The FIRE project
DOI: https://doi.org/10.4414/smw.2011.13142
Summary
QUESTIONS UNDER STUDY/PRINCIPLES: Research is scarce where most patients are found [1]. One of the main reasons is the difficulty in extracting data from traditionally conducted paper-based medical records. Thus, until now most existing patient records have originated from invoicing-tools. Endeavours to truly reflect a doctor’s consultation have been rare. FIRE (Family Medicine ICPC-Research using Electronic Medical Records) is an ambitious project to establish a proper knowledge base in primary care by using the ongoing implementation of EPR (electronic patient records). FIRE will enable many questions on epidemiology and performance within the PC (primary care) setting to be answered.
METHODS: GPs (general practitioners) throughout Switzerland working with EPR were eligible for participation. Workshops were held to train and standardise ICPC-coding (International Classification of Primary Care), a classification system especially designed for the PC-setting. The recorded data included administrative information on the GP and patient, vital signs, ICPC codes, laboratory analysis and medication. Data exporter software was developed for extracting anonymised data automatically from the EPR onto a database for further statistical analysis.
RESULTS: From 1.1.2009 until the beginning of April 2010 24 GPs were successfully recruited providing standardised information on 127922 consultations in 29398 patients and 159956 medical problems according to the ICPC-2 classification.
CONCLUSION: The project proves the feasibility of standardised ongoing collection of research data embedded in routine clinical practice. FIRE provides a unique database for research in PC and highlights the potential of broad implementation of EPR in a PC-setting. Studies resulting from the ongoing project have the potential to assess the quality of care provided by GP’s.
A milestone for research in primary care in Switzerland
Keywords and Abbreviations:
FIRE: Family Medicine ICPC-Research using Electronic Medical Records
ICPC-2: International Classification of Primary Care, second version
ICD-10: International Classification of Diseases
GP: General Practitioner
PC: Primary Care
EPR: Electronic Patient Record
Introduction
In many countries a proper knowledge base on the characteristics of PC (primary care) does not exist, even though computerised PC records are fundamental components for any national health information system [2]. So far, data on PC in Switzerland have mainly originated from invoicing-tools. A majority (87%) [3] of GPs (general practitioners) in Switzerland still solely use paper-based patient records, making data evaluation extremely time-consuming [4] and incomprehensive.
Commonly EPRs (Electronic Patient Records) include administrative patient data, documented vital-signs, medications and laboratory results. Specific elements of the doctor-patient encounter, such as reasons for consultation, medical problems and procedures, are usually filed in free text. This hinders standardised analysis and research. It is therefore crucial to establish a reliable database with an appropriate documentation system that reflects the above mentioned key elements of a patient’s visit systematically. Only one system has been specially designed to meet the needs of PC research as well as of day-to-day practice [5]: The ICPC (International Classification of Primary Care, WONCA (World Organisation of National Colleges and Academics 1987)) [6]. ICPC reflects the essential elements of each doctor-patient encounter and has been accepted by the World Health Organization (WHO) as a system of classification to be used for health information recording in PC [6–7]. In contrast to ICPC, ICD was developed as a coding system for detailed mortality statistics [8] and does not focus on the special context of PC.
The Association of the Swiss General Practitioners declared ICPC-2 as the classification standard for current medical problems in electronic patient documentation [9–12], thus encouraging providers to implement an appropriate ICPC-tool in their EPR-software.
The ongoing FIRE project (Family Medicine ICPC-Research using Electronic Medical Record) aims to embed standardised collection of research data by means of an EPR into routine clinical practice. The aim of this study is to investigate whether the adoption of the ICPC-codes is a feasible means of standardising data from electronic patient records as a research tool in the primary care context. This paper also describes the data structure and first results of the ongoing project. It demonstrates the huge potential of collecting data in PC.
Design/Method
The FIRE Project, an overview
In the year 2009 the project was initiated by two members of the SGAM (Association of Swiss General Practitioners) in collaboration with the Institute of General Practice in Zurich. The data export structure was defined by a study group of the SGAM (SGAM Informatics) and the providers of EPRs were convinced to implement the necessary changes. By the end of 2009, 15 participants were successfully recruited as test users and workshops were held to train ICPC coding. Data collection and data export are continuously optimised and recruitment of new participants is ongoing. This paper reports from the stage of the project, where a continuous influx of data is established thus enabling first systematic analysis. Further important steps will be the development of an import tool with inbuilt quality control mechanisms and the establishment of an “episode of care” discussed below.
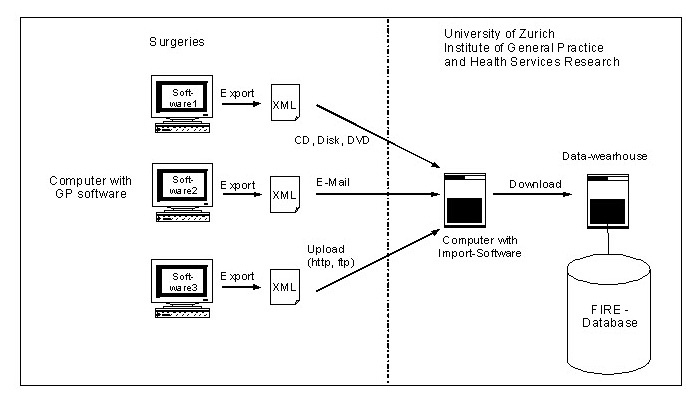
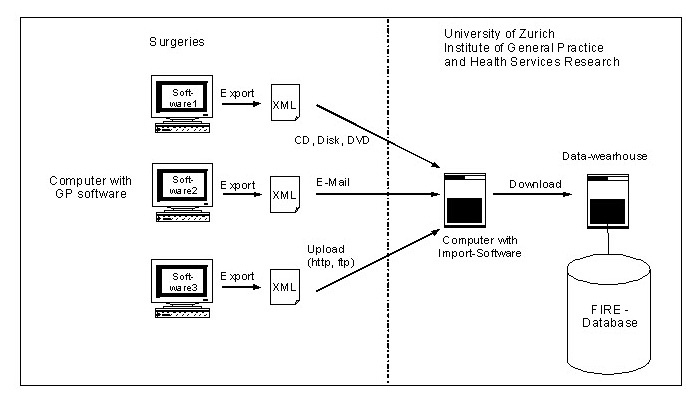
Figure 1
The data transfer structure of FIRE is displayed. Individual EPR data from the GP surgeries are exported using an XML (eXtensible Markup Language) standard, which is independent from any medical software and thus can be processed with the same import software in order to be integrated into the FIRE database. By means of a customised import program, the project manager downloads the XML data periodically, validates for XML-syntax mistakes and feeds the data into the FIRE-database.
Recruiting
GPs throughout Switzerland working with EPR were eligible for participation. Notifications in “PrimaryCare”, the Swiss Journal for GP’s, and direct emailing were used to recruit GP’s [13]. Starting from January 2009, to date 24 GPs are participating in the project.
The basic items of the FIRE-EPR
Participants continuously entered the data of each patient encounter (in practice, home visit or telephone call) into the EPR and saved the data onto the practice computer. Core variables of the FIRE project can be grouped into the following clusters:
– Administrative data: Year of birth, gender, contact date, patient-identification-number consistent of the combined GP and patient identification-number.
– Vital signs: Systolic blood pressure, diastolic blood pressure, pulse, height, weight, waist circumference.
– ICPC-2-Code: Between one and maximally seven codes per contact date as assessed by the GP can be registered.
– Laboratory data: Haemoglobin, leukocytes, C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), creatinin, cholesterol, HDL-cholesterol, LDL-cholesterol, triglycerides, GOT (ASAT), GPT (ALAT), GGT, fasting glucose, HbA1c, prostate-specific antigen (PSA) including their date of analysis.
– Medication data: Medication code (Swiss version of the Anatomical Therapeutic Chemical Classification (ATC)), medication doses, in-take time (morning, noon, evening, night-time), cessation date and comments.
ICPC-Coding
Workshops were held regularly to train and standardise ICPC-coding. A Mediawiki-data-bank was generated to offer the participants a web-based code-book in German and French, combined with a discussion forum for problems occurring while coding [14].
The participants were instructed to code each problem discussed in a consultation with a separate code, thus multiple codings per consultation are possible. This code represents the diagnosis or problem from the doctor’s perspective. If no diagnostic code could be matched, the numbers 1 to 29 of the same chapter could be chosen, representing the leading symptom of the current medical problem.
During the first week of November 2009, a phase of “hot-coding” was launched. For this week the participants were asked to code as comprehensively as possible and to check for missing codings retroactively. In all the other weeks codings were only covered as far as the workload allowed. The idea of the “hot-coding” phase was to evaluate how many diagnoses per consultation actually occur and to be able to compare this phase with routine data collection.
Software, data transfer and security
One of the main concerns of the project was the development of a tool to extract the data from the already existing EPR. Simplified data extraction minimising the additional workload for the GP’s is crucial, otherwise the applicability and utility of EPR data for large-scale research purposes remains limited. Most companies providing EPR software in Switzerland have been convinced by FIRE project leaders to update their products with an exporting tool, enabling the automatic downloading of core FIRE variables from the individual EPR to a central server. The tool enables the GP to provide the data needed for research by pressing a button, thus embedding research in daily clinical routine. Figure 1 illustrates the data transfer architecture.
In line with the Swiss data protection regulations, anonymity is ensured if just birth year, gender and patients’ case number are transmitted. Further analysis of the anonymised data for research purposes is allowed without an explicit consent of the patient. The official Swiss data protection agency approved data transmission and processing procedures (Permit date 5.3.2009).
Assessment of feasibility/practicability
The assessment of the outcome feasibility of the ICPC-coding was done in a qualitative manner: During the regularly held workshops and communication via email and telephone between project leaders and participants, feedbacks on the implementation of the ICPC-coding in routine clinical practice were collected and improvements were implemented as far as technically possible.
Results
By the beginning of April 2010, 24 GPs using 4 different EPR systems were successfully recruited. The participating GPs are predominantly male (79%) and work in a group practice (83%). Their combined mean age is 51 (SD 7.8). Recruited female GPs are on average 9 years younger then their male colleagues. The mean GP working experience is 16 years (SD 9.1). The majority of participants have been using EPR systems for a mean of 3.4 (range 1–7) years. The participant’s practices are located in 8 of the 26 Swiss cantons, all in the German-speaking part of Switzerland.

Figure 2
Number of ICPC-2 codes per consultation (y-axis) of each GP (x-axis). The index shows variation across participants ranging between 0.55 and 1.78 with a mean of 1.31.
They provided standardised information on 127'922 consultations in 29'398 patients and 159'956 medical problems according to the ICPC-2 classification (table 1). The number of patients covered by each GP ranges from 147 to 2625, numbers of ICPC-codes range from 388 to 15640 and consultations from 270 to 15109. The index of ICPC-codes in relation to the number of consultations varied across participants ranging between 0.55 and 1.78 with a mean of 1.31. The variation in index is moderate with a coefficient of variation of 26.9% (SD 0.35) figure 2. The GP with the fewest patients documented is also the GP with the lowest number of ICPC-Codes and consultations, but does not show the lowest index. During the “hot-coding” week the mean index significantly rose to 1.52 ICPC codes per patient visit (p = 0.01, paired t-test). The mean cholesterol and Hba1c are displayed in table 1 and show a low variabilty for the GPs that measured them (cholesterol: range 4.5–5.7, 95% CI 5.1–5.4, Hba1c: range 5.7–8.3, 95%, 95% CI 6.6–7.1).
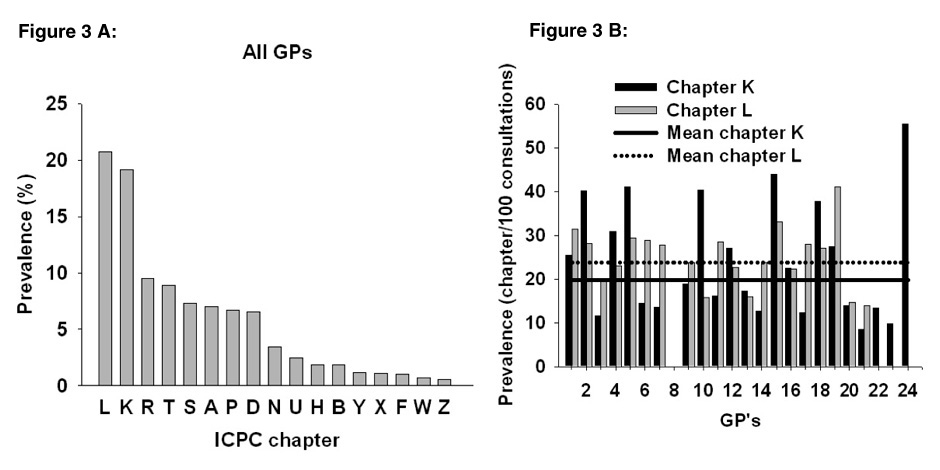
The broad distribution of medical problems according to ICPC-2 chapters is reflected in the wide variability of different diagnoses within the 17 different chapters. Cardiovascular (chapter K) and musculoskeletal (chapter L) were the most prevalent conditions (fig. 3, panel A). To further investigate variability between GPs, we analysed the prevalence of the most common 2 chapters K and L (fig. 3, panel B). The prevalence varied strongly and ranged from 0.01% to 55.5% for chapter K and 0 to 41% for chapter L.
Clinical data included 30'705 instances of blood pressure measurement, 21'905 pulse measurements, 12'596 weights, 8'754 heights and 587 waist circumferences. The most common laboratory analyses were haemoglobin (20'753) and leukocytes (24'205), followed by lipids (triglycerides 10'547, HDL-cholesterol 5'297, cholesterol 4'602, LDL-cholesterol 1'269), Potassium (8'976), CRP (8'535) and glucose (8'566). Liver enzymes (ASAT 7'041, ALAT 6'439, GGT 2'348, ALP 592), ESR (5'778), creatinin (3'036), Hba1c (3'055) and PSA (539) were less commonly measured.
The most commonly noted medications per consultation were Aspirin, Paracetamol, Phenprocoumon, Calcium carbonate combined with Cholecalciferol, Magnesium, Metoprolol, Atorvastatin, Diclofenac, Chondroitin and Budesonid combined with Formoterol.
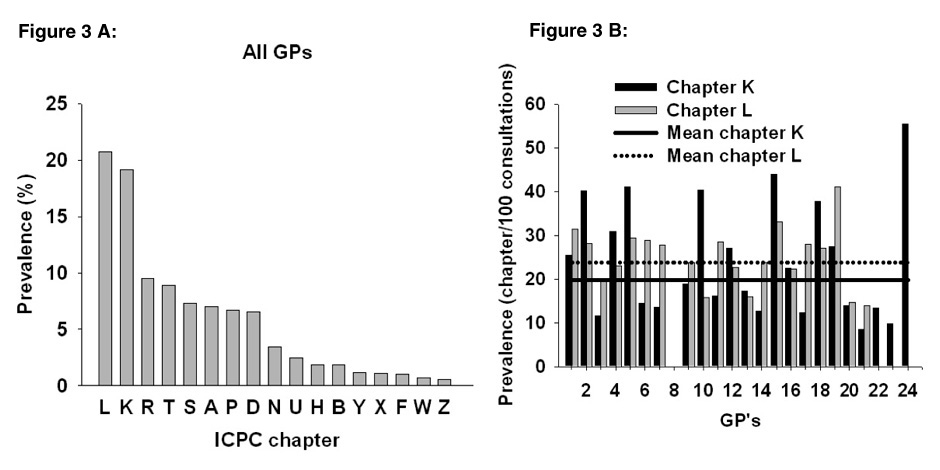
Figure 3
Frequency distribution of medical problems (%) on the y-axis according to ICPC-Chapters (x-axis) that resulted from physician patient encounters.
The ICPC contains 17 Chapters:
– A General and unspecified
– B Blood, blood forming organs, lymphatics, spleen
– D Digestive
– F Eye
– H Ear
– K Circulatory
– L Musculoskeletal
– N Neurological
– P Psychological
– R Respiratory
– S Skin
– T Endocrine, metabolic and nutritional
– U Urology
– W Pregnancy, childbirth, family planning
– X Female genital system and breast
– Y Male genital system
– Z Social problems
Panel A demonstrates the distribution of medical problems in the whole sample (i.e. 24 GP’s representing 29'298 patient contacts and 159'956 codes). Cardiovascular (chapter K) and musculoskeletal (chapter L) were the most prevalent problems.
Panel B shows the prevalence of the most common 2 chapters K and L in % (x-axis) according to GP (y-axis). The prevalence varied strongly and ranged from 0.01% to 55.5% for chapter K (mean 19.88%) and 0 to 41% for chapter L (mean 23.71&).
During the regularly held workshops and communication between project leaders and participants different types of feedback on the implementation of the ICPC-coding in routine clinical practice could be collected: the obvious additional effort of coding and the necessary training were reported as a negative characteristics. Nevertheless the overwhelming majority of feedbacks were extremely positive, concluding that the additional effort is justified. The prevailing opinion was that ICPC can be coded easily through the technical solutions provided by FIRE and is much more sensible for primary care than existing coding systems. Arterial hypertension, hypertension and elevated blood pressure now have one clearly defined code. ICPC provides a clear structure for diagnoses and constitutes an immense alleviation when GPs convert from paper based medical records to EMRs. After implementation of the coding the participants were amazed by how much they actually accomplish within a consultation of 15 minutes and that ICPC reflects their own performance. The fact that ICPC enables a benchmarking tool between the collective of GPs, a quality control tool for primary care, as well as a basis for research make the additional effort even more acceptable.
|
Table 1: Number of patients, ICPC-2-Codes, number of consultations per participant, ICPC to consultation index, ICPC to consultation index during the “hot-coding” week, Hba1c and cholesterol measurements. |
|
Doctor
|
Number of Patients
|
Number of ICPC Codes
|
Number of Consultations
|
Index ICPC to Consultation
|
Index ICPC to Consultation “Hot”
|
Mean Hba1c
|
Mean
Cholesterol
|
| 1 |
1442 |
10143 |
7743 |
1.30 |
1.40 |
7.49 |
5.33 |
| 2 |
1206 |
13111 |
8451 |
1.55 |
2.30 |
6.36 |
|
| 3 |
643 |
1989 |
2178 |
0.91 |
0.88 |
6.72 |
5.52 |
| 4 |
1709 |
10081 |
8737 |
1.15 |
1.72 |
7.16 |
5.50 |
| 5 |
1685 |
14245 |
9785 |
1.45 |
1.48 |
7.34 |
5.30 |
| 6 |
1930 |
8583 |
9684 |
0.89 |
0.80 |
7.10 |
5.43 |
| 7 |
2139 |
9558 |
8936 |
1.06 |
1.20 |
5.87 |
5.22 |
| 8 |
1212 |
4280 |
3276 |
1.30 |
1.65 |
5.70 |
5.44 |
| 9 |
2056 |
10012 |
7939 |
1.26 |
1.32 |
6.72 |
5.18 |
| 10 |
2490 |
13012 |
9505 |
1.36 |
|
6.95 |
5.51 |
| 11 |
2355 |
9944 |
8913 |
1.11 |
1.57 |
6.89 |
5.56 |
| 12 |
512 |
2202 |
1455 |
1.50 |
1.66 |
6.95 |
5.01 |
| 13 |
548 |
2561 |
1438 |
1.78 |
|
6.68 |
5.01 |
| 14 |
865 |
3372 |
2448 |
1.37 |
1.42 |
7.27 |
5.32 |
| 15 |
1037 |
10180 |
5847 |
1.74 |
2.72 |
6.70 |
5.25 |
| 16 |
488 |
1560 |
1208 |
1.21 |
|
6.91 |
5.00 |
| 17 |
2625 |
15640 |
15109 |
1.03 |
0.69 |
|
|
| 18 |
1049 |
7506 |
4507 |
1.66 |
1.94 |
6.79 |
|
| 19 |
1359 |
8574 |
7178 |
1.19 |
1.72 |
6.89 |
4.51 |
| 20 |
147 |
388 |
270 |
1.43 |
|
7.44 |
5.33 |
| 21 |
284 |
574 |
460 |
1.24 |
|
8.34 |
5.01 |
| 22 |
311 |
765 |
528 |
1.44 |
|
|
|
| 23 |
375 |
746 |
648 |
1.15 |
|
|
|
| 24 |
931 |
930 |
1679 |
0.55 |
|
|
|
|
Mean (SD)
|
|
|
|
1.31 (0.35)
|
1.52 (0.52)
|
6.91 (0.57)
|
5.24 (0.26)
|
|
Total
|
29'398
|
159'956
|
127'922
|
|
|
|
|
Discussion
The project has proven the feasibility of standardised ongoing collection of research data embedded in routine clinical practice. As soon as the maintenance of a problem-list according to ICPC becomes routine, practically no additional effort arises from participating in the project. The vision of data collection at the touch of a button has come within reach, even in a country with virtually no standardised patient record keeping [15]. FIRE provides a unique database for research in PC and highlights the potential of the broad implementation of EPR in a PC-setting.
The FIRE-project was developed following the example of the CONTENT-Project in Germany [16]. The principle of creating a database over EPRs is the same, with some project specific differences. FIRE was initiated by “SGAM informatics”, a study group of the Swiss Association of GPs. This initiative reflects an intrinsic desire of the participants to be part of a data-pool representing their own performance. The German project was initiated by the University of Heidelberg and participants were recruited only from the city. In Germany, only one software company developed a software system for data export, whereas in Switzerland the companies generated their own solutions, in order to offer participation to all GP’s interested in the project independently of their EPR system. The main difference between the two projects relates to the implementation of the “episode of care”. In the current phase of the FIRE project only problem codes were recorded, thus solely the doctor’s view of the consultation without the reason for encounter (patient’s view) is currently represented. In contrast, the German project contains the complete “episode of care” structure over time, including reasons for consultation from the patient’s perspective, problems and diagnoses in the GP’s view, decisions and action plans followed over the course of a medical problem [7, 19–20]. The implementation of these missing elements is planned in the FIRE project, but adequate software solutions still have to be developed and participants have to be trained accordingly.
At this stage of the project different limitations have to be taken into account. The fact that only 13% [3] of doctors in Switzerland use an EPR and only a small proportion of these are participating in the project (n = 24) raises questions about the generalisability of the clinical data. However, we found similar frequency distributions of medical problems according to ICPC-2 chapters in German GP data collection [17] with a peak in chapters K and L, showing that patients treated by “selected” FIRE participants are likely representative for the PC setting with regard to morbidity. In addition, gender and age distribution compared well with the annual statistics on GPs performed by the Swiss Medical Association [18]. The participants only differed from the general Swiss GP population in two points: They are mainly working in group practices (83.3%), where only 36.6% of the general Swiss GPs work in group practices, and only GPs working in the German part of Switzerland were recruited for participation. Nevertheless the initial goal of the project, to demonstrate the feasibility and to highlight its potential, has been achieved. Generalisability will further increase by future recruitment of more GPs in the ongoing project.
Not all the software-providers offer an export-tool at this time. This problem will be resolved after the implementation of EPR becomes routine, thus forcing the software-providers to offer competitive solutions. The implementation of ICPC in the existing software is still very unequal and either facilitates or complicates the coding in daily work, offering potential for improvement. The implementation of the electronic version of the 2nd ICPC edition (ICPC-2-E) for use in EPR [21] could resolve this problem. Moreover, this electronic version includes well-defined converting tables to map ICPC-codes to the more often used International Classification of Diseases (ICD-10) [8]), which easily enables allocating diagnosis coded in hospitals or other institutions.
Although reliability of the ICPC-2 coding with regard to intra-coder and inter-coder agreement has been documented in the PC setting [22], the careful ICPC-coding by doctors in routine practice is crucial for the validity of the morbidity data, thus strategies for a high quality implementation of coding practices are pivotal for the FIRE project. The current variation in absolute numbers of registered patients, ICPC codes and consultations can be explained by differences among the GPs: part time working, delayed participation in the project and participants which mainly submit clinical data with very few codings (“FIRE-light” participants). However the variation in the index of ICPC-codes in relation to the number consultations was moderate with a variation index of 26.9%. The variation of ICPC index seems not only to be related to the adherence to complete codings, but seems to be explained by differences in practice structure and the GPs main clinical focus. This can be illustrated with GP number 8, who shows a very low prevalence for chapters K and L, although his coding index is representative for the GP population (fig. 2 and 3). This shows that the data structure allows analysis of practice or GP-specific data, thus enabling characterisation of practices with regard to their main focus. In addition the data structure can be used as a benchmarking tool allowing comparisons of various performances between individual GPs and the whole sample.
The observation that the mean index of ICPC-codes in relation to the number of consultations rose significantly in the “hot-coding” week has different implications: on the one hand the test phase showed that participants appreciated the appeal of more complete coding, resulting in a significant rise if the index. On the other hand it implies that the currently observed numbers of diagnoses per consultation is underestimated, suggesting room for improvement. In the future phases of the project the average estimated index could be used as a quality control tool. Ongoing education of the participants is needed and coding workshops with the participants are regularly offered. In patients where the diagnosis is unclear, GPs were currently instructed to record the less specific but more appropriate chapter code rather than the more specific but erroneous rubric code, thus favouring quality over quantity. To further optimise the data validity, the development of a sophisticated import tool has already been initiated. Its implementation will enable an automatic error search and elimination of unrealistic values. Additionally, an automated cross check between medication, laboratory results and the ICPC-Code will help to identify missing diagnosis, hence offering a quality control tool for coding.
Recruiting of participants, continuous recording of patient physician encounters and optimising data quality as outlined above is an ongoing process. Nevertheless, the current FIRE database already offers a solid database for performing health services research studies. The current data structures will allow analysis of age- and gender specific prevalence rates of chronic medical conditions and multimorbidity in the PC setting. The combination of morbidity data with vital signs or laboratory data will provide insights into quality of care, especially for the most common chronic diseases. Treatment effects in multimorbid PC patients can be assessed, reflecting effectiveness in a “real world” setting rather than in a randomised controlled study design, which often lacks generalisability [23]. Medical therapies for prevalent chronic diseases coupled with quality performance indicators such as HbA1c can be tracked. FIRE offers not only a huge potential for health services research, but also as a means of quality control offering a benchmarking tool for the participating physicians. In the near future EPRs will become more common offering massive potential in opportunities for a new generation of family physicians [24]. Studies resulting from the ongoing project have the potential to demonstrate the quality of care provided by GPs thus strengthening their role in the health care system. The core competence of a GP is the management of multimorbid patients. FIRE provides a valid database to demonstrate the performance of PC in managing chronically ill patients. The implementation of “pay for performance” [25] is evident around the globe and its potential to optimise the quality of care has been proven in different health care systems (CONTENT [16] and DETECT [9]) [26–27]. FIRE is a framework that allows the collection of data currently needed to optimise resource allocation in the Swiss health care system.
Conclusion
The project proves the feasibility of standardised ongoing collection of research data embedded in routine clinical practice. The FIRE-data represents a knowledge base with the potential to approach scientific questions that could not previously be addressed in primary care in Switzerland, and offers the basis for demonstrating the important contribution of general practice to an efficient and economic health care system.
Thanks to:
– The board of directors of the Swiss Association of General Practitioners (SGAM) for their long-lasting benevolent support including the grants for the study group SGAM Informatics.
– Lucerne University of Applied Sciences and Arts, Prof Thomas Olnoff, for the provision of the online-servers with two relational MySQL-databases.
– The FIRE-Study Group:
– Steering committee: Battegay Edouard, Bhend Heinz, Klaus Daniel, Rosemann Thomas, Zoller Marco.
– Members: Bhend Heinz (Aarburg), Braun Bettina (Zürich), Bürke Hans-Ulrich (Zürich), Cadisch Reto (Kriens), Duner Peter (Eggiwil), Frey Claudius (Aarburg), Günthard Matthias (Winterthur), Haller Denis (Aarburg), Hansselmann Marcel (Solothurn), Horschick Dorothea (Zürich), Joos Bettina (Zürich), Klaus Daniel (Strengelbach), Köstner Beat (Neuenegg), Kuster Benedict (Luzern), Lauffer Giovanni (Möriken), Leibundgut Hans Werner (Müntschemier), Maier Christoph (Volketswil), Schlatter Georg (Stein am Rhein), Staeger Jacques (Oberägeri), Suter Othmar (Suhr), Weber Fritz (Buchs), Weber-Schär Johanna (Buchs), Widler Josef (Zürich), Zimmermann Rahel (Zürich).
– Coordinating and data managing team: Bend Heinz, Kaplan Vladimir, Senn Oliver.
Correspondence:
Dr. med. Corinne Chmiel
Institute of General Practice and Health Services Research
University Hospital of Zurich
Rämistrasse 100
CH-8091 Zürich
Switzerland
Corinne.Chmiel@usz.ch
References
1 NZZ Online: Wo die meisten Patienten sind, wird am wenigsten geforscht. In.; 2008.
2 de Lusignan S, Teasdale S, Little D, Zapp J, Zuckerman A, Bates DW, Steele A. Comprehensive computerised primary care records are an essential component of any national health information strategy: report from an international consensus conference. Inform Prim Care. 2004;12(4):255–64.
3 Zoller M, Marty F, Bhend H, Wagner J, Hess L, Rosemann T. Utilization of information technologies in ambulatory care in Switzerland. Swiss Medical Weekly (submitted) 2010.
4 Marty F. Das Beach Projekt. Primary Care. 2005;5:32–3.
5 De Maeseneer JM, van Driel ML, Green LA, van Weel C. The need for research in primary care. Lancet. 2003;362(9392):1314–9.
6 WONCA: ICPC-2: International Classification of Primary Care Oxford: Oxford University Press; 1987.
7 Okkes I, Lamberts H. Classification and the domain of family practice. In: Oxford Textbook of Primary Medical Care. Edited by R J, R B, L C, D G, R G, D M, C S. Oxford: Oxford University Press; 2004:139–53.
8 WHO: Manual of the International Classification of Diseases, Injuries, and Causes of Death. Tenth revision, ICD-10. Geneva: World Health Organisation; 1993.
9 [http://www.icpc.ch]
10 Bhend H, Rosemann T, Zoller M. ICPC-2 – Missing Link. Primary Care. 2008;8:13.
11 Meyer RL. Von der ICHPPC zur ICPC. Primary Care. 2005, 10.
12 Bhend H, Zoller M. Roadmap für die elektronische Krankengeschichte. Schweizerische Ärztezeitung. 2008;32:1361–3.
13 Bhend H. ICPC-2 -First Steps. Primary Care. 2008;8:6.
14 http://www.icpc.ch/wiki or http://www.icpc.ch/mediawikifr
15 Zoller M. Forschung bei Hausärzten – auf Knopfdruck möglich? Primary Care. 2006, 4.
16 Laux G, Koerner T, Rosemann T, Beyer M, Gilbert K, Szecsenyi J. The CONTENT project: a problem-oriented, episode-based electronic patient record in primary care. Inform Prim Care. 2005;13(4):249–55.
17 Zentralinstitut für die kassenärztliche Versorgung in der Bundesrepublik Deutschland. http://www.zi-berlin.de/morbilitaetsanalyse/downloads/Beispiel-WWW-Seite.pdf
18 http://www.fmh.ch/themen/aerztedemographie.html : FMH-Ärztestatistik 2009. Schweizerische Ärztezeitung. 2010;91:11.
19 Körner T. Die Episode als Grundlage der Dokumentation. Deutsches Ärzteblatt. 2005;10:46.
20 Okkes I, Jamoulle M, Lamberts H, Bentzen N, ICPC-2-E: Severity of episodes of care assessed by family physicians and patients. The DUSOI/WONCA as an extension of the International Classification of Primary Care (ICPC). Fam Pract. 2002;19:350–6.
21 Okkes I, Jamoulle M, Lamberts H, Bentzen N. ICPC-2-E: the electronic version of ICPC-2. Differences from the printed version and the consequences. Fam Pract. 2000;17(2):101–7.
22 Britt H, Angelis M, Harris E. The reliability and validity of doctor-recorded morbidity data in active data collection systems. Scandinavian Journal of Primary Health Care 1998;16:50–5.
23 Asthma data from the Swiss Sentinel Surveillance Network, 1989–2005 – from monitoring to research (http://www.smw.ch/docs/PdfContent/smw-12767.pdf)
24 The new generation of family physicians – career motivation, life goals and work-life balance (http://www.smw.ch/docs/pdf200x/2008/21/smw-12103.PDF)
25 Campbell S, Reeves D, Kontopantelis E, Middleton E, Sibbald B, Roland M. Quality of primary care in England with the introduction of pay for performance. N Engl J Med. 2007;357(2):181–90.
26 Hummers-Pradier E, Beyer M, Chevallier P, Eilat-Tsanani S, Lionis C, Peremans L, et al. The Research Agenda for General Practice/Family Medicine and Primary Health Care in Europe. Part 1. Background and methodology. Eur J Gen Pract. 2009;15(4):243–50.
27 Towards Consensus on Best Practice: Use of patient records from general practice for research. In: The WellcomeTrustReport. 2009.