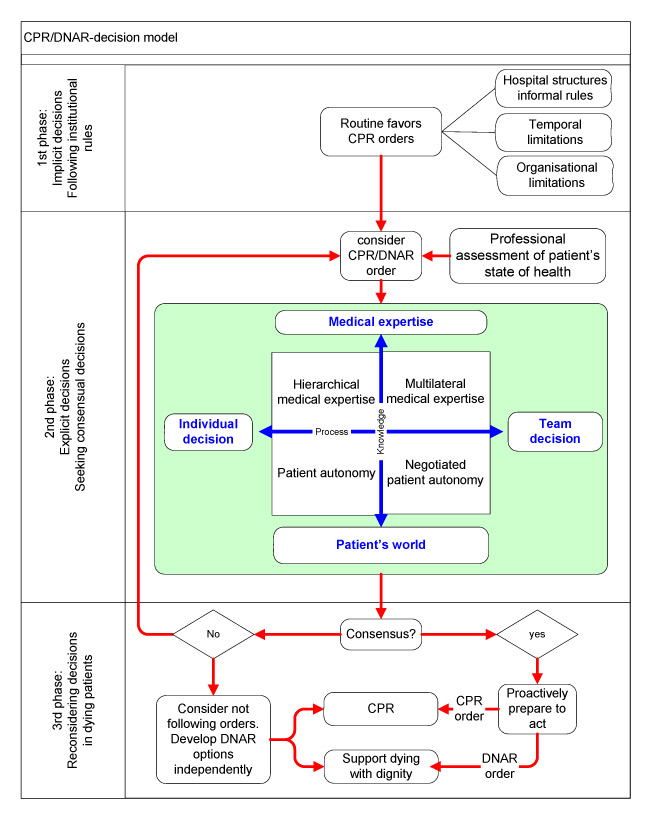
Figure 1
Model of DNAR decision-making.
DOI: https://doi.org/10.4414/smw.2011.13157
A qualitative study
Since the 1980s, “do-not-attempt-resuscitation (DNAR)” orders have become common in medical practice. DNAR orders are given for 50–60% of patients who die a non-sudden death, with wide variations among countries. DNAR orders apply to only 19% of hospitalised patients in Italy, but to as many as 83% in Sweden and 86% in Switzerland [1, 2]. The frequency of DNAR decisions in which competent patients had been involved in the decision is as low as 10% in Italy and as high as 84% in the Netherlands. Several other authors reported strong reluctance on the part of medical professionals to raise the question of potential resuscitation efforts with their patients [3–9]. While U.S. law has long required that consent be given not to undergo cardiopulmonary resuscitation (CPR), neither formal legal regulations nor deontological ethics recommendations on when to proceed with DNAR orders existed until 2000 [10]. The physicians’ and nurses’ associations of the UK were the first Europeans to publish mutual national guidelines on DNAR order enactment in 2001 [11]. In Switzerland, the Swiss Academy of Medical Sciences very recently published guidelines on how DNAR decisions should be made and how patients and next of kin should be involved in the decision-making process [12]. These current guidelines advocate explicit discussion of DNAR orders with all competent patients and/or their relatives, unless there is an obvious reason why this would not be in the patient’s best interests. Yet, in daily clinical practice, patient involvement, specific professional responsibilities and communication between professionals regarding DNAR orders remain a major challenge [13–15]. The particularity of DNAR orders is that they anticipate what should be done or omitted in the event of unexpected cardiopulmonary arrest (CPA), and that these anticipating orders are obviously based on hypothetical facts and scenarios, without knowing the time or circumstances when CPA will occur and what the outcome of CPR will be. It is thus a very difficult and ambitious task to obtain true, informed consent for DNAR orders. On the other hand, there is a high incidence of conflicting judgement with regard to the expected quality of life, burden of illness, and social well-being between potential candidates for DNAR and their physicians [16–21]. Patient autonomy notwithstanding, this finding underlines the importance of the patient’s involvement in the DNAR decision-making process.
International guidelines further state that DNAR orders should include the coordinated expertise of interdisciplinary teams. Observations by nurses may be crucial and the importance of their input in the decision-making process is increasingly recognised. However, nurses still report frequent exclusion from CPR decisions [22].
There are very few data on the DNAR decision-making process in clinical practices that highlight the attitudes of physicians and nurses towards the involvement of other professionals and patients, the agreement and disagreements in the decision-making process and their consequences. We therefore decided to use qualitative research methodology, specifically Grounded Theory, to explore physicians’ and nurses’ preferences, attitudes and practices with regard to DNAR decisions, to identify the most important factors influencing the decision-making process, to analyse decision patterns and to understand the consequences of such decisions in daily work.
One-time open-ended interviews were used to collect data describing the DNAR decision-making process and emphasising meanings, experiences, and the views of physicians and nurses. To explore actual experiences an appropriate sampling strategy was adopted in acute critical care units where DNAR or CPR orders can be assumed to be part of daily practice.
The nurses and physicians working in acute care settings of seven different hospitals with mixed heterogeneous cases in the German-speaking part of Switzerland (cantons of Zurich and Central Switzerland) were approached. Hospitals and wards were selected so as to include medical, surgical, emergency and ICU wards in teaching and non-teaching, rural and urban settings (table 1). During an information session we explained the goals of the study to the staff, answered their questions, and then invited them to participate. Participation was voluntary. Participants were contacted by phone and the interviews were scheduled at places and times convenient to them. Before the interview all participants gave informed consent to have their interview recorded on tape. The open-ended, face-to-face interviews allowed the physicians and nurses to describe their experiences and general reflections on DNAR orders. All interviews were conducted by the third author, who also recorded the impressions arising from each interview and possible further questions for forthcoming interviews.
The content of the interview was accompanied by a short topic guide including questions asking for explanation of actual daily practice, for narratives of good experiences with the decision-making process in relation to resuscitation orders and for attitudes to collaboration with other professionals, patients and family members. As the categories and themes emerged in the course of the study the topic guide was expanded to include the consequences of the orders according to the decision-making process. The study was approved by the local ethics committees of Zurich und Lucerne and in accordance with the Helsinki Declaration.
The goal of this qualitative study with a Grounded Theory approach was to capture possible patterns and variation in the social process of resuscitation orders [23, 24]. It was assumed that the accounts of approximately 60 nurses and 60 physicians would be needed for data saturation (table 2).
| Table 1: Work setting of participants (n = 92). | |||
| Total n = 92 | Nurses n = 52 | Physicians n = 40 | |
| University hospital | 42% | 23% | 8% |
| Regional hospital | 40% | 29% | 55% |
| Local community hospital | 16% | 46% | 38% |
| Private hospital | 2% | 2% | – |
| Intensive care unit | 32% | 31% | 33% |
| Emergency department | 8% | 3% | 13% |
| Surgical ward | 23% | 25% | 20% |
| Medical ward | 32% | 37% | 27% |
| Other | 5% | 4% | 7% |
| Table 2: Demographic data of participants (n = 92). | |||
| Total n = 92 | Nurses n = 52 | Physicians n = 40 | |
| Median age in years (SD) | 40.9 (9.2) | 38.2 (9.0) | 44.4 (8.3) |
| Median work experience in years/SD (range) | 16.5/9.0 (1–36) | 16.3/9.5 (1–36) | 16.8/8.4 (2–35) |
| Gender: Female | 61% | 87% | 28% |
First, the data from 23 interviews were openly coded sentence by sentence, to categorise the activities and events as well as the conditions and consequences of the DNAR process and their properties. Second, in order to relate categories and their dimensions, the data were analysed by exploring similarities and differences using constant comparison and situational mapping [25, 26]. This axial coding enabled us to describe the structures of the decision-making processes in resuscitation orders, identify the persons involved and the underlying criteria for the decisions. Third, theoretical sampling was used to enhance variability [23–25]. Analysis of additional interviews allowed us to refine, change or confirm the categories developed and enabled us to incorporate more variations in the data. Once no new insights were found through additional interviews, we assumed saturation and stopped collecting data. This was achieved after 69 additional interviews, bringing their total to 92. All were included in the analysis. At this stage the analysis included 4942 relevant quotes from which 58 categories were built as main elements of the decision process. All categories had to be underlined by several quotes. From the categories a model of three decision-making phases and patterns of decision-making was developed by the first, second and third authors. Considerable efforts were made to confirm that the findings reflected the participants’ experiences. In addition to the discussion with all members of the research team and other experienced qualitative researchers, the emerging model was presented and discussed with physicians and nurses from three of the participating hospitals. They deemed the model to mirror their experience well.
Many participants reported that discussing possible DNAR orders with patients was an extremely delicate matter but a necessary/indispensable professional task. They emphasised the importance of professional experience and of senior physicians as role models. “No one becomes a senior physician overnight, and no one learns how to make a decision pertaining to DNAR orders overnight either.” Less experienced physicians and nurses saw heads of department and senior physicians as a valuable “backup system.” They appreciated their medical counsel, their presence as mediators in conflicts and their function as role models during patient encounters. Physicians and nurses alike reported the necessity of advanced social skills and the ability to reflect on core issues such as a patient’s life situation and the limitations of medical treatment. Thus most professionals advocated giving DNAR orders high priority and having the discussion led by the most experienced and respected professionals. In the opinion of a physician, “The highest priority needs to be given to DNAR orders. It’s the responsibility of the chief physician... This isn’t a task for a resident.”A nurse added, “Nurses should participate. But a lot of clinical experience is needed to do so.”
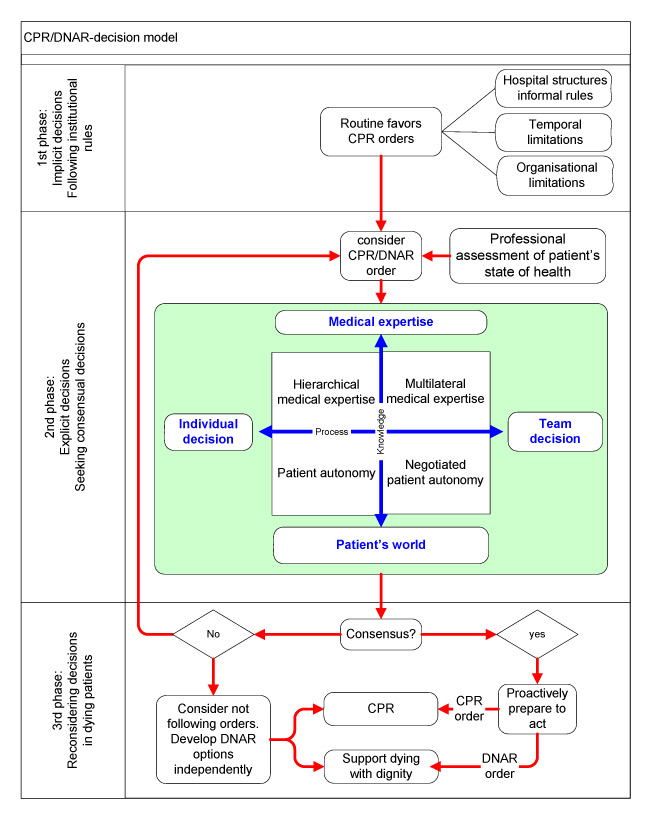
Figure 1
Model of DNAR decision-making.
Decisions on CPR/DNAR were not described as discrete events but as cascades of decisions and actions. The contribution of different healthcare professionals, the range of professional experience, anticipated health outcome, interactions with patients and families and institutional rules produced a variety of decision processes. The descriptions by the participants showed that CPR/DNAR decisions are the product of three distinct decisional phases: 1) the phase of implicit decision, 2) the phase of explicit decision, and 3) the phase of reconsidering decisions.
The implicit decision is regulated by institutional rules, generally representing institutional orders in favour of CPR and rarely tailored to the specific situation of individual patients. Typically, such implicit decisions were valid in emergency rooms, during the first 24–48 hours of hospitalisation in intensive care units, and regularly used on surgical wards. A nurse said, “It doesn’t matter whether the patient is 95 years old, lives in a nursing home, or complains about his or her health. This “yes”[in favour of CPR] will remain for at least 48 hours after surgery.”Participants argued that in the phase of implicit decision, the focus was on diagnostic and therapeutic procedures and often only medical facts were at the staff’s disposal. Pertinent information about a patient’s personal situation and his/her wishes and preferences was not available and/or was not considered to be important at that time.
Most physicians and nurses emphasised the temporary nature of implicit decisions and judged that they should be reconsidered as soon as possible. Willingness to make a decision explicit through discussion and reflection differed among the wards. Whereas CPR/DNAR orders were discussed on a daily basis in most intensive care units, reluctance to consider new orders was remarkable on surgical wards. The explicit decision process consisted in seeking consensual decisions on CPR/DNAR orders. This process typically started when the patient’s condition led the healthcare professionals to question the implicit decision. Nurses repeatedly described the considerable efforts required on their part to obtain explicit, written CPR/DNAR orders when a patient’s state of health was deteriorating. Many physicians were aware of the nurses’ role in this process: “Normally, nurses are the ones who challenge us to make explicit decisions[on DNAR orders]when the patient’s state of health worsens or when they expect deterioration.”Physicians and nurses reported that discussions were typically started when nurses 1) noticed a patient’s increasing level of pain; 2) observed that a patient’s state of health was worsening despite therapeutic interventions; and 3) had learned how a patient viewed his/her health and illness and/or his/her preferred course of action (or those of his/her next of kin) in the event of CPA.
Once the adequacy of the implicit order was questioned, evaluation of an explicit DNAR order started within the teams. For this evaluation, on the one hand, physicians as well as nurses relied on “hard facts” such as medical, disease-centred knowledge to justify their decision. On the other hand, they considered “soft facts” such as the patients’ outlook on the world, their experience with the illness, their suffering, the impact on their quality of life and social connections with families and friends. These elements were regarded as individual-centred knowledge of the patients and their next of kin’s everyday world. The healthcare professionals reported that these different types of information were weighed and combined in various ways depending on the professionals’ role, power and experience, translated in a continuum between “an individual’s decision” and “a team decision” on the one hand, and between an everyday world-centred and a medical prognosis-centred decision on the other. This essentially results in four patterns of consensus pursuit and decision-making for explicit orders: 1) hierarchical medical expertise, 2) multilateral medical expertise, 3) patient autonomy, and 4) negotiated patient autonomy.
This pattern represents decisions made exclusively by one physician, providing the medical rationale for the decision, be it a DNAR order or an order in favour of CPR. It is based on the deciding person’s professional hierarchical status and the mutual acceptance of this status by nurses and fellow physicians. This type of unilateral decision-making represented a consensus in unambiguous situations such as multimorbid patients with incurable disease (DNAR) or young patients with a curable disease (in favour of CPR). As a physician said,“I would say 99.99% would agree with CPR in this situation. No discussion is needed in those cases.”
This pattern consisted in decision-making based on broad medical expertise. In complex situations especially, the opinions of team members were sought, discussed and negotiated to reach a consensus. In the words of a physician, “If we feel that a patient with let’s say severe head trauma will not recover, and consider that a DNAR decision is appropriate, the physicians from neurology, neurosurgery and ICU will decide collectively.” ICU nurses were reported to participate in such team discussions regularly. In this pattern, patients and their next of kin were rarely involved in the decision and were only occasionally informed of DNAR orders. When patients or relatives disagreed with such a decision, the professionals tried to convince them. The opinion of a physician: “It is necessary to state the medical facts. If the patient does not agree, we have to explain the consequences to him or her.”
In this pattern, nurses and physicians rated the patients’ wishes and preferences higher than anything else. A nurse stated, “If the patient is aware of the consequences once we have explained everything, then it is his or her decision. It is not my duty to qualify this decision.” A physician said, "DNAR orders cannot be the decision of the professional team or, worse, one person, except the patient himself.”
Professionals highly respectful of the patients’ wishes regretted the paucity of advance directives. Physicians thought that directives “are helpful because then we know that patients have thought about these situations,” or, “We know there is a directive, so we can compare our medical conclusion with it.”
In this pattern, a patient’s opinions and wishes were considered to be important to the decision; however, his or her autonomy was restricted in the sense that he or she was confronted with medical/scientific considerations and that the patient was considered one among the various partners in the negotiation process. A nurse reported, “This is how the group likes to proceed: The physicians, the nurses, the patient and the relatives (if they want to be involved or if the patient wants them to be involved) assess the situation and decide as a group, weighing each participant’s arguments.”The content of advance directives was questioned with arguments such as: “It is problematic when[the directives] are outdated and when statements are so general that they don’t help us to decide in the patient’s best interests.”
Any of the four patterns of explicit orders described above could represent a consensus or provoke disagreement or even a conflict, depending on the concrete situation and the persons involved. The most serious and most frequent disagreements were described when a physician acted exclusively on his or her authority (pattern one) and collaborators thought that the subject should have been discussed within the interdisciplinary team and/or with the patient/next of kin. Participants stated that sometimes professionals were caught up in “who-has-the-power-to-decide” arguments, with discussions ending in trench warfare between nurses and physicians. In these situations, interdisciplinary teamwork put in question by negative emotions and stereotypes such as “nurses are too emotional to decide“or “physicians know the results of diagnostic tests; nurses know the patients.”
On the other side of the spectrum, well-accepted decisions typically combined profound, mutually respected medical and nursing expertise, communication and negotiation skills, common sense and life experience coupled with empathy for patients and colleagues. As a physician who was the head of department stated, “I appreciate physicians with a feeling for human beings, for colleagues and patients: educated physicians – educated in the sense of having a fine grasp on personhood.”Experienced professionals with well-developed professional and social skills were described as being able to pragmatically move back and forth between the four patterns, depending on the situation.
The fact that the decision in favour or against CPR was or was not the result of a team consensus had practical consequences. Consensual decisions were accepted even when they contradicted personal opinions.“Acting professionally as a nurse comes natural to me, even if I personally do not agree with the CPR decision. We work together and decide together on how to proceed for the good of the patient.”
Non-consensual decisions, however, were prone to involve team conflicts and non-compliance. In cases of dissent the nurses in particular felt heavily burdened and often insisted on further discussion, hoping to achieve consensus after all. In order to clarify the situation, they first sought to have the order reconsidered by using the following strategies: Collecting additional facts pertaining to their patients before re-initiating the discussion; waiting until another physician was on duty; asking the head of department to change the orders; or encouraging the patients and/or their relatives to discuss the matter with the attending physician. Occasionally there were situations when the nurses’ input was simply not heard. In such instances they considered disobeying the existing orders, either openly or secretly. Sometimes an entire team chose to disobey the order and refused to initiate resuscitation procedures if CPA were to occur: “The resident as well as the nurses did not agree with the decision of the head of department. We decided not to act in the event of CPA. That was a collective decision.”Such situations were stressful for all those involved and had dysfunctional long-term effects on the teams.
As nurses felt they were the closest to the patients, the most knowledgeable about their needs and most able to detect minor changes in their condition, they felt it was their right and duty to question CPR decisions frequently. They considered that professional performance should always include the critical appraisal of every situation. One physician alluded to a legal issue, “If there is a CPR/DNAR order written down and they[the nurses] do not follow it, they will be in trouble. Thus, there is nothing to consider, it’s just not acceptable.” Physicians as well as nurses emphasised that nurses are at the forefront of patient care and normally the first to execute CPR or to withhold it in the event of DNAR orders. Their adherence or non-adherence to orders for or against CPR is therefore pivotal for the fate of the patient.
CPR/DNAR orders also led participants to reconsider direct patient care. The nurses directly took CPR/DNAR orders into consideration when planning their activities with regard to the intensity of observation and monitoring. Said one nurse, “I am more aware of the degree to which this patient’s health is at risk [with confirmed CPR orders].” Furthermore, DNAR orders did not have the same meaning for all interviewees. Most physicians tended to understand DNAR orders purely as “not undertaking CPR in case of CPA.” Some nurses viewed DNAR orders as a new phase in a patient’s life when his/her state of health deteriorated and involved measures of palliative care in order to guarantee the patient’s dignity. A nurse stated, “DNAR has something to do with dignity. I remember a woman who died after CPR on her way to the ICU. It was terrible to witness her dying this way, without any dignity.” Certain physicians acknowledged the link between the nurses’ palliative care and CPR/DNAR orders. Alluding to dignity, one physician said, “DNAR allows passing away with dignity, without chemotherapy and all that stuff, painlessly and fast. It’s my obligation to make people aware of this possibility. Unfortunately, whether it can happen or not depends on the physician.”
To our knowledge this is the first study to analyse the decision-making process pertaining to CPR/DNAR orders and to explore the views of nurses and physicians who work in various acute care settings [27]. Most healthcare professionals stated that establishing DNAR orders in the best interests of the patient is a challenging task that needs professional, human and relational expertise and that should not be left to junior physicians. Fundamentally there are two types of decision, implicit and explicit ones; the implicit decisions follow institutional rules, the explicit ones result from 4 patterns of decision-making. Implicit and explicit decisions potentially represent a consensus. Achieving a consensual decision is crucial, whereas the negotiation process by which the consensus is reached is less important. Non-consensual decisions lead to non-compliance and provoke conflicts, be it on the personal or team level. The meaning of a DNAR order is not unequivocal and definite among all healthcare workers. DNAR orders have direct implications for patient care.
The study revealed the central importance of negotiation and consensus. By analysis of the open-ended interviews it was possible to formulate a decision model consisting of three decision phases, as illustrated in the figure and described in detail in the results section. Experienced professionals with well-developed professional and social skills were described as being able to move back and forth pragmatically between phases and patterns, depending on the situation. Whatever the predominant pattern, the key element for satisfaction and compliance with the decision was that the decision process had been interdisciplinary and consensual, integrating the nurses’ observations and views. A consensus did not mean that all team members had to share the same opinion, but that the expertise and perspectives of different members of the team had become part of the decision. The presence or absence of consensus therefore conditioned phase 3. If a consensus was reached, the nurses adapted their care plan, putting more emphasis on patient safety when an order in favour of CPR had been given, as opposed to more emphasis on patient comfort when a DNAR order had been issued.
A finding we consider important is that nurses and physicians alike stated that in some situations, DNAR orders influenced the delivery of nursing care as they shifted its focus. The statements in phase three show that DNAR orders made it possible to emphasise palliative nursing interventions, to maintain closer contact with relatives and allow the patient a dignified end, but in no way to “hasten that end,“ as described by other authors [28–30]. A DNAR order did not imply “restricted nursing care” or, in extreme cases, “no nursing care” [31]. Although the intention and necessity to keep DNAR orders strictly separate from other treatment plans was broadly accepted among participants, they emphasised the difficulty of separating them in some cases. Participants from ICUs reported that they differentiated among orders ranging from DNAR to full CPR, comprising as many as four different levels of advanced life support such as mechanical ventilation or vasopressor support. They emphasised that these levels ease customisation of individual treatment plans but heighten the difficulties experienced by many participants in unambiguously isolating the kind of treatments that are exclusively associated with near death or CPA. The quote of a physician, “DNAR allows passing away with dignity, without chemotherapy and all that stuff, painlessly and fast” illustrates particularly well the confusion which may exist between the decision against active treatment of an incurable disease and the decision not to intervene in the event of CPA, i.e. a DNAR decision. Several authors have shown that the treatment of patients with DNAR orders in terminal care was significantly limited [30], and up to 6.5% of physicians and 15% of nurses considered certain interventions inappropriate when combined with DNAR orders [29]. The recommendations on DNAR orders by the Swiss Academy of Medical Sciences and the British Medical Association both state that neither DNAR orders nor DNAR intentions expressed by patients should influence medical treatment or care [12]. They allude to potential treatment restrictions that are not in relation to near death or CPA. We deem it important to underline that for dying patients with DNAR orders, it may be appropriate to limit other active treatment options (e.g., antibiotics, transfer to ICU), while this should not be the case for patients not suffering from an incurable disease.
Our findings also showed that if there was no consensus nurses had a more marked tendency than physicians to stimulate reconsideration of the order established, moving back to phase 2. When team members felt that their opinion was not taken seriously, they sometimes considered non-compliance.
Our findings are in accordance with literature data indicating that nurses would not start CPR on a substantial number of patients regardless of their DNAR status [22]. This non-compliance deserves special attention, given that choosing not to attempt CPR is a straightforward clinical decision with immediate consequences that raise ethical and legal concerns. Furthermore, non-compliance within the healthcare team can raise conflicts on the team level as well as the individual level, and can lead to long-term dysfunction and even burn-out [32]. Moreover, we were able to establish for the first time that non-consensual decision-making is the principal cause of such non-compliance. Recognising a non-consensus should encourage the optimisation of the doctor-nurse relationship and, in turn, urge them to seek a consensus, all of which results in better healthcare practices.
Official guidelines recommend that the clinician in charge with the most seniority, ideally a consulting physician, the GP or an experienced nurse, should decide on CPR/DNAR orders [33]. As in other studies [34], our findings showed that the realities of daily clinical practice often preclude compliance with such recommendations, and that young interns and residents are often responsible for DNAR orders. This can be explained by the way work is organised in Swiss public hospitals: junior physicians are usually the first and principal discussion partners of patients and next of kin, and it is they who write most of the medical orders. Nevertheless, the participants in our study stressed that in their opinion the most experienced healthcare professionals should be responsible for decisions in favour or against CPR, and that this would guarantee good clinical practices. Young staff members, head nurses and chief physicians alike confirmed this standpoint, emphasising the need not only for profound medical and/or nursing expertise, but also for life experience and social skills. Contrary to junior physicians and nurses, senior physicians and experienced nurses were described as being able to grasp the clinical situation rapidly, to reach a progressive understanding of the patient’s history and response patterns, and to integrate all of these components as basic elements in their clinical judgment. Our findings therefore support the claim for senior leadership in British and Swiss recommendations. Obviously, however, major educational efforts are needed to translate these claims and profound convictions into everyday practice. Senior leaders can lead the discussion after listening to and disseminating narratives of shared practice that can open up common ground for all involved parties, allowing them to reinterpret and learn from each other’s experiences [35, 36]. The model presented may itself make it easier for practitioners to reflect on their own practice and patient care [37, 38].
Our study involved respondents in a limited number of care settings and was limited to the German-speaking part of Switzerland. The study may therefore lack important structural and cultural diversity. Future studies should be undertaken in other care settings and cultural environments.
This Grounded Theory study made it possible to develop a DNAR decision model. The model emphasises the coexistence of implicit and explicit decisions as well as the consequences of such decisions. It shows that reaching consensual decisions is crucial and that non-consensual decisions open the door to individual counter-decisions that may imperil professional integrity and the patients’ needs. CPR/DNAR decision-making requires high social skills and profound medical and nursing expertise. Hence leadership by experienced senior physicians and nurses is needed. They can be the expert coaches on the wards who initiate reflection and discussion on ethical issues, and can also counsel residents and nurses in decision-making and consensus formation. To improve the DNAR decision-making process calls for a major effort in favour of multidisciplinary education.
The study was funded by the Käthe-Zingg-Schwichtenberg Fund (Swiss Academy of Medical Sciences) Researchers were independent of the funding entity.
1 Aune S, Herlitz J, Bang A. Characteristics of patients who die in hospital with no attempt at resuscitation. Resuscitation. 2005;65(3):291–9.
2 van Delden JJ, et al. Do-not-resuscitate decisions in six European countries. Crit Care Med. 2006;34(6):1686–90.
3 Vetsch G, Uehlinger DE, Zuercher-Zenklusen RM. DNR orders at a tertiary care hospital – are they appropriate? Swiss Med Wkly. 2002;132(15–16):190–6.
4 Chevrolet J. L’ordre “not to be resuscitated” (NTBR) chez l’adulte et chez l’enfant et Avis du Conseil d’éthique clinique des HUG. Médecine&Hygiène. 2003: p. 775–85.
5 Hofmann JC, et al. Patient Preferences for Communication with Physicians about End-of-Life Decisions. Ann Intern Med. 1997;127:1–12.
6 Levin JR, et al. Life-sustaining treatment decisions for nursing home residents: who discusses, who decides and what is decided? J Am Geriatr Soc. 1999;47(1):82–7.
7 Meisel A, Snyder L, Quill T. Seven legal barriers to end-of-life care: myths, realities, and grains of truth. JAMA. 2000;284(19):2495–501.
8 Morrison RS, Morrison EW, Glickman DF. Physician reluctance to discuss advance directives. An empiric investigation of potential barriers. Arch Intern Med. 1994;154(20):2311–8.
9 Richter J, Eisemann MR. Attitudinal patterns determining decision-making in the treatment of the elderly: a comparison between physicians and nurses in Germany and Sweden. Intensiv Care Med. 2000;26(9):1326–33.
10 American Heart Association and International Liaison Committee on Resuscitation, Guidelines for cardiopulmonary resuscitation and emergency cardiovascular care: An international consensus on science. Resuscitation. 2000;46:3–430.
11 British Medical Association, Royal College of Nursing, and Resuscitation Council (UK) (2007) Decision relating to cardiopulmonary resuscitation. A joint statement from the British Medical Association, the Resuscitation Council (UK) and the Royal College of Nursing.
12 Schweizerische Akademie der Medizinischen Wissenschaften, Reanimationsentscheidungen. Medizinisch-ethische Richtlinien und Empfehlungen. 2008, SAMW: Basel.
13 Burns JP, et al. Do-not-resuscitate order after 25 years. Crit Care Med. 2003;31(5):1543–50.
14 De Gendt C, et al. Do-not-resuscitate policy on acute geriatric wards in Flanders, Belgium. J Am Geriatr Soc. 2005;53(12):2221–6.
15 Ebrahim S. Do not resuscitate decisions: flogging dead horses or a dignified death? Resuscitation should not be withheld from elderly people without discussion. BMJ. 2000;320(7243):1155–6.
16 Junod Perron N, Morabia A, A. de Torrente. Quality of life of Do-Not-Resuscitate (DNR) patients: how good are physicians in assessing DNR patients’ quality of life? Swiss Med Wkly. 2002;132(39–40):562–5.
17 Ebell MH, et al. Survival after in-hospital cardiopulmonary resuscitation. A meta-analysis. J Gen Intern Med. 1998;13(12):805–16.
18 Eliasson AH, et al. Do-not-resuscitate decisions in the medical ICU: comparing physician and nurse opinions. Chest. 1997;111(4):1106–11.
19 Layde PM, et al. Surrogates’ Predictions of Seriously ill Patients’ Resuscitation Preferences. Arch Fam Med. 1995;4:518–24.
20 Phillips RS, et al. Choices of Seriously Ill Patients About Cardiopulmonary Resuscitation: Correlates and Outcomes. Am J Med. 1996;100:128–37.
21 Seckler AB, et al. Substituted Judgment: How Accurate Are Proxy Predictions? Ann Intern Med. 1991;115:92–8.
22 De Gendt C, et al. Nurses’ involvement in “do not resuscitate” decisions on acute elder care wards. J Adv Nurs. 2007;57(4):404–9.
23 Strauss A. Qualitative analysis for social scientist. 1987, Cambridge: Cambridge University Press.
24 Strauss A, Corbin JM. Basic of qualitative research: Techniques and procedures for developing Grounded Theory. 1998, Thousand Oaks, CA: Sage.
25 Charmaz K. Constructing grounded Theory: A practical guide through qualitative analysis. 2006, London: SAGE.
26 Clarke A. Situational analysis: Grounded theory after the postmodern turn. 2004, Thousand Oaks: SAGE.
27 Robinson F, Cupples M, Corrigan M. Implementing a resuscitation policy for patients at the end of life in an acute hospital setting: qualitative study. Palliat Med. 2007;21(4):305–12.
28 Naess M. “Do-Not-Attempt-Resuscitation”-orders in ICCUs: A survey of attitudes and experiences of nurses in Norway. Intensive Crit Care Nurs. 2008.
29 Smith GB, Poplett N, Williams D. Staff awareness of a “Do Not Attempt Resuscitation” policy in a District General Hospital. Resuscitation, 2005;65(2):159–63.
30 Holzapfel L, et al. A four-step protocol for limitation of treatment in terminal care. An observational study in 475 intensive care unit patients. Intensive Care Med. 2002;28(9):1309–15.
31 Fields L. DNR does not mean no care. J Neurosci Nurs. 2007;39(5):294–6.
32 Meltzer LS, Huckabay LM. Critical care nurses’ perceptions of futile care and its effect on burnout. Am J Crit Care. 2004;13(3):202–8.
33 British Medical Association, The Recuscitation Council (UK), and Royal College of Nursing. Decisions relating to cardiopulmonary resuscitation. A joint statement from the British Medical Association, the Resuscitation Council (UK) and the Royal College of Nursing. 2007 [cited 2008 December 26th]; Available from: http://www.bma.org.uk .
34 Butler JV, et al. Improving decision-making and documentation relating to do not attempt resuscitation orders. Resuscitation. 2003;57(2):139–44.
35 Giacomini MK, Cook DJ. Users’ guides to the medical literature: XXIII. Qualitative research in health care B. What are the results and how do they help me care for my patients? Evidence-Based Medicine Working Group. JAMA. 2000;284(4):478–82.
36 Giacomini MK, Cook DJ. Users’ guides to the medical literature: XXIII. Qualitative research in health care A. Are the results of the study valid? Evidence-Based Medicine Working Group. JAMA. 2000;284(3):357–62.
37 Mahrer R, Imhof L. Pflegegeschichten – Erfahrungslernen im pflegerischen Alltag, in Pflege lehren und lernen: Pädagogische und fachdidaktische Impulse zur Ausbildung im Gesundheitswesen, WE’G Weiterbildungszentrum für Gesundheitsberufe, Editor. 2004, h.e.p.: Bern. p. 53–63.
38 Benner P, Tanner CA, Chesla CA. Expertise in nursing practice. 1996, New York: Springer.