
Figure 1
Patients flow chart throughout the study.
DOI: https://doi.org/10.4414/smw.2010.13133
LBP represents a major health problem which places a substantial economic burden on society in Switzerland [1] and other developed countries [2]. The monthly prevalence of LBP in the Swiss adult population is estimated to be 10%, representing the highest prevalence of all major physical disorders [3]. The prognosis is favourable, with 60–70% of patients recovering in 6 weeks and 80–90% in 12 weeks [4]. However, 85% of costs are ascribable to chronic cases, which represent only 10% of total cases. [5]. The return to work rate declines abruptly from 3 to 6 months off work [4]. The longer the patients with LBP are sick, the more difficult the return to work.
According to a widely used classification based on symptom duration, low back pain can be acute (<6 weeks), subacute (6–12 weeks) or chronic (>12 weeks). A conceptual framework linking back pain and occupational activity was presented by the Paris task force to render explicit the progress from LBP to the restriction in employment participation [6]. Occupational activity was divided into three categories: regular, reduced and interrupted. According to the biopsychosocial model proposed by Waddell [7], interventions aiming to help patients change from interrupted to reduced, or reduced to regular occupational activity should not be limited to a biologic conception of pain but take into account all dimensions of the individual. This multidisciplinary management of low back pain was introduced as early as the 1980’s with the concept of functional restoration [8], in an attempt to reduce work absenteeism due to low back pain and improve patients’ functional status. This is a tertiary form of reeducation that is considered when low back pain persists after less expensive conservative treatments. The whole person is taken into account by the intervention of a multidisciplinary team over an outpatient programme of 3 to 6 weeks [8–11].
In a systematic review in 2001, Guzman et al. found that multidisciplinary biopsychosocial rehabilitation improves function (strong evidence) and pain (moderate evidence) when compared to non-multidisciplinary treatments or usual care. There was contradictory evidence regarding vocational outcomes [12]. In a recent systematic review, Ravenek et al. concluded that there is still conflicting evidence for the effectiveness of multidisciplinary programmes to improve employment outcomes in chronic LBP. No demonstrable effect was found on pain reduction and functional improvement compared to control treatment [13]. These results contrast with those obtained in the systematic review of van Geen et al. on the long-term effects of multidisciplinary rehabilitation, who found a positive effect on work participation but contradictory effects on pain and functional status [14]. In a systematic review including a meta-analysis, Norlund et al. found a positive effect on return to work for sick-listed adults with subacute or chronic low back pain [15].
The following randomised controlled trials (RCT) are worthy of attention. In Denmark, Bendix et al. [16] found a significant difference in favour of a 3-week functional restoration programme compared to outpatient physiotherapy (1.5 hours three times per week for 8 weeks) as regards overall assessment, but no difference in health care contacts, sick leave days, back pain, leg pain and activities of daily living. Another Danish group [17] recently compared a 12-week group-based multidisciplinary rehabilitation programme with a 12-week individual back muscle exercise programme. Both interventions resulted in long-term improvements in pain and disability, with only a minor statistically significant difference in disability in favour of the group-based multidisciplinary rehabilitation programme. In France, Jousset et al. [18] randomised 86 patients with chronic low back pain to a functional restoration or an active individual physiotherapy programme. The mean number of sick-leave days was significantly lower in the functional restoration group, but functional capacity improved in both groups, with no significant difference between groups. In a Finnish RCT [19], 120 women with chronic low back pain were allocated to multidisciplinary rehabilitation or individual physiotherapy. No difference was observed between both interventions in subjective working capacity, sick leave due to back pain, beliefs of working ability after 2 years and disability. The before-and-after comparison showed favourable effects, which were still maintained at 2 years’ follow-up.
The aim of the present study was to compare long-term functional status and work status in a non-specific LBP population randomised to a 3-week FMR or 18 supervised outpatient physiotherapy sessions lasting 9 weeks.
All patients were from the rheumatological outpatient clinic of Lausanne University Hospital Switzerland. Patients were examined by a primary-care physician then referred to physicians at the Spine Unit, where an interview and a physical evaluation were performed to determine whether FMR was appropriate. For the purpose of this study, low back pain was defined as pain, muscle tension, or stiffness localised below the costal margin and above the gluteal folds. Inclusion criteria were subacute (>6 weeks) or chronic (>12 weeks) low back pain, phases 2 to 6 of the Krause classification [20], without irritative neurological deficit, and age between 18 and 60. Phase 2 of the Krause classification refers to the report of an injury or illness affecting the lower back and phase 6 corresponds to late rehabilitation with 3 to 6 months off work. All patients had therefore been either at or off work for less than six months at the beginning of treatment. Exclusion criteria were acute neurological deficit in progress, sciatica, pregnancy, acute inflammatory rheumatic disease, non-osteoarticular thoracic pain, spinal fracture within the last 3 months, severe osteoporosis, tumour, severe heart failure or respiratory failure, active drug addiction, current involvement in litigation related to low back pain, and active psychiatric pathology.

Figure 1
Patients flow chart throughout the study.
The study was designed as a prospective randomised clinical trial. The procedures followed were in accordance with the Helsinki Declaration. Ethical approval was granted by the Ethics Committee of the University Medical School of Lausanne, Switzerland. Patients who met all inclusion criteria and gave written informed consent were allocated by a secretary not involved in the study to a functional multidisciplinary rehabilitation programme (FMR) or outpatient physiotherapy (OP) according to computer-generated random numbers sealed in opaque envelopes with consecutive numbering.
Functional multidisciplinary rehabilitation (FMR). The FMR conception was based on the principles introduced by Mayer et al. [21]. Five patients were treated from Monday to Friday for 5–7 hours per day in a 3-week ambulatory setting. The goals were to improve coping with pain, increase the activity level and optimise the rate of return to work. The multidisciplinary interventions involved occupational, psychological and physical therapists supervised by a medical doctor. The programme included intensive physical and ergonomic training, psychological pain management, back school, instruction in social and work-related issues and a functional evaluation to increase self-responsibility. Each patient received individually tailored pharmacotherapy and regular follow-up by a medical doctor. All treatments corresponded to 31 individual and 63 group hours per patient.
Outpatient physiotherapy (OP). OP consisted in 18 supervised outpatient physiotherapy sessions over 9 weeks. The 45-minute sessions were individually tailored by a physical therapist and included active and passive modalities. The objectives were to manage pain, improve mobility and increase activity level.
Both groups were managed by the same physical therapists. Patients in FMR and OP did not meet each other and thus did not share their feelings about the programmes. Outcomes were assessed by physiotherapists and occupational therapists who were also involved in FMR and OP treatments. They could therefore not be blinded to group allocation.
Primary outcomes were back-related functional disability and work status. Back-related functional disability was measured by the Oswestry Disability Index (ODI) [22, 23] , which is a 10-item scale ranging from 0 to 100%. A high score indicates a high degree of restriction. The ODI was validated in French [24]. ODI was recorded at the beginning of treatment (T), at 3-week (T3w), 9-week (T9w), 6-month (T6m), 9-month (T9m) and 12-month (T12m) follow-up. Work status was quantified by the percentage of professional activity reported by patients and was recorded at T, T6m, T9m and T12m. Values were categorised as off work (work status <20%), part time (20% ≤ work status <100%) or full time working (work status = 100%).
Secondary outcomes were physical assessments. The Spinal Function Sort (SFS) [25] was used to auto-evaluate lifting capacity and the progressive isoinertial lifting evaluation (PILE) [26] to quantify lifting capacity. SFS contains 50 items consisting of a task illustrated by a drawing and a short description. A final score ranging from 0 to 200 is provided, a high score indicating a good perception of lifting capacity. Lumbar PILE and cervical PILE corresponded to the maximum weight the subject could lift four times from floor to waist and from waist to shoulder respectively. The percentage of the body mass was reported. Lumbar flexion and extension range-of-motion was quantified by the modified-modified Schöber technique [27] (MMS). The fingertip-to-floor test [28] was used to complement the measure of lumbar flexion range-of-motion by the MMS technique. The Biering-Sörensen [29] and Shirado [30] tests were used to measure isometric endurance of the trunk extensor and flexor muscles respectively. Aerobic exercise capacity was measured on a treadmill using the modified Bruce protocol [31, 32] . For safety reasons, the test was stopped when subjects reached 85% of predicted maximal heart rate (220 – age). All secondary outcomes were recorded at T, T3w, T9w and T12m.
All study results were collected in a computerised database using PASW for Windows (version 18.0.0, SPSS Inc, Chicago, IL, USA). The significance level was set at P <0.05. Sample size calculation was based on the ODI being compared by an independent samples t-test. To detect a minimal important change of 10 (standard deviation, 14.6) [33] with 90% power at a significance level of 0.05, 47 and 45 patients were required in each group. Estimating a dropout rate of 15%, it was planned to recruit a total of 109 patients. Normality of distribution for all data was controlled with the Kolmogorov-Smirnov test completed by examination of histograms. Baseline group differences were assessed using independent samples t-test for numerical variables and the Goodman and Kruskal tau test for categorical variables. Within groups changes over time were assessed by the paired samples t-test. Between groups comparisons at all follow-ups were computed by an analysis of covariance with baseline as covariate to correct for baseline differences between groups. For work-related variables, non-parametric methods were used. Within groups changes over time were assessed by the Wilcoxon signed-rank test. Between groups differences were assessed using the Goodman and Kruskal tau test. Analyses were done according to the “intention-to-treat” principle, using all randomised participants who provided any follow-up data. Missing values were estimated using multiple linear regressions for subjects who provided at least half the follow-up assessments.
Imputation of missing data has the advantage of limiting the reduction in power of the analysis. On the other hand, this inevitably involves some assumptions that may introduce bias. For this reason missing data were imputed only for subjects who provided at least half of the follow-up assessments, as mentioned before. This method appeared adequate to limit the reduction in power of the analysis with a reasonable amount of assumptions. To examine the robustness of the main analysis, two sensitivity analyses were performed with alternative methods of ODI imputation. The first method involved assumptions oriented towards “difference between groups”. Missing data of subjects who provided less than half of the follow-up assessments were imputed as in the main analysis using multiple linear regressions. The second method was more conservative and consisted of replacement of the missing observations by the last observed value.
109 patients were included in the study and were randomised to FMR (n = 56) or OP (n = 53). Baseline subjects’ characteristics are reported in table 1. FMR patients were significantly younger, taller and more frequently single than OP patients. Other characteristics did not differ significantly between the two groups. As illustrated in figure 1, seven patients of OP never started treatment. Two subjects of OP dropped out due to exacerbation of pain. 40 patients of FMR and 27 patients of OP provided at least half the follow-up assessments and could be included in the ITT analysis. Their baseline characteristics, as well as ODI at baseline, did not significantly differ from those of patients who completed all follow-up assessments.
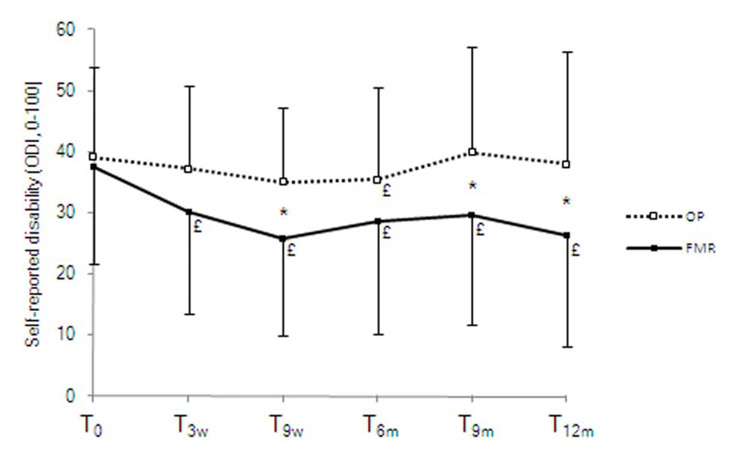
Figure 2
Self-reported disability (Oswestry disability index, ODI) for outpatient physiotherapy (OP) and functional multidisciplinary rehabilitation (FMR) at baseline (T), 3-week (T3w), 9-week (T9w), 6-month (T6m), 9-month (T9m) and 12-month (T12m) follow-up. £ indicates a significant within group difference compared to baseline; *, significant between groups difference.
As illustrated in figure 2, disability decreased largely for FMR from 37.6 (15.8) at T to 30.1 (16.5) at T3w, 25.7 (15.8) at T9w, 28.6 (18.4) at T6m, 29.6 (17.9) at T9m and 26.2 (18.0) at T12m. The decrease was much less marked for OP, which fell from 39.1 (14.7) at T to 37.2 (13.5) at T3w, 35.0 (12.3) at T9w, 35.4 (15.0) at T6m, 39.8 (17.3) at T9m and 38.0 (18.4) at T12m. The decrease compared to T was significant at all follow-ups (P<0.01) for FMR but only at T6m (P= 0.016) for OP. Between-group comparisons showed a significant difference between FMR and OP at T9w (P= 0.012), T9m (P= 0.023) and T12m (P= 0.011). After the sensitivity analyses the first method of data imputation did not change the differences within and between groups observed in the main analysis. The second method did not change the within-group differences but the between-group differences were not significant, a tendency being however observed at T12m (P= 0.089).
Work status evolved favourably in both FMR and OP groups, with an increasing number of patients working full time and a decreasing number off work (table 2). The change compared to T was significant only for FMR and only at T12m (P= 0.012). Between-group comparisons produced a significant difference between FMR and OP at T12m (P= 0.012). Among the 14 patients of FMR who were off work at baseline, 5 (36%) returned to full time work at 6 months, 5 (36%) at 9 months and 6 (43%) at 12 months. Among the 10 patients of OP who were off work at baseline, one (10%) returned to full work at 6 months, 0 at 9 months and 1 (10%) at 12 months. This difference between groups was not significant (Goodman and Kruskal tau test) at 6 months (P= 0.160), significant at 9 months (P = 0.038) and tended to be significant at 12 months (P= 0.087).
Secondary outcomes are shown in table 3. Isometric endurance of the trunk extensor and flexor muscles as well as aerobic exercise capacity improved to a significantly greater extent for FMR compared to OP at short term. Fingertip to floor distance was significantly improved in the short and long terms for FMR compared to OP. MMS extension evolved significantly more favourably for OP compared to FMR in the short term.
| Table 1: Baseline characteristics of subjects by treatment group. | |||||
| FMR n | Mean (SD) or % | OP n | Mean (SD) or % | P* | |
| Age (years) | 56 | 37.8 (9.2) | 46 | 41.8 (8.7) | .029 |
| Height (cm) | 56 | 172.5 (8.3) | 46 | 168.2 (8.0) | .016 |
| Weight (kg) | 56 | 79.1 (15.0) | 46 | 75.5 (13.7) | .255 |
| BMI (kg∙m–2) | 56 | 26.5 (4.1) | 46 | 26.8 (4.5) | .726 |
| Gender Males Females | 41 15 | 73.2% 26.8% | 28 18 | 60.9% 39.1% | .187 |
| Origin Switzerland Other | 25 30 | 45.5% 54.5% | 19 27 | 41.3% 58.7% | .677 |
| Marital status Married Divorced Separated Single | 31 4 1 17 | 58.5% 7.5% 1.9% 32.1% | 32 5 2 5 | 72.7% 11.4% 4.5% 11.4% | .029 |
| FMR indicates functional multidisciplinary rehabilitation; OP, outpatient physiotherapy; SD, standard deviation; BMI, body mass index; *, independent samples t-test or Goodman and Kruskal tau test | |||||
| Table 2: Work status at baseline and after functional multidisciplinary rehabilitation or outpatient physiotherapy. | ||||||
| FMR n | % | OP n | % | P* | ||
| T | Off work Part time Full time | 14 10 16 | 35.0 25.0 40.0 | 10 10 7 | 37.0 37.0 25.9 | .436 |
| T6m | Off work Part time Full time | 9 11 20 | 22.5 27.5 50.0 | 7 11 9 | 25.9 40.7 33.3 | .320 |
| T9m | Off work Part time Full time | 9 9 22 | 22.5 22.5 55.0 | 7 11 9 | 25.9 40.7 33.3 | .133 |
| T12m | Off work Part time Full time | 9 6 25 | 22.5£ 15.0 62.5 | 6 12 9 | 22.2 44.4 33.3 | .012 |
| FMR indicates functional multidisciplinary rehabilitation; OP, outpatient physiotherapy; T, baseline; T3w, 3-week follow-up; T9w, 9-week follow-up; T12m, 12-month follow-up; *, Goodman and Kruskal tau test; £, significant within group difference compared to baseline (Wilcoxon signed-rank test). | ||||||
| Table 3: Secondary outcomes at baseline and after functional multidisciplinary rehabilitation or outpatient physiotherapy. | ||||||
| FMR n | Mean (SD) | OP n | Mean (SD) | P* | ||
| SFS (0-200) | T T3w T9w T12m | 38 32 33 36 | 120.7 (50.1) 142.6 (42.6)£ 138.4 (42.1)£ 132.2 (50.3) | 27 18 22 26 | 109.8 (45.0) 121.0 (45.2) 115.2 (50.1) 105.5 (53.3) | .366 .081 .063 .064 |
| PILE lumbar (%)† | T T3w T9w T12m | 34 34 33 38 | 29.4 (15.7) 32.6 (17.7) 31.4 (14.3) 29.3 (15.0) | 26 17 21 25 | 24.6 (13.5) 23.8 (15.5) 25.0 (17.6) 22.3 (17.4) | .205 .078 .323 .238 |
| PILE cervical (%)† | T T3w T9w T12m | 34 34 33 38 | 25.6 (15.0) 28.3 (14.5)£ 27.5 (11.4) 25.4 (13.3) | 26 17 21 25 | 18.3 (12.6) 20.6 (11.6) 21.5 (14.0)£ 18.7 (13.8) | .041 .320 .779 .628 |
| Biering-Sörensen test (s) | T T3w T9w T12m | 38 34 33 39 | 50.0 (42.9) 72.9 (62.3)£ 71.9 (49.1)£ 56.5 (48.9) | 25 22 23 27 | 43.3 (34.0) 50.0 (33.2) 48.5 (32.2) 38.7 (43.1) | .496 .051 .025 .182 |
| Shirado test (s) | T T3w T9w T12m | 38 34 33 39 | 54.8 (42.5) 92.0 (62.1)£ 82.9 (49.3)£ 75.6 (69.6) | 26 23 23 27 | 43.4 (36.1) 54.5 (57.9) 61.4 (43.1)£ 63.8 (68.3) | .259 .029 .159 .839 |
| Fingertip-floor distance (cm) | T T3w T9w T12m | 38 34 33 40 | 16.6 (14.4) 9.2 (14.3)£ 8.5 (15.6)£ 10.7 (14.5)£ | 26 23 23 27 | 21.0 (18.0) 17.6 (16.3)£ 14.6 (14.2)£ 19.5 (15.6) | .272 .018 .237 .037 |
| MMS test, flexion (cm) | T T3w T9w T12m | 38 34 33 40 | 5.6 (1.3) 6.1 (1.3)£ 6.0 (1.5) 6.4 (1.4)£ | 26 23 23 27 | 5.6 (1.5) 5.9 (1.2) 6.1 (1.3) 6.0 (1.0) | .929 .510 .685 .238 |
| MMS test, extension (cm) | T T3w T9w T12m | 38 34 33 40 | 1.6 (1.0) 1.5 (0.7) 1.6 (0.6) 1.6 (0.9) | 26 23 23 27 | 1.3 (0.7) 1.9 (0.8)£ 1.7 (0.7)£ 1.8 (0.8)£ | .186 .001 .292 .168 |
| Modified Bruce test (ml•min–1•kg–1) | T T3w T9w T12m | 38 33 33 39 | 37.1 (11.3) 42.8 (10.3)£ 42.7 (12.1)£ 39.3 (12.6) | 26 22 23 26 | 29.6 (8.0) 32.8 (8.5)£ 32.1 (7.9)£ 31.2 (8.6) | .009 .004 .010 .138 |
| FMR indicates functional multidisciplinary rehabilitation; OP, outpatient physiotherapy; †, percent body weight; T, baseline; T3w, 3-week follow-up; T9w, 9-week follow-up; T12m, 12-month follow-up; SD, standard deviation; *, independent samples t-test (T) or analysis of covariance (T3w, T9w, T12m); £, significant within group difference compared to baseline (paired samples t-test). | ||||||
The aim of this study was to compare long-term functional status and rate of return to or maintenance at work in a non-specific LBP population randomised to a 3-week functional multidisciplinary rehabilitation or 18 supervised outpatient physiotherapy sessions during 9 weeks. The results indicate that the FMR group evolved significantly more favorably compared to the OP group in disability in the short and long terms, and in work status at long term.
The additional effects of FMR compared to OP are likely to be due to a cumulative effect of the multiple treatment modalities included in FMR, rather than every one taken individually. This is illustrated by the fact that secondary outcome differences were not as great as those in primary outcomes. Physical training components of FMR lead to improvements at short term in trunk muscle endurance, cardiovascular endurance and range of motion, but only fingertip to floor distance remained significantly improved at 12 months and favourable results in MMS in extension were obtained for OP at short term. Occupational therapy contribution translated into a tendency for better auto-evaluated lifting capacity, as assessed by the SFS, and a trend towards a better lumbar PILE in the short term only. Due to the multiple factors for incidence and recurrence of low back pain and to the heterogeneity that is characteristic of this patient population, each modality of FMR does not necessarily lead to a significant improvement in its focused area, but contributes to improvements in functional status and work capacity. This may be especially true for patients who are off work at baseline. Although this subgroup analysis was based on a small number of subjects and consequently underpowered, it resulted in a significantly better return to work rate of FMR compared to OP patients at 9 months, which tended to be maintained at 12 months. Work status was not analysed according to potential adjustments at the workplace or job changes. Such factors may partly explain the favourable work status of FMR compared to OP patients obtained at long term, as a result of the intervention of occupational therapists.
A major strength of this study is its prospective, randomised design with multiple follow-up assessments. FMR and OP patients were managed and tested by the same therapists, thus excluding any inter-rater bias. On the other hand, it rendered therapists’ blindness impossible. The chosen Krause phases ensured homogeneity of the presence and duration of work disability between the two groups. Respect for this inclusion criterion was essential, given the poor chance of returning to work in phases 7 and 8. Bendix et al. showed that the longer the time away from work, the less likely are patients to benefit from FMR [34].
The favourable effect on work status of FMR compared to OP is in line with the RCT of Jousset et al. [18] and with the conclusions of systematic reviews [14, 15], but in contradiction to the RCTs of Bendix et al. [16] and Kääpä et al. [19] as well as other systematic reviews [12, 13]. As regards disability, the difference in favour of FMR compared to OP obtained in the present study reinforces the minor but statistically significant difference reported in the RCT of Dufour et al. [17] and the conclusions of the systematic review of Guzman et al. [12], but contrasts with other RCTs [16, 18, 19] and systematic reviews [13, 14]. RCT comparison is difficult and hazardous due to the heterogeneity in the content of the interventions, the population characteristics, the selected outcomes and the duration of follow-up after treatment. Ravenek et al. suggest that the discrepancy in the reviews’ conclusions may be related to the methods used to evaluate consistency and quality of studies when determining levels of evidence [13].
As stressed by van Geen et al. [14] it should be borne in mind that the responsiveness of the questionnaires used to measure disability differs. The present study used the ODI, which is specially designed for patients with low back pain. Moreover, disability at baseline differed considerably between the present study (38.4) and the only other RCT which used the ODI (24.6) [19], suggesting that less disabled patients benefit less from FMR than more disabled patients. It is interesting to note that the present study included subacute and chronic non-specific low back pain patients, whereas only chronic patients were enrolled in previously cited RCTs, with less difference between FMR and OP. This could be an argument for patients undergoing FMR before low back pain becomes chronic.
A limitation of the present study is the large number of patients lost to follow-up (29% and 32% of FMR and OP groups respectively), which may have resulted in overestimation of improvements measured over time. Nevertheless, the sensitivity analyses showed that within groups comparisons were robust. Between groups comparisons may have been overestimated, considering a more conservative method of data imputation. This must be interpreted with caution, because baseline characteristics of patients lost to follow-up did not significantly differ from those of patients who completed all follow-up assessments. Moreover, the proportion of missing data was comparable in both groups. Random allocation of patients in FMR and OP groups led to a significant baseline difference for age, height and marital status (see table 1). Moreover, secondary variables tended to be more favourable at baseline for the FMR group than for the OP group (see table 3). However, the influence of these baseline differences between groups comparisons was corrected by the introduction of baseline value as covariate. Another limitation is that co-interventions were not recorded. Although this may have affected the internal validity of the study, it is very likely that both groups received a comparable number of additional treatments.
To conclude, the present study underlines the importance of treating all aspects of non-specific low back pain in a multidisciplinary team following cognitive-behavioural principles. Outpatient physiotherapy included active exercises, in accordance with current recommendations, but was insufficient to significantly improve functional and work status. On the other hand, these primary outcomes were significantly improved after and 1 year after functional multidisciplinary rehabilitation. The contrasting literature in this area suggests that further research is still needed. Given the high cost of health care in Switzerland, a cost-effectiveness study is needed to determine whether the benefits of functional multidisciplinary rehabilitation, compared to outpatient physiotherapy, are worth the additional costs.
The authors wish to thank the personnel of the Service of Rheumatology and particularly Mrs. Claudine Marcant-Pittet and Mrs. Anne-Françoise Gueguen for evaluating the patients, Dr. Jean Dudler for his help in recruiting the patients for this study, and Profs. Frédéric Stiefel and Jean-Blaise Wasserfallen for their advice on study design.
1 Wieser S, Horisberger B, Schmidhauser S, Eisenring C, Brugger U, Ruckstuhl A, et al. Cost of low back pain in Switzerland in 2005. Eur J Health Econ. in press.
2 Dagenais S, Caro J, Haldeman S. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J. 2008;8:8–20.
3 Swiss Federal Office of Statistics [homepage on the internet]. Bern [last accessed 16 September 2010]. Available from: http://www.bfs.admin.ch/.
4 Andersson GB. Epidemiological features of chronic low-back pain. Lancet. 1999;354:581–5.
5 Hashemi L, Webster BS, Clancy EA, Volinn E. Length of disability and cost of workers’ compensation low back pain claims. J Occup Environ Med. 1997;39:937–45.
6 Abenhaim L, Rossignol M, Valat JP, Nordin M, Avouac B, Blotman F, et al. The role of activity in the therapeutic management of back pain. Report of the International Paris Task Force on Back Pain. Spine. 2000;25:1S–33S.
7 Waddell G. Biopsychosocial analysis of low back pain. Baillieres Clin Rheumatol. 1992;6:523–57.
8 Mayer TG, Gatchel RJ. Functional restoration for spinal disorders: the sports medicine approach. Philadelphia: Lea and Febiger. 1988.
9 Poiraudeau S, Rannou F, Revel M. Functional restoration programs for low back pain: a systematic review. Ann Readapt Med Phys. 2007;50:425–9.
10 Bendix T, Bendix AF, Busch E, Jordan A. Functional restoration in chronic low back pain. Scand J Med Sci Sports. 1996;6:88–97.
11 Vanvelcenaher J. Restauration fonctionnelle du rachis dans les lombalgies chroniques. Paris: Editions Frison-Roche; 2003.
12 Guzman J, Esmail R, Karjalainen K, Malmivaara A, Irvin E, Bombardier C. Multidisciplinary rehabilitation for chronic low back pain: systematic review. BMJ. 2001;322:1511–6.
13 Ravenek MJ, Hughes ID, Ivanovich N, Tyrer K, Desrochers C, Klinger L, et al. A systematic review of multidisciplinary outcomes in the management of chronic low back pain. Work. 2010;35:349–67.
14 van Geen JW, Edelaar MJ, Janssen M, van Eijk JT. The long-term effect of multidisciplinary back training: a systematic review. Spine. 2007;32:249–55.
15 Norlund A, Ropponen A, Alexanderson K. Multidisciplinary interventions: review of studies of return to work after rehabilitation for low back pain. J Rehabil Med. 2009;41:115–21.
16 Bendix T, Bendix A, Labriola M, Haestrup C, Ebbehoj N. Functional restoration versus outpatient physical training in chronic low back pain: a randomized comparative study. Spine. 2000;25:2494–500.
17 Dufour N, Thamsborg G, Oefeldt A, Lundsgaard C, Stender S. Treatment of Chronic Low Back Pain: A Randomized, Clinical Trial Comparing Group-Based Multidisciplinary Biopsychosocial Rehabilitation and Intensive Individual Therapist-Assisted Back Muscle Strengthening Exercises. Spine (Phila Pa 1976). 2010;35:469–76.
18 Jousset N, Fanello S, Bontoux L, Dubus V, Billabert C, Vielle B, et al. Effects of functional restoration versus 3 hours per week physical therapy: a randomized controlled study. Spine. 2004;29:487–93; discussion 94.
19 Kaapa EH, Frantsi K, Sarna S, Malmivaara A. Multidisciplinary group rehabilitation versus individual physiotherapy for chronic nonspecific low back pain: a randomized trial. Spine. 2006;31:371–6.
20 Krause N, Ragland DR. Occupational disability due to low back pain: a new interdisciplinary classification based on a phase model of disability. Spine. 1994;19:1011–20.
21 Mayer TG, Gatchel RJ, Kishino N, Keeley J, Capra P, Mayer H, et al. Objective assessment of spine function following industrial injury. A prospective study with comparison group and one-year follow-up. Spine. 1985;10:482–93.
22 Fairbank JC, Couper J, Davies JB, O'Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66:271–3.
23 Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine. 2000;25:2940–52; discussion 52.
24 Vogler D, Paillex R, Norberg M, de Goumoens P, Cabri J. Cross-cultural validation of the Oswestry disability index in French. Ann Readapt Med Phys. 2008.
25 Matheson LN, Matheson ML. Spinal Function Sort. Wildwood, MO: Employment Potential Improvement Corporation. 1989.
26 Mayer TG, Barnes D, Kishino ND, Nichols G, Gatchel RJ, Mayer H, et al. Progressive isoinertial lifting evaluation. I. A standardized protocol and normative database. Spine. 1988;13:993–7.
27 Williams R, Binkley J, Bloch R, Goldsmith CH, Minuk T. Reliability of the modified-modified Schober and double inclinometer methods for measuring lumbar flexion and extension. Phys Ther. 1993;73:33–44.
28 Perret C, Poiraudeau S, Fermanian J, Colau MM, Benhamou MA, Revel M. Validity, reliability, and responsiveness of the fingertip-to-floor test. Arch Phys Med Rehabil. 2001;82:1566–70.
29 Latimer J, Maher CG, Refshauge K, Colaco I. The reliability and validity of the Biering-Sorensen test in asymptomatic subjects and subjects reporting current or previous nonspecific low back pain. Spine. 1999;24:2085–9; discussion 90.
30 Ito T, Shirado O, Suzuki H, Takahashi M, Kaneda K, Strax TE. Lumbar trunk muscle endurance testing: an inexpensive alternative to a machine for evaluation. Arch Phys Med Rehabil. 1996;77:75–9.
31 Bruce RA, Kusumi F, Hosmer D. Maximal oxygen intake and nomographic assessment of functional aerobic impairment in cardiovascular disease. Am Heart J. 1973;85:546–62.
32 McInnis KJ, Balady GJ, Weiner DA, Ryan TJ. Comparison of ischemic and physiologic responses during exercise tests in men using the standard and modified Bruce protocols. Am J Cardiol. 1992;69:84–9.
33 Ostelo RW, Deyo RA, Stratford P, Waddell G, Croft P, Von Korff M, et al. Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine. (Phila Pa 1976). 2008;33:90–4.
34 Bendix AF, Bendix T, Haestrup C. Can it be predicted which patients with chronic low back pain should be offered tertiary rehabilitation in a functional restoration program? A search for demographic, socioeconomic, and physical predictors. Spine. (Phila Pa 1976). 1998;23:1775–83; discussion 83–4.
No funding; no competing interests.