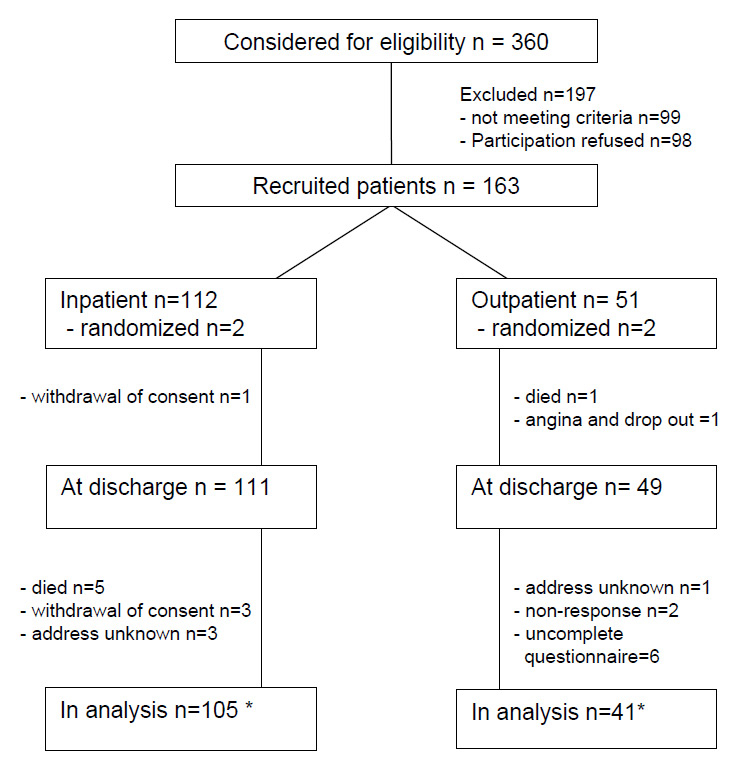
Figure 1
Patient flow. all patients aged 30–65 with acute coronary syndrome (ACS) at day 2 to 5 after ACS during the study period were considered for eligibility. *fatal cases included in analysis
DOI: https://doi.org/10.57187/smw.2011.13141
Although overall mortality from cardiac diseases and coronary heart disease (CHD) in particular is decreasing, CHD it is still the major cause of death in western countries. Even patients that survive ST-elevation myocardial infarction have a risk of dying during the next 12 months in the range of 3–25%, depending on their individual risk [1].
To reduce post-infarction mortality, exercise-based cardiac rehabilitation has been evaluated and subsequently proven as being an effective approach in secondary prevention [2, 3], resulting not only in less deaths but also in an improved quality of life [4, 5]. In Germany, comprehensive cardiac rehabilitation (CCR) is a well established component in the sequence of medical care for patients having had a coronary event like myocardial infarction, unstable angina, coronary intervention or coronary bypass surgery [6–10]. CCR is usually employed within the first fourteen days after discharge from the hospital and consists of endurance training, walking, small games and education on health promoting habits like weight reduction and smoking cessation. CCR is mostly performed in rehabilitation hospitals which are traditionally situated in rural areas that are supposed to have a health-promoting climate [6]. This setting is an “ideal type” setting where the patient is assumed to change habits and “regenerate” from the disease, and this setting is also partly found in the social security systems of Switzerland and Austria. However, recovery is much related to the social relations and functions of a patient [11] which can be disturbed by such a setting, and a possible social isolation may have negative effects like promoting somatisation.
Since a majority of patients from the working population to date live in urban areas, increasingly patients wish to conduct CCR near their domicile in an outpatient setting. Therefore, outpatient CCR has also been started in Germany, gaining promising results [6–9, 12]. However, the quality and efficacy of outpatient CCR has not yet been compared with the classical German inpatient CCR. The SARAH trial (Stationäre versus ambulante Rehabilition nach akutem Herzereignis) addressed this question by investigating long-term effects of inpatient and outpatient rehabilitation for cardiac diseases.
The study was carried out according to the Declaration of Helsinki and was approved by the Institutional Ethics Board of Ulm University. Written informed consent was obtained from all participants. Patient enrolment began in July 2002 and ended in September 2004. A total of 163 patients were included. All patients had coronary heart disease that had recently led to a coronary event such as ST-elevation myocardial infarction (STEMI), Non-ST-elevation myocardial infarction (NSTEMI) or unstable angina.
The study was planned to be conducted in a comprehensive cohort design, which means that a randomisation procedure was intended [13]. After patients had agreed to participate in the study, patients could either be randomised to inpatient versus outpatient CCR or if randomisation was rejected patients were offered the option of choosing the treatment arm according to their preference [14].
Patients were medically evaluated at the beginning and the end of CCR. Assessment included history, physical examination, anthropometry, electrocardiogram and laboratory tests. Physical performance was determined in an all-out stepwise increased cycle ergometer test (25 watt, 25 watt increase each 2 min). Echocardiographically determined LV function was assessed from normal (1) to severely reduced (4).
Self reported physical activity during the last 12 months was determined with a questionnaire adapted from a large German cardiac register (MONICA/KORA) asking for a patient’s engagement in sports in hours/per week (15). Secondly, activity was measured during CCR by an accelerometer (ActiTrac, IM Systems, Baltimore, USA) attached to the patient’s lower leg over two to three days.
Patients’ follow up visits were scheduled at 6 weeks, 6 and 12 months after completion of rehabilitation. At those time points, the same tests as in the beginning and the end of rehabilitation were performed.
Possible participants were identified from the catheter lab of the Ulm University Hospital, Germany, and were enrolled two to five days after the acute event. All patients admitted to acute care for an acute coronary event, such as ST elevation MI, non-ST elevation MI or unstable angina were considered for recruitment. The main inclusion criteria were existence of angiographically proven coronary stenosis as the cause of the event, age between 30 to 65 years, and distance from the patient’s residence to the potential outpatient rehabilitating institution of not more than 50 km. Patients of other ages, patients with severe complications, and unstable patients (e.g. patients treated at the intensive care unit, patients with concomitant coronary operations, or patients transferred to other hospitals or hospital departments) were not screened.
Patients in either an inpatient or outpatient setting were subjected to CCR for six hours per day on average. The major elements on the schedule were endurance training on the cycle ergometer, strength and flexibility training and small games (approx. 45% of CCR time), medical educational sessions (approx. 15%), psychological support (e.g., stress management, individual therapy, relaxation techniques; approx. 20%), professional nutritional advice (approx. 15%), and social or occupational advice (approx. 5%). The CCR programme was standardised according to pension fund regulations before the study. There were no differences between the institutions except application of physical therapy (6.4% inpatients vs. 1.6% outpatients) and tendencies in recreational measures (18.1% vs. 11.0%) and sports (41.5 % vs. 54.1%). The outpatients had to travel by public transportation (bus, train) or by car each day, and could perform house hold and social activities.
As the primary combined outcome measure, event-free survival (EFS) and its association with the setting of rehabilitation (inpatient or outpatient, respectively) was defined. Event-free survival was calculated for the following events: myocardial infarction, stroke, heart failure, life-threatening rhythm events, unstable angina and death. A further combined outcome measure was interventional (EFS-I) comprised of percutaneous coronary intervention (PCI) or coronary artery bypass graft (CABG). Secondary predefined binary outcome measures were overall mortality, and occurrence or recurrence of one of the above mentioned events.
Members of a central committee who were unaware of study-group assignments adjudicated potential binary outcomes as reported by the investigators.
Quantitative secondary outcome measures during rehabilitation and follow up consisted of body-mass-index (BMI) expressed as kg/m2, and exercise performance. Physical activity was assessed by a questionnaire before CCR and at follow up, and was measured by accelerometer during CCR.
Binary outcome measures were depicted as cross-tables and analysed using Fisher’s exact test. For non-randomised patients, due to potential predefined confounders adjustments were made applying the logistic regression method. Potential predefined confounders were: left ventricular function, gender, body mass index, age, maximal performance in the ergometer test before rehabilitation, and physical activity before the acute event (moderate and high activity levels).
For secondary metric data, the two-sided t-test was applied. For ordinal data the non-parametric Mann-Whitney U-test was used. All tests were computed using SPSS 16.0 statistical package.
Between July 2002 and September 2004, 360 patients were screened for eligibility of which 99 met the exclusion criteria and 98 otherwise eligible patients refused to participate. Of the remaining patients, only four (2.5%) agreed to randomisation. In total, 163 patients were included of which 51 were enrolled in the outpatient CCR and 112 were in the inpatient CCR (fig. 1). The evaluation of effects as presented here was finally possible for 105 patients of the inpatient arm and 41 patients of the outpatient arm, due to drop outs and losses at follow up (fig. 1). Gender, age, BMI and smoking status did not differ significantly between both groups (table 1).
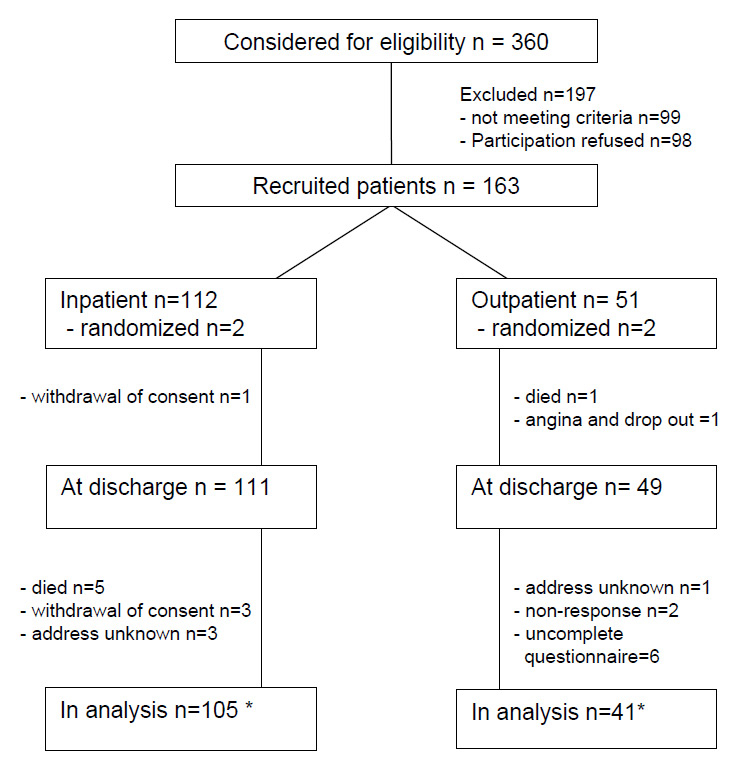
Figure 1
Patient flow. all patients aged 30–65 with acute coronary syndrome (ACS) at day 2 to 5 after ACS during the study period were considered for eligibility. *fatal cases included in analysis
The rate of ST-elevation myocardial infarction was 81.8 % (inpatient) and 67.3% (outpatient). The rate of non-ST-elevation myocardial infarction was 14.5% vs. 30.6%, which was not a statistical significant difference (p = .058). LV function was not different, 11.7 vs 10.3% with moderately to severely reduced LV function. There was a significant difference in maximal performance (p <0.001). STEMI and maximal performance were included as possible confounders in the statistical analysis. More baseline characteristics are described in the concomitant analysis by Schweikert et al. [14].
Adjusted event-free survival (EFS) was not different in the groups, with 21.9% of patients having an event in the inpatient group and 17.1% in the outpatient group (odds ratio: 0.68 (0.16–2.84) in favour of outpatients, p = 0.650), after all results were adjusted by logistic regression for confounders: age, BMI, LV-function, exercise capacity and physical activity before the event. When interventions (PCI or CABG) were also counted as events (EFS-I), the difference between groups was higher with 35.3% in inpatients and 46.3% in outpatients (p = 0.341).
A detailed analysis revealed a considerable but non-significant difference in the frequency of PCI, with 34.3% in the inpatient and 43.9% in the outpatient arm (p = 0.257), which contributed largely to the greater difference in EFS-I between the two groups (table 2).
Both groups did not significantly differ in the rate of myocardial infarction, stroke, heart failure, life-threatening arrhythmias, unstable angina, rate of CABG or death. As in the outpatient group, one patient had a new onset of angina and one patient died during CCR; an as‑treated analysis was performed with no difference in the calculated outcome (table 3).
At baseline, physical performance of inpatients and outpatients differed (98.5 ± 26.3 W vs. 129.2 ± 42.1 W, p <0.001). During CCR, (adjusted) change of performance increased significantly in both groups (32.8 (26.2–37.4) W vs. 21.9 (12.0–31.8) W, mean increase and 95% confidence interval, respectively, difference: p = 0.096). During follow up, the adjusted increase in performance was 41.7 (30.9–52.5) W vs. 20.7 (0.122–41.4) (W, difference: p = 0.091).
Before CCR, leisure time related physical activity was not different and 10% of inpatients had an activity of more than 2 hours per week, and 26% more than 1 hour/week (10.8 vs. 54.2% in outpatients), with no significant difference, p = 0.815 and p = 0.843, respectively. At follow up, these activity rates increased and 23.1% of inpatients had an activity of more than 2 hours per week, and 49.1 % had more than 1 hour/week (30.8 vs. 54.2% in outpatients), with significance values of p = 0.721 and p = 0.807 between groups for the activity rates. The overall change in reported activity at follow up was significant also after adjustment for covariates (p <0.001).
The accelerometric measurement during CCR revealed 68.9% of recorded time was spent inactive in inpatients compared to 60.0% in outpatients (difference 8.9%, p = 0.003). Furthermore, inpatients spent significantly more time in the range of low activity than outpatients (p <.001). Conversely, inpatients spent less time with medium activities.
BMI was similar in both groups (table 1). At 12 months after CCR, BMI in inpatients increased (+0.69 kg/m2) and slightly decreased in outpatients (–0.27 kg/m2). Multivariate analysis after adjustment for physical activity, maximal performance, age, gender, and LV-function revealed no difference between the in- and outpatients. After 12 months, there was no difference in either the univariate or in multivariate analysis. Performing a complete case analysis, no different trend could be observed; the whole study population significantly gained weight during follow-up (from 27.4 at baseline to 28.4 at 12 months, p = 0.005) with no difference between groups (p = 0.845).
| Table 1:Baseline characteristics of study sample (n = 163). | ||||
| Inpatient (n = 112) | Outpatient (n = 51) | |||
| n | n | |||
| Age (mean ± sd) | 112 | 56.7 ± 9.9 | 51 | 54.4 ± 10.3 |
| Gender (% male pts.) | 112 | 78 | 51 | 76 |
| LV function1 (mean ± sd) | 103 | 1.43 ± 0.66 | 39 | 1.54 ± 0.76 |
| Reduced LV function2 (% grade 3 + 4 pts.) | 103 | 11.7 | 39 | 10.3 |
| STEMI (% of all patients)3 | 90 | 81.8 | 33 | 67.3 |
| BMI (mean ± sd) | 105 | 27.3 ± 4.6 | 40 | 28.2 ± 5.0 |
| Maximal performance (Watt, mean ± sd) | 103 | 98.5 ± 26.3 | 41 | 129.1 ± 42.1 |
| Current smoker | 105 | 30 | 41 | 9 |
| 1 Ordinate measure ranging from 1 (normal) to 4 (severely reduced) left ventricular function 2 The same measure, with pooled analysis for grade 1 and 2, or 3 and 4, respectively 3 ST-elevation myocardial infarction | ||||
| Table 2:Event-free survival (EFS) calculated as combined outcome measure without PCI / CABG, with PCI, with CABG and EFS-I (EFS with interventions) with PCI / CABG. The table gives the absolute and relative incidents, the crude odds ratios and the adjusted odd ratios after logistic regression for in- and outpatients1. | ||||||||
| Inpatient | Outpatient | Crude results Crosstables | Adjusted results Logistic regression1 | |||||
| events / pts. (%) | events / pts. (%) | Odds ratio2 | Confidence intervall | p-value (2-sided) | Odds ratio2 | Confidence intervall | p-value | |
| EFS: Combined outcome measure w/o PCI / CABG | 23 / 105 (21.9) | 7 / 41 (17.1) | 0.713 | 0.288–1.871 | 0.650 | 0.678 | 0.162–2.838 | 0.595 |
| Combined outcome measure with PCI | 36 / 105 (34.3) | 18 / 41 (43.9) | 1.500 | 0.718–3.134 | 0.341 | 1.706 | 0.603–4.829 | 0.314 |
| Combined outcome measure with CABG | 24 / 105 (22.9) | 9 / 41 (22.0) | 0.949 | 0.398–2.262 | 1.000 | 1.143 | 0.313–4.143 | 0.839 |
| EFS-I: Combined outcome measure with PCI or CABG | 37 / 105 (35.3) | 19 / 41 (46.3) | 1.5987 | 0.763–3.303 | 0.257 | 1.952 | 0.692–5.509 | 0.206 |
| 1 for adjustment, logistic regression analysis was performed employing the covariates age, gender, body mass index, maximum performance on the cycle ergometer before rehabilitation, left ventricular function and physical activity before the acute cardiac event 2 values <1.0 favour outpatient rehabilitation | ||||||||
| Table 3:Secondary outcome measures of morbidity and overall mortality. The table gives the absolute and relative incidents, the crude odds ratios and the adjusted odd ratios after logistic regression for in- and outpatients1. | ||||||
| Inpatient | Outpatient | Crude results Crosstables | Adjusted results Logistic regression4 | |||
| events / pts. (%) | events / pts. (%) | Odds ratio1 (confidence interval) | p-value (2-sided) | Odds ratio4 (confidence interval) | p-value (2-sided) | |
| Myocardial infarction | 3 / 105 (2.9) | 2 / 40 (5.0) | 1.789 (0.288–11.128) | 0.616 | –5 | –5 |
| Cerebral ischeamia | 3 / 105 (2.9) | 0 / 41 (0) | 0.353 (0.018–6.982 ) | 0.559 | –5 | –5 |
| Heart failure | 0 / 105 (0) | 1 / 41 (2.4) | 7.815 (0.312–195.8) | 0.281 | –5 | –5 |
| Severe rhythm event | 2 / 105 (1.9) | 0 / 41 (0) | 0.499 (0.023–10.613) | 1.000 | –5 | –5 |
| New onset angina or recurrent angina2 | 17 /105 (16.2) | 4 / 41 (9.8) | 0.560 (0.176–1.776) | 0.4342 | 0.55 (0.11–2.91) | 0.49 |
| PCI | 23 /105 (21.9) | 14 / 41 (34.1) | 1.849 (0.836–4.090) | 0.142 | 2.510 (0.788–7.995) | 0.119 |
| CABG | 3 /105 (2.9) | 2 / 41 (4.9) | 1.744 (0.281–10.835) | 0.620 | 1.898 (0.156–23.072) | 0.615 |
| Death3 | 5 / 105 (4.8) | 1 / 41 (2.4) | 0.500 (0.057–4.415) | 0.4593 | –5 | –5 |
| 1 values <1.0 favor outpatient rehabilitation 2 As-treated analysis (only events after completion of rehabilitation): adjusted p = 1.00 3 As-treated analysis (only events after completion of rehabilitation): adjusted p = 0.29 4 for adjustment, logistic regression analysis was performed employing the covariates age, gender, body mass index, maximum performance on the cycle ergometer before rehabilitation, left ventricular function and physical activity before the acute cardiac event –5 Logistic regression was not possible because of low event rate | ||||||
As a consequence of a particular historical development, rehabilitation after myocardial infarction and other cardiac events in Germany is, for the most part, conducted in an inpatient setting in specialised facilities [6, 7]. Due to the demands of urban work and social life, CCR is increasingly offered in an outpatient setting. The efficacy of this approach with respect to mean maximum performance and lipid management has been demonstrated recently [2, 7, 9, 16–19]. The aim of this study was to add additional information to this topic by directly comparing the effects of inpatient and outpatient rehabilitation, with an emphasis on long term outcome.
The primary research question was explorative evaluation of the new outpatient setting. As the first University hospital in Germany, we established a cardiac outpatient rehabilitation unit and compared it to a “gold standard” inpatient rehabilitation hospital in a prospective study which included not only the rehabilitation but also a follow up period of 12 months.
It was very complicated to achieve approval for such a prospective study. Since the certification process for such outpatient units is very complicated in Germany, a multicentre approach to increase patient numbers was not possible and would not have been financed. Furthermore, a blinded randomisation independent of patient’s preferences with a control group was not possible due to social legislation in Germany. The grant funded a specific time period and all willing patients who were able able to take part in the study were included.
We intended to include 200 patients within 2 years based on the analysis of patient structure in the referring clinic. This number seemed to be high enough to enable an adjusted multivariate analysis for 3–6 confounders. As we had no other information (e.g. no estimation on the patients’ agreement on randomisation), a detailed calculation of samples size was not possible in advance.
An initial result of this study revealed a low acceptance of randomisation among eligible patients, or in other terms 97.5% of patients showed a strong preference for either of the two rehabilitation settings. The determinants and factors contributing to this preference would be worth further investigation and should be taken into account for subsequent trials in this field.
Regarding overall survival and event-free survival (EFS) as well as particular events separately (e.g., infarction, bypass surgery), the effects of rehabilitation were similar in both treatment groups and are in a low risk range compared to other studies [17, 20, 21]. The broadest difference was observed when comparing PTCA rates or EFS comprising of PTCA, respectively. However, these differences were far from reaching statistical significance, and might be due to access barriers, in that the facility performing outpatient rehabilitation was connected to a cardiology department, whereas the inpatient facility was not. There was also no difference for secondary outcomes.
Regarding secondary outcome measures, we observed an increase of physical performance during CCR in both groups, like in previous studies [2, 18, 19], which was stronger in the inpatient group due to a lower baseline performance. This gain of performance was at least maintained for twelve months after in both groups.
Patients that chose outpatient rehabilitation spent about 9% more time of the day in an active state, compared to the inpatient group during CCR. Moreover, ambulatory patients spent more time with occupations in the highest activity level and less time in occupations with the lowest activity level, when compared to those in the outpatient setting, for which findings were vice versa. This difference was not maintained in the reported activity at follow up. In general, the increase in activity was considerably high in both groups as the percentage of reporting more than 2 hours exercise per week nearly doubled.
Similarly, physical performance increased in both intervention groups until follow up.
Finally, as seen in similar trials [4, 6, 9], despite successful intervention in terms of maximum performance, there was a significant weight gain of 1kg from baseline to the 12 month follow-up.
Adherence to the prescribed rehabilitation measures can impact on the outcome of the rehabilitation program; it can be useful to assess possible predictors of adherence, such as illness perception, psychological distress or self-efficacy. Still, we did not observe a lack of adherence, since during the actual course of rehabilitation considerable control was exerted as demonstrated by the fact that only one patient of the whole study population dropped out during rehabilitation. Furthermore, during follow-up patients could maintain or even increase their individual performance level on average. In the present analysis, we could demonstrate that general daily activities could be remarkably increased by CCR in the follow up-period of 12 months. We could not demonstrate that the higher activity in outpatient CCR translated to higher activity and maximum performance compared to inpatients, which was probably due to the study size. However, we could demonstrate furthermore that these effects translated to improved quality of life [14].
The small but considerable weight gain comparing baseline values to the follow-up recordings, as it was observed in this study as well as in former trials [4, 9, 19, 22], suggests insufficient risk factor control [23]. As a consequence, both exercise and motivational intervention should be tailored more towards increasing daily activity (also outside rehabilitation) rather than focusing on increasing maximum performance (mainly inside rehabilitation). On the other hand, an increased fat free body mass could have the same effect on BMI and would be beneficial and would lower morbidity and mortality [5, 24, 25]. However, this is hypothetical and should be addressed in future trials.
This study has the limitation that interventions could not be compared in a randomised fashion which possibly might result in selection bias. Primarily, the study was intended as a comprehensive cohort study [13] with incorporated randomised arms. However, patients rarely complied with randomisation but chose according to their preferences, resulting in only 2.5% of patients consenting to being randomised; which may be typical for expectations of German patients [6, 7]. Therefore, the study had to be conducted and analysed as an observational trial [13]. Still, both intervention groups at baseline were well balanced in most regards [14]. There was only a statistically significant imbalance between the study groups with respect to physical performance. In order to handle the limitations of the cohort design properly, all results were adjusted by logistic regression for all relevant confounders.
However, there might be additional limitations due to the relatively limited number of patients which make it difficult to detect smaller differences. For example, the reported smoking status was low (table 1) and did not change after 12 months. Although smoking is a major risk factor, in this study it explained no differences between the groups in the multivariate analysis, mainly due to underreporting and small numbers.
Taken together, despite the limitations of this trial, its results suggest that comprehensive outpatient and inpatient cardiac rehabilitation programs lead to comparable outcomes in terms of morbidity and mortality; this is underscored by the cost-effectiveness of outpatient rehabilitation in the concomitant analysis by Schweikert et al. [14]. Therefore, this form of rehabilitation service has positive effects on the health related costs in the year following the acute cardiac event. CCR increased physical activity and physical performance for 12 months which underlines the effects of structured rehabilitation programs in Germany.
| Table 4: Physical performance (cycle ergometer test) at the beginning, at the end and at the 12 months follow-up of rehabilitation (Watt). | ||||
| Start (S) of rehabilitation | End (E) of rehabilitation | 12 months follow-up (FU12) | Delta (FU12-A)1 | |
| Both groups | 106.1 | 135.1 | 146.7 | + 36.3 (p <.0012) |
| Inpatient group | 98.5 | 126.5 | 141.5 | + 42.8 |
| Outpatient group | 129.1 | 156.4 | 161.0 | + 18.8 |
| p value (between groups) | < .001 | .004 | .151 | .018 |
| 1 complete case analysis 2 paired analysis, two-sided t test | ||||
Funded by the German pension insurance and the German Ministry of Research and Education (BMBF), Grant number: 02 7 06 and 01GD0108. No conflict of interest.
1 Boden WE, Shah PK, Gupta V, Ohman EM. Contemporary approach to the diagnosis and management of non-ST-segment elevation acute coronary syndromes. Prog Cardiovasc Dis. 2008;50(5):311–51.
2 Jolliffe JA, Rees K, Taylor RS, Thompson D, Oldridge N, Ebrahim S. Exercise-based rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2007;(3):1–62.
3 Giannuzzi P, Mezzani A, Saner H, Bjornstad H, Fioretti P, Mendes M, et al. Physical activity for primary and secondary prevention. Position paper of the Working Group on Cardiac Rehabilitation and Exercise Physiology of the European Society of Cardiology. Eur J Cardiovasc Prev Rehabil. 2003;10(5):319–27.
4 Marchionni N, Fattirolli F, Fumagalli S, Oldridge N, Del LF, Morosi L, et al. Improved exercise tolerance and quality of life with cardiac rehabilitation of older patients after myocardial infarction: results of a randomized, controlled trial. Circulation. 2003;107(17):2201–6.
5 Giannuzzi P, Saner H, Bjornstad H, Fioretti P, Mendes M, Cohen-Solal A, et al. Secondary prevention through cardiac rehabilitation: position paper of the Working Group on Cardiac Rehabilitation and Exercise Physiology of the European Society of Cardiology. Eur Heart J. 2003;24(13):1273–8.
6 Karoff M, Held K, Bjarnason-Wehrens B. Cardiac rehabilitation in Germany. Eur J Cardiovasc Prev Rehabil. 2007;14(1):18–27.
7 Iseringhausen O, Schott T, Orde vA. The quality of organization in cardiac rehabilitation – a comparison of inpatient and outpatient forms of service delivery. Rehabilitation. 2002;41:130–9.
8 Heidrich J, Liese AD, Kalic M, Winter-Enbergs A, Wellmann J, Roeder N, et al. Secondary prevention of coronary heart disease. Results from EuroASPIRE I and II in the region of Munster, Germany. Dtsch Med Wochenschr. 2002;127(13):667–72.
9 Bjarnason-Wehrens B, Predel HG, Graf C, Rost R. Ambulatory cardiac phase II rehabilitation – “the Cologne model” – including 3-year-outcome after termination of rehabilitation. Herz. 1999;24(Suppl 1):9–23.
10 Unverdorben M, Unverdorben S, Edel K, Degenhardt R, Brusis OA, Vallbracht C. Risk predictors and frequency of cardiovascular symptoms occurring during cardiac rehabilitation programs in phase III-WHO. Clin Res Cardiol. 2007;96(6):383–8.
11 Mookadam F, Arthur HM. Social support and its relationship to morbidity and mortality after acute myocardial infarction: systematic overview. Arch Intern Med. 2004;164(14):1514–8.
12 Stilgenbauer F, Reißnecker S, Steinacker JM. Heart rate predictions for the training of cardiac patients. Dtsch Z Sportmed. 2003;54(10):295–6.
13 Muche R, Imhof A. The Comprehensive Cohort Design as alternative to the randomized controlled trial in rehabilitation research: advantages, disadvantages, and implementation in the SARAH study. Rehabilitation. 2003;42:243–9.
14 Schweikert B, Hahmann H, Steinacker J, Imhof A, Muche R, Koenig W, Liu Y, et al. Intervention study shows outpatient cardiac rehabilitation to be economically at least as attractive as inpatient rehabilitation. Clin Res Cardiol. 2009;79(12):787–95.
15 Meisinger C, Löwel H, Heier M, Kandler U, Döring A. Association of sports activities in leisure time and incident myocardial infarction in middle-aged men and women from the general population: the MONICA/KORA Augsburg cohort study. Eur J Cardiovasc Prev Rehabil. 2007;14(6):788–92.
16 Hambrecht R, Gielen S, Linke A, Fiehn E, Yu J, Walther C, et al. Effects of exercise training on left ventricular function and peripheral resistance in patients with chronic heart failure: A randomized trial. JAMA. 2000;283(23):3095–101.
17 Heidrich J, Wellmann J, Hense HW, Siebert E, Liese AD, Lowel H, et al. Classical risk factors for myocardial infarction and total mortality in the community – 13-year follow-up of the MONICA Augsburg cohort study. Z Kardiol. 2003;92(6):445–54.
18 Taylor RS, Brown A, Ebrahim S, Jolliffe J, Noorani H, Rees K, et al. Exercise-based rehabilitation for patients with coronary heart disease: systematic review and meta-analysis of randomized controlled trials. Am J Med. 2004;116(10):682–92.
19 Bjarnason-Wehrens B, Bott D, Benesch L, Bischoff KO, Buran-Kilian B, Gysan D, et al. Long-term results of a three-week intensive cardiac out-patient rehabilitation program in motivated patients with low social status. Clin Res Cardiol. 2007;96(2):77–85.
20 Corra U, Giannuzzi P, Adamopoulos S, Bjornstad H, Bjarnason-Weherns B, Cohen-Solal A, et al. Executive summary of the position paper of the Working Group on Cardiac Rehabilitation and Exercise Physiology of the European Society of Cardiology (ESC): core components of cardiac rehabilitation in chronic heart failure. Eur J Cardiovasc Prev Rehabil. 2005;12(4):321–5.
21 Pohlen M, Bunzemeier H, Husemann W, Roeder N, Breithardt G, Reinecke H. Risk predictors for adverse outcomes after percutaneous coronary interventions and their related costs. Clin Res Cardiol. 2008;97(7):441–8.
22 Shaw K, Gennat H, O'Rourke P, Del MC. Exercise for overweight or obesity. Cochrane Database Syst Rev. 2006; 4:CD003817.
23 Peytremann-Bridevaux I, Santos-Eggimann B. Health correlates of overweight and obesity in adults aged 50 years and over: results from the Survey of Health, Ageing and Retirement in Europe (SHARE). Swiss Med Wkly. 2008;138(17–18):261–6.
24 Schunkert H, Moebus S, Hanisch J, Bramlage P, Steinhagen-Thiessen E, Hauner H, et al. The correlation between waist circumference and ESC cardiovascular risk score: data from the German metabolic and cardiovascular risk project (GEMCAS). Clin Res Cardiol. 2008;97(11):827–35.
25 Bucksch J, Schlicht W. Is Mortality reduced by Physical Activity in Normal- and Overweight Men and Woman? Dtsch Z Sportmed. 2010;61(3):72–8.