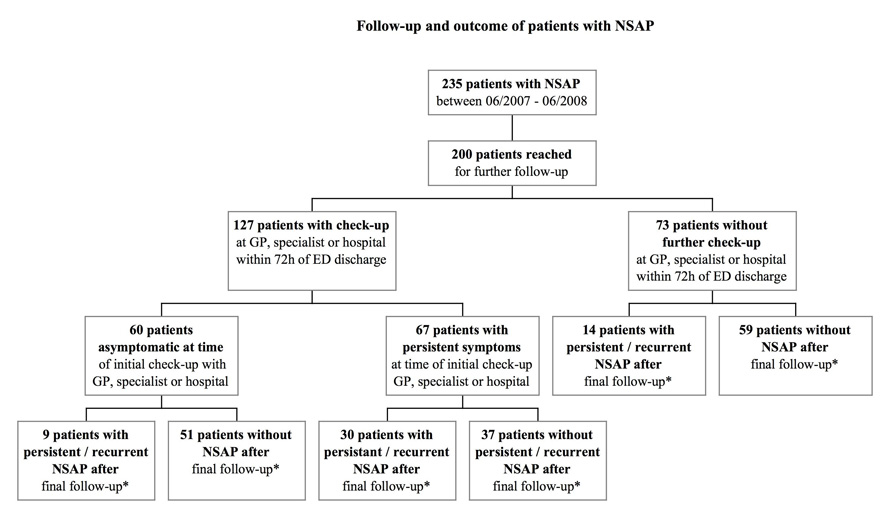
Figure 1
This figure summarises follow up and outcome of the 235 patients admitted to our ED with NSAP.
DOI: https://doi.org/10.4414/smw.2011.13167
A follow up of an underestimated problem
There is a high prevalence of depression in patients suffering from chronic pain [1–3] , resulting in a significant impact on overall quality of life [4–6] . Previous authors have shown that approximately 10% of all patients with chronic abdominal (or chest) pain without a somatic disorder suffered from major depression [7, 8].
Acute non-specific abdominal pain (NSAP) is defined as the presence of acute abdominal pain for less than seven days for which no somatic cause is found [9].
Some researchers have reported that more than 10% of all patients admitted to the emergency department (ED) with abdominal pain leave the hospital without identification of an underlying somatic cause [10]. Five year follow up of these patients reveals that more than one quarter have persistent NSAP [11]. Therefore, there is potentially a large group of patients suffering from concomitant depressive disorders.
NSAP is an obvious burden on financial and human resources [10]. Moreover, chronic NSAP significantly impairs the long term physiological and psychological well-being of patients [12]. The prevalence of anxiety and depression is increased in these patients, with serious impairments in their quality of life.
The primary aim of this survey was to evaluate the potential influence of long term NSAP on overall physical and mental health using the SF-36® questionnaire. The SF-36® questionnaire has proven useful in surveys of general and specific populations, comparing the relative burden of diseases, and in differentiating the health benefits produced by a wide range of different treatments. We chose to use the SF-36® questionnaire as it has been judged to be the most widely evaluated generic patient assessed health outcome measure, documented in nearly 4000 publications [13].
Retrospective analysis of a prospectively collected database included evaluation of all patients aged ≥16 years, discharged from our University Hospital ED between June 2007 and June 2008 with the diagnosis of NSAP (N = 235). Patients in whom other differential diagnoses such as “irritable bowel syndrome” or “chronic constipation” were listed in the discharge letter were not included for further evaluation. Furthermore, patients younger than 16 years of age, patients with abdominal trauma prior to admission or confirmed pregnancy were excluded from the analysis. 200 patients (85.1%) could be contacted for further follow-up.
Mean follow up between initial ED admission and administration of the SF-36® questionnaire was 12.5 months (range 3–15 months).
NSAP was defined as any acute abdominal pain less than seven days in duration prior to ED admission without evidence of an organic cause. All patients had radiological examinations (plain abdominal radiography and/or computed tomography of the abdomen and/or abdominal sonography), which had to be deemed normal by the on call radiologist as well as blood tests (full blood count, kidney and serum electrolyte test, amylase and liver function test) with either normal or non-specific results. If necessary, a specialist physician was involved (abdominal surgeon, gynaecologist, physician, gastroenterologist, urologist or psychiatrist).
Current health and overall well-being was evaluated using the SF-36® health questionnaire, Version 1 ( http://www.qualitymetric.com ). The overall score of the SF-36® health survey is based on eight scales: physical functioning, physical role, bodily pain, general health perceptions, vitality, social functioning, emotional role and mental health. Two summary measures can be calculated from these scales – the physical component score (PCS) and the mental component score (MCS) [14]. For ease of interpretation, each scale is transformed to a 0–100 scale using a transformation formula, hereby making it possible to compare results to the norms derived from the general population. A high score indicates a good health status. All questions relate to the four weeks preceding the questionnaire. A licensing agreement was obtained from the Office of Scholarly Grants and Research (OGSR) of QualityMetric Incorporated for the use of the SF-36® questionnaire ( http://www.qualitymetric.com/ ).
All patients were contacted by means of a telephone interview by two researchers working independently of this survey. Eligible patients were given details of the survey, including contact information of the researchers involved. The aim of the survey was explained and all patients were guaranteed anonymity and confidentiality with regard to any information given to the researcher.
To compare categorical variables, cross tables were calculated and a Fisher’s exact test performed. To predict the influence of specific factors such as migrational background, known previous psychiatric illness or chronic pain on the SF-36® health survey, ordinal linear regression models were chosen for each factor separately. Age and gender were also included in the regression models in order to adjust for these variables. Regression results were expressed as differences of means between the two levels of the predictor. Baseline level is defined as the absence of the corresponding attribute. 95% confidence intervals and p-values were also reported. To explore potential confounders regressions were performed with and without age, gender, concomitant disorders, chronic pain, previous surgery and psychiatric diagnosis.
A p-value <0.05 was considered statistically significant. As this survey is exploratory, p-values were not adjusted for multiple comparisons. All statistical analyses were performed by a statistician using the software R, version 2.9.2.
Of the 200 patients with NSAP, 57% were women and median age at admission 33 years (range 16–91) (table 1). With the exception of a higher prevalence of concomitant psychiatric illnesses in patients who could not be reached and subsequently not included in the study, versus patients who were reached for follow up and subsequently included in the study (20% versus 7.5%, p = 0.03), all other patient demographics were similar between the two groups. A comparison between patients with (N = 53) and without persistent NSAP (N = 147) at follow up revealed a higher incidence of other chronic pain syndromes and psychiatric diagnoses in patients with NSAP (p <0.001 and p = 0.03, respectively). Further details are given in table 2.
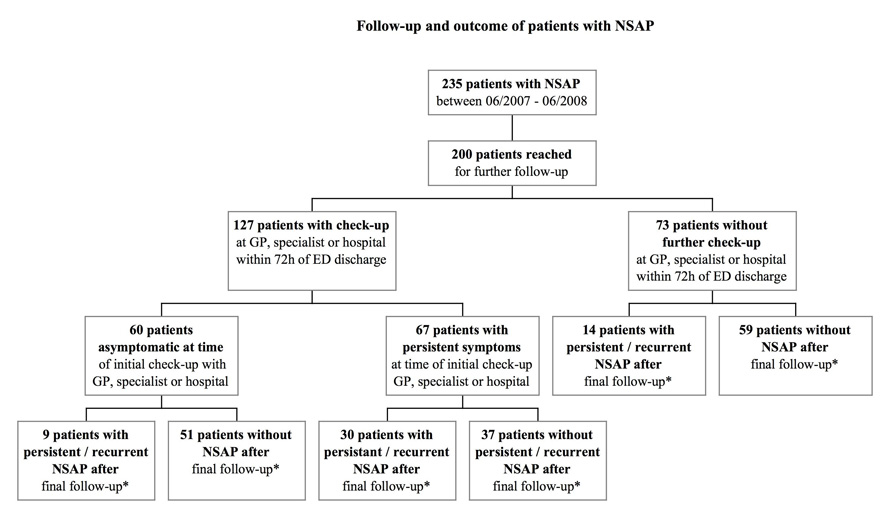
Figure 1
This figure summarises follow up and outcome of the 235 patients admitted to our ED with NSAP.
127 (63.5%) patients were either seen by their GP, an additional specialist or by a physician in our ED or in an ED of another hospital for a follow up clinical examination within 72 hours after discharge. 60 (47.2%) of these patients were asymptomatic at the check-up, with only a few (N = 9, 15%) of these pain free patients suffering from persistent/recurrent NSAP at the time-point of our questionnaire follow-up. The remaining 67 patients (52.8%) went for a check-up due to persistent symptoms. Of these patients, nearly half (N = 30 or 44.8%) were still symptomatic at our follow up. 73 patients (36.5%) did not chose to see another physician for follow up, irrespective of their pain status at that time. Within this group, 14 patients (19.2%) had recurrent NSAP at the time of the SF-36® follow up. In summary, 53 (26.5%) patients had recurrent/persistent NSAP. All results are summarised in figure 1.
Of the 127 patients seen within 72h post ED discharge, nearly half (N = 60, 47.2%) received further diagnostic tests, most often blood tests only. 59 (46.5%) patients received a simple check-up and additional pain medication, four patients also received laxatives. Eight (6.3%) patients eventually required explorative or therapeutic surgery. The diagnostic examinations carried out are summarised in table 3.
Just over half of all patients (N = 107, 53.5%) were on sick leave for one day or more (median 3 days, range 1–200 days).
Analysis of the unadjusted SF-36® scores revealed statistical differences for the PCS, MCS and all eight sub-scores for patients with and without persistent NSAP. NSAP persistence resulted in significantly worse overall physical and mental scores (p <0.001 on both occasions, 95% CI, -9-98 to –4.49 and 95% CI, –9.99 to –3.24) and significantly lower values for all eight sub-scores. The presence of a psychiatric diagnosis (e.g. major depression, schizophrenia, bipolar disease) also resulted in significantly reduced physical and mental scores (p <0.001) and worse sub-scores, such as bodily pain, general health perception or vitality. Patients with previously diagnosed chronic pain syndromes scored worse for physical components, with mental health slightly less affected. All results are summarised in table 4.
After adjustment for confounding factors (e.g. presence of a psychiatric illness/chronic pain syndrome, etc) NSAP persistence remained a statistically significant predictor for worse SF-36® scores for all eight sub-scores. Furthermore, significantly lower MCS and PCS scores were achieved (p <0.001 for both scores, 95% CI, –9.58 to –2.59 and 95% CI, –7.76 to –2.32). Details are given in table 5.
| Table 1: Patient demographics of the 200 patients who could be reached for follow-up. | |
| Sociodemographic details | Patients reached (N = 200) |
| Gender, female (%) | 114 (57) |
| Age median, overall (range) in years | 33 (16–91) |
| Age median, female (range) in years | 27.5 (16–91) |
| Age median, male (range) in years | 44.5 (16–86) |
| Migrational background = N (%) | |
| Swiss national | 120 (60.0) |
| Non-Swiss national | 80 (40.0) |
| Chronic pain syndrome = N (%) | 20 (10) |
| Psychiatric diagnosis = N (%) | 15 (7.5) |
| Concomitant diagnosis = N (%) | |
| Cardiovascular | 14 |
| Previous Cancer | 10 |
| Diabetes | 8 |
| COPD / Asthma | 5 |
| Infectious diseases | 4 |
| Intravenous drug use | 2 |
| Total number of diagnoses | 43 (21.5) |
| Number of patients with concomitant diagnoses | 39 (19.5) |
| Previous abdominal surgery = N (%) | 51 (25.5) |
| Table 2: Compares patient demographics between patients who suffered from persistent NSAP at the time point of the follow-up (N = 53) and those without NSAP (N = 147). | |||
| Sociodemographic details | Patients with persistent NSAP N = 53 | Patients without persistent NSAP N = 147 | p-value |
| Gender, female (%) | 34 (64.2) | 80 (54.4) | 0.26 |
| Age, median (range) in years | 34 (16–91) | 33 (16–86) | 0.75 |
| – Swiss national– Non-Swiss national | 31 (58.5) 22 (41.5) | 89 (60.5) 58 (39.5) | 0.87 |
| Chronic pain syndrome = N (%) | 14 (26.4) | 6 (4.1) | <0.001 |
| Psychiatric diagnosis = N (%) | 8 (15.1) | 7 (4.8) | 0.03 |
| Concomitant diagnosis = N (%) | 14 (26.4) | 25 (17.0) | 0.16 |
| Previous abdominal surgery = N (%) | 18 (34.0) | 33 (22.4) | 0.14 |
| A p value of <0.05 was considered statistically significant and this is highlighted in bold print. | |||
| Table 3: Patients who consulted a GP, a specialist or a physician in our ED or in the ED of another hospital after initial discharge. | |
| Number of Patients = N (%) | |
| Additional diagnostics*– Blood test only– Colonoscopy / gastroscopy– Imaging– Imaging and endoscopy | 60 (47.2)3315102 |
| Clinical examination, additional analgesics (or laxatives) | 59 (46.5) |
| Diagnostic / therapeutic surgery– Appendectomy– Cholecystectomy– Percutaneous nephrostomy– Oophorectomy | 8 (6.3)3311 |
| Total number of patients | 127 |
| * All patients requiring additional diagnostics underwent a repeat blood test ± further tests | |
| Table 4: Analysis of mean (± SD) physical and mental component scores influencing NSAP. The analyses of the risk factors predictive for the different SF-36® scores are adjusted for age and gender. | ||||||||||
| Migrational background | Chronic pain syndrome | Psychiatric diagnosis | Previous abdominal surgery | Persistent NSAP | ||||||
| No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | |
| Mean (± SD) | ||||||||||
| Physical function | 52.3 (7.8) | 52.9 (6.9) | 53.4 (6.6)** | 42.3 (9.6)** | 53.7 (5.7)** | 42.6 (12.4)** | 53.69 (6)* | 49.2 (9.9)* | 53.9 (5.5)** | 48.9 (10.5)** |
| Role of physical | 48.6 (11.2) | 48.2 (11.5) | 49.6 (10.6)* | 35 (11.3)* | 49.3 (10.7)** | 40.7 (13.3)** | 49.3 (10.8) | 45.8 (12.4) | 50.6 (9.9)** | 42.6 (12.6)** |
| Bodily pain | 51 (11.7) | 50.2 (11) | 51.5 (11.1)* | 40.6 (11.4)* | 51.5 (11)** | 43.5 (12.8)** | 51.8 (11.1)* | 47.6 (12.1)* | 53.2 (9.5)** | 43.7 (13.3)** |
| General health perception | 47.3 (12.1) | 45.8 (12.3) | 47.6 (11.8)** | 35.8 (12.1)** | 47.7 (11.7)* | 38.1 (13.1)* | 47.9 (12.5) | 43.2 (10.5) | 48.5 (12.1)** | 41.8 (10.9)** |
| Vitality | 52.1 (11.4) | 50.2 (12.3) | 52 (11.7) | 43.1 (8.9) | 51.8 (11.6)* | 47.6 (12.5)* | 52 (11.8) | 49.5 (11.6) | 53.1 (11.2)** | 46.5 (11.9)** |
| Social functioning | 48.3 (11.8) | 49 (10.2) | 49.3 (10.7)** | 39.8 (13)** | 49.6 (10.3)* | 39.5 (14.3)* | 49.2 (10.7) | 46.6 (12.2) | 51.3 (9.2)** | 41.1 (12.6)** |
| Role of emotional | 50.2 (9.4) | 50.7 (9) | 51.2 (8.2)* | 40.6 (14.8)* | 51.1 (8.3)** | 44.3 (13.9)** | 50.4 (9.2) | 50.4 (9.3) | 51.5 (7.4)* | 47.2 (12.5)* |
| Mental health | 49.6 (10.4) | 47.6 (12.5) | 50 (10.5)* | 34.4 (10.7)* | 49.5 (10.6)** | 43 (15.5)** | 49.1 (11.8) | 48.1 (9.8) | 50.8 (10.2)** | 43.4 (12.5)** |
| Physical component score | 50.3 (9.3) | 50 (9.3) | 51 (8.7)** | 40.1 (10.3)** | 51.2 (8.5)** | 41.2 (10.7)** | 51.6 (8.4)* | 46.1 (10.5)* | 52.1 (7.5)** | 44.9 (11.4)** |
| Mental component score | 49.5 (10.9) | 48.5 (11.3) | 50 (10.4) | 38.7 (13.4) | 49.6 (10.6)** | 44.4 (13.9)** | 49.1 (11.3) | 49.2 (10.5) | 50.9 (9.9)** | 44.2 (12.7)** |
| * denotes a value of p <0.05, ** a value of p <0.001. Statistically significant values are highlighted in bold. Values without a * / ** are statistically not significant, where p >0.05. | ||||||||||
| Table 5: Analysis of persistent NSAP on physical and mental component scores according to the SF-36® questionnaire. The table shows the unadjusted score differences as well as the score differences adjusted for confounders (psychiatric or concomitant diagnosis, chronic pain syndrome, previous abdominal surgery). | ||||
| Persistent NSAP | p-value | Persistent NSAP | p-value | |
| Unadjusted score difference | Adjusted score difference | |||
| Physical function | –5 (–7.25, –2.75) | <0.001 | –2.47 (–4.41, –0.52) | 0.013 |
| Role of physical | –7.93 (–11.3, –4.5) | <0.001 | –6.21 (–9.69, –2.73) | <0.001 |
| Bodily pain | –9.51 (–12.9, –6.14) | <0.001 | –7.74 (–11.2, –4.29) | <0.001 |
| General health perception | –6.62 (–10.4, –2.89) | <0.001 | –4.92 (–8.78, –1.06) | 0.013 |
| Vitality | –6.65 (–10.3, –3.04) | <0.001 | –6.33 (–10.16, –2.5) | 0.001 |
| Social functioning | –10.21 (–13.4, –6.9) | <0.001 | –8.77 (–12.19, –5.34) | <0.001 |
| Role of emotional | –4.35 (–7.2, –1.5) | 0.003 | –3.18 (–6.11, –0.26) | 0.033 |
| Mental health | –7.37 (–10.8, –3.95) | <0.001 | –6.22 (–9.7, –2.74) | <0.001 |
| Physical component score | –7.23 (–9.98, –4.49) | <0.001 | –5.04 (–7.76, –2.32) | <0.001 |
| Mental component score | –6.62 (–9.99, –3.24) | <0.001 | –6.09 (–9.58, –2.59) | <0.001 |
| P-values of <0.05 are considered statistically significant. | ||||
Results from this survey suggest that long term persistence of NSAP is associated with a reduced mental and physical well-being, reflected by a much lower MCS and PCS as defined by the SF-36® questionnaire. Other scores such as general health perception, bodily pain, social functioning and vitality are also greatly reduced when compared to patients without NSAP. This remains true, even after adjustment for other potentially confounding factors, such as the presence of a known psychiatric illness or previous chronic pain disorders.
Interestingly, significantly more patients with persistent NSAP suffered from concomitant psychiatric illnesses such as depression (majority of patients), bipolar disorders or schizophrenia (classified according to the International Classification of Diseases (ICD-10) at the time point of ED admission) than patients without NSAP.
Persistence of NSAP raises the question whether these patients either have an unidentified abdominal ailment despite extensive diagnostics or whether other independent factors, possibly of psychological nature, influence pain persistence.
It has been suggested that poor illness perception, exaggerated attention to bodily changes and sensations, depression and other psychiatric disorders influence unexplained physical symptoms or may even be the cause of the latter [15–17]. There is some evidence that psychological disorders can contribute at least partially to NSAP [18]. Baune and colleagues emphasize that pain, even in non-chronic forms, is associated with depression and this in turn is associated with lower quality of life scores [7]. However, not all studies support the notion that systemic complaints without objective findings are necessarily due to somatoform disorders [19, 20].
Although the percentage of patients with persistent NSAP (N = 53) who do meet the criteria for a current psychiatric disorder is higher than in patients without NSAP (15.1 versus 4.8 percent, p = 0.03), many patients with persistent NSAP do not suffer from a mental illness.
Twenty patients (10%) in our study population also suffered from chronic pain, mainly lower back pain or neck and/or shoulder pain, which negatively influenced general quality of life as measured by the SF-36® questionnaire. Previous work has shown that psychosocial factors have a strong influence on the onset and chronicity of pain that is primarily of non-organic origin, such as low back pain or chronic, widespread pain [21, 22]. More recently, Halder et al. have shown that psychological distress, fatigue and anxiety behaviour are predictors of the future onset of NSAP, rather than being a mere consequence of the symptoms [23]. Furthermore, reported low back pain at baseline significantly predicted the new onset of NSAP. The interaction between pain symptoms, physical illness and depressive symptoms is complex. Depressive disorders may amplify both medically explained and unexplained symptoms, such as NSAP. Whether physical pain, such as NSAP, precipitates depressive symptoms is not always straightforward to answer.
Non-organic chronic pain, including persistent NSAP, is responsible for up to 50% of all physician visits [24, 25] and half of all consultations for gastrointestinal problems.
Only eight patients (6.3%) patients consequently required surgery for what was later deemed to be the actual cause of the abdominal pain, such as appendicitis or cholecystitis. This still leaves 53 patients (26.5%) with persistent abdominal pain without an identifiable cause. Previous work from our group has shown similar long term persistence of NSAP, with over one quarter of patients (27.9%) suffering from recurring NSAP five years after initial ED [11].
Based on our own findings we aim to set up a new diagnostic and therapeutic algorithm, which includes all patients discharged from our ED with a provisional diagnosis of NSAP. Once an organic cause has been ruled out, patients are integrated into carefully organized follow up consultations with their GP and our ED. Pain persistence will lead to involvement of pain specialists and/or psychiatric/psychosomatic help, again, only once a somatic cause has been ruled out. Early problem identification with a more structured and better organized support will aim to improve long term outcome in patients, who often feel that they are not taken seriously enough.
Our study has several limitations. Our sample size is small and represents a single institution experience in a tertiary care ED setting and may therefore not be generalisable to all populations. Furthermore, some bias may exist, although the response rate was quite high at 85%. While patient demographics of those who could and those who could not be reached did not differ statistically – with the exception of an increased prevalence of psychiatric disorders in the non-responder group – it remains speculative whether the non-responders represent the entire study population.
A notable limitation in our cross-sectional analysis is that cause and effect cannot be established. Notably, there is no way to determine if a decreased quality of life is a result of persistent NSAP or a causative factor.
Differences in time to follow up may distort the significance of the reported results, as certain symptoms influencing sub-scores – such as bodily pain or general health perception – may alter with the time since ED discharge. Our sample size is too small to allow a detailed analysis of the effect of time to follow-up on symptom resolution and resulting changes in the SF-36® score. Finally, all quality of life surveys have advantages and disadvantages. We chose to use the SF-36® questionnaire as a generic quality of life measure, as it has been repeatedly proven to be an effective and accurate measure of an individual’s perception of his or her quality of life in health outcome research.
In conclusion, this study for the first time evaluates the long-term association of persistent NSAP on a patient’s general mental and physical well-being. It highlights the fact that what clinicians may see as annoying abdominal pain without organic cause may indeed result in significant morbidity for the patient.
Given the high prevalence of NSAP, these results indicate that NSAP has a substantial social impact in this country and greater efforts should be undertaken to explore early support and potential (psychological) treatment options.
This study was not specifically funded and the authors do not have any competing interests to declare.
1 Dworkin RH, Gitlin MJ. Clinical aspects of depression in chronic pain patients. Clin J Pain. 1991;7:79–94.
2 Fishbain DA, Cutler R, Rosomoff HL, et al. Chronic pain-associated depression: antecedent or consequence of chronic pain? A review. Clin J Pain. 1997;13:116–37.
3 Rush AJ, Polatin P, Gatchel RJ. Depression and chronic low back pain: establishing priorities in treatment. Spine. 2000;25:2566–71.
4 Booth BM, Zhang M, Rost KM, et al. Measuring outcomes and costs for major depression. Psychopharmacol Bull. 1997;33:653–8.
5 Eaton WW, Anthony JC, Mandel W, et al. Occupations and the prevalence of major depressive disorder. J Occup Med. 1990;32:1079–87.
6 Greenberg PE, Kessler RC, Birnbaum HG, et al. The economic burden of depression in the United States: how did it change between 1990 and 2000? J Clin Psychiatry. 2003;64:1465–75.
7 Baune BT, Caniato RN, Garcia-Alcaraz MA, et al. Combined effects of major depression, pain and somatic disorders on general functioning in the general adult population. Pain. 2008;138:310–7.
8 Magni G, Caldieron C, Rigatti-Luchini S, et al. Chronic musculoskeletal pain and depressive symptoms in the general population. An analysis of the 1st National Health and Nutrition Examination Survey data. Pain. 1990;43:299–307.
9 Morino M, Pellegrino L, Castagna E, et al. Acute nonspecific abdominal pain: A randomized, controlled trial comparing early laparoscopy versus clinical observation. Ann Surg. 2006;244:881–6; discussion 6–8.
10 Sheridan WG, White AT, Havard T, et al. Non-specific abdominal pain: the resource implications. Ann R Coll Surg Engl. 1992;74:181–5.
11 Banz VM, Sperisen O, de Moya M, et al. A 5-year follow-up of patients discharged with non-specific abdominal pain: out of sight, out of mind? Intern Med J. 2010; Epub ahead of print.
12 van den Heuvel-Janssen HA, Borghouts JA, Muris JW, et al. Chronic non-specific abdominal complaints in general practice: a prospective study on management, patient health status and course of complaints. BMC Fam Pract. 2006;7:12.
13 Garratt A, Schmidt L, Mackintosh A, et al. Quality of life measurement: bibliographic study of patient assessed health outcome measures. BMJ. 2002;324:1417.
14 Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83.
15 Kirmayer LJ, Looper KJ. Abnormal illness behaviour: physiological, psychological and social dimensions of coping with distress. Curr Opin Psychiatry. 2006;19:54–60.
16 Henningsen P, Zimmermann T, Sattel H. Medically unexplained physical symptoms, anxiety, and depression: a meta-analytic review. Psychosom Med. 2003;65:528–33.
17 Nimnuan C, Hotopf M, Wessely S. Medically unexplained symptoms: an epidemiological study in seven specialities. J Psychosom Res. 2001;51:361–7.
18 Joyce PR, Bushnell JA, Walshe JW, et al. Abnormal illness behaviour and anxiety in acute non-organic abdominal pain. Br J Psychiatry. 1986;149:57–62.
19 Epstein SA, Kay G, Clauw D, et al. Psychiatric disorders in patients with fibromyalgia. A multicenter investigation. Psychosomatics. 1999;40:57–63.
20 Johnson SK, DeLuca J, Natelson BH. Assessing somatization disorder in the chronic fatigue syndrome. Psychosom Med. 1996;58:50–7.
21 Papageorgiou AC, Croft PR, Thomas E, et al. Psychosocial risks for low back pain: are these related to work? Ann Rheum Dis. 1998;57:500–2.
22 Thomas E, Silman AJ, Croft PR, et al. Predicting who develops chronic low back pain in primary care: a prospective study. BMJ. 1999;318:1662–7.
23 Halder SL, McBeth J, Silman AJ, et al. Psychosocial risk factors for the onset of abdominal pain. Results from a large prospective population-based study. Int J Epidemiol. 2002;31:1219–25; discussion 25–6.
24 Barsky AJ, Borus JF. Somatization and medicalization in the era of managed care. JAMA. 1995;274:1931–4.
25 Kroenke K, Price RK. Symptoms in the community. Prevalence, classification, and psychiatric comorbidity. Arch Intern Med. 1993;153:2474–80.