Medical treatment of hypertension in Switzerland
DOI: https://doi.org/10.4414/smw.2011.13169
Summary
OBJECTIVES: Despite a broad and efficient pharmacological antihypertensive armamentarium, blood pressure (BP) control is suboptimal and heterogeneous throughout Europe. Recent representative data from Switzerland are limited. The goal of the present survey was therefore to assess the actual control rate of high BP in Switzerland in accordance with current guidelines. The influence of risk factors, target organ damage and medication on BP levels and control was also evaluated.
METHODS: A cross-sectional visit-based survey of ambulatory hypertensive patients was performed in 2009 in Switzerland. 281 randomly selected physicians provided data on 5 consecutive hypertensive patients attending their practices for BP follow-up. Data were anonymously collected on demographics, comorbidities and current medication, and BP was recorded. Subsequent modification of pharmacological antihypertensive therapy was assessed.
RESULTS: Data from 1376 patients were available. Mean age was 65 ± 12 years, 53.9% were male subjects. 26.4% had complicated hypertension. Overall, BP control (<140/90 mm Hg for uncomplicated and <130/80 mm Hg for complicated hypertension) was achieved in 48.9%. Compared to patients with complicated hypertension, BP control was better in patients with uncomplicated hypertension (59.4% vs. 19.2%, p <0.001). As a monotherapy the most prescribed drug class were angiotensin receptor blockers (ARB, 41%), followed by angiotensin converting enzyme (ACE) inhibitors (21.5%), betablockers (20.8%) and calcium channel blockers (CCB, 10.8%). The most prescribed drug combinations were ARB + diuretic (30.1%) and ACE inhibitors + diuretic (15.3%). 46% were receiving a fixed drug combination. In only 32.7% of patients with uncontrolled hypertension was a change in drug therapy made.
CONCLUSION: This representative survey on treated adult hypertensive patients shows that, compared to earlier reports, the control rate of hypertension has improved in Switzerland for uncomplicated but not for complicated, particularly diabetes-associated hypertension. ARBs and ACE inhibitors are the most prescribed antihypertensive drugs for monotherapy, whereas diuretics and ARBs were the most used for combination therapy.
The 2009 Swiss Hypertension Survey (SWISSHYPE)
Introduction
Control of arterial hypertension in Europe [1–3] and the United States [4] is far from optimal even though the armamentarium of hypertension treatment has been substantially broadened over the last 30 years. In a survey performed in 2004 in different Western European countries as well as in the United States, after the publication of the hypertension guidelines promoting BP goals <140/90 mm Hg [5], the BP normalisation rate was 31% in Italy, 26% in the United Kingdom, 40% in Germany and in Spain, 46% in France and 63% in the United States. This, as well as other studies, revealed a substantial heterogeneity in the pharmacological treatment of elevated BP between Europe and North America [1–3, 6, 7]. In the cross-sectional EUROASPIRE III trial evaluating coronary heart disease in patients <70 in 8 European countries, 60.9% of the patients had uncontrolled BP [8], and comparison with the previous EUROASPIRE I and II showed an unchanged BP control rate (58.1% and 58.3% respectively). In Switzerland, the last available data on BP control in hypertensive patients are almost 10 years old and refer to a cut-off value for controlled hypertension based on the individual judgment of the attending physician [9]. The objective of this survey was therefore to evaluate current BP control rates in adult hypertensive individuals in Switzerland and to compare them with earlier reports. The influence of cardiovascular risk factors, target organ damage and antihypertensive medication on BP levels and hypertension control was also evaluated.
Methods
Data collection
Data was collected in 2009 in Switzerland by performing a cross-sectional survey of ambulatory patients visiting their physicians. The randomisation of the participating physicians was as follows: Switzerland was geographically divided into 8 regions including 5 German-speaking, 2 French-speaking and 1 Italian-speaking region. For each region, physicians were recruited randomly among general practitioners, internists and cardiologists until the number of 38 (34 for the Italian-speaking region) was reached. The participating physicians were asked to give information on the next five treated hypertensive patients aged >20 years attending their office. The inclusion criteria stated that patients had to be hypertensive and were specially treated for this condition for at least 3 months. Diagnosis relied on the judgment of the attending physician and treatment had not necessarily to be pharmaceutical, lifestyle only being an acceptable alternative.
Information on demographic characteristics, history of hypertension, current antihypertensive medication, presence of target organ damage and cardiovascular risk factors was collected by standardised questionnaire. In agreement with previous studies [5], antihypertensive medication was classified as follows: angiotensin receptor blockers (ARB), calcium channel blockers (CCB), betablockers, angiotensin converting enzyme (ACE) inhibitors, diuretics and other antihypertensive drugs.
Blood pressure measurement
In accordance with the guidelines [10], three consecutive oscillometric BP readings at 1 min intervals were performed in the seated position after a prior resting period of at least 5 min. A BP measurement was also performed after 2 min in the upright position. The physicians used their own BP measuring devices and appropriate cuff dimensions were chosen according to the upper-arm circumference. For statistical analysis the last two measured sitting BP values were used.
The anonymous case report forms were collected by an independent data management office (Five Office ltd, Zurich, Switzerland). All patients gave written informed consent. The study was approved by regional ethical committees throughout Switzerland.
Outcome measures
We analysed the BP data on the basis of three groups according to the classification system of the 2007 ESH-ESC guidelines [11]: BP <140 mm Hg, between 140 and 159 mm Hg and ≥160 mm Hg for systolic values and <90 mm Hg, between 90 and 99 mm Hg and ≥100 mm Hg for diastolic values. Hypertension control was defined as systolic blood pressure (SBP) <140 mm Hg and diastolic blood pressure (DBP) <90 mm Hg in patients with uncomplicated hypertension and <130 mm Hg and <80 mm Hg in patients with diabetes, chronic kidney disease (CKD) or proteinuria. The influence of demographic factors, cardiovascular risk factors, comorbidities and pharmacotherapy on BP levels and control was analysed. The effect of fixed combination pharmacotherapy on BP control was also assessed.
Definition of comorbidities
The participating physicians were asked to report their patients’ cardiovascular comorbidities. Since no clear-cut definition criteria of these comorbidities were applied, interpretation and reporting of high-risk conditions such as previous myocardial infarction or stroke, left ventricular hypertrophy, CKD, proteinuria and microalbuminuria were at the discretion of the physician involved. Diabetes mellitus was considered present if an antidiabetic therapy was prescribed.
Statistical analyses
The Chi-squared test was used to compare relative frequencies and Student’s t-test to compare mean values of two groups. One-way ANOVA was used to compare the mean difference between several groups. To indentify independent predictors of uncontrolled BP we performed a multivariate logistic regression analysis with inclusion of univariate predictors (p <0.1) in the model by the forced entry method. The analysis was performed using SAS/STAT Software (SAS Institute Inc, Version 9.1).
Results
Patient characteristics
281 randomly selected physicians participated in this study, 181 general practitioners, 91 internists and 9 cardiologists. A total of 1376 hypertensive patients were analysed. The majority of patients included were recruited by general practitioners (68%); 30% were recruited by internists and 2% by cardiologists.
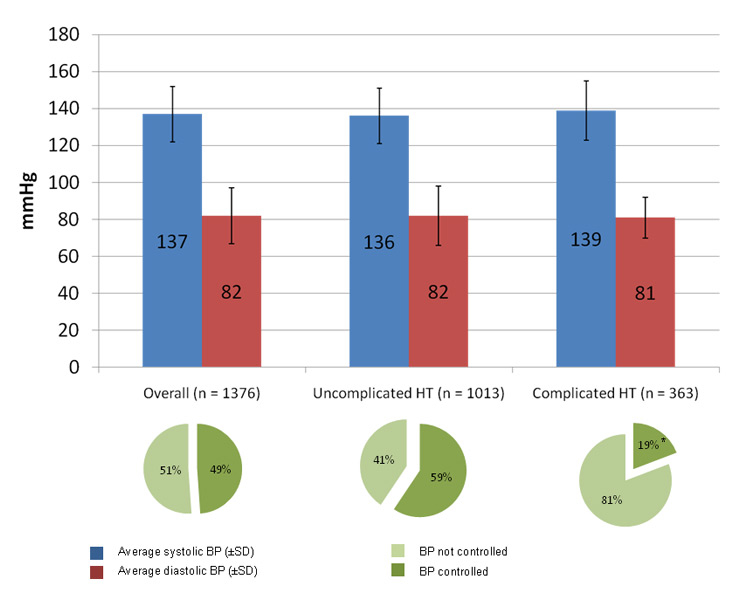
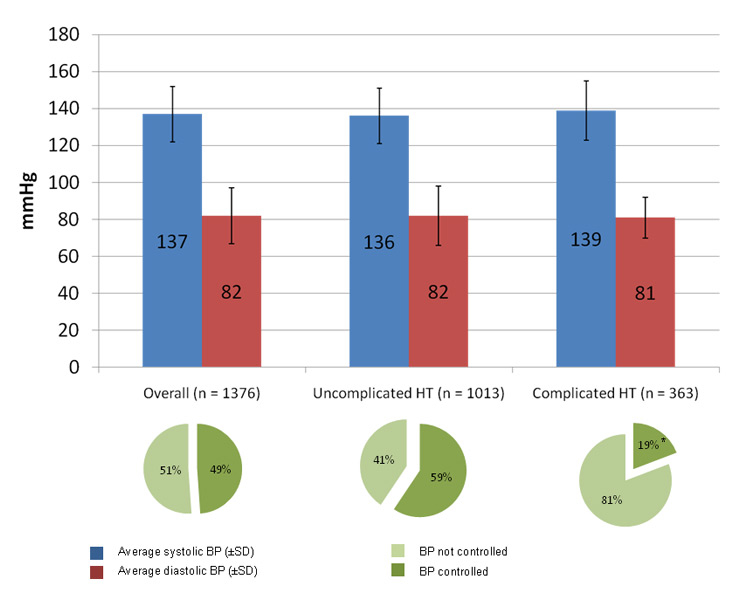
Figure 1
Average systolic and diastolic blood pressure values in the different subgroups of treated hypertensive patients (bar graph). The diagram under the bar graph shows the rate of controlled hypertension according to the individual blood pressure target in the different subgroups. HT: hypertension. BP: blood pressure. SD: standard deviation. * p <0.001, complicated vs uncomplicated hypertension.
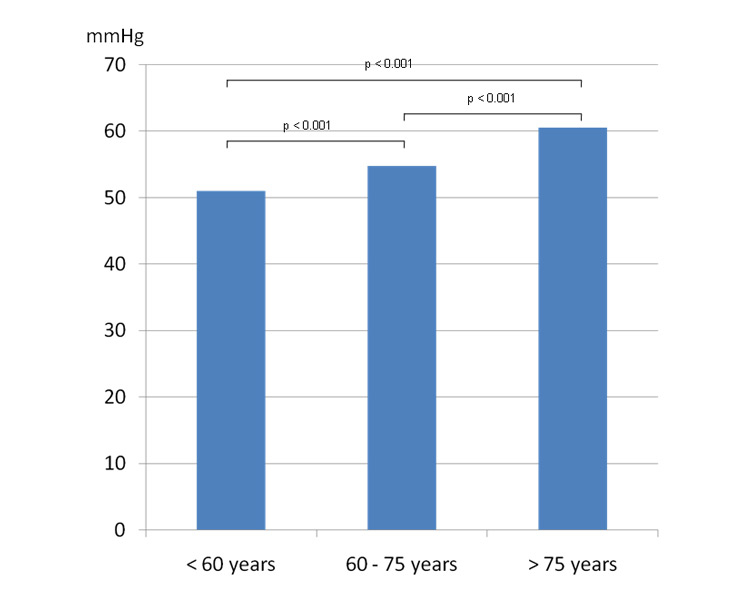
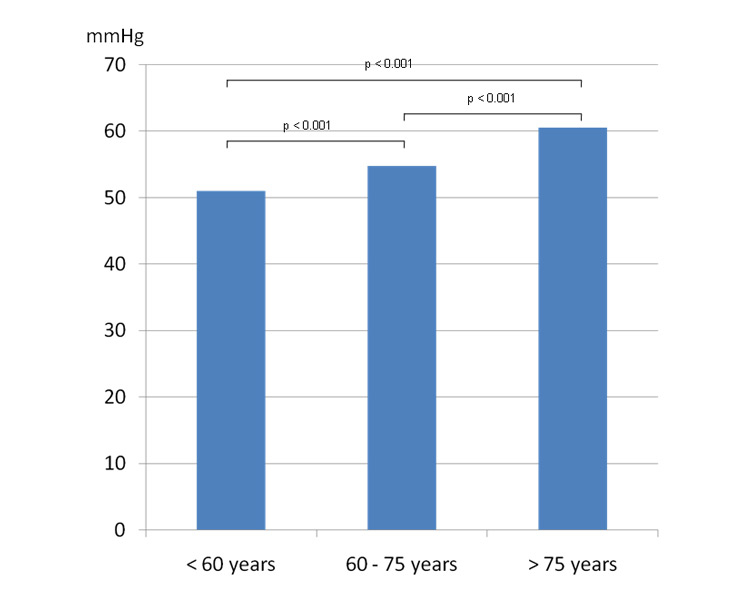
Figure 2
Pulse pressure by different age groups in treated hypertensive patients.
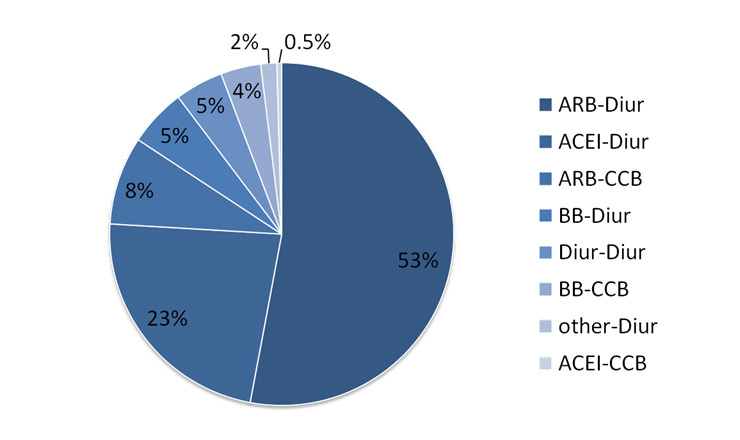
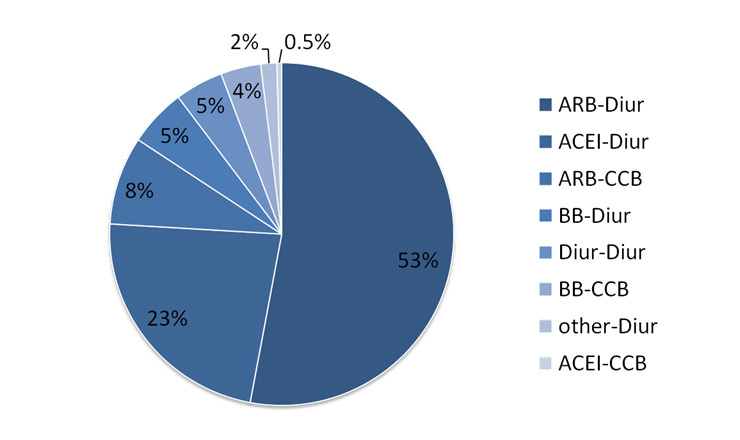
Figure 3
Composition of the different fixed combination therapies used in the study population. ACEI: angiotensin converting enzyme inhibitor; CCB: calcium channel blocker; ARB: angiotensin receptor blocker; Diur: diuretic; BB: betablocker; other: other antihypertensive therapy.
Patient characteristics stratified according to systolic and diastolic BP values are presented in tables 1 – 4. 74% of the patients were overweight (body mass index [BMI] ≥25 kg/m2), and mean BMI was 28.8 ± 5.2 kg/m2.
73.4% of the patients included had uncomplicated hypertension, while 26.4% had hypertension associated with diabetes mellitus, CKD and / or proteinuria. Among the patients with complicated hypertension, 83.4% had diabetes mellitus, 24.7% proteinuria and 14.2% CKD. Compared to patients with uncomplicated hypertension, patients with complicated hypertension had more often left ventricular hypertrophy (13.9% vs. 7.7%, p = 0.001), coronary revascularisation (17.5% vs. 9.2%, p <0.001), previous myocardial infarction (13.6% vs. 7.6%, p = 0.001), angina pectoris (13.9% vs. 7.7%, p = 0.001), peripheral vascular disease (13.3% vs. 5.3%, p <0.001), cerebrovascular disease (11.3% vs. 7.9%, p = 0.049) and microalbuminuria (40% vs. 7.9%, p <0.001).
Influence of baseline characteristics on blood pressure
Average BP in patients with complicated hypertension was 138.8 ± 15.6 / 81.0 ± 10.0 mm Hg compared to 136.0 ± 15.3 / 82.1 ± 16.3 mm Hg in patients with uncomplicated hypertension (p = 0.003 for SBP, fig. 1). There were significantly more patients with complicated hypertension in the subgroup with SBP levels ≥160 mm Hg compared to the two other subgroups (34.6% vs. 30.2% vs. 22.9%, p = 0.003). 18.2% of the patients with uncomplicated hypertension had SBP ≥140 mm Hg in combination with DBP <90 mm Hg and 6.3% had SBP ≥150 mm Hg and DBP <90 mm Hg. Women were more likely than men to have isolated systolic hypertension (21.7% vs. 15%, p = 0.006). Patients in the subgroup with SBP between 140 mm Hg and 159 mm Hg were older than patients in the group with SBP <140 mm Hg (66.4 ± 11.6 years vs. 64.3 ± 11.8 years, p = 0.005). By contrast, patients with DBP <90 mm Hg were significantly older than patients with DBP 90–99 mm Hg (66.1 ± 11.8 years vs. 61.7 ± 11.6 years, p <0.001) and patients with DBP ≥100 mm Hg (66.1 ± 11.8 years vs. 60.6 ± 10.4 years, p <0.001). Thus, as expected, there was a significant age-dependent pulse pressure increase (fig. 2). Correspondingly, patients with isolated systolic hypertension were older than patients without this condition (68.7 years vs. 64.5 years, p <0.001).
BMI was significantly associated with DBP (p = 0.001) but not SBP. Compared to the subgroups with higher SBP, diabetes (p = 0.026), proteinuria (p = 0.045), microalbuminuria (p = 0.005) and CKD (p = 0.013) were less frequent in the subgroup with SBP <140 mm Hg. Myocardial infarction and coronary revascularisation were more frequent in patients with DBP <90 mm Hg (p = 0.008 and p = 0.004 respectively) compared to subgroups with higher DBP.
Blood pressure control
Overall, 56.9% of the patients had BP measurements <140/90 mm Hg and 19.6% had BP measurements <130/80 mm Hg. Diabetes mellitus (24.9% vs. 19.2%, p = 0.012), microalbuminuria (21.5% vs. 14%, p = 0.002), proteinuria (8.7% vs. 5.3%, p = 0.03) and CKD (5.1% vs. 2.9%, p = 0.04) were more prevalent in patients with a BP ≥140/90 mm Hg than in those with a BP <140/90 mm Hg. Moreover, patients with coronary revascularisation or myocardial infarction had BP ≥140/90 mm Hg (33.1% vs. 44.3%, p = 0.009 and 32% vs. 44.1%, p = 0.01, respectively) less frequently than patients without these conditions.
The proportion of hypertensive patients achieving individual target values as recommended in the current guidelines [10] and according to their low- or high-risk status is shown in figure 1. Hypertension was uncontrolled in 51% of the participants because target SBP was not achieved in 19.5%, target DBP in 6.6% and both target systolic and diastolic BP in 24.9% of patients.
Significantly fewer diabetic patients achieved BP target (<130/80 mm Hg) compared to patients without diabetes mellitus (19% vs. 57%, p <0.001). This proportion increased to 50% if goal BP was set at <140/90 mm Hg but remained statistically inferior to the 57% controlled hypertensive patients without diabetes (p = 0.012). Moreover, diabetes was more prevalent in the subgroup of patients with uncontrolled compared to the subgroup of patients with controlled hypertension (34.1% vs. 8.6%, p <0.001). Similarly, patients with CKD, proteinuria or microalbuminuria reached BP goal significantly less frequently than patients without CKD (20.4% in patients with CKD vs. 50.2% in patients without CKD, p <0.001), proteinuria (16.2% vs. 51.6%, p <0.001) or microalbuminuria (28.7% vs. 53%, p <0.001).
Not surprisingly, patients with a BMI <25 kg/m2 had a significantly higher rate of controlled hypertension than overweight or adipose patients (54% vs. 47%, p = 0.029).
In a multivariate logistic regression analysis with inclusion of BMI, diabetes, microalbuminuria and CKD and/or proteinuria (nephropathy) as univariate predictors (p <0.1), and after adjustment for other variables, only diabetes (OR 5.1, 95% CI 3.7–7.1, p <0.001) and nephropathy (OR 3.3, 95% CI 2.0.–5.5, p <0.001) remained independently predictive of uncontrolled hypertension. The R2 for the model was 0.15.
Medication
Overall, diuretics and ARBs were prescribed with the greatest frequency (diuretics 51.7%, ARBs 51.4%), followed by betablockers (36.2%), ACE-inhibitors (27.3%), CCB (26.7%) and others (4.7%).
Detailed information on antihypertensive treatment according to different BP subgroups is given in tables 5 and 6. Overall, the mean duration of pharmacological antihypertensive therapy was 9 ± 7.3 years. 1.6% of the patients had no current drug therapy, 33.9% were treated with one, 36.8% with two, 20.4% with three and 7.2% with four or more drug classes. As expected, complicated hypertension was associated with the prescription of more drug classes (p <0.001 vs. uncomplicated hypertension).
46.2% of the patients had at least one fixed combination pill and 40.2% were treated by a free combination of drugs. As a monotherapy, ARBs (41.0%) were used preferentially, followed by ACE inhibitors (21.5%), betablockers (20.8%), CCB (10.7%), diuretics (2.8%) and other drugs (2.4%). Monotherapy by betablockers was more likely to be prescribed in patients with prior myocardial infarction or previous coronary revascularisation than in patients without these comorbidities (48% vs. 19.3%, p = 0.001 and 37% vs. 19.9%, p = 0.033 respectively).
A combination ARB + diuretic was taken in 30.1% of all patients, in 25.4% as a fixed combination. Corresponding data for ARB + CCB were 12.7% and 4% respectively, for ACE inhibitor + diuretic 15.3% and 11%, and for ACE inhibitor + CCB 6.5% and 0.2% respectively. Among patients receiving a fixed combination therapy the most prescribed drug association was ARB + diuretic (53%) followed by other combinations (fig. 3).
Among diabetic patients, 58.3% were treated with a diuretic, 50.7% with an ARB and 33.8% with an ACE inhibitor. Compared to patients without diabetes, significantly more patients with this risk factor received either an ARB or an ACE inhibitor (82.1% vs. 76.5%, p = 0.037).
Prescription rates for patients not at goal for systolic BP (isolated systolic hypertension under therapy) were 51.6% for diuretics, 50.0% for ARBs, 38.6% for betablockers, 32.6% for CCBs and 22.3% for ACE inhibitors. These patients were more likely to be treated by a CCB compared to patients without this condition.
BP was controlled in 11.8% of patients receiving no medication, in 53.8% treated by monotherapy, in 47.0% receiving a fixed combination and in 47.3% treated by a free combination therapy.
Modification of antihypertensive drug regimen
As a result of the BP values measured at the study visit, current antihypertensive drug therapy was changed in 18.2% of patients either by switching to a different drug or by changing the existing dosage. Not surprisingly, treatment adaptations were carried out more frequently in patients with uncontrolled compared to those with controlled BP (32.7% vs. 6.4%, p <0.001). In 67.3% of patients in whom BP was not controlled, no change in therapy was made.
|
Table 1: Patient characteristics by systolic blood pressure subgroups. |
| |
Overall |
SBP <140 |
SBP 140 – 159 |
SBP ≥160 |
p-value |
| Frequency (%) |
100.0 |
62.3 |
29.6 |
8.1 |
|
| Male (%) |
53.9 |
54 |
53.5 |
55.1 |
0.95 |
| Age (years) |
65.1 ± 11.9 |
64.3 ± 11.8 |
66.4 ± 11.6 |
66.1 ± 12.1 |
0.012 |
| Average BP (mm Hg), sitting |
137 ± 15/82 ± 15 |
127 ± 8/78 ± 9 |
147 ± 6/85 ± 9 |
170 ± 10/93 ± 13 |
<0.001 |
| Heart rate (beats per minute) |
72 ± 10 |
72 ± 13 |
72 ± 11 |
74 ± 11 |
0.168 |
| Body mass index (kg/m2) |
28.8 ± 5.2 |
28.7 ± 5.3 |
28.9 ± 5.1 |
29.2 ± 5.3 |
0.594 |
| Family history of premature cardiovascular disease (%) |
27.4 |
27.0 |
28.7 |
26.0 |
0.77 |
| Current smoker |
22.9 |
22.1 |
24.5 |
23.4 |
0.66 |
| Lipid lowering drugs (%) |
45.2 |
45.1 |
45.9 |
43.9 |
0.93 |
| Antidiabetic drugs (%) |
21.6 |
19.4 |
24.2 |
29.0 |
0.026 |
| BP: blood pressure; SBP: systolic blood pressure |
|
Table 2: Patient characteristics by diastolic blood pressure subgroups. |
| |
Overall |
DBP <90 |
DBP 90–99 |
DBP ≥100 |
p-value |
| Frequency (%) |
100.0 |
78.3 |
17.2 |
4.5 |
|
| Male (%) |
53.9 |
51.8 |
58.1 |
72.9 |
0.003 |
| Age (years) |
65.1 ± 11.9 |
66.1 ± 11.8 |
61.7 ± 11.6 |
60.6 ± 10.4 |
<0.001 |
| Average BP (mm Hg), sitting |
137 ± 15/82 ± 15 |
133 ± 13/78 ± 8 |
148 ± 14/93 ± 3 |
161 ± 17/106 ± 7 |
<0.001 |
| Heart rate (beats per minute) |
72 ± 10 |
71 ± 12 |
75 ± 10 |
78 ± 12 |
<0.001 |
| Body mass index (kg/m2) |
28.8 ± 5.2 |
28.5 ± 5.2 |
29.5 ± 5.6 |
30.7 ± 5.1 |
0.001 |
| Family history of premature cardiovascular disease (%) |
27.4 |
27.7 |
27.6 |
22.8 |
0.72 |
| Current smoker |
22.9 |
22.1 |
24.8 |
29.3 |
0.34 |
| Lipid lowering drugs (%) |
45.2 |
47.2 |
40.4 |
28.8 |
0.006 |
| Antidiabetic drugs (%) |
21.6 |
21.2 |
22.7 |
25.4 |
0.69 |
| BP: blood pressure; DBP: diastolic blood pressure |
|
Table 3: Comorbidities by systolic blood pressure subgroups. |
| |
Overall |
SBP <140 |
SBP 140–159 |
SBP ≥160 |
p-value |
| Left ventricular hypertrophy1 (%) |
24.0 |
22.7 |
25.8 |
28.2 |
0.35 |
| Angina pectoris (%) |
9.5 |
9.1 |
11.1 |
6.6 |
0.33 |
| Previous myocardial infarction (%) |
9.3 |
10.4 |
7.7 |
5.7 |
0.13 |
| Coronary revascularisation (%) |
11.5 |
12.8 |
10.5 |
4.7 |
0.039 |
| Peripheral artery disease (%) |
7.4 |
6.9 |
7.7. |
9.3 |
0.64 |
| Cerebrovascular disease (%) |
8.8 |
8.0 |
10.5 |
8.4 |
0.35 |
| Chronic kidney disease (%) |
3.8 |
2.8 |
5.0 |
8.1 |
0.013 |
| Proteinuria (%) |
6.7 |
5.5 |
8.1 |
11.8 |
0.045 |
| Microalbuminuria (%) |
17.1 |
14.1 |
21.9 |
23.7 |
0.005 |
|
1 based on ECG or echocardiography. SBP: systolic blood pressure |
|
Table 4: Comorbidities by diastolic blood pressure subgroups. |
| |
Overall |
DBP <90 |
DBP 90–99 |
DBP ≥100 |
p-value |
| Left ventricular hypertrophy1 (%) |
24.0 |
24.1 |
22.0 |
30.4 |
0.48 |
| Angina pectoris (%) |
9.5 |
10.4 |
7.1 |
3.4 |
0.08 |
| Previous myocardial infarction (%) |
9.3 |
10.6 |
4.4 |
5.1 |
0.008 |
| Coronary revascularisation (%) |
11.5 |
13.0 |
5.8 |
6.8 |
0.004 |
| Peripheral artery disease (%) |
7.4 |
7.7 |
5.7 |
8.5 |
0.57 |
| Cerebrovascular disease (%) |
8.8 |
9.2 |
5.7 |
6.8 |
0.61 |
| Chronic kidney disease (%) |
3.9 |
4.1 |
3.3 |
1.9 |
0.63 |
| Proteinuria (%) |
6.7 |
6.7 |
6.8 |
7.1 |
0.99 |
| Microalbuminuria (%) |
17.1 |
16.1 |
22.2 |
15.4 |
0.17 |
|
1 based on ECG or echocardiography. DBP: diastolic blood pressure |
|
Table 5: Antihypertensive medication by systolic blood pressure subgroups. |
| |
Overall |
SBP <140 |
SBP 140–159 |
SBP ≥160 |
p-value |
| Angiotensin receptor blocker (%) |
51.4 |
51.9 |
49.6 |
52.3 |
0.75 |
| Calcium channel blocker (%) |
26.7 |
26.2 |
27.4 |
30.8 |
0.58 |
| Betablocker (%) |
36.2 |
35.2 |
36.3 |
41.1 |
0.48 |
| Angiotensin converting enzyme inhibitor (%) |
27.3 |
28.5 |
26.3 |
24.3 |
0.54 |
| Diuretic (%) |
51.7 |
50.5 |
52.9 |
57.9 |
0.3 |
| Others (%) |
4.7 |
4.1 |
5.4 |
7.5 |
0.25 |
| Fixed combination (%) |
46.2 |
44.4 |
48.6 |
51.4 |
0.21 |
| SBP: systolic blood pressure |
|
Table 6: Antihypertensive medication by diastolic blood pressure subgroups. |
| |
Overall |
DBP <90 |
DBP 90–99 |
SBP ≥100 |
p-value |
| Angiotensin receptor blocker (%) |
51.4 |
51.1 |
53.3 |
46.6 |
0.63 |
| Calcium channel blocker (%) |
26.7 |
28.3 |
21.1 |
25.9 |
0.09 |
| Betablocker (%) |
36.2 |
37.5 |
29.1 |
37.9 |
0.06 |
| Angiotensin converting enzyme inhibitor (%) |
27.3 |
27.6 |
25.1 |
36.2 |
0.24 |
| Diuretic (%) |
51.7 |
52.9 |
47.1 |
50.0 |
0.28 |
| Others (%) |
4.7 |
4.5 |
5.3 |
6.9 |
0.66 |
| Fixed combination (%) |
46.2 |
47.1 |
42.7 |
44.8 |
0.49 |
| DBP: diastolic blood pressure |
Discussion
In this cross-sectional visit-based study conducted in 1376 treated adult hypertensive patients in Switzerland in 2009, nearly three quarters had uncomplicated and one quarter complicated hypertension. Among the latter group, more than 80% were diabetic patients. The control rate of hypertension was 49% overall, 59% in uncomplicated and 19% in complicated hypertension (fig. 1). It was also 19% for the group of diabetic patients. The most prescribed antihypertensive drug class, alone or in combination, were ARBs and diuretics, followed by betablockers, ACE inhibitors, CCB and others.
Comparison of high BP control rates with earlier surveys in Switzerland is difficult because the study design [12–14] and/or the definitions of hypertension (control) [9, 14, 15] employed differ. For example, a comparison with the last available report, the prevalence, awareness, treatment and control of high BP from Lausanne [12], is not possible because the survey was population-based and in the present study it was visit-based. The difference is of major importance since visit-based studies concentrate on treated hypertensive patients visiting their physician, but ignore undiagnosed and untreated hypertensive patients and are likely to report better control rates than population-based studies. Moreover, in the CoLaus study BP was considered to be controlled if its level was <140/90 mm Hg, without differentiating between uncomplicated and complicated hypertension [12], while in the present study differentiated blood pressure goals are reported. When applying the same definition of BP control as that used in the CoLaus study, the control rate increases to 59% in the current SWISSHYPE study and compares favourably with the 48% reported in the Lausanne cohort [12]. Using the same definition of BP control (<140/90 mm Hg overall), the control rate in SWISSHYPE is also higher than recently reported in other western European countries (31–46%) [5] but lower than in the United States [5]. Overall, compared to earlier reports from Switzerland [9, 15] control of high BP seems to have improved, particularly in uncomplicated hypertension. However, the reported data are not entirely objective since they were provided by the attending physicians and may therefore be prone to embellishment.
As expected [16], high BP was not controlled in most cases (87.1%) because target SBP, isolated or jointly with target DBP, was not reached. This chiefly reflects aging of the population and its associated vessel stiffening (fig. 2) [16]. Moreover, and not surprisingly [17–19], compared to controlled hypertensives, patients not at goal had higher BMI, were more frequently diabetic, and had CKD more often. Conversely, better BP control was found in patients with established coronary heart disease. This finding is in agreement with other studies [14, 20] and may reflect increased attention of both physician and patient with regard to risk factor management in secondary prevention [21].
In SWISSHYPE, 33.9% of the patients were treated by antihypertensive monotherapy. Consequently, the remaining two thirds of the patients were treated by multiple drug classes including fixed combinations in 46.2% of cases or freely combined antihypertensive drugs in 40.2%. In 2001, as well as in a more recent survey from Lausanne, considerably more hypertensive patients (57% and 69% respectively) were treated by monotherapy in Switzerland [12, 15]. This change over time most probably reflects adherence to the newer guidelines [11, 22] which permit or even recommend initiating antihypertensive treatment with low-dose combination therapy (instead of performing sequential monotherapy).
Overall, the two most frequently prescribed drug classes were ARBs (51.4%) and diuretics (51.7%). Similar results were reported in the recent Swiss CoLaus study [12]. Thus, ARB use is frequent in Switzerland compared to other countries, where frequencies between 18–36% were reported [5]. This is in accordance with the guidelines of the Swiss Society of Hypertension [22] and may reflect the choice of the practitioners to prescribe a very well tolerated antihypertensive drug class which has similar antihypertensive efficacy to other classes [23, 24]. It may also reflect a trend towards early adoption of the newer medications on the market by doctors or intense commercial promotion [12]. Compared to data from Switzerland from 2001, the most common agents used for monotherapy have changed. Currently the class preferentially used were ARBs followed by ACE inhibitors, betablockers, CCB and diuretics, whereas in the earlier report the most frequently prescribed category were ACE-inhibitors followed by CCB, betablockers and hydrochlorothiazide [15]. The present drug prescription pattern is not strictly in keeping with the Swiss [22] or other hypertension guidelines [11, 25], especially with regard to the prescription of betablockers. The rate of use of betablockers as a monotherapy in SWISSHYPE is very similar to that recently reported in the UK, where the prescription rate fell from 29% in 2003 to 21% in 2006 [26].
Fixed combination therapy was used in 46% of the treated patients in the present SWISSHYPE survey. This rate seems relatively high but due to lack of data comparison with earlier Swiss reports or other European countries is not possible. The preferred fixed combination prescribed was by far the association of ARB + diuretic (53%) (fig. 3).
Among diabetic patients, 82.1% were treated with either an ACE inhibitor (33.8%) or an ARB (50.7%). This is in keeping with the guidelines [11, 22] but, even though the rate of use of inhibitors of the renin-angiotensin system is fairly good compared to other surveys [27–30], there is still room for improvement even if taking into account the very few diabetic patients who do not need such therapy and those who do not tolerate it. Considering that diabetes-associated hypertension is very often more salt-sensitive than other forms of hypertension, the rate of diuretic use in the present study (58.3%) seems low.
Diuretics and CCB are particularly efficacious and recommended for the treatment of isolated systolic hypertension, especially in elderly patients [11, 25]. In the current study, 33% of treated patients not at SBP target (<140 mm Hg) were receiving CCBs and 52% diuretics.
The study has some limitations which have been discussed and include the design (visit-based vs population-based), the diagnostic criteria applied for hypertension and comorbidities (which all relied on the judgment of the attending physician), the use of different BP-measuring devices (each physician using his/her own device) and the possibly embellished BP control results reported by the physicians.
In conclusion, this representative visit-based Swiss survey on treated adult hypertensive patients shows that control rates of hypertension have improved over time in Switzerland for uncomplicated but not for complicated, particularly diabetes-associated hypertension [9]. Compared to earlier reports [12, 15], and in accordance with the newer guidelines, more patients are treated by multiple antihypertensive drug classes with 46% receiving a fixed combination. As a monotherapy, ARBs are the most frequently used antihypertensive drug class, and betablockers represent the third most prescribed category, this being not strictly in keeping with the latest guidelines [11, 22]. Diuretics are probably underused in diabetes-associated as well as in isolated systolic hypertension, and more frequent use of CCBs in isolated systolic hypertension may improve control rates in this difficult-to-treat category of hypertensive patients. Finally, in as many as 67.3% of the uncontrolled hypertensive patients, no change in pharmacological treatment was made in the present SWISSHYPE survey.
Correspondence:
Prof. Yves Allemann MD FESC
Cardiology
Swiss Cardiovascular Centre Bern
University Hospital Bern
CH-3010 Bern
Switzerland
yves.allemann@insel.ch
References
1 Banegas JR, Rodriguez-Artalejo F, de la Cruz Troca JJ, Guallar-Castillon P, del Rey Calero J. Blood pressure in Spain: distribution, awareness, control, and benefits of a reduction in average pressure. Hypertension. 1998;32(6):998–1002.
2 Thamm M. Blood pressure in Germany – current status and trends. Gesundheitswesen. 1999;61 Spec No:S90–3.
3 Primatesta P, Brookes M, Poulter NR. Improved hypertension management and control: results from the health survey for England 1998. Hypertension. 2001;38(4):827–32.
4 Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. JAMA. 2003;290(2):199–206.
5 Wang YR, Alexander GC, Stafford RS. Outpatient hypertension treatment, treatment intensification, and control in Western Europe and the United States. Arch Intern Med. 2007;167(2):141–7.
6 Joffres MR, Ghadirian P, Fodor JG, Petrasovits A, Chockalingam A, Hamet P. Awareness, treatment, and control of hypertension in Canada. Am J Hypertens. 1997;10(10 Pt 1):1097–102.
7 Burt VL, Whelton P, Roccella EJ, Brown C, Cutler JA, Higgins M, et al. Prevalence of hypertension in the US adult population. Results from the Third National Health and Nutrition Examination Survey, 1988–1991. Hypertension. 1995;25(3):305–13.
8 Kotseva K, Wood D, De Backer G, De Bacquer D, Pyorala K, Keil U. Cardiovascular prevention guidelines in daily practice: a comparison of EUROASPIRE I, II, and III surveys in eight European countries. Lancet. 2009;373(9667):929–40.
9 Pechere-Bertschi A, Greminger P, Hess L, Philippe J, Ferrari P. Swiss Hypertension and Risk Factor Program (SHARP): cardiovascular risk factors management in patients with type 2 diabetes in Switzerland. Blood Press. 2005;14(6):337–44.
10 Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, et al. 2007 Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2007;25(6):1105–87.
11 Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, et al. 2007 ESH-ESC Practice Guidelines for the Management of Arterial Hypertension: ESH-ESC Task Force on the Management of Arterial Hypertension. J Hypertens. 2007;25(9):1751–62.
12 Danon-Hersch N, Marques-Vidal P, Bovet P, Chiolero A, Paccaud F, Pecoud A, et al. Prevalence, awareness, treatment and control of high blood pressure in a Swiss city general population: the CoLaus study. Eur J Cardiovasc Prev Rehabil. 2009;16(1):66–72.
13 Nedeltchev K, Arnold M, Baumgartner R, Devuyst G, Erne P, Hayoz D, et al. Vascular risk factors in the Swiss population. J Neurol. 2005;252(10):1210–6.
14 Jaussi A, Noll G, Meier B, Darioli R. Current cardiovascular risk management patterns with special focus on lipid lowering in daily practice in Switzerland. Eur J Cardiovasc Prev Rehabil. 2010;17(3):363–72.
15 Ferrari P, Hess L, Pechere-Bertschi A, Muggli F, Burnier M. Reasons for not intensifying antihypertensive treatment (RIAT): a primary care antihypertensive intervention study. J Hypertens. 2004;22(6):1221–9.
16 Chobanian AV. Clinical practice. Isolated systolic hypertension in the elderly. N Engl J Med. 2007;357(8):789–96.
17 Zaninelli A, Parati G, Cricelli C, Bignamini AA, Modesti PA, Pamparana F, et al. Office and 24-h ambulatory blood pressure control by treatment in general practice: the “Monitoraggio della pressione ARteriosa nella medicina TErritoriale” study. J Hypertens. 2010;28(5):910–7.
18 Kjeldsen SE, Naditch-Brule L, Perlini S, Zidek W, Farsang C. Increased prevalence of metabolic syndrome in uncontrolled hypertension across Europe: the Global Cardiometabolic Risk Profile in Patients with hypertension disease survey. J Hypertens. 2008;26(10):2064–70.
19 Saely CH, Risch L, Frey F, Lupi GA, Leuppi JD, Drexel H, et al. Body mass index, blood pressure, and serum cholesterol in young Swiss men: an analysis on 56784 army conscripts. Swiss Med Wkly. 2009;139(35-36):518–24.
20 Fang J, Alderman MH, Keenan NL, Ayala C, Croft JB. Hypertension control at physicians' offices in the United States. Am J Hypertens. 2008;21(2):136–42.
21 Berlowitz DR, Ash AS, Hickey EC, Friedman RH, Glickman M, Kader B, et al. Inadequate management of blood pressure in a hypertensive population. N Engl J Med. 1998;339(27):1957–63.
22 http://www.swisshypertension.ch . accessed in July 2010.
23 Yusuf S, Teo KK, Pogue J, Dyal L, Copland I, Schumacher H, et al. Telmisartan, ramipril, or both in patients at high risk for vascular events. N Engl J Med. 2008;358(15):1547–59.
24 Turnbull F, Neal B, Ninomiya T, Algert C, Arima H, Barzi F, et al. Effects of different regimens to lower blood pressure on major cardiovascular events in older and younger adults: meta-analysis of randomised trials. BMJ. 2008;336(7653):1121–3.
25 http://www.nice.org.uk/guidance/CG34. accessed in July 2010.
26 Falaschetti E, Chaudhury M, Mindell J, Poulter N. Continued improvement in hypertension management in England: results from the Health Survey for England 2006. Hypertension. 2009;53(3):480–6.
27 Ginsberg HN, Elam MB, Lovato LC, Crouse JR, 3rd, Leiter LA, Linz P, et al. Effects of combination lipid therapy in type 2 diabetes mellitus. N Engl J Med. 2010;362(17):1563–74.
28 Belletti DA, Zacker C, Wogen J. Effect of cardiometabolic risk factors on hypertension management: a cross-sectional study among 28 physician practices in the United States. Cardiovasc Diabetol. 2010;9:7.
29 ADVANCE – Action in Diabetes and Vascular Disease: patient recruitment and characteristics of the study population at baseline. Diabet Med. 2005;22(7):882–8.
30 Krempf M, Parhofer KG, Steg PG, Bhatt DL, Ohman EM, Rother J, et al. Cardiovascular event rates in diabetic and nondiabetic individuals with and without established atherothrombosis (from the REduction of Atherothrombosis for Continued Health [REACH] Registry). Am J Cardiol. 2010;105(5):667–71.