partner or non-academic partner most frequently considered their own career to be paramount (p ≤0.001). Female physicians with a physician partner most frequently considered their partners’ careers to be of prime importance, while female physicians with an academic or non-academic partner most frequently considered both careers to be of equal importance (p ≤0.001).
Neither female nor male physicians (with or without children) differed on the basis of type of couple with regard to possession of board certification.
| Table 3: Compromising on career by gender. | ||||
| Have you or your partner compromised on career? | Male physicians (n = 200) | Female physicians (n = 214) | Total (n = 414) | |
| No | 51.0% | 46.3% | 48.6% | p≤0.001 |
| Yes, I have | 1.0% | 29.4% | 15.7% | |
| Yes, both of us have | 12.5% | 18.7% | 15.7% | |
| Yes, my partner has | 35.5% | 5.6% | 20.0% | |
| Total | 100.0% | 100.0% | 100.0% | |
This study investigated the career arrangements of physicians and their partners in a cohort of Swiss physicians. Considering the high response rate of 74.8%, the data provided by the 414 physicians furnish important indications as to the most common career and family arrangements of female and male physicians in the upcoming generation of Swiss physicians.
Although specialist training, as regulated by the Swiss Medical Association, only lasts five to six years [19], over 40% of the study participants were still working as resident physicians eight years after graduation, regardless of parenthood status . Unlike in the USA [20] and most European countries, there is no nationwide residency-matching program in Switzerland and furthermore, many training institutions do not offer structured residency programs [12]. Both of these factors imply a delay in specialist training, which is reported as only being completed after an average of eight years [19].
Postgraduate specialty training falls in the stage of life in which a family is often started. As reported in other studies [5, 6, 8, 10, 21–23] and as also found in the present study, significantly fewer women with than without children hold senior physician posts. Working in a private practice[11], mostly as an employee practitioner [22], seems to offer an attractive alternative for physician-mothers. For male physicians, starting a family does not slow down career progress, although having a family might influence their choice of career; significantly more physician-fathers worked in private practice than male physicians without children. Male physicians were more often the owners or co-owners of their practice than were their female colleagues. Consequently, we must assume that working in private practice enables greater flexibility when it comes to starting a family and coordinating the careers of both spouses. However, running a private practice implies private investment and working at one’s own risk. Women physicians, especially those with children, are presumably more reluctant to take the risk of running their own practice, especially when they only work part-time. They seem to prefer to be an employee practitioner in a private specialist or general practitioner practice at the family stage when they have young children. The same trend is described in the Royal College of Physicians’ report [22].
Looking at the employment status of male and female physicians, both partners usually start their relationship as equals in terms of their careers [24]. Despite this, with most couples, having children goes hand in hand with a tendency to fall back into more traditional gender roles in terms of working arrangements and family responsibilities: the male partner usually continues to work full-time while the female partner cuts back to part-time work and assumes more family responsibilities [5, 25]. Similar data as found in the current study were also reported in the Swiss Labour Force Participation Rate Survey SAKE [26, 27]: One third of mothers with a child of 0–6 years were not employed, one third had an employment status below 50%, a quarter worked 50–89%, and only 12% worked full-time; of the fathers, 90% worked full-time. In our study, the mean age of the children was only 3 to 4 years. With children at this age, physician mothers had taken over more family responsibilities and reduced their employment status. To date we do not know whether they will increase their employment status when their children grow older. Data from the 2009 national statistics indicated that 81% of academically educated mothers with children below the age of fifteen living in a partnership were employed, but there were no data available on the percentage of employment depending on the age of their children [28].
In the current study, the mean length of the partnership was eight years. This indicates that the majority of couples met just before or at the beginning of their postgraduate training. On average, the male physician’s partner was three years younger, while the female physician’s partner was two years older. As also found in other studies, female physicians were more likely than male physicians to have a physician partner or a partner with another academic degree, while male physicians were more likely to have a non-academic partner [2, 13, 29]. What implications do these two factors have for the career arrangements of the spouses? Firstly, significantly more female than male physicians reported having compromised on their careers in favour of their partners’, whether or not they had children. Secondly, before couples started their families, two-thirds of both partners worked full-time. Once they had started a family, however, there was a tendency to fall back into more traditional gender roles in terms of working arrangements and family responsibilities, as also reported in other studies [5, 25]. The physician-father continued to work full-time, while the physician-mother cut back to part-time. Several factors support this traditionalising effect. Being more often older and therefore further ahead in his career, the male partner frequently has a higher income. Furthermore, cutting back his professional involvement would have negative consequences for his career. The working world does not yet concede the same rights to men in terms of part-time work opportunities when they are ready to take on family responsibilities [12, 30, 31]. Inflexible working conditions and a shortage of adequate childcare services, as well as internalised gender-role ideology, might be further reasons that a model of equality vis-à-vis career and family arrangements is not yet widespread, even for academic couples [32].
Whereas 40% of the women physicians live in a dual-doctor relationship and the same percentage have a partner with another academic degree, only about 30% of the men have a physician partner, and 30% a partner with another academic qualification. As also reported in other studies [2], women more frequently choose a partner who is educated to the same level, as well as one of the same age or older. Although most of the women physicians wish to pursue their careers and to remain in the medical workforce after having started a family [6], many nonetheless admitted that their partner’s career takes precedence over theirs [5, 25]. Surprisingly, they prioritised their partner’s career to an even greater extent when he is a physician, and these findings are also reported in other surveys [29, 33, 34]. However, there has been another study which emphasised that female physicians seem to benefit in dual-doctor partnerships in terms of early specialty qualification and in terms of a higher percentage of full-time work [14]. From the male physicians’ perspective, they were expected to prioritise their own careers [2, 24, 35]. The results of our and another study show that this applies in particular to male physicians with a non-physician academic partner or a non-academic partner [33]. In dual-doctor couples, however, almost half of the male physicians rated their partner’s career as having equal priority. Similar findings have been reported in several previous studies [13, 14].
As seen in the current study and reported by other authors, a further phenomenon currently exerts considerable influence on medicine as a profession. Among the younger generation of physicians, the priority given to work and career is decreasing [11, 36]. Increasingly, men as well as women are matching their choice of specialty and their career preferences to a controllable lifestyle that allows a good work-life balance, which is apparently not guaranteed in surgical specialties [37–41]. Presumably, a model of mutuality in career arrangements, which allows the balancing of career and family and equal career chances for both partners, will gain increasing acceptance and currency among the younger generation of medical school graduates.
The priority given by couples to the man’s career reflects traditional gender-role attitudes in male and female physicians. This has also been found in general population statistics [26–28]. Together with a shortage of childcare facilities and a lack of flexible part time jobs for physicians of both sexes [11, 42], these attitudes would appear to contribute to the considerable reduction in the working hours of female physicians with children, while the careers of male physicians are only marginally influenced by parenthood.
A further factor has an impact on the medical workforce. In the past two decades, the majority of new medical graduates in Switzerland and in most other Western countries were females, while the absolute number of male graduates decreased [43]. This trend seems to continue. In 2009, two thirds of the Swiss medical school entrants were women [44]. New working models in which both partners can coordinate their careers and private lives have to be developed to prevent a shortage of physicians in a number of specialties. Changes have to be made in medical school, in specialty training curricula, in the structural organisation of health care delivery systems, but also in the attitudes of the individual as well as in society to realise not only gender equality in terms of educational opportunities but also in terms of career opportunities and private life arrangements.
MS and BBF are principal investigators and designed the study. MS conducted the statistical analyses. Both authors were involved in interpreting the data and in drafting the manuscript. Both authors read and approved the final manuscript.
We thank Dr. iur. Catherine Gasser and lic. phil. Maria Hodel, Swiss Office of Public Health, for their important input in determining the study issues.
Funding: This study was supported by grants from the Swiss National Science Foundation (NF Nos. 3200-061906.00, 3200 BO-102130, 3200 BO-113836) and the Swiss Federal Office of Public Health. No other potential conflict of interest relevant to this article was reported.
1 Gramespacher E, Funk J, Rothäusler I. Dual Career Couples an Hochschulen – wissenschaftliche Grundlagen, praktische Erfahrungen und politische Rahmungen. In Dual Career Couples an Hochschulen. Ed. Gramespacher E, Funk J, Rothäusler I. Opladen: Barbara Budrich; 2010;13–8.
2 Solga H, Wimbauer C. «Wenn zwei das Gleiche tun ...» – Ideal und Realität sozialer (Un-) Gleichheit in Dual Career Couples. Eine Einleitung. In: «Wenn zwei das Gleiche tun» – Ideal und Realität sozialer (Un-)Gleichheit in Dual Career Couples. Eds. Solga H, Wimbauer C. Opladen: Barbara Budrich; 2005;9–25.
3 Rusconi A, Solga H. Determinants of and obstacles to dual careers in Germany. Zeitschrift für Familienforschung. 2007;19(3):311–36.
4 Niessen C, Sonnentag S, Neff A, Unger D. Ressourcen und Belastungen von Doppelkarrierepaaren in der Wssenschaft – eine arbeitspsychologische Perspektive. In: Dual Career Couples an Hochschulen. Eds. Gramespacher E, Funk J, Rothäusler I. Opladen: Barbara Budrich; 2010;75–88.
5 Rusconi A, Solga H. Doppelkarrieren – eine wichtige Bedingung für die Verbesserung der Karrierechancen von Frauen. In: Dual Career Couples an Hochschulen. Eds Gramespacher E, Funk J, Rothäusler I. Opladen: Barbara Budrich; 2010;37–55.
6 Buddeberg-Fischer B, Stamm M, Buddeberg C, Bauer G, Hämmig O, Knecht M, et al. The impact of gender and parenthood on physicians’ careers – professional and personal situation seven years after graduation. BMC Health Serv Res. 2010;10(40).
7 Abele AE. Doppelkarrierepaare – Entstehung und Relevanz der Thematik. In: Dual Career Couples an Hochschuolen. Eds. Gramespacher E, Funk J, Rothäusler I. Opladen: Barbara Budrich; 2010;21–35.
8 Barnett RC, Gareis KC, Carr PL. Career satisfaction and retention of women physicians who work reduced hours. J Womens Health. (Larchmt) 2005;14(2):146–53.
9 McMurray J, Cohen M, Angus G, Harding J, Gavel P, Horvath J, et al. Women in medicine: a four-nation comparison. J Am Med Womens Assoc. 2002;57(4):185–90.
10 Carr PL, Gareis KC, Barnett RC. Characteristics and outcomes for women physicians who work reduced hours. J Womens Health. (Larchmt) 2003;12(4):399–405.
11 Heiligers PJM, Hingstman L. Career preferences and the work-family balance in medicine: gender differences among medical specialists. Soc Sci Med. 2000;50:1235–46.
12 Buddeberg-Fischer B, Stamm M. Medical profession and young physicians’ lifestyles in flux: challenges for specialty training and health care delivery systems. Swiss Med Wkly. 2010;140:w13134.
13 French F, Andrew J, Awramenko M, Coutts H, Leighton-Beck L, Mollison J, et al. Why do work patterns differ between men and women GPs? J Health Organ Manag. 2006;20(2–3):163–72.
14 Gjerberg E. Dual-doctor marriages. Tidsskr Nor Laegeforen. 2003;123(16):2300–3.
15 Bowles A, Kevorkian C, Rintala D. Gender differences regarding career issues and promotion in academic physical medicine and rehabilitation. Am J Phys Med Rehabil. 2007;86:918–25.
16 Allen I. Women doctors and their careers: what now? BMJ. 2005;331(Sept 10):369–72.
17 Hohner H-U, Grote S, Hoff E-H. Geschlechtsspezifische Berufsverläufe. Unterschiede auf dem Weg nach oben. Dtsch Ärztebl. 2003;100(4):A 166–9.
18 Schiebinger L. Dual career academic couples: University strategies, opportunities, policies. In: Dual Career Couples an Hochschulen. Eds. Gramespacher E, Funk J, Rothäusler I. Opladen: Barbara Budrich; 2010;113–26.
19 Swiss Medical Association. Weiterbildungsordnung. Bern: Swiss Medical Association; 2009.
20 National Resident Matching Program. National Resident Matching Program. Results and data: 2008 Match. Washington, DC: National Resident Matching Program; 2008.
21 Abele AE. Erwerbsverläufe von Frauen und Männern in der Medizin. In: Arbeitsbedingungen und Befinden von Ärztinnen und Ärzten. Befunde und Interventionen. Vol 2. Eds. Schwartz FW, Angerer P. Köln: Deutscher Ärzteverlag; 2010;149–58.
22 Elston MA. Women and medicine. The future. London: The Royal College of physicians; 2009.
23 Boulis AK, Jacobs JA. The changing face of medicine: Women doctors and the evolution of health care in America. Ithaca: Cornell University Press; 2008.
24 Levy R, Ernst M. Lebenslauf und Regulation in Paarbeziehungen: Bestimmungen der Ungleichheit familialer Arbeitsteilung. Zeitschrift für Familienforschung. 2002;14(2):103–31.
25 Schulz F, Blossfeld HP. Wie verändert sich die häusliche Arbeitsteilung im Eheverlauf. Eine Längsschnittstudie der ersten 14 Ehejahre in Westdeutschland. Kölner Zeitschrift für Soziologie und Sozialpsychologie. 2006;58(2):23–49.
26 Erwerbsmodelle in Paarhaushalten mit und ohne Kinder [http://www.bfs.admin.ch/bfs/portal/de/index/themen/20/05/blank/key/Vereinbarkeit/03.html]
27 Erwerbssituation von Müttern und Vätern nach Alter des jüngsten Kindes [http://www.bfs.admin.ch/bfs/portal/de/index/themen/20/05/blank/key/Vereinbarkeit/01.html]
28 Erwerbsquote von Müttern (25–54 Jahre) mit Partner und mindestens einem unter 15-jährigen Kind nach Bildungsstand, 1996–2009 [http://www.bfs.admin.ch/bfs/portal/de/index/themen/01/04/blank/01/04/01.html]
29 Hansen MN. Social status and marriage within the medical profession. Tidsskr Nor Laegeforen. 2002;122(19):1881–4.
30 Behnke C, Meuser M. Vereinbarkeitsmanagement. Die Herstellung von Gemeinschaft bei Doppelkarrierepaaren. Soziale Welt: Zeitschrift für sozialwissenschaftliche Forschung und Praxis. 2003;54(2):163–74.
31 Dettmer S, Hoff EH. Berufs- und Karrierekonstellationen in Paarbeziehungen: Segmentation, Integration, Entgrenzung. In: «Wenn zwei das Gleiche tun» Ideal und Realität sozialer (Un)Gleichheit in Dual Career Couples. Eds. Solga H, Wimbauer C. Opladen: Barbara Budrich; 2005:53–75.
32 McGuire LK, Bergen MR, Polan ML. Career advancement for women faculty in a U.S. school of medicine: perceived needs. Acad Med. 2004;79(4):319–25.
33 Dyrbye LN, Shanafelt TD, Balch CM, Satele D, Freischlag J. Physicians married or partnered to physicians: A comparative study in the American College of Surgeons. J Am Coll Surg. 2010;211:663–71.
34 Schrager S, Kolan A, Dottl S. Is that your pager or mine: a surevy of women academic family physicians in dual physician families. WMJ. 2007;106(5):251–5.
35 Hoff EH, Grote S, Dettmer S, Hohner HU, Olos L. Work-Life-Balance: Berufliche und private Lebensgestaltung von Frauen und Männern in hoch qualifizierten Berufen. Z Arbeits- Organisationspsychol. 2005;49(4):196–207.
36 Sanfey HA, Saalwachter-Schulman AR, Nyhof-Young JM, Eidelson B, Mann BD. Influences on medical student career choice. Gender or generation? Arch Surg. 2006;141:1086–94.
37 Wendel TM, Godellas CV, Prinz RA. Are there gender differences in choosing a surgical career? Surgery. 2003;134(4):591–6.
38 Lambert EM, Holmboe ES. The relationship between specialty choice and gender of U.S. medical students, 1990–2003. Acad Med. 2005;80(9):797–802.
39 Dorsey ER, Jarjoura D, Rutecki GW. Influence of controllable lifestyle on recent trends in specialty choice by US medical students. JAMA. 2003;290(9):1173–8.
40 Gargiulo DA, Hyman NH, Hebert JC. Women in surgery: do we really understand the deterrents. Arch Surg. 2006;141(4):405–7.
41 McCord JH, McDonald R, Leverson G, Mahvi DM, Rikkers LF, Chen HC, Weber SM. Motivation to pursue surgical subspecialty training: Is there a gender difference? J Am Coll Surg. 2007;205:698–703.
42 Fuss I, Nübling M, Hasselhorn H, Schwappbach D, Rieger M. Working conditions and work-family conflict in German hospital physicians: psychosocial and organisational predictors and consequences. BMC Public Health. 2008; 8(353).
43 Universitäte Abschlüsse nach Geschlecht und Fachbereich [http://www.bfs.admin.ch/bfs/portal/de/index/themen/15/06/key/ind1.indicator.10401.104.html]
44 Eintritte ins Medizinstudium [http://www.bfs.admin.ch/bfs/portal/de/index/theen/15/06/key/ind1.indicator.10202.102.html?open=106#106]