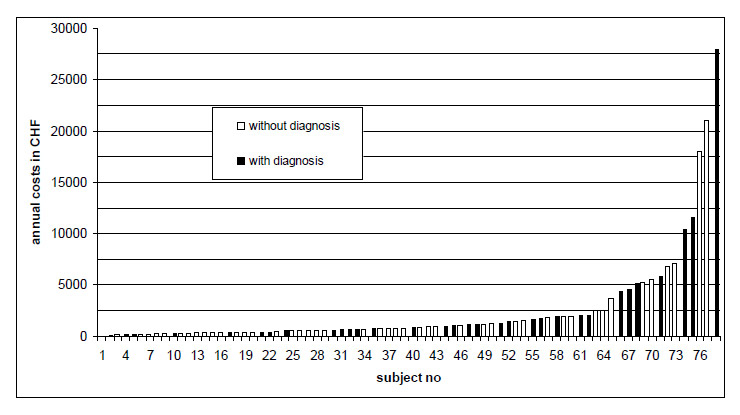
Figure 1
Distribution of annual healthcare costs by individual. N = 78.
DOI: https://doi.org/10.4414/smw.2010.13110
Migrants, especially refugees and asylum seekers, are at increased risk of multiple health problems [1–3]. Mental health problems appear to be a particularly relevant issue [1, 2, 4–6]. Many of those who leave their home countries to apply for asylum in Western countries are traumatised by war, war-like conditions, or political or ethnic oppression – these are indeed the factors mentioned in the description of a refugee as defined by the United Nations Convention Relating to the Status of Refugees [7]. However, only a small proportion of asylum seekers migrating to Western countries are eventually recognised as refugees within the meaning of the UN Convention. Acceptance rates vary considerably from country to country. For 2008 the UNHCR reports a worldwide average acceptance rate of 29% with a downward trend [8]. In Switzerland, the acceptance rate in 2008 was 23% [9].
Asylum seekers usually have restricted access to medical treatment, although international human rights conventions prescribe a right to at least basic health care. Given that this population is known to be particularly vulnerable to mental health problems [1, 2, 4, 5, 10–13], it is probable that asylum seekers are in need of more health care than residents. However, if access to medical services is restricted, actual healthcare delivery and healthcare utilisation may be insufficient or inadequate. It is thus likely that some asylum seekers receive inadequate treatment or that inappropriate treatments are administered due to mis- and/or underdiagnosis. Patients are not familiar with treatment options or the service structures available, and healthcare professionals are not sufficiently trained, skilled, or equipped to assess and treat patients from other countries and cultures [14]. However, given the lack of empirical data, very little is known about asylum seekers’ actual use of medical services or patterns of healthcare usage. To the best of our knowledge, no previous study has evaluated general healthcare use in unselected asylum seekers compared with residents, or the relationship between mental health problems and healthcare use patterns.
Switzerland admits between 15,000 and 45,000 new asylum seekers per year—one of the highest rates in first world countries in proportion to its population (7.7 million). Owing to the protracted legal procedures, most asylum seekers live in the country for several years, although the eventual acceptance rates of refugees are very low (ranging from 10% to 25%). The Swiss government provides asylum seekers with mandatory basic health care coverage. Theoretically, they have full access to a wide range of medical treatments. However, their first point of contact is usually a general practitioner (GP), who acts as a ‘gatekeeper,’ deciding whether a patient needs additional hospital treatment or referral to a specialist. As GPs do not usually use translation services, their communication with asylum speakers is extremely limited, especially concerning mental health problems [15, 16].
We aimed to assess a representative sample of adult asylum seekers after their first year of residence in Switzerland. A sample of n = 78 individuals was recruited with the help of the Swiss Federal Office for Migration, which provided us with the names and addresses of all individuals above the age of 18 years who applied for asylum after a defined point of time (1 August 2007) and were assigned to the canton of Zurich. Given our limited financial and time resources we aimed to recruit a sample of 80–100 subjects for this study. For this purpose we consecutively (according to the date of application for asylum) went through the lists provided by the Federal Office until the planned sample size was obtained. Out of 116 asylum seekers eligible we were able to locate, contact, and recruit 78 individuals (67%). Twenty individuals refused participation and 18 could not be located. The subjects who agreed to participate gave written informed consent to the interviews and to disclosure of their individual health insurance records. Recruitment and interviews took place between July 2008 and February 2009. Prior to the assessments, potential participants were informed in detail through interpreters about the aims of the study. The approximately 90-minute assessment consisted of a structured interview covering sociodemographic characteristics, reasons for flight, living conditions in Switzerland, and questionnaires on different aspects of current mental health (see Measures section for details). Trained clinical psychologists from the Department of Psychiatry at Zurich University Hospital conducted the interviews – if necessary, with the assistance of trained interpreters. All mental health questionnaires used were translated and back-translated into the 11 main languages currently spoken by asylum seekers and refugees in Switzerland (Albanian, Arabic, Bosnian, English, Farsi, French, Kurdish Kurmanci, Kurdish Sorani, Russian, Tamil, Turkish) using established translation and blind back-translation procedures [17]. The original and back-translated versions were assessed for meaning equivalence, and all discrepancies were reconciled in a consensus discussion with the psychologist and both psychologically trained translators. Most participants were able to answer the mental health questionnaires by themselves using computer-based touch screen questionnaires (MultiCASI® [18]). Individuals who did not understand any of these languages or who did not have the necessary level of literacy completed the mental health questionnaires in interpreter-assisted face-to-face interviews. Participants who experienced distress after the interview were referred to local health professionals. Participants were interviewed in their homes or at our department, at their convenience. Inclusion criteria were application for asylum in Switzerland within the defined time frame, age over 18 years, and written informed consent to participate in our study. The ethics committee of the canton of Zurich approved the study.
We assessed the current mental health status using a standardised neuropsychiatric interview (MINI) [19]. The MINI provides broad coverage of psychiatric diagnoses according to DSM-IV [20]. Additionally, several standardised self-rating questionnaires were used to assess psychopathological symptoms and quality of life. These results are not the subject of the following analyses. The health insurance company (Helsana®) provided us with complete records of the healthcare services delivered to each participant since their arrival in Switzerland. The data cover periods ranging from 11–16 months. For the ensuing analyses we standardised all measures on a 12-month basis by linear extrapolation. The files contain precise data on the nature, dates and providers of all medical interventions (in the code used by the Swiss medical tariff system). All diagnostic procedures and medications prescribed are also recorded in detail. The Swiss medical tariff system separately encodes psychotherapeutic sessions provided by psychiatrists and psychosocial counselling provided by GPs. Both treatments and prescription of psychotropic drugs (either by GPs or by psychiatrists) are counted as ‘psychiatric treatments’ and assessed for each participant. Doctors do not report medical diagnoses to the insurance company. However, the information available in the files allows for the identification of certain medical conditions – e.g. pregnancy, tuberculosis, diabetes, cancer, hypertension, traumatic injuries, and HIV. Costs associated with pregnancy and motherhood were excluded from the calculations (4 cases).
The data were coded and analysed using SPSS 17.0. Descriptive statistics were used to examine the demographic variables, characteristics of the living situation in Switzerland, and the mental health variables. Kolmogorov-Smirnov tests were used to analyse whether the interval data (age, number of visits, number of diagnoses, duration of stay) were normally distributed. One-sample t-tests (one-tailed) were used to analyse differences between our sample (n = 78) and population measures; two-sample t-tests were used to calculate differences between subgroups of the sample (normally distributed continuous data), e.g. cost differences between participants with and without a psychiatric diagnosis.
The sample consisted of 78 asylum seekers aged between 18 and 63 years. Participants were predominately male (73%) and unmarried (56%); they originated from 18 different countries. Their average duration of stay in Switzerland at the time of the interview was 14 months. At the time of the interview, 71 individuals (91%) still had their cases pending, 4 had been recognised as refugees, and 3 had a temporary humanitarian visa. Table 1 reports details of the sample’s sociodemographic characteristics.
| Table 1: Sociodemographic characteristics (N = 78). | |||
| Sociodemographic variables | |||
| Sex | Male | N (%) | 57 (73%) |
| Female | N (%) | 21 (27%) | |
| Age (in years) | M (±SD) | 29.9 (± 8.4) | |
| Marital status | Unmarried | N (%) | 44 (56%) |
| Married | N (%) | 34 (44%) | |
| Education (in years) | M (±SD) | 9.7 (± 4.6) | |
| Duration of stay in Switzerland (in months) | M (±SD) | 13.96 (± 3.7) | |
| Status of residence | Asylum seeker, case pending | N (%) | 71 (91%) |
| Temporary humanitarian visa | N (%) | 3 (4%) | |
| Permanent visa (refugee) | N (%) | 4 (5%) | |
| Region of origin | Asia (incl. Turkey) | N (%) | 37 (47%) |
| Africa | N (%) | 21 (27% ) | |
| Europe | N (%) | 20 (26%) | |
The participants showed high levels of psychopathology. Diagnostic results from the MINI International Neuropsychiatric Interview indicated that 2 of every 5 individuals in our sample had a clinically relevant mental disorder. Major depression was the most common disorder, followed by posttraumatic stress disorder (PTSD) and somatoform pain disorder. Details are presented in table 2. High rates of PTSD suggest that a large proportion of participants have experienced traumatic stress. Major depression, chronic pain, and substance abuse, as found in our sample, are also known to be frequent consequences of traumatic stress.
Twenty-nine percent of participants had at least two comorbid diagnoses; 11% had three or more diagnoses. The most frequent comorbid combination was major depression with another diagnosis, followed by PTSD with another diagnosis (see table 3 for details).
| Table 2: Psychiatric diagnoses according to DSM-IV, as determined by the MINI Neuropsychiatric Interview (N = 78). | ||
| Psychiatric diagnosis (DSM-IV) | N | % |
| Major depression (MD) | 26 | 33% |
| Posttraumatic stress disorder (PTSD) | 19 | 24% |
| Pain disorder | 10 | 13% |
| Anxiety disorder | 8 | 10% |
| Alcohol abuse | 4 | 5% |
| Table 3: Rates and types of comorbid disorders according to DSM-IV, as measured by the MINI Neuropsychiatric Interview (N = 78). | ||
| Psychiatric diagnoses (DSM-IV) | N | % |
| At least one diagnosis | 32 | 41% |
| Only one diagnosis | 9 | 11% |
| Two diagnoses | 14 | 18% |
| Three or more diagnoses | 9 | 11% |
| PTSD & any other diagnosis | 17 | 22% |
| MD & any other diagnosis | 20 | 26% |
| MD & PTSD & any other diagnosis | 7 | 9% |
The average annual healthcare cost in our sample was CHF1 24452 per individual (SD 4637). The comparable annual healthcare cost among general Swiss residents (costs per capita adjusted for age and sex) were CHF 13663 in 2008 [21]. Hence the annual cost incurred in the medical treatment of asylum seekers was almost 1.8 times that of the comparable resident population. The difference between our sample and the general population is statistically significant (t = 2.06, df = 77, p = .022**, one-tailed). The annual healthcare costs in the sample ranged from 0 to CHF 27 901, median CHF 807. Forty-seven participants (60%) scored below the population mean and 31 (40%) above. Seventeen individuals (22%) incurred healthcare costs of more than twice the population average of CHF 1366. Cost distribution in the sample shows a regular exponential increase, as is to be expected for any unselected population sample and for the general population. Linear regression with the logarithmised data provides a correlation coefficient of r = 0.965. This regular pattern of cost distribution indicates that higher average costs are unlikely to be caused by a few high cost outliers. After exclusion of the participant with the highest annual healthcare costs (CHF 27 901), the sample mean of CHF 2114 (SD 3625) is still significantly higher than the population mean (t = 1.81, df = 76, p = .037**, one-tailed).
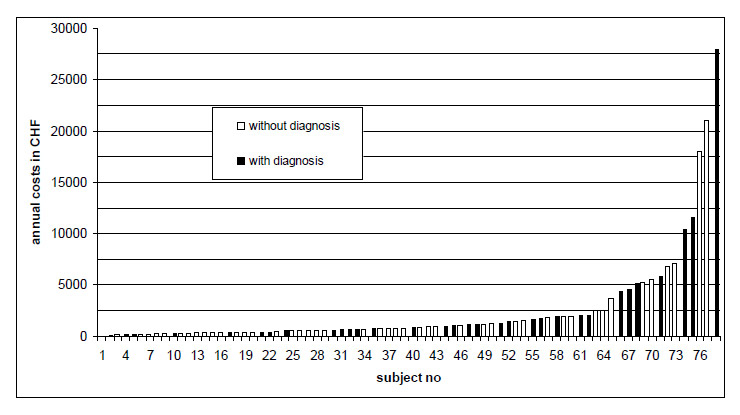
Figure 1
Distribution of annual healthcare costs by individual. N = 78.
1 Exchange rate CHF → US$: x 0.94 (Dec. 31, 2008)
2 Costs associated with pregnancy and childbirth excluded (4 cases)
3 Costs associated with pregnancy and childbirth included
As shown in table 4, the annual healthcare costs increase with the number of psychiatric diagnoses. However, the difference in costs between asylum seekers with at least one psychiatric diagnosis and those without a diagnosis failed to reach significance (t = 0.67, df = 77, p= .25, one-tailed). Details are reported in table 4. The cost differences between diagnostic subgroups and the basic population failed to reach significance. Sample sizes are too small to establish potential differences.
| Table 4: Annual healthcare costs for the Swiss resident population and by psychiatric diagnoses, as determined by the MINI Neuropsychiatric Interview. | |||
| Subgroups | N | Average annual healthcare costs (CHF) M (SD) | Percentage relative to the costs in the Swiss resident population |
| Swiss resident population (adjusted for age and sex) | 7.7m | 1,366 (SD not available) | 100% |
| Whole sample | 78 | 2,445 (4,637) | 179% |
| With major depression | 26 | 3,221 (5,807) | 235% |
| With PTSD | 19 | 3,148 (6,444) | 230% |
| With any psychiatric diagnosis | 32 | 2,889 (5,334) | 211% |
| Two or more diagnoses | 23 | 3,024 (5,763) | 221% |
| No psychiatric diagnosis | 46 | 2,136 (4,108) | 156% |
On average, participants had 10.7 (SD = 15.4, range = 0–113) appointments with a doctor (all visits, GP or specialist) per year (see table 5 for details). This is more than twice the average for the resident population [22]. The difference between our sample and the resident population is statistically significant (t = 3.95, df = 77, p < .001***, one-tailed). Participants with a psychiatric disorder reported significantly more appointments (t = 2.03, df = 31, p = .025*, one-tailed) than those without a psychiatric disorder.
| Table 5: Annual number of appointments with a doctor. | ||
| Subgroups | N | Average number of appointments M (SD) |
| Swiss resident population (adjusted for age and sex) | 7.7m | 3.8 |
| Whole sample | 78 | 10.7 (15.4) |
| Major depression | 26 | 16.5 (24.6) |
| PTSD | 19 | 18.7 (27.7) |
| Any diagnosis | 32 | 15.6 (22.4) |
| Two or more diagnoses | 23 | 16.8 (24.6) |
| No diagnosis | 46 | 7.4 (5.7) |
Although 32 participants (41%) had a clinically relevant mental disorder at the time of the interview, only 20 (26%) had received any kind of psychiatric treatment (psychotherapy, psychosocial counselling, psychopharmacotherapy or a combination of these, provided either by psychiatrists or GPs) during the previous 12 months. The “psychiatric treatment received” ranged from a single session of psychiatric counselling (by a GP) or a single prescription of antidepressants, to 9 days of inpatient treatment or 32 psychotherapy sessions. The average annual costs for psychiatric treatments in our sample amounted to CHF 352 (SD = 1633), or 14% of the total average annual healthcare costs in the sample. This is close to the average proportion of healthcare costs spent on mental health in the Swiss healthcare system in general (16%) [23]. Psychiatric drugs (antidepressants, neuroleptics, mood stabilisers, tranquillisers) accounted for only 4.5% of the costs of psychiatric treatment. Given the high psychological morbidity of the sample, the amount spent on mental health care is alarmingly low.
Only 11 of the 20 participants who received psychiatric treatment during the 12 months under investigation were diagnosed with a psychiatric disorder by the MINI, whereas 21 of those participants diagnosed with a psychiatric disorder at the time of the interview had received no psychiatric treatment. However, it should be considered that the two parameters (psychiatric treatment and diagnosis) are categorically different (treatment is a process, diagnosis a momentary condition) and cannot be easily related to each other. The nine individuals who had received treatment but showed no manifest mental disorder at the time of the assessment may have improved because of treatment. A comparison of those participants who received psychiatric treatment with those that did not receive treatment is shown in table 6.
The cost difference between those with psychiatric treatment and those without treatment – either with or without a psychiatric diagnosis – is significant (t= 2.15; df: 20, doublesided p = .043*). Differences between the subgroups do not reach significance, probably because of the small sample sizes.
| Table 6: Average annual healthcare costs, psychiatric treatment and psychiatric diagnosis. | |||
| Any diagnosis N = 32 | No diagnosis N = 46 | Total N = 78 | |
| Received any type of psychiatric treatment | CHF: 6204 (SD: 8132) N = 11 | CHF: 3584 (SD: 8132) N = 9 | CHF: 5025 (SD: 7065) N = 20 |
| Received no psychiatric treatment | CHF: 1151 (SD: 1347) N = 21 | CHF 1784 (SD: 3675) N = 37 | CHF: 1555 (SD: 3043) N = 58 |
As we did not physically examine the participants and had no access to the medical records of attending physicians, we cannot draw firm conclusions on physical diseases in our sample. However, serious medical conditions or surgical interventions are easily identifiable from insurance company records. Analysis of the data in this regard supports the assumption that serious medical problems played no major role in the sample. Two cases of tuberculosis were identified but no cases of malaria, HIV or other relevant infectious diseases. The records indicated one case of myocardial infarction and several cases of hypertension, but there did not seem to be any cases of stroke, insulin-dependent diabetes, cancer, or other distinct chronic disease. From this perspective, there are no indications that participants with severe physical illnesses or other medical outliers may have distorted the results to a relevant degree.
The results of this study confirm earlier findings that asylum seekers are a high-risk group with regard to mental health. A considerable body of literature on the mental health status of refugees traumatised by war and torture has been compiled in recent decades. Following the early work of Eitinger and Chodoff [24–26] on Holocaust survivors resettled abroad, several studies have focused on refugees from Southeast Asian war areas (Vietnam, Cambodia, Laos) resettled in Western countries [27–40]. Later, research focused on refugees from former Yugoslavia [41–48]. All these studies report considerable psychopathology and distress among traumatised refugees living away from their home countries. Some authors have presented results of longitudinal studies on the course of mental health in these populations [36, 43, 45, 49, 50, 51]. The data reveal that, although some improvements in mental health are observed over time, the general health status of traumatised refugees remains poor and unstable. Few authors have evaluated the health status (especially mental health status) of unselected asylum seekers (i.e. non-clinical and ethnically diverse samples) in Western communities. Silove et al. [4] compared Tamil asylum seekers with refugees and regular immigrants living in Australia in an attempt to analyse the specific impact of asylum-seeking procedures and legal restrictions on mental health status. Asylum seekers reported more subjective distress than recognised refugees, but the two groups did not differ on measures of psychiatric symptoms. Laban et al. [13] interviewed 294 Iraqi asylum seekers in the Netherlands using interpreters and translated instruments. They found significant relationships between psychopathology and postmigration problems such as family issues, discrimination, asylum procedures, and socioeconomic conditions.
In our sample of n = 78 unselected, non-clinical, adult asylum seekers, we found a high prevalence of mental disorders, especially major depression, PTSD, and somatoform pain. Although our results indicate an alarmingly high level of psychiatric morbidity in an unselected community sample, they are consistent with previous data on mental health in asylum seekers [3, 5, 13, 52]. The fact that these diagnoses were established through direct interviews conducted by experienced clinicians supports the reliability of the results. The nature of the disorders identified and the patterns of psychiatric comorbidity observed confirm that many of these individuals are severely traumatised. The diagnoses and patterns of comorbidity found are also largely congruent with previous findings and with our own clinical experience. It is known that postmigratory stressors, alone or in combination with earlier traumatic stress, often lead to depressive syndromes [53]. It is therefore not surprising that major depression was the most frequent mental disorder in our sample (33%). The high proportion of psychiatric comorbidity, while not uncommon in psychiatric populations in general, indicates the marked severity of the prevailing psychopathology and the high burden of disease in our sample.
Our findings provide insights into how this highly vulnerable group of individuals use the healthcare system and how adequately the medical system serves them. Because this analysis draws on health insurance company records rather than on patient self-reports (as is often the case in comparable studies), these results represent highly objective and reliable measures. We found that asylum seekers (1) incur significantly higher healthcare costs than the comparable resident population and (2) consult doctors more frequently, but (3) rarely receive specific treatment for their mental health problems.
We did not directly assess the physical health condition of our participants. But based on the analysis of insurance files there are no indications that the higher healthcare expenses and the more frequent consultations in our sample are attributable to relevant identifiable physical illnesses. Participants with mental health problems, however, visited doctors significantly more often than participants without manifest psychiatric disorders. There is a trend towards increased healthcare costs associated with poorer mental health in our sample. However, this correlation is not statistically significant, and participants without manifest mental health problems have on average used more healthcare services than the basic population. This may reflect the general stress asylum seekers are facing while waiting for their cases to be decided.
The comparably low levels of psychiatric treatments (including medication) suggest that mental disorders are frequently underdiagnosed. We should stress that there are no a priori legal or financial restrictions on psychiatric treatment for asylum seekers in the Swiss healthcare system. Doctors are able to prescribe specific treatments, but rarely do so. Language problems may be a major reason for this deficit. Communication problems also compromise the availability of appropriate treatment, even when mental disorders are correctly diagnosed. Qualified psychotherapy is often not available in the asylum seekers’ languages, making it impossible to provide many mentally ill asylum seekers with adequate treatment. This is a major deficiency of the Swiss healthcare system.
On the other hand, asylum seekers consult doctors and receive treatment more frequently, resulting in above-average healthcare costs. This somewhat contradictory finding underlines the important role of the medical system in the care of marginalised populations and the high credibility of doctors despite their occasional shortcomings [54]. It also suggests that mechanisms of somatisation may play an important role in asylum seekers’ patterns of healthcare utilisation (and in the patterns of healthcare delivery to this population).
In conclusion, we propose improvements in the Swiss healthcare system to provide ethically correct and cost-effective treatments for asylum seekers:
– Health professionals, especially GPs, should receive better training in the identification and diagnosis of mentally ill migrant patients.
– Treatment options, especially psychotherapy, should also be made available in other languages – for example, through the widespread use of interpreters.
1 Harris MF, Telfer BL. The health needs of asylum seekers living in the community. Med J Aust. 2001;175(11-12):589–92.
2 Fazel M, Wheeler J, Danesh J. Prevalence of serious mental disorder in 7000 refugees resettled in western countries: A systematic review. Lancet. 2005;365:1309–14.
3 Johnson H, Thompson A. The development and maintenance of post-traumatic stress disorder (PTSD) in civilian adult survivors of war trauma and torture: A review. Clin Psychol Rev. 2008;28:36–47.
4 Silove D, Steel Z, McGorry P, Mohan P. Trauma exposure, postmigration stressors, and symptoms of anxiety, depression and post-traumatic stress in Tamil asylum-seekers: Comparison with refugees and immigrants. Acta Psychiatr Scand. 1998;97(3):175–81.
5 Gerritsen AA, Bramsen I, Devillé W, van Willigen LH, Hovens JE, van der Ploeg HM. Physical and mental health of Afghan, Iranian and Somali asylum seekers and refugees living in the Netherlands. Soc Psychiatry Psychiatr Epidemiol. 2006;41:18-26.
6 Hollifield M, Warner TD, Nityamo L, Krakow B, Jenkins JH, Kesler J, Stevenson J, Westermeyer J. Measuring trauma and health status in refugees. JAMA. 2002;288:611–21.
7 United Nations High Commissioner for Refugees (UNHCR) The refugee convention. 1951; URL: http://www.unhcr.org/3b66c2aa10.html (accessed July 24, 2009).
8 United Nations High Commissioner for Refugees (UNHCR) 2008 Global Trends: Refugees, Asylum-seekers, Returnees, Internally Displaced and Stateless Persons, Country Data Sheets. 2009; URL: http://www.unhcr.org/4a375c426.html (accessed March 22, 2010).
9 Swiss Federal Office for Migration. Asylstatistik 2008. 2009; URL: http://www.bfm.admin.ch/etc/medialib/data/migration/statistik/asylstatistik/jahresstatistik/kommentierte_jahresstatistik.Par.0001.File.tmp/Statistik-J-d-2008-Kommentar.pdf (accessed July 27, 2009).
10 Laban CJ, Gernaat HB, Komproe IH, Schreuders BA, De Jong JT. Impact of a long asylum procedure on the prevalence of psychiatric disorders in Iraqi asylum seekers in the Netherlands. J Nerv Ment Dis. 2004;192(12):843–51.
11 Carta MG, Bernal M, Hardoy MC, Haro-Abad JM, et al. Migration and mental health in Europe (the state of the mental health in Europe working group: appendix I). Clinical Practice and Epidemiology in Mental Health. 2005;1(13):1–16.
12 Gerritsen AA, Bramsen I, Devillé W, van Willigen LH, Hovens JE, van der Ploeg HM. Use of health care services by Afghan, Iranian, and Somali refugees and asylum seekers living in the Netherlands. Eur J Public Health. 2006;16(4):394–9.
13 Laban CJ, Gernaat HB, Komproe IH, van der Tweel I, De Jong JT. Postmigration living problems and common psychiatric disorders in Iraqi asylum seekers in the Netherlands. J Nerv Ment Dis. 2005;193(12):825–32.
14 Maggi J, Cattacin S. Needed basic research in “Migration and Health” 2002–2006 in Switzerland. 2003; Bern, Swiss Federal Office of Public Health.
15 Jacobs EA, Lauderdale DS, Meltzer D, Shorey JM, Levinson W, Thisted RA. Impact of interpreter services on delivery of health care to limited-English-proficient patients. J Gen Intern Med. 2001;16(7):493–5.
16 Flores G. The impact of medical interpreter services on the quality of health care: a systematic review. Med Care Res Rev. 2005;62(3):255–99.
17 Bontempo R. Translation fidelity of psychological scales: An item response theory analysis of an individualism – collectivism scale. Journal of Cross Cultural Psychology. 1993;24:149–66.
18 Knaevelsrud C, Müller J. Multilingual Computer-Assisted Self-Interview (MultiCASI) system for psychiatric diagnostic of migrants. (Version 1.0). 2007; Heidelberg: Springer.
19 Sheehan DV, Lecrubier V, Sheehan KH, Amorim P, Janvas J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl. 20):22–33.
20 American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed.). 1994; Washington, DC: American Psychiatric Association.
21 Gemeinsame Einrichtung KVG. 2009; URL: http://www.kvg.org/ra/statistik/default.htm (accessed July 25, 2009)
22 Swiss Federal Statistical Office. Gesundheitsstatistik 2009. 2009; Neuchâtel, BFS.
23 Jäger M, Sobocki P, Rössler W. Cost of disorders of the brain in Switzerland with a focus on mental disorders. Swiss Med Wkly. 2008;12, 138(1-2):4–11.
24 Eitinger L. Pathology of the concentration camp syndrome. Arch Gen Psychiatry. 1961;5:79–87.
25 Eitinger L. Concentration camp survivors in Norway and Israel. 1964; London: Allan & Unwin.
26 Chodoff P. Late effects of the concentration camp syndrome. Arch Gen Psychiatry. 1963;8:323–33.
27 Kinzie JD. Evaluation and psychotherapy of Indochinese refugee patients. Am J Psychother. 1981;35(2):251–61.
28 Kinzie JD, Fredrickson RH, Ben R, Fleck L, Karls W. Post-traumatic stress disorder among survivors of Cambodian concentration camps. Am J Psychiatry. 1983;141:645–50.
29 Westermeyer J, Vang TF, Neider J. Refugees who do and do not seek psychiatric care: An analysis of premigratory and postmigratory characteristics. J Nerv Ment Dis. 1983;171(2):86–91.
30 Boehnlein JK, Kinzie JD, Ben R, Fleck J. One-year follow-up study of posttraumatic stress disorder among survivors of Cambodian concentration camps. Am J Psychiatry. 1985;142(8):956–9.
31 Boehnlein JK. Clinical relevance of grief and mourning among survivors of Cambodian concentration camps. Soc Sci Med.1987;25(7):765–72.
32 Boehnlein JK. A review of mental health services for refugees between 1975 and 1985 and a proposal for future services. Hosp Community Psychiatry. 1987;38(7):764–8.
33 Mollica RF, Wyshak G, de Marneffe D, Khuon F, Lavelle J. Indochinese versions of the Hopkins Symptom Checklist-25: A screening instrument for the psychiatric care of refugees. Am J Psychiatry. 1987;144(4):497–500.
34 Mollica RF, Wyshak G, Lavelle J. The psychosocial impact of war trauma and torture on Southeast Asian refugees. Am J Psychiatry. 1987;144:1567–72.
35 Carlson EB, Rosser-Hogan R. Trauma experiences, posttraumatic stress, dissociation, and depression in Cambodian refugees. Am J Psychiatry. 1991;148(11):1548–51.
36 Hauff E, Vaglum P. Chronic posttraumatic stress disorder in Vietnamese refugees. A prospective community study of prevalence, course, psychopathology, and stressors. J Nerv Ment Dis. 1994;182(2):85–90.
37 Silove D, Chang R, Manicavasagar V. Impact of recounting trauma stories on the emotional state of Cambodian refugees. Psychiatr Serv. 1995;46(12):1287–8.
38 Holtz T. Refugee trauma versus torture trauma: A retrospective controlled cohort study of Tibetan refugees. J Nerv Ment Dis. 1998;186:24–34.
39 Moisander PA, Edston E. Torture and its sequel: A comparison between victims from six countries. Forensic Sci Int. 2003;137(2-3):133–40.
40 Thapa SB, van Ommeren M, Sharma B, de Jong JT, Hauff E. Psychiatric disability among tortured Bhutanese refugees in Nepal. Am J Psychiatry. 2003;160(11):2032–7.
41 Turner SW, Gorst-Unsworth C. Psychological sequelae of torture: A descriptive model. Br J Psychiatry. 1990;157:475–80.
42 Loutan L, Subilia L. Torture et violence organisée: leur conséquences sur les requérants d’asile et les refugiés. Médecine et Hygiène. 1995;49:1942–50.
43 Weine SM, Vojvoda D, Becker DF, McGlashan TH, Hodzic E, Laub D, et al. PTSD symptoms in Bosnian refugees 1 year after resettlement in the United States. Am J Psychiatry. 1998;155(4):562–4.
44 Favaro A, Maiorani M, Colombo G, Santonastaso P. Traumatic experiences, posttraumatic stress disorder, and dissociative symptoms in a group of refugees from former Yugoslavia. J Nerv Ment Dis. 1999;187(5):306–8.
45 Mollica RF, Sarajlic N, Chernoff C, Lavelle J, Vukovic IS, Massagli MP. Longitudinal study of psychiatric symptoms, disability, mortality and emigration among Bosnian refugees. JAMA. 2001;286:546–54.
46 Moser C, Nyfeler D, Verwey M. (eds) Traumatisierungen von Flüchtlingen und Asyl Suchenden. Einfluss des politischen, sozialen und medizinischen Kontextes. 2001; Zürich: Seismo-Verlag.
47 Turner SW, Bowie C, Dunn G, Shapo L, Yule W. Mental health of Kosovan Albanian refugees in the UK. Br J Psychiatry. 2003;182:444–8.
48 Momartin S, Silove D, Manicavasagar V, Steel Z. Comorbidity of PTSD and depression: Associations with trauma exposure, symptom severity and functional impairment in Bosnian refugees resettled in Australia. J Affect Disord. 2004;80(2-3):231–8.
49 Westermeyer J, Neider J, Callies A. Psychosocial adjustment of Hmong refugees during their first decade in the United States: A longitudinal study. J Nerv Ment Dis. 1989;177(3):132–9.
50 Steel Z, Silove D, Phan T, Bauman A. Long-term effect of psychological trauma on the mental health of Vietnamese refugees resettled in Australia: A population-based study. Lancet. 2002;360(9339):1056–62.
51 Boehnlein JK, Kinzie D, Sekiya U, Riley C, Pou K, Rosborough B. A ten-year treatment outcome study of traumatized Cambodian refugees. J Nerv Ment Dis. 2004;192:658–63.
52 Silove D, Steel Z, McGorry P, Miles V, Drobny J. The impact of torture on post-traumatic stress symptoms in war-affected Tamil refugees and immigrants. Compr Psychiatry. 2002;43(1):49–55.
53 Fenta H, Hyman I, Noh S. Determinants of depression among Ethiopian immigrants and refugees in Toronto. J Nerv Ment Dis. 2004;192(5):363–72.
54 Maier T. Psychosocial and psychodynamic factors influencing healthcare utilization. Health Care Analysis. 2006;14(2):69–78.
First and foremost, we would like to thank our participants for taking part in this study. The research was funded by the Swiss Federal Office for Migration, which also aided in the recruitment of participants. Additional thanks are due to Helsana Insurance Company for providing the insurance data and to Susannah Goss for her support in editing this paper. We further thank Nadia Copiery and Andrea Staeheli for help with data collection and Hanspeter Mörgeli for statistical advice.