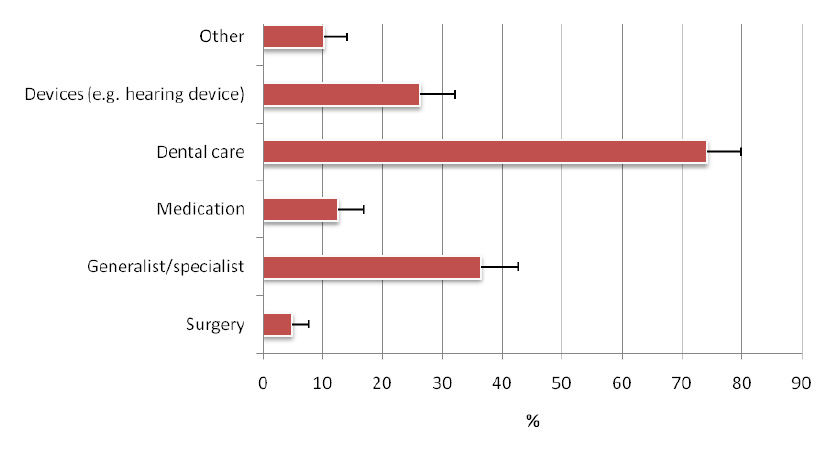
Figure 1
Type of renounced health care during the previous 12 months among a representative sample of 35 to 74 year old citizens of the canton of Geneva, Switzerland (2008-9).
DOI: https://doi.org/10.4414/smw.2011.13165
Equivalence of currencies: 1 CHF ≈ 1$ ≈ 1.35€
Most societies elaborate ways to contain increasing health care expenditure. Switzerland, which ranks second in the list of the world’s most expensive health care systems, has universal health-insurance coverage, permitting access to a broad range of services. Patients are largely satisfied with the health care they receive [1].
Health insurance is compulsory for all citizens of Switzerland (7 million) and insurance premiums are paid independently of earnings [2]. Subsidies are paid for citizens with low income (e.g., in Geneva, subsidies were paid for 30.7% of citizens in 2009, a figure similar to the national mean [31.4%]) [3]. Health insurance covers the costs of medical treatment and hospitalisation of the insured. However, the insured person pays part of the cost of treatment: 1. an annual flat deductible, called the franchise, which ranges from CHF 300 to a maximum of CHF 2,500 (1CHF ≈ 1$ ≈ 1.35€), at the insured person’s choice (premiums are adjusted accordingly); and 2. a 10% deductible of the costs up to a stop-loss amount of CHF 700. Dental care is not included in the basic health insurance. In 2010, the average monthly compulsory basic insurance premiums were: CHF 351 for adults >25, CHF 294 for those aged 19–25 and CHF 84 for those <18 years [4]. Some 40% of the Swiss population choose to top up their insurance coverage with private health insurance, which offers a wider choice of treatments and health professionals, or more comfortable accommodation during a hospital stay. In contrast to basic insurance, insurers may refuse applicants for private insurance or only accept them subject to conditions. Between 1999 and 2009, health insurance premiums increased by 54%, with increasing out-of-pocket payments; cuts in the catalogue of reimbursed health care services were decided as cost-containment measures [5].
Health and socioeconomic status are closely related: in general, lower socioeconomic status is related to worse health outcomes [6, 7]. Ensuring socioeconomic equity and responsiveness of the health care system is often considered a high priority in health policymaking, as lack of access and responsiveness may cause or at least reinforce any socioeconomic gradient in health [8, 9]. Health care renunciation for economic reasons may worsen chronic diseases and increase the risk of complications and hospitalisation [10].
The aims of the study were to estimate the extent of of health care renunciation for economic reasons and to identify associated factors.
Our study used a population-based cross-sectional survey (2008–2009) of a representative sample in the Canton of Geneva, Switzerland. The “Bus Santé”-survey is an ongoing population-based cross-sectional study which collects information on cardiovascular (CV) risk factors. Details about the population and sampling methods are described elsewhere [11]. Briefly, every year the Unit of Population Epidemiology contacts and studies a representative stratified sample of men and women from the population of Geneva Canton (inhabitants in 2009). This ongoing, community-based surveillance has been designed to monitor chronic disease risk factors continuously since 1993 [12]. Subjects are selected independently throughout each year to represent the canton’s approximately 100 000 male and 100 000 female non-institutionalised residents aged 35–74 years. Eligible subjects are identified by means of a standardised procedure using an annual residential list established by local government. This list includes all potential eligible participants except persons living illegally in the country. Stratified random sampling is performed on the basis of the list, by gender, within 10-year age strata, proportional to the corresponding population distributions. Selected subjects are mailed an invitation to participate, and, if they do not respond, up to 7 telephone attempts are made at different times on various days of the week. If telephone contact is unsuccessful, 2 letters are mailed. Subjects not reached are replaced using the same selection protocol. Subjects who refuse to participate are not replaced. The participation rates reached 51% in 2008 and 54% in 2009. Each participant receives several self-administered, standardised questionnaires covering lifestyle and the risk factors for major chronic diseases.
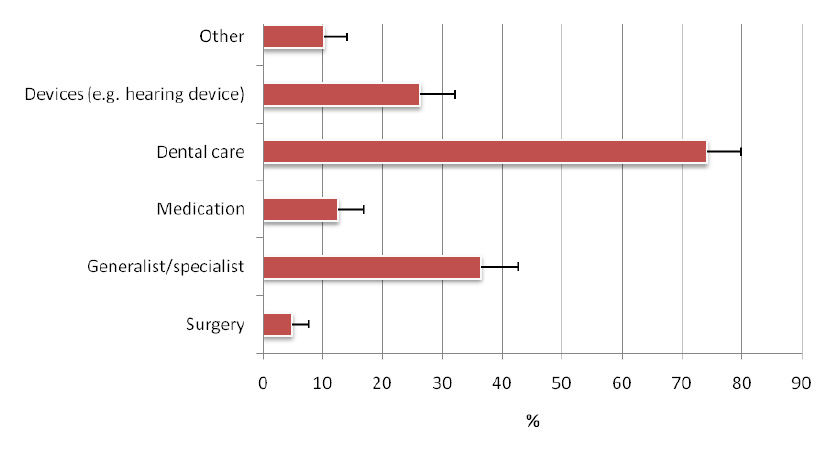
Figure 1
Type of renounced health care during the previous 12 months among a representative sample of 35 to 74 year old citizens of the canton of Geneva, Switzerland (2008-9).
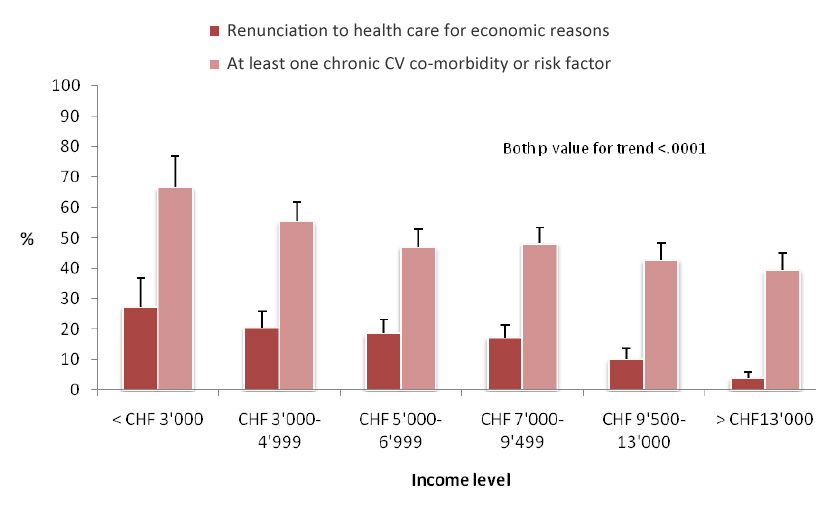
Figure 2
Health care renunciation for economic reasons during the previous 12 months and cardiovascular co-morbidity or risk factor among a representative sample of 35 to 74 year old citizens of the canton of Geneva, Switzerland (2008-9).
Renouncing health care for economic reasons was assessed by questionnaire. Participants were asked whether, during the previous 12 months, they had renounced any health care service for economic reasons. Participants specified the type of renounced health care (e.g. surgery), if any. Participants were also asked whether, during the previous 12 months, they had been unable to pay their premiums for economic reasons. For the present analyses, renounced health care was classified using the following six categories: devices (e.g., glasses or hearing device), healthcare provider consultation (generalist or specialist physician), surgery, dental health, medication, and others.
Information on CV comorbidities and risk factors (smoking, diabetes, hypertension, hypercholesterolaemia, myocardial infarction, angina, arterial thrombosis) were collected using questionnaires and defined as follows: yes to both questions: “Have you ever been told that you had diabetes/high blood pressure/high cholesterol/myocardial infarction? If so, are you taking a drug for it?” (if appropriate). Smoking was defined as current smoker.
Occupation, education, and income were used to characterise socioeconomic status. Occupation was grouped into independent/non-manual and non-independent/manual. Education was grouped as high (≥13 years), medium (9–12 years), and low (≤8 years). Income was grouped into 6 categories (<CHF 3000/month, 3000–4999, 5000–6999, 7000–9499, 9500–13000, >13000). Deductible was grouped into 3 categories (CHF ≤500, 1000–1500 and ≥2000). All information was self-reported. There were no language restrictions as long as the participants were able to understand and answer the questionnaires. In 2008–9, 0.8% of the subjects were ineligible because of language problems. All participants gave written informed consent. The “Bus Santé”-survey was approved by the ethical research committee of the Geneva University Hospitals.
Means and frequencies (with 95% confidence intervals) of study variables were calculated. Cochran-Armitage test was used to test trends. Logistic regression models were used to test associations between renunciation of health care for economic reasons and study variables. In Switzerland most subjects do not have insurance for dental care, so we conducted a subanalysis among subjects who renounced care but not dental care. All p values were 2-tailed and significance set at <0.05. All analyses were performed using SAS software (SAS Institute, Inc., Cary, North Carolina).
Information on renunciation of care was missing for only 2 subjects who were excluded from the analyses. 765 men and 814 women aged 35–74 years participated (participation rate = 51.5%). Mean age was 51.9 (standard deviation [SD] 10.9) for men and 51.5 (SD 10.8) for women. 229 out of 1579 (14.5%) (95%CI 12.7–16.2) renounced health care for economic reasons. Among those who renounced health care, 74% (95%CI 12.7–16.2) renounced dental care and 36% (82/225), (95%CI 30.1–42.7) physician consultation (21% specialist, 15% general practitioner), 26% (59/225) (95%CI 20.4–31.9) health devices, 12% medication (28/225) (95%CI 8.1–16.7) and 4.9% (11/225) (95%CI 2.0–7.7) surgery (fig. 1).
Income level was negatively correlated with renunciation of care (r = –0.18; p-value = 0.02, fig. 2, table 1). 58 subjects renounced care but not dental care. When the analysis was restricted to this subgroup, the association between health care renunciation and income remained. Thus, dental care was not the only relevant factor for the association.Persons with the lowest income (<3000 CHF/month) renounced health care 9 times more frequently than those with the highest income (≥13 000 CHF) (27.3% vs. 3.8%). Further, those with the lowest income presented with the highest burden in terms of CV disease or risk factors (r = –0.12, p <0.0001 (fig. 2). Compared to non-renouncing subjects, renouncers were 54% more likely to have at least one CV comorbidity or risk factor (OR 1.54 95%CI 1.10–2.17, adjusted for age, gender, Swiss citizenship, education, occupation, income and deductible level). We found no interaction between income and renunciation of health care on the prevalence of CV co-morbidity or risk factors.
After adjustment for smoking, age, sex, education, occupation, CV co-morbidities, deductible level, and Swiss citizenship, each decrease in the income level provided a 48% increased risk of renouncing health care for economic reasons (aOR 1.48, 1.31–1.65).
During 2008 and 2009, 4.7% of participants declared they were unable to pay their health insurance premium at least once.
| Table 1: Adjusted odds ratios (OR) and 95% confidence intervals (CI) for risk of health care renunciation for economic reasons by income during the previous 12 months among a representative sample of 35- to 74-year-old citizens of the Canton of Geneva, Switzerland (2008–9). | |
| Adjusted* OR (95%CI) | |
| Income < CHF 3000 vs >13 000 3000–4999 vs >13 000 5000–6999 vs >13 000 7000–9499 vs >13 000 9500–13 000 vs >13 000 | 13.46 (5.85–30.93) 6.17 (2.98–12.76) 4.98 (2.44–10.14) 4.84 (2.43–9.64) 2.50 (1.20–5.21) |
| * Odds ratios are adjusted for smoking, age, gender, CV comorbidity, Swiss citizenship, education, occupation, and deductible level. | |
A substantial proportion (14.5%) of a representative sample of the general population of Geneva renounced health care for economic reasons during the previous year. 75% renounced dental care, 36% physician consultation and 26% health devices such as eyeglasses or hearing devices. Because dental care is not covered by the basic health insurance in Switzerland, dental care may be the first health care to be renounced among people with scarce economic resources. Nevertheless, the association between income and health care renunciation remained after removing dental care renunciation. Thus, dental care was not the only relevant factor associated with health care renunciation.
Another expected finding was the inverse correlation of income with health care renunciation. The poorest were 13 times more likely to renounce health care than the richest, even after adjustment for CV comorbidities, smoking, education and occupation.
Strengths of the study are the representativeness of the participants, as well as the large sample size which allowed conclusions for an entire Swiss Canton. However, our results may not be representative of Switzerland as a whole. Another limitation is the self-reported nature of part of the data. Also, since no former data exist, it is difficult to relate health care renunciation to cost containment instruments. It could also be related to other factors connected with health care underuse not assessed in our survey, such as culture, patient-doctor communication, or patient motivation [13–15]. Finally, a complete physical morbidity assessment would have improved the strength of the study but was not available.
Delay in access to health care and prevention may worsen health problems and, in the end, increase costs, as diseases are not detected in their early stages [10, 16–19]. Also, the accumulation of negative social determinants of health, such as lower educational level or lower income, determines a higher burden of disease [6, 7]. Our findings highlight the fact that persons with lower income have the highest burden of disease and renounce care more frequently. The highest proportion of dental care renunciation is worrying and must be interpreted in the light not only of the association between dental health with socioeconomic status, but also with cardiovascular outcomes [20, 21]. A meta-analysis found a 20% higher risk of future cardiovascular events in individuals with periodontal disease compared with those without. This increase in relative risk is more pronounced (44%) in persons aged ≤65 years. Although the increase in CV risk between subjects with or without periodontal disease in the general population is modest, it may have a profound public health impact since nearly 40% of the population has periodontal disease [22].
Income is a strong determinant of health and relates to various social determinants of health, such as housing, healthy food or access to health care [6]. In our study each decrease in income level provided a 48% higher risk of renouncing health care for economic reasons. This finding stresses how important it is that the organisation of public health systems should ensure equity in access to health care, which means that it should be available to all, including the socioeconomically disadvantaged. Our results suggest that this goal is not realised in one of the wealthiest countries of the world.
In a region of Switzerland with a high cost of living, such as Geneva, socioeconomic status may influence the use of the health care system and health care renunciation for economic reasons was not uncommon. In the previous year more than 30% of the lowest income group renounced health care for economic reasons. This effect is most pronounced in dental care, which is not included in the basic health insurance. Health care underuse and renunciation may worsen the health status of a substantial part of society.
The authors thank all collaborators of the Unit of Population Epidemiology for their involvement in the “Bus Santé” study. IG is supported by a Swiss National Science Foundation grant (SNF 33CM30-124087/1).
The authors declare no conflict of interest. Funding: budget of Bus Santé, University Hospitals of Geneva and the General Directorate of Health, Canton of Geneva, Switzerland.
1 OECD. OECD and WHO survey of Switzerland’s health system. http://www.oecd.org/document/47/0,2340,en_2649_201185_37562223_1_1_1_1,00.html. 19-10-2006.
2 Reinhardt UE. The Swiss health system: regulated competition without managed care. JAMA. 2004;292(10):1227–31.
3 Office cantonal de la statistique. Prestations allouées dans le cadre de la réduction individuelle de primes et bénéficiaires de réductions individuelles de primes dans l'assurance obligatoire des soins LAMal (AOS), par canton, depuis 1999. http://www.ge.ch/statistique/tel/domaines/13/13_03_3/T_13_03_3_6_02.xls . 2010.
4 Federal Office of Public Health. Kantonale Durchschnittsprämien 2010/2011 der oblig. Krankenpflegeversicherung. http://www.bag.admin.ch/themen/krankenversicherung/00261/index.html?lang=de. 2010.
5 Swiss Federal Statistical Office. Krankenversicherungsprämien – Daten, Indikatoren. http://www.bfs.admin.ch/bfs/portal/de/index/themen/05/03/blank/key/index.html. 2010.
6 Wilkinson R, Marmot M. Social determinants of health: the solid facts. World Health Organization, Europe 2003; 2. edition: 10–25.
7 Marmot M. Social determinants of health inequalities. Lancet. 2005;365(9464):1099–104.
8 Wagstaff A, Van Doorslaer E. Income inequality and health: what does the literature tell us? Annu Rev Public Health. 2000;21:543–67.
9 Van Doorslaer E, Wagstaff A, van der BH, Christiansen T, De Graeve D, Duchesne I, et al. Equity in the delivery of health care in Europe and the US. J Health Econ. 2000;19(5):553–83.
10 Heisler M, Choi H, Rosen AB, Vijan S, Kabeto M, Langa KM, et al. Hospitalizations and deaths among adults with cardiovascular disease who underuse medications because of cost: a longitudinal analysis. Med Care. 2010;48(2):87–94.
11 Galobardes B, Costanza MC, Bernstein MS, Delhumeau CH, Morabia A. Trends in risk factors for the major “lifestyle-related diseases” in Geneva, Switzerland, 1993–2000. Ann Epidemiol. 2003;13(7):537–40.
12 Galobardes B, Costanza MC, Bernstein MS, Delhumeau C, Morabia A. Trends in risk factors for lifestyle-related diseases by socioeconomic position in Geneva, Switzerland, 1993–2000: health inequalities persist. Am J Public Health. 2003;93(8):1302–9.
13 Baroletti S, Dell'Orfano H. Medication adherence in cardiovascular disease. Circulation. 2010;121(12):1455–8.
14 Piette JD, Heisler M, Wagner TH. Cost-related medication underuse among chronically ill adults: the treatments people forgo, how often, and who is at risk. Am J Public Health. 2004;94(10):1782–7.
15 Piette JD, Heisler M, Wagner TH. Cost-related medication underuse: do patients with chronic illnesses tell their doctors? Arch Intern Med. 2004;164(16):1749–55.
16 Cummings JR, Lavarreda SA, Rice T, Brown ER. The effects of varying periods of uninsurance on children's access to health care. Pediatrics. 2009;123(3):e411–e418.
17 Van Doorslaer E, Masseria C, Koolman X. Inequalities in access to medical care by income in developed countries. CMAJ. 2006;174(2):177–83.
18 Weissman JS, Stern R, Fielding SL, Epstein AM. Delayed access to health care: risk factors, reasons, and consequences. Ann Intern Med. 1991;114(4):325–31.
19 Epstein AM, Stern RS, Weissman JS. Do the poor cost more? A multihospital study of patients' socioeconomic status and use of hospital resources. N Engl J Med. 1990;322(16):1122–8.
20 Destefano F, Anda RF, Kahn HS, Williamson DF, Russell CM. Dental disease and risk of coronary heart disease and mortality. BMJ. 1993;306(6879):688–91.
21 Madrid C, Abarca M, Pop S, Bodenmann P, Wolff H, Bouferrache K. Oral health: social determinants of a health inequality. Rev Med Suisse. 2009;5(219):1946–51.
22 Janket SJ, Baird AE, Chuang SK, Jones JA. Meta-analysis of periodontal disease and risk of coronary heart disease and stroke. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95(5):559–69.